Abstract
Pathology practice is significantly advanced in various frontiers. Therefore, “slide less digital” pathology will not be a mere imagination in near future. Digitalization of histopathological slides (whole slide imaging [WSI]) is possible with the help of whole slide scanner. The WSI has a positive impact not only in routine practice but also in research field, medical education and bioindustry. Even if digital pathology has definitive advantages, its widespread use is not yet possible. As it is an upcoming technology in our field, this article is aimed to discussessential aspects of WSI.
Key Words: Digital pathology, medical education, telepathology, whole slide imaging
INTRODUCTION
The current imaging modalities in pathology practice are static photomicrography of the slide, slide scanning by robotic microscope and whole slide imaging (WSI). Wetzel and Gilbertson developed automated WSI system in 1999 and since then methodology of imaging has been changing slowly but steadily.[1]
Whole slide image (virtual image, digital slides) denote a digitalized image of entire histopathology slide or a selected area of it.[2] These digital images have high-resolution and offer access to all areas on a slide. These images can be viewed on personal computers, laptops or iPhones in any magnification.[3]
DIGITALIZATION OF IMAGES
The digital imaging has four important steps: Image acquisition, storage, editing and display of images.[4] Digitalization is performed with the help of WSI scanners, which has a hardware and software component. Hardware component is for handling and scanning the slides, storing the images, transmission and display of the images to pathologists. Software part facilitates formatting, compressing and viewing the images. Other important requirements associated with WSI system is high-speed internet connection and security measures to protect patient information.[5]
Slide scanning can be done in tile or linear pattern. In tile pattern, the slide is scanned as a series of rectangular tiles [Figure 1a and b]. In linear pattern, image acquisition is done as long narrow strips [Figure 1c]. Focusing strategies can also vary among scanners. In “focus every field” method [Figure 1a], each field/tile is auto-focused and is imaged. It is an accurate but time-consuming method. In “focus every nth field” method [Figure 1b], focusing occurs every nth field. It is a faster and simpler method. “Focus map” method [Figure 1c] can be used with either tile or line pattern of scanning. Here, focus points are distributed over the tissue forming a surface. It is faster but less accurate method.[6,7]
Figure 1.
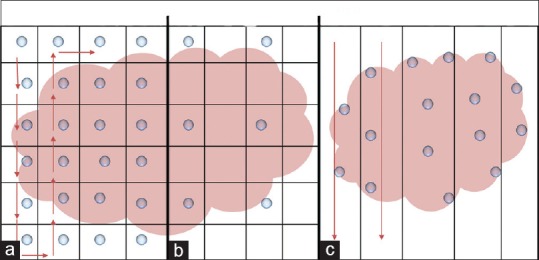
(a and b) Tile pattern of scanning. The arrows show direction of scanning. Blue dots in 1a indicate “focus every field” method. Dots in 1b indicate “focus every nth field” method. (Courtesy: Dr. Toby C. Cornish, PhD, Assistant Professor of Pathology, John Hopkins Medicine). (c) Linear pattern of scanning. Blue dots in 1c indicate “focus map” method ( = focus point,
= focus point,  = direction of scanning)
= direction of scanning)
WSI can be broadly divided into bright field, fluorescence and multispectral. Bright field WSI is the most common and least expensive type of method. Fluorescent WSI works on the same principle as a standard fluorescence microscope and only tile scanners are appropriate for fluorescence scanning. It is mainly used with immunofluorescence and fluorescent in situ hybridization (FISH).[8]
Multispectral imaging is a specialized form of digital microscopy for capturing spectral information across the visible range of light to near infrared bands. Multispectral systems are capable of working with fluorescence or bright field-based analysis.[1] Spectral imaging helps fluorescent imaging to overcome problems created by autofluorescence in tissue specimens.[1,9] The main disadvantage is its slow working pattern and complexity of the sample preparation.[9]
Scanning of slides occurs at multiple planes (x, y and z-axis) and magnifications.[5] Finally, small images are digitally “knits” into a single large image. Many scanners have auto loading facility where up to 200 slides can be loaded in the racks instead of one slide at a time.[3]
WHOLE SLIDE IMAGING FILE SIZE AND FORMAT
The file size of digital images is large, which comes in gigabits. As it is difficult to store such large files, they are usually compressed using Joint Photographic Experts Group (JPEG) or JPEG 2000 algorithms.[10,11]
APPLICATIONS OF WHOLE SLIDE IMAGING
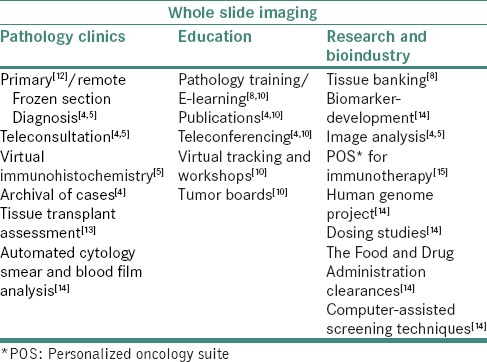
Different sectors of pathology are aided by WSI. Applications of WSI are summarized in Table 1.
