Abstract
Liposarcomas are extremely rare in the oral cavity. Less than 100 cases of oral liposarcoma have been reported in the world wide literature, mostly occurring in the buccal mucosa, whereas only <10 cases have been reported in the floor of the mouth. We present a rare case of oral liposarcoma that occurred in the floor of the mouth of a 45-year-old female patient. She had a history of two previous recurrences and underwent surgical excision with 24 months of follow-up. Clinical as well as histopathological features and therapeutic approaches of liposarcomas are discussed here, and a literature review is presented. Intraoral liposarcomas have a high rate of local recurrences but generally favorable prognosis based on the histopathologic subtype, location and clear surgical margins. Conservative surgical therapy without adjuvant chemoradiotherapy is recommended, due to the rarity of distant metastasis.
Key Words: Floor of the mouth, head and neck liposarcoma, well-differentiated liposarcoma
INTRODUCTION
Liposarcoma is one of the most common malignant mesenchymal neoplasms of adipose tissue, which was first described by Virchow in 1857.[1,2] It accounts for approximately 20% of all soft tissue sarcomas and occurs mostly in lower extremities and retroperitoneum.[3] Up to 9% of liposarcomas are found in the head and neck area.[2] Oral liposarcomas have been reported mainly in the buccal mucosa, with other sites including the floor of the mouth, tongue, palate and mandible.[4,5,6] Liposarcomas can attain very large sizes but those identified in head and neck rarely exceed 10 cm.[3]
Dedifferentiated liposarcoma, myxoid liposarcoma, pleomorphic liposarcoma and liposarcoma not otherwise specific are the four forms of liposarcomas in the recently updated World Health Organization (WHO) classification of soft tissue tumors with unique clinical settings and behaviors.[7] In this new classification, atypical lipomatous tumor/well-differentiated liposarcoma (ALT/WDL) has been described as an intermediate, locally aggressive adipocytic tumor and is divided into three main subgroups: Adipocytic, sclerosing and inflammatory types.
Here, we present a rare case of WDL occurring in floor of the mouth. We also present a review of the current published data.
CASE REPORT
A 45-year-old female patient was referred to the cancer institute in June 2014 for the assessment of a painless and slow growing nodular swelling in the floor of the mouth. Intraoral examination revealed a firm, oval mobile mass measuring 6 cm in diameter, resembling a benign tumor on the left side of the floor of the mouth. The previous medical history of the patient showed that the lesion was first diagnosed as a fatty tissue with lymphoid nodule measuring 2 cm in greatest diameter in the same area in 2006. After 3 years, the lesion had recurred, was diagnosed as angiolipoma in another pathology center in 2009. The patient believed that the lesion had again enlarged very slowly for the third time since the last excision in 2009 and did not seek any treatments until 2014. The lesion was then removed with an excisional biopsy under local anesthesia. On gross examination, it appeared as multiple pieces of creamy-brownish tissue with soft to elastic consistency measuring 6 cm in greatest diameter. The otherwise past medical history of the patient was noncontributory.
Microscopic examination revealed a neoplastic tissue composed of fibrotic zones with infiltration of numerous highly atypical bizarre spindle cells with hyperchromatic nuclei showing slight variation in size and shape [Figure 1]. Univacuolated and multivacuolated lipoblasts [Figure 2] were also noted. These lipoblasts were numerous, alternating and intermingling with slightly pleomorphic adipocytes. Patchy lymphoid infiltration, mast cells and perineural invasion were also present. The neoplastic cells expressed immunoreactivity for S100, Ki67 (3%) and focal but strong nuclear staining for MDM2 [Figure 3]. The diagnosis of sclerosing type of ALT/WDL was made according to the above histopathologic features.
Figure 1.
