Abstract
Temporomandibular joint pain has various medical and dental etiological factors. The etiology of the temporomandibular joint pain is enigmatic, no single etiological factor is regarded as the cause. Its distribution is also not confined to a single area. This article presents the basic etiologic factors, its epidemiology, distribution of pain, classification of patients and the psychosocial behavior of patients suffering with temporomandibular pain. As overwhelming majority of medical and dental conditions/issues related to etiology of temporomandibular pain in patients have traditionally been presented and interpreted from the clinician's point of view.
Key Words: Musculoskeletal, pain, psychological distress, temporomandibular joint
INTRODUCTION
Temporomandibular disorder (TMD)-associated pain is the third most prevalent chronic pain condition worldwide, after tension headaches and back pain.[1,2] Temporomandibular pain embraces a spectrum of specific and nonspecific disorders that produce symptoms of pain and dysfunction of the muscles of mastication and temporomandibular joint.[2,3] Persistent musculoskeletal pain and resulting physical impairment are serious health problems that afflict a substantial proportion of the adult population. With daily lifestyle habits, working conditions and increasing pollution in the environment, all health hazards are increasing including musculoskeletal and temporomandibular joint pain. All other body pains such as neck; wrist; lower, middle and upper back are addressed by the patient, but temporomandibular joint pains were not mentioned.[4,5,6,7]
The aim of the article is to enhance our understanding of persistent temporomandibular pain, its causes and its impact on patient's lives.
SYNONYMS
TMDs is- more comprehensive term preferred by many authors and by National Institute of Health.[1] Temporomandibular pain and dysfunction syndrome is the term preferred by International Association for the study of pain.[3] Temporomandibular joint pain is the term accepted by general public including patients and patient support groups.[3]
TMDs encompass heterogeneous collection of non-malignant musculoskeletal conditions that affect the temporomandibular joint and the masticatory muscles, as well as contagious tissue components.[1] Typical complaints or findings include pain in the masticatory muscles, the preauricular area and/or the temporomandibular joints during mandibular movements such as jaw opening. Temporomandibular joint sounds such as clicking, popping or grating noises and recurrent headaches are also observed.[4,8,9]
All the conditions as well as the criteria to diagnose them vary from classification to classification, and guidelines for the evaluation, diagnosis and management of TMDs are lacking.[1] Of all the clinical problems commonly associated with TMDs, pain is the most typical, silent feature and is typically described as aching, tight, throbbing and tender.[4,10] Most of the TMD patients seek treatment because of pain which can be in the form of mild, moderate or severe. In many temporomandibular pain patients, pain is not confined to the temporomandibular region, but exceeds the boundaries of head and face, radiating to the neck, shoulders and even the upper, middle and lower back, the upper arms and the knees.[11] Most of the patients who have pain other than the joint pain do not reveal, unless specifically asked, so the clinician should be aware that certain conditions may mimic temporomandibular pain including tension-type headache, odontogenic pains, Eagle's syndrome, fibromyalgia, inflammation of the parotid gland and neoplasms. Therefore, these conditions have to be ruled out before the diagnosis of TMDs.
EPIDEMIOLOGY
The prevalence of pain in temporomandibular joint in general population lies in the range of about 10%, and the sex distribution of pain is approximately twice as common in females as males. The age distribution of pain in temporomandibular joint is within the reproductive age.[12]
Etiological and pathophysiological aspects
Many theories and etiological models have been presented by various authors in the literature which includes dental occlusal interferences, extraction of teeth for orthodontic treatment, use of certain orthodontic appliances, non-concentricity of the mandibular condyle, internal derangements, hyperactivity or hypoactivity of masticatory muscles, hyperactivity or hypoactivity of central nervous system, emotional disturbances with or without bruxism and increased psychological strain of life. The etiology of TMDs is multidimensional. Biomechanical, neuromuscular, biopsychosocial and neurobiological factors may contribute to the disorder. These factors are classified as:
Predisposing (structural, metabolic and/or psychologic conditions)
Initiating (e.g., trauma or repetitive adverse loading of the masticatory system)
Aggravating (parafunction, hormonal or psychosocial factors) to emphasize their role in the progression of TMD.[5,6,7,13,14,15,16]
Degeneration of articular structures causes evolution of noninflammatory disorders to inflammatory ones. These degenerative states enhance tissue destruction and joint dysfunction by releasing the inflammatory mediators to joint space. Increased interleukin 1 beta (IL-1ß), IL-6, tumor necrosis factor-alpha and prostaglandin E2 levels in synovial fluid are seen in internal derangements of TMJ such as anterior disc displacement and osteoarthritis. However, no one has succeeded in pointing out a single causative factor.
The degenerative condition that causes TMD pain can be classified into low-inflammatory arthritic disorders and high-inflammatory arthritic disorder [Table 1].[17]
Table 1.