Table 1.
Applications of whole slide imaging
WHOLE SLIDE IMAGING IN ROUTINE PRACTICE AND TELEPATHOLOGY
Digital slides are currently entering into day-to-day pathology practice. Adoption of WSI for routine diagnostic procedures has been done only in few centers.[4,5,16] Digital slides offer several advantages over glass slides such as portability and ease of sharing.[4,5]
According to Jen et al., digital slides are reliable for the evaluation of renal allograft biopsies.[13] Krishnamurthy et al. compared digital slides with optical microscopy for interpretation of breast carcinoma tissues. They concluded that both methods have similar accuracy, precision and reproducibility in interpretation.[12]
Good correlation between standard glass slide and digital slides are noted with gastrointestinal,[17] pulmonary[18] and prostate[19] specimens.
Telepathology system includes a digital imaging station, telecommunications network to transmit images and monitor or screen to remotely view the digital images. WSI telepathology has several advantages over telepathology using precaptured still images. Accessibility to an entire digital slide, the ability to choose automated or manual scanning, high-resolution of images and the option to use software for image analysis are main advantages of WSI telepathology.[4]
Digitalization combined with telepathology is helpful when there is a shortage of pathologists, when the hospital is in remote location with large number of difficult cases/frozen sections, which require rapid interpretations.[5,20] The University Health Network Canada found this technology safe, accurate and reliable.[5] According to Piccolo et al., telepathology for dermatologic diagnosis appears to be reliable.[21]
WHOLE SLIDE IMAGING FOR MEDICAL EDUCATION AND RESEARCH
Many medical schools accepted digital slides for undergraduate and resident training.[22,23] According to Pantanowitz, this is the best possible application for pathology education.[4] At the Poznan University of Medical Sciences in Poland, WebMicroscope (online interactive teaching and examination platform) facilitate accessibility to pathology for dental students.[24]
Digital slides are easy to handle in many ways.[3] In newly established medical and dental colleges, there will be shortage of histopathological slides and microscopes. Digital slides can encourage self-study as it can view on laptop or iPhones.[25] Online slide-sharing services such as PathXchange, Slide2Go provide accessibility to online virtual teaching sets.[10,26] Case presentations can be made more effective and interactive with help of digital images. It takes less preparation time than photographing the histopathological details. Salient pathological features can be marked on digital slides for teaching purpose and presentations.[3]
Most common problems encountered with fluorescent labels, especially in sensitive research areas such as genomic FISH, are small signal size and fading of fluorescent signals which can leads to false negative results. WSI reveals these small signals by scanning several focal planes through the sample (z-stacking) and these digital slides act as permanent records. Therefore, WSI is an accurate method to assess quantification and location of gene/chromosome.[8] Tissue microarray (TMA) has been extensively used for biomarker screening and validation studies in cancer research and toxicology testing. TMA image acquisition is a tedious procedure with optical microscopy. Digital TMA is more ergonomic and accurate.[8,27] Digital pathology can also assist virtual tumor banks such as the European human frozen tumor tissue bank.[28]