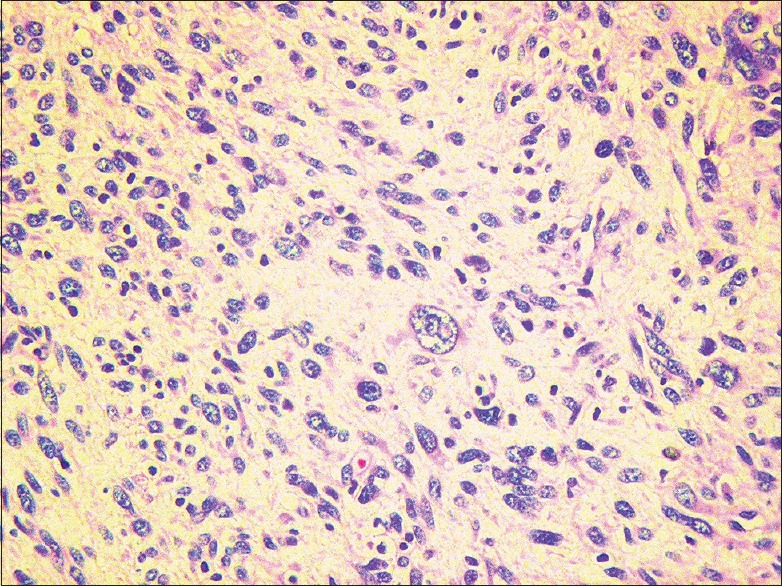
Neoplastic tissue composed of infiltrating numerous highly atypical bizarre spindle cells with hyperchromatic nuclei showing slight variation in size and shape (H&E stain, ×100)
Figure 2.
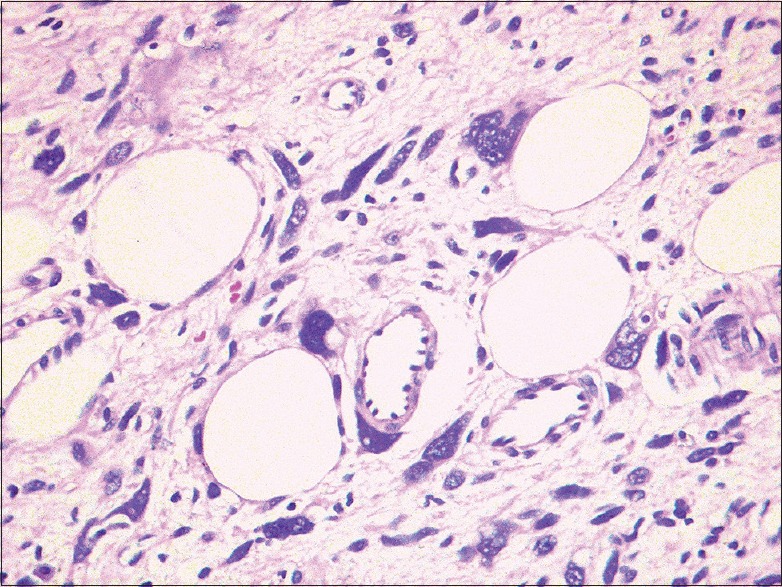
Univacuolated and multivacuolated nucleated lipoblasts were seen among the bizarre spindle cells (H&E stain, ×400)
Figure 3.
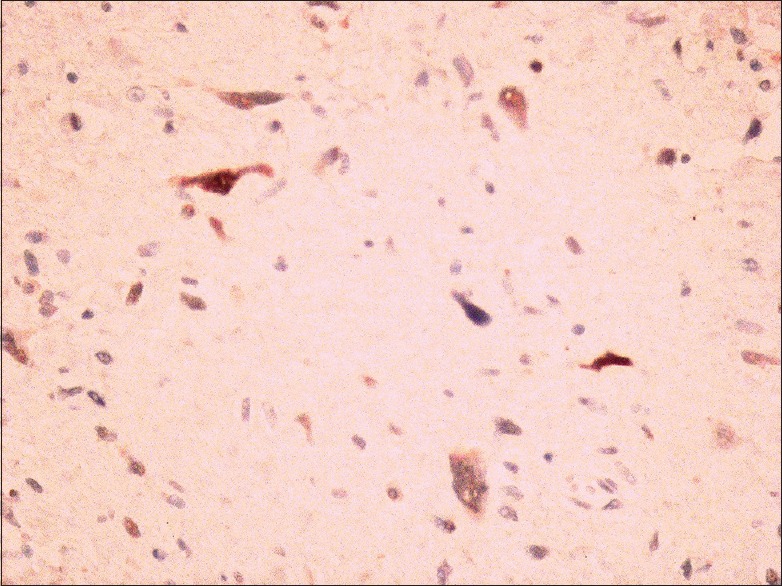
Neoplastic cells showed focal but strong positivity for MDM2 (IHC stain, ×400)
The patient refused to undergo any radiation or chemotherapy and decided to be followed every 3 months. At 24 months of follow-up, the patient remained free of disease, without any obvious signs of recurrences on clinical examination and also on cervical magnetic resonance imaging findings.