Classification of temporomandibular pain disorders (TMDs)
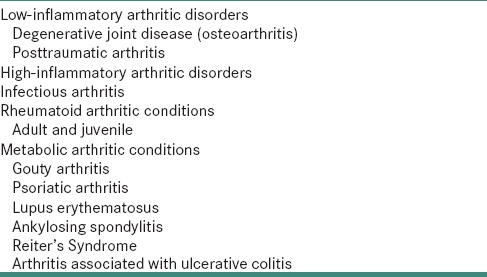
Discussing all the factors as mentioned in Table 1, in sum, the etiology of TMDs related pain still remains enigmatic.
Neurophysiological aspects
Neurophysiological mechanisms are useful to explain the phenomenon that is related to acute pain and mechanisms involved in the transition from acute to persistent pain. Increased neural activity caused by intense or prolonged noxious stimuli from the body periphery leads to hyperexcitability and sensitization of spinal nerves. Central sensitization is accompanied by metabolic, structural and morphological changes as well as by longer-lasting functional reorganizations. Many investigations have concluded that the function of the somatosensory system in temporomandibular pain patients is disturbed and hypothesized that disinhibition of the ascending reticular activity system, due to impairments in the baso-receptor mediated regulation of this system may contribute to the development and enhancement of temporomandibular pain. Ascending reticular activity system is thought to play an important role in the perceptual, physiological and psychological responses toward physical and emotional stressors.[7,18,19]
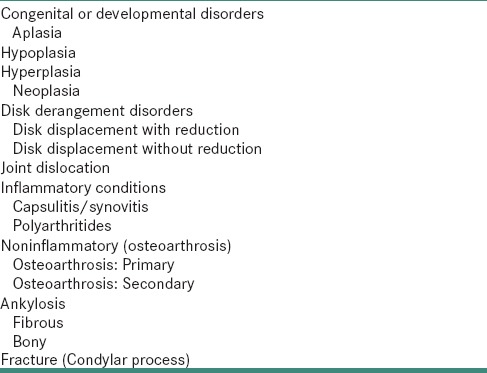
American academy of orofacial pain (AAOP) Classification of TMDs is presented in Table 2[20] and the developmental and genetic disorders associated with TMJ pain is presented in Table 3.
Table 2.
American academy of orofacial pain (AAOP) Classification of TMDs
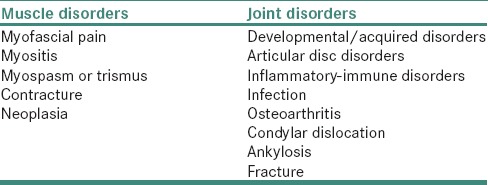
Table 3.
The developmental and genetic disorders associated with TMJ pain
Consequences and impact on the patient
Long-lasting and recurrent pain acts as a severe stressor which affects psychological state and social well-being of patient. Patients with temporomandibular pain can be classified into subgroups depending on their psychological and behavioral functioning.
Butterworth and Deardorff identified three subgroups as follows:
Psychologically normal
Hypochondriasis profile
Psychopathological appearing.
Turk et al. found that temporomandibular pain patients with comparable degrees of somatic and psychopathologic findings could be assigned to one of three subgroups.
Adaptive copers
Interpersonally distressed
Dysfunctional.
These groups were characterized by the presence or absence of specific psychosocial and behavioral features. In comparison to the other two groups, adaptive copers had low levels of pain, psychological distress (somatization and depression, affective distress, fear of pain, fear of movement and catastrophizing), characteristics of pain amplification (hyperalgesia and allodynia), pain-related impairment and higher levels of activity and controllability of their lives. The most typical feature of interpersonally-distressed individuals was their impression that they received little support for their pain condition from their families or spouses. Dysfunctionally, patients were characterized by a high level of pain, increased psychological distress, severe pain-related impairment in daily life, a reduced level of activity and the perception of loss of control over their lives. The authors also showed that these patterns were not only common to the temporomandibular pain patients but also in patients suffering from persistent headache and low back pain.
Suvinen et al. distinguished three distinctive subtypes of TMD patients:
Predominantly physical disorder group with an unremarkable psychosocial profile
Moderately distressed, behaviorally functional group
Highly distressed, psychosocially maladaptive group.