WHOLE SLIDE IMAGING FOR IMAGE ANALYSIS
WSI image analysis assesses cytomorphometry, antibodies detection and quantification of biomarkers.[5]
Slodkowskaet al. tried to detect accuracy of Ki-67 assessment in brain tumors with computer-assisted image analysis using WSI. They proved that computer-assisted image analysis using WSI can be an effective alternative.[29] Virtual immunohistochemistry is done routinely for human epidermal growth factor receptor 2, estrogen receptor and progesterone receptor analysis.[4,5,30] Biomarker quantification in TMA can be more accurately done with the automated image analysis options.[8] Multispectral image analysis is valuable tool in cytopathology to differentiate the similar lesions.[31]
VALIDATION OF WHOLE SLIDE IMAGING SYSTEM
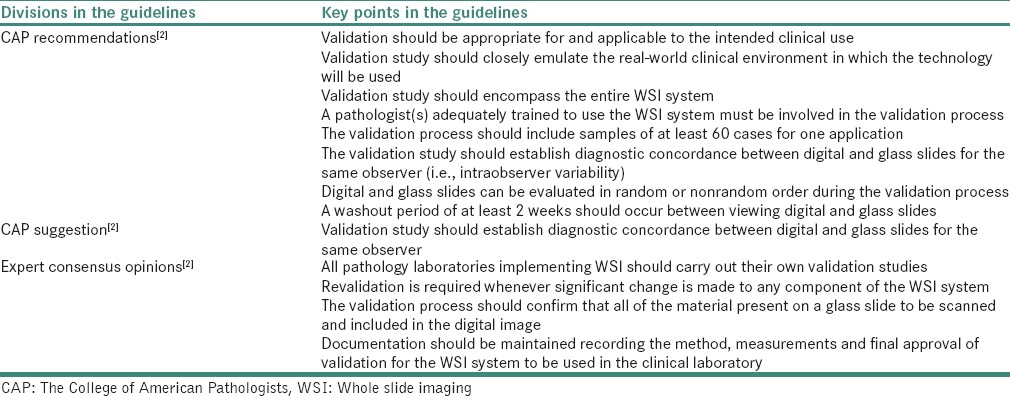
The Food and Drug Administration included WSI in Class III (highest risk) medical devices. Class III devices require quality system regulation and premarket approval.[32] Therefore, validation of WSI is vital to ensure its diagnostic performance. Currently, there are no standard guidelines for validation of WSI.[2]
The College of American Pathologists's (CAP) Pathology and Laboratory quality center proposed certain guidelines for validation of WSI.[2] CAP guidelines are summarized in Table 2.
Table 2.
The College of American Pathologists guidelines regarding validation of whole slide imaging
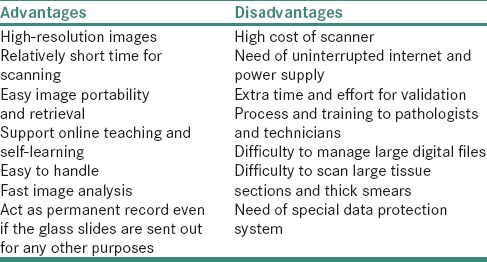
ADVANTAGES OF WHOLE SLIDE IMAGING
Digital slides have several advantages over conventional method. Digitalization provides high-resolution digital images within relatively short time span. Redondo et al. compared digital slides with photomicrographs taken with help of optical microscope. Better image quality in term of color and contrast was noted with digital slides. Sharma et al. reported that some attributes of digital images might be better than conventional methods such as portability, archiving, sharing and performing image analysis.[22] Ramey et al. reported positive results in terms of concordance when virtual slides of frozen sections were reviewed on a mobile device (iPad).[33,34]
Easy retrieval of archival images is another advantage. There will not be any issue related to slide breakage and fading of stains. Ability to make use of computer-aided image analysis becomes possible by the advent of digital images. Quality assurance and testing can be done easily with the use of digital slides. It can also act as a permanent record of sent-out slides, slides sent for medico legal cases and digital image analysis.[4,5]
DISADVANTAGES OF WHOLE SLIDE IMAGING
However, the cost for infrastructure, additional human resources and validation of the process cannot be affordable for institutions/laboratories in developing countries.
The pathologist, histotechnologists and information technology staffs who form the backbone of telepathology team should be available at the center. Continuous supply of power during overnight scanning, uninterrupted internet services and high-resolution monitors are other difficult areas.[5] Technical problems such as scanning difficulties, hardware and software problems are main limitations for WSI telepathology.[4]
Large size of the digital file would be an issue while digital archiving of slides. Z-scanning of glass slides increases scanning time and file size. Few currently available scanners can afford slides from large tissue blocks.[35] It was also observed by some investigators that the time required to review a virtual slide took longer than that needed to examine a glass slide.