DISCUSSION
Mesenchymal malignant tumors constitute about 1% of all neoplasms, 20% of which are liposarcomas.[2,8,9] Head and neck liposarcomas are uncommon, including 5–9% of all liposarcomas,[10,11] involving neck (19%), face (13%), larynx (9%), pharynx, dura and orbit (each one 6%), oral cavity (5%), ear/mastoid (2%), mandible (2%) and parotid (1%).[7,12] The peak incidence of all liposarcomas ranges between 40–60 years and men are more frequently affected than women.[2] Oral liposarcomas have been reported to occur mainly in the buccal mucosa (38%) and tongue (33%), followed by the palate (7%) and floor of the mouth (7%).[2,5,13] Liposarcomas grow slowly and silently and most patients have no symptoms until the tumor reaches a size large enough to cause pain, tenderness or functional disturbances. They are usually grossly well-circumscribed neoplasms, not encapsulated, firmer and less easily compressible than lipomas.[4] To the best of our knowledge, the reported cases of liposarcoma in the floor of the mouth in the English language literature are less than the number of fingers of our hands.[3,8,14]
Of the types mentioned in the new classification of WHO in 2013,[7] well-differentiated and myxoid liposarcomas tend to recur locally and rarely metastasize or lead to death. Liposarcomas do not metastasize unless these tumors become dedifferentiated. Transition from ALT or WDL to nonlipogenic sarcoma happens at about 5–15%.[3,15] The risk of this transformation depends on the site of the tumor which is more frequent in deep locations such as retroperitoneum.[12] Dedifferentiated liposarcomas behave more aggressively, with 41% local recurrence, 17% metastasis and 28% of disease-related mortality.[16,17]
Clinical and radiologic findings have limited value for definite diagnosis and histopathologic examination is necessary. The histopathologic appearance of liposarcoma can mimic development of fat tissue, ranging from an ALT to pleomorphic liposarcomas which are sometimes hard to distinguish from other forms of sarcomas. Many authors believe that the existence of lipoblasts are necessary to establish the histopathologic diagnosis of a WDL,[18] while others consider more important features such as the presence of variation in adipocyte size, atypical and enlarged adipocyte nuclei with hyperchromatic and bizarre stromal cells in fibrous septa.[13] Several neoplastic and nonneoplastic conditions such as lipoma with fat necrosis, lipoma with lochkern, atrophy of fat, silicone reaction, diffuse lipomatosis, spindle cell lipoma/pleomorphic lipoma, myolipoma, angiolipoma, lipomatous hemangiopericytoma and solitary fibrous tumor must be differentiated from ALT/WDL.[7] In most of these conditions, appropriate sampling and careful examination for identifying lipoblasts (large cells with a hyperchromatic indented nuclei and lipid rich droplets in the cytoplasm) in an appropriate histologic background, comprise the mainstay of accurate diagnosis.[12]
From the immunohistochemical view which is usually of limited value in adding to the accurate diagnosis, adipocytes and lipoblasts are known to stain positive for vimentin and S100. Overexpression of MDM2 and CDK4 had been shown to be valuable in diagnostic confirmation and differentiating from benign neoplastic and nonneoplastic conditions.[9,17] Cytogenic markers may provide a new criterion where neither morphological features nor immunohistochemical stains lead to a definite diagnosis.[10,19] The point which all authors agree is that the histopathologic appearance of liposarcomas can predict the biologic behavior of the tumor.[18] This case was identified as slow growing mass having multiple episodes of recurrence and multiple misdiagnoses, but upon revisions, sclerosing type of ALT was confirmed. This type is composed of broad and dense fibrous bands containing atypical and bizarre-appearing cells characterized by lipoblasts with hyperchromatic nuclei and areas of lipomatous proliferation. Rarity of the tumor in this location and overlapping of the histopathological features can lead to misdiagnosis. To make a definite diagnosis in these situations, molecular and immunohistochemical studies for identifying MDM2 overexpression/amplification and cytogenetics abnormalities are helpful and recommended. With agreement, complete surgical excision with free margins is considered the most valuable treatment.