Psychological factors are known to be capable of sustaining and exacerbating temporomandibular, and other pain conditions even without nociceptive input from the periphery. They are also considered to be important for the transition from acute to persistent pain. Those who have temporomandibular pain and other persistent pain conditions reflect signs of nonspecific psychological distress such as suffering anxiety, fear, annoyance, irritability, frustration, anger, sadness and depressive preoccupation. Persistent pain affects all aspects of patient's lives including their social, familial, vocational and recreational functioning.[2,7,15,21]
CONCLUSION
Musculo-skeletal facial pain affects a significant portion of the adult population. Many etiological hypotheses have been explained. Dental factors do not seem to play the primary role for the genesis of this condition. On the other hand, neurological mechanisms including primary and secondary hyperalgesia, sensitization and central neuroplasticity, as well as psychosocial factors are considered to be important for the development and perseverance of temporomandibular pain. With regard to their psychological and behavioral characteristics, temporomandibular pain patients have shown to share typical features with other persistent pain patients. Together these findings challenge the assumption that temporomandibular pain is a primary dental condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Management of temporomandibular disorders. National institutes of health technology assessment conference statement. J Am Dent Assoc. 1996;127:1595–606. [PubMed] [Google Scholar]
- 2.Maísa Soares G, Rizzatti-Barbosa CM. Chronicity factors of temporomandibular disorders: A critical review of the literature. Braz Oral Res. 2015;29:pii: S1806-83242015000100300. doi: 10.1590/1807-3107BOR-2015.vol29.0018. [DOI] [PubMed] [Google Scholar]
- 3.Turp JC. Temporomandibular Pain – Clinical Presentation and Impact. 1st ed. Berlin: Quintessenz Verlags-GmbH; 2000. [Google Scholar]
- 4.Okeson PJ. Management of Temporomandibular Disorders and Occlusion. 3rd ed. St. Louis: Mosby; 1993. [Google Scholar]
- 5.Kirveskari P, Alanen P, Jämsä T. Association between craniomandibular disorders and occlusal interferences in children. J Prosthet Dent. 1992;67:692–6. doi: 10.1016/0022-3913(92)90173-8. [DOI] [PubMed] [Google Scholar]
- 6.Oral K, Bal Küçük B, Ebeoglu B, Dinçer S. Etiology of temporomandibular disorder pain. Agri. 2009;21:89–94. [PubMed] [Google Scholar]
- 7.Furquim BD, Flamengui LM, Conti PC. TMD and chronic pain: A current view. Dental Press J Orthod. 2015;20:127–33. doi: 10.1590/2176-9451.20.1.127-133.sar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laskin DM. Etiology of the pain-dysfunction syndrome. J Am Dent Assoc. 1969;79:147–53. doi: 10.14219/jada.archive.1969.0234. [DOI] [PubMed] [Google Scholar]
- 9.De Boever JA, Carlsson GE. Temporomandibular Joint and Masticatory Muscle Disorders. 2nd ed. Copenhagen: Mosby; 1994. pp. 171–87. [Google Scholar]
- 10.Türp JC, Kowalski CJ, Stohler CS. Temporomandibular disorders – Pain outside the head and face is rarely acknowledged in the chief complaint. J Prosthet Dent. 1997;78:592–5. doi: 10.1016/s0022-3913(97)70010-6. [DOI] [PubMed] [Google Scholar]
- 11.Türp JC, Kowalski CJ, O'Leary N, Stohler CS. Pain maps from facial pain patients indicate a broad pain geography. J Dent Res. 1998;77:1465–72. doi: 10.1177/00220345980770061101. [DOI] [PubMed] [Google Scholar]
- 12.Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993;124:115–21. doi: 10.14219/jada.archive.1993.0200. [DOI] [PubMed] [Google Scholar]
- 13.Kolbinson DA, Epstein JB, Burgess JA, Senthilselvan A. Temporomandibular disorders, headaches, and neck pain after motor vehicle accidents: A pilot investigation of persistence and litigation effects. J Prosthet Dent. 1997;77:46–53. doi: 10.1016/s0022-3913(97)70206-3. [DOI] [PubMed] [Google Scholar]
- 14.Grzesiak RC. Psychologic considerations in temporomandibular dysfunction. A biopsychosocial view of symptom formation. Dent Clin North Am. 1991;35:209–26. [PubMed] [Google Scholar]
- 15.Shaefer JR, Holland N, Whelan JS, Velly AM. Pain and temporomandibular disorders: A pharmaco-gender dilemma. Dent Clin North Am. 2013;57:233–62. doi: 10.1016/j.cden.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Christensen L, Luther F. Adults seeking orthodontic treatment: Expectations, periodontal and TMD issues. Br Dent J. 2015;218:111–7. doi: 10.1038/sj.bdj.2015.46. [DOI] [PubMed] [Google Scholar]
- 17.Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J Dent Res. 2008;87:296–307. doi: 10.1177/154405910808700406. [DOI] [PubMed] [Google Scholar]
- 18.Lund JP, Sessle BS. Temporomandibular Joint and Masticatory Muscle Disorders. 2nd ed. Copenhagen: Mosby; 1994. Neurophysiological mechanisms; pp. 188–207. [Google Scholar]
- 19.Chaudhuri SK. Concise Medical Physiology. 4th ed. Calcutta: New Central Book Agency; 2002. [Google Scholar]
- 20.Dworkin SF, LeResche L, DeRouen T, Von Korff M. Assessing clinical signs of temporomandibular disorders: Reliability of clinical examiners. J Prosthet Dent. 1990;63:574–9. doi: 10.1016/0022-3913(90)90079-r. [DOI] [PubMed] [Google Scholar]
- 21.Dworkin SF. The case for incorporating biobehavioral treatment into TMD management. J Am Dent Assoc. 1996;127:1607–10. doi: 10.14219/jada.archive.1996.0094. [DOI] [PubMed] [Google Scholar]