Other issues limiting the use of digital pathology include the perception among pathologists that WSI systems are inferior in terms of performance and legal issues related to teleconsultation across states and internationally.[1,5]
Quality of virtual slides depends on the quality of the original slide to a certain extent. The glass slides to be scanned have to be free of artifacts such as folds, knife marks, air bubbles and stain deposits. Current scanning technology does not satisfactorily accommodate thick smears and three-dimensional cell groups in cytopathology.[3] Inadequate clinical data (gross pathology description, prior pathology reports, clinical history), missed tissue on the digital slide, pathologists' lack of experience using a WSI system can lead to erroneous diagnosis.[36] Table 3 summarizes the advantages and disadvantages of WSI.
Table 3.
Advantages and disadvantages of whole slide imaging
HOW TO OVERCOME LIMITATIONS OF WHOLE SLIDE IMAGING?
The main limitations of WSI system are its high cost and lack of proper training for the use of the new technology. Discrepancies in diagnoses between digital and glass slides were reported in few publications.[12]
Discrepancies in diagnoses between digital and glass slides were attributed to poor image quality, rarely missed tissue on the digital image, inadequate clinical data and pathologists' lack of experience using the WSI system. Increased time taken for digital slide analysis is perhaps because of the inherent learning curve associated with the new technology.[12] Proper training of pathologists and technicians could overcome these problems. It is still difficult to scan thick smears using WSI. This can be overcome by multiplane scanning along multiple z-axes or intercalation of scanned images along different focal points.[4]
WSI was perceived to be more time-consuming than optical microscopy.[12] Independent dual sensor scanning is helpful to reduce the time for image acquisition.[7] According to the study conducted by Yagi and Gilbertson, thinner tissue sectioning (by automated tissue sectioning) significantly reduces slide scanning times and improve image quality.[37]
The main limitation, i.e., cost of scanners, is expected to be decreased by invention of new technologies for economic manufacturing. This may lead to adoption of WSI even in developing countries.
CONCLUSION
Until now, microscopes remain to be the cornerstone of pathology practice. However, in near future, slide scanners can share that position. More accurate and speedy diagnosis of lesions is the ultimate goal of pathology practice regardless of the methods/instruments used. A state of mind that accepts and adapts to the better changes is the most important tool to overcome any limitation.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Toby C. Cornish, MD, PhD, Assistant Professor of Pathology, John Hopkins Medicine. Figure 1a–c in this article is based on his educative communication – “An introduction to digital whole slide imaging and whole slide image analysis.”
REFERENCES
- 1.Ghaznavi F, Evans A, Madabhushi A, Feldman M. Digital imaging in pathology: Whole-slide imaging and beyond. Ann Rev Pathol Mech Dis. 2013;8:331–59. doi: 10.1146/annurev-pathol-011811-120902. [DOI] [PubMed] [Google Scholar]
- 2.Pantanowitz L, Sinard JH, Henricks WH, Fatheree LA, Carter AB, Contis L, et al. Validating whole slide imaging for diagnostic purposes in pathology: Guideline from the College of American Pathologists Pathology and Laboratory Quality Center. Arch Pathol Lab Med. 2013;137:1710–22. doi: 10.5858/arpa.2013-0093-CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandra M. Digital pathology slides in medical education. Indian J Dermatopathol Diagn Dermatol. 2014;1:17–20. [Google Scholar]
- 4.Pantanowitz L. Digital images and the future of digital pathology. J Pathol Inform. 2010;1:15. doi: 10.4103/2153-3539.68332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pantanowitz L, Valenstein PN, Evans AJ, Kaplan KJ, Pfeifer JD, Wilbur DC, et al. Review of the current state of whole slide imaging in pathology. J Pathol Inform. 2011;2:36. doi: 10.4103/2153-3539.83746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parwani AV, Feldman M, Balis U, Pantanowitz L. Digital imaging. In: Pantanowitz L, Balis UJ, Tuthill JM, editors. Pathology Informatics: Theory and Practice. Canada: ASCP Press; 2012. pp. 231–56. [Google Scholar]
- 7.Montalto MC, McKay RR, Filkins RJ. Autofocus methods of whole slide imaging systems and the introduction of a second-generation independent dual sensor scanning method. J Pathol Inform. 2011;2:44. doi: 10.4103/2153-3539.86282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krenacs T, Zsakovics I, Micsik T, Fonyad L, Varga SV, Ficsor L. Digital microscopy – The upcoming revolution in histopathology teaching, diagnostics, research and quality assurance. In: Vilas M, Díaz M, editors. Microscopy: Science, Technology, Applications and Education. Badajoz: Formatex Research Center; 2010. pp. 965–77. [Google Scholar]
- 9.Levenson RM, Fornari A, Loda M. Multispectral imaging and pathology: Seeing and doing more. Expert Opin Med Diagn. 2008;2:1067–81. doi: 10.1517/17530059.2.9.1067. [DOI] [PubMed] [Google Scholar]
- 10.Pantanowitz L, Szymas J, Yagi Y, Wilbur D. Whole slide imaging for educational purposes. J Pathol Inform. 2012;3:46. doi: 10.4103/2153-3539.104908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khushi M, Edwards G, de Marcos DA, Carpenter JE, Graham JD, Clarke CL. Open source tools for management and archiving of digital microscopy data to allow integration with patient pathology and treatment information. Diagn Pathol. 2013;8:22. doi: 10.1186/1746-1596-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krishnamurthy S, Mathews K, McClure S, Murray M, Gilcrease M, Albarracin C, et al. Multi-institutional comparison of whole slide digital imaging and optical microscopy for interpretation of hematoxylin-eosin-stained breast tissue sections. Arch Pathol Lab Med. 2013;137:1733–9. doi: 10.5858/arpa.2012-0437-OA. [DOI] [PubMed] [Google Scholar]
- 13.Jen KY, Olson JL, Brodsky S, Zhou XJ, Nadasdy T, Laszik ZG. Reliability of whole slide images as a diagnostic modality for renal allograft biopsies. Hum Pathol. 2013;44:888–94. doi: 10.1016/j.humpath.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 14.Soenksen D. Digital pathology at the crossroads of major health care trends: Corporate innovation as an engine for change. Arch Pathol Lab Med. 2009;133:555–9. doi: 10.5858/133.4.555. [DOI] [PubMed] [Google Scholar]
- 15.Dander A, Baldauf M, Sperk M, Pabinger S, Hiltpolt B, Trajanoski Z. Personalized Oncology Suite: Integrating next-generation sequencing data and whole-slide bioimages. BMC Bioinformatics. 2014;15:306. doi: 10.1186/1471-2105-15-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slodkowska J, Pankowski J, Siemiatkowska K, Chyczewski L. Use of the virtual slide and the dynamic real-time telepathology systems for a consultation and the frozen section intra-operative diagnosis in thoracic/pulmonary pathology. Folia Histochem Cytobiol. 2009;47:679–84. doi: 10.2478/v10042-010-0009-z. [DOI] [PubMed] [Google Scholar]
- 17.Molnar B, Berczi L, Diczhazy C, Tagscherer A, Varga SV, Szende B, et al. Digital slide and virtual microscopy based routine and telepathology evaluation of routine gastrointestinal biopsy specimens. J Clin Pathol. 2003;56:433–8. doi: 10.1136/jcp.56.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slodkowska J, Chyczewski L, Wojciechowski M. Virtual slides: Application in pulmonary pathology consultations. Folia Histochem Cytobiol. 2008;46:121–4. doi: 10.2478/v10042-008-0018-3. [DOI] [PubMed] [Google Scholar]
- 19.Fine JL, Grzybicki DM, Silowash R, Ho J, Gilbertson JR, Anthony L, et al. Evaluation of whole slide image immunohistochemistry interpretation in challenging prostate needle biopsies. Hum Pathol. 2008;39:564–72. doi: 10.1016/j.humpath.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Feldman MD. Beyond morphology: Whole slide imaging, computer-aided detection, and other techniques. Arch Pathol Lab Med. 2008;132:758–63. doi: 10.5858/2008-132-758-BMWSIC. [DOI] [PubMed] [Google Scholar]
- 21.Piccolo D, Soyer HP, Burgdorf W, Talamini R, Peris K, Bugatti L, et al. Concordance between telepathologic diagnosis and conventional histopathologic diagnosis: A multiobserver store-and-forward study on 20 skin specimens. Arch Dermatol. 2002;138:53–8. doi: 10.1001/archderm.138.1.53. [DOI] [PubMed] [Google Scholar]
- 22.Sharma G, Chenevert J, Dangott BJ, Muse A, Duboy JD, Pantanowitz L, et al. Development of a head and neck pathology slide teaching set for trainee education. J Pathol Inform. 2010;1:38. doi: 10.4103/2153-3539.63822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weaker FJ, Herbert DC. Transition of a dental histology course from light to virtual microscopy. J Dent Educ. 2009;73:1213–21. [PubMed] [Google Scholar]
- 24.Szymas J, Lundin M. Five years of experience teaching pathology to dental students using the WebMicroscope. Diagn Pathol. 2011;6(Suppl 1):S13. doi: 10.1186/1746-1596-6-S1-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Betigeri AM, Aparna P, Pasupathi P. Could India become the digital pathology hub of the future? A consideration of the prospects telepathology outsourcing. Int J Biol Med Res. 2010;1:300–2. [Google Scholar]
- 26.Conran R, Fontelo P, Liu F, Fontelo M, White E. Slide2Go: A virtual slide collection for pathology education. AMIA Annu Symp Proc. 2007;11:918. [PubMed] [Google Scholar]
- 27.Whiteford CC, Bilke S, Greer BT, Chen Q, Braunschweig TA, Cenacchi N, et al. Credentialing preclinical pediatric xenograft models using gene expression and tissue microarray analysis. Cancer Res. 2007;67:32–40. doi: 10.1158/0008-5472.CAN-06-0610. [DOI] [PubMed] [Google Scholar]
- 28.Teodorovic I, Isabelle M, Carbone A, Passioukov A, Lejeune S, Jaminé D, et al. TuBaFrost 6: Virtual microscopy in virtual tumour banking. Eur J Cancer. 2006;42:3110–6. doi: 10.1016/j.ejca.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 29.Slodkowska J, Markiewicz T, Grala B, Kozlowski W, Papierz W, Pleskacz K, et al. Accuracy of a remote quantitative image analysis in the whole slide images. Diagn Pathol. 2011;6(Suppl 1):S20. doi: 10.1186/1746-1596-6-S1-S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bloom K, Harrington D. Enhanced accuracy and reliability of HER-2/neu immunohistochemical scoring using digital microscopy. Am J Clin Pathol. 2004;121:620–30. doi: 10.1309/Y73U-8X72-B68T-MGH5. [DOI] [PubMed] [Google Scholar]
- 31.Mansoor I, Zalles C, Zahid F, Gossage K, Levenson RM, Rimm DL. Fine-needle aspiration of follicular adenoma versus parathyroid adenoma: The utility of multispectral imaging in differentiating lesions with subtle cytomorphologic differences. Cancer. 2008;114:22–6. doi: 10.1002/cncr.23252. [DOI] [PubMed] [Google Scholar]
- 32.FDA. U.S. Food and Drug Administration. Device Classification. Medical Devices. [Last accessed on 2015 Jul 22]. Available from: http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/Overview/ClassifyYourDevice/default.htm .
- 33.Ramey J, Fung KM, Hassell LA. Use of mobile high-resolution device for remote frozen section evaluation of whole slide images. J Pathol Inform. 2011;2:41. doi: 10.4103/2153-3539.84276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Redondo R, Bueno G, Cristóbal G, Vidal J, Déniz O, García-Rojo M, et al. Quality evaluation of microscopy and scanned histological images for diagnostic purposes. Micron. 2012;43:334–43. doi: 10.1016/j.micron.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 35.Camparo P, Egevad L, Algaba F, Berney DM, Boccon-Gibod L, Compérat E, et al. Utility of whole slide imaging and virtual microscopy in prostate pathology. APMIS. 2012;120:298–304. doi: 10.1111/j.1600-0463.2011.02872.x. [DOI] [PubMed] [Google Scholar]
- 36.Jara-Lazaro AR, Thamboo TP, Teh M, Tan PH. Digital pathology: Exploring its applications in diagnostic surgical pathology practice. Pathology. 2010;42:512–8. doi: 10.3109/00313025.2010.508787. [DOI] [PubMed] [Google Scholar]
- 37.Yagi Y, Gilbertson JR. A relationship between slide quality and image quality in whole slide imaging (WSI) Diagn Pathol. 2008;3(Suppl 1):S12. doi: 10.1186/1746-1596-3-S1-S12. [DOI] [PMC free article] [PubMed] [Google Scholar]