[2,3,9] The risk of recurrence for this intermediate type of liposarcoma is high. However, the risk of metastasis is low and becomes high when the tumor shows dedifferentiated features.[15] Histologic grade, tumor subtype, location and free surgical margins are considered as most reliable prognostic factors.[20] A <5 cm maximum diameter is also considered a favorable prognostic factor for oral liposarcomas.[3,5,8] Palliative radiotherapy can enhance the survival rate of the patients with all types of nonresectable liposarcomas and also delay or prevent the local recurrence in certain cases; however, its value is still controversial.[4] The role of adjuvant chemotherapy has also not been adequately evaluated.[2]
CONCLUSION
Intraoral liposarcoma is a rare lesion with a generally favorable prognosis based on the histopathologic subtype, location and clear surgical margins. Due to the importance of esthetic considerations in the head and neck area, conservative surgical excision with close and long periods of follow-up is preferable instead of radical surgical approach.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Virchow R. A case of malignant occurring in part in the form of fat neuroma tumors. Virchows Arch Pathol Anat. 1857;11(3):281–8. [Google Scholar]
- 2.Kim YB, Leem DH, Baek JA, Ko SO. Atypical lipomatous tumor/well-differentiated liposarcoma of the gingiva: A case report and review of literature. J Oral Maxillofac Surg. 2014;72:431–9. doi: 10.1016/j.joms.2013.06.222. [DOI] [PubMed] [Google Scholar]
- 3.Piperi E, Tosios KI, Nikitakis NG, Kyriakopoulos VF, Tzerbos F, Koutlas IG, et al. Well-differentiated liposarcoma/atypical lipomatous tumor of the oral cavity: Report of three cases and review of the literature. Head Neck Pathol. 2012;6:354–63. doi: 10.1007/s12105-011-0327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis EC, Ballo MT, Luna MA, Patel SR, Roberts DB, Nong X, et al. Liposarcoma of the head and neck: The University of Texas M. D. Anderson cancer center experience. Head Neck. 2009;31:28–36. doi: 10.1002/hed.20923. [DOI] [PubMed] [Google Scholar]
- 5.Fanburg-Smith JC, Furlong MA, Childers EL. Liposarcoma of the oral and salivary gland region: A clinicopathologic study of 18 cases with emphasis on specific sites, morphologic subtypes, and clinical outcome. Mod Pathol. 2002;15:1020–31. doi: 10.1097/01.MP.0000027625.79334.F5. [DOI] [PubMed] [Google Scholar]
- 6.Gritli S, Khamassi K, Lachkhem A, Touati S, Chorfa A, Ben Makhlouf T, et al. Head and neck liposarcomas: A 32 years experience. Auris Nasus Larynx. 2010;37:347–51. doi: 10.1016/j.anl.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, editors. Pathology and Genetics of Tumours of Soft Tissue and Bone. 4th ed. Lyon: IARC Press; 2013. WHO Classification of Tumours of Soft Tissue and Bone. [Google Scholar]
- 8.Cheng J, Wang Y, Cheng A, Wang L, Tian Z, Yu H, et al. Primary liposarcoma in oral and maxillofacial region. J Craniofac Surg. 2011;22:1765–71. doi: 10.1097/SCS.0b013e31822e626a. [DOI] [PubMed] [Google Scholar]
- 9.Kaczmarczyk D, Jesionek-Kupnicka D, Kubiak M, Morawiec-Sztandera A. Atypical lipomatous tumor of the cheek – A case report. Otolaryngol Pol. 2013;67:218–21. doi: 10.1016/j.otpol.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 10.Allon I, Vered M, Dayan D. Liposarcoma of the tongue: Clinico-pathologic correlations of a possible underdiagnosed entity. Oral Oncol. 2005;41:657–65. doi: 10.1016/j.oraloncology.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Angiero F, Sidoni A, Stefani M. Liposarcoma of the oral cavity – Case reports of the pleomorphic and the dedifferentiated variants and a review of the literature. Anticancer Res. 2006;26:4857–67. [PubMed] [Google Scholar]
- 12.Goldblum JR, Weiss SW, Folpe AL. Enzinger and Weiss's Soft Tissue Tumors. 6th ed. Philadelphia: Saunders Elsevier Health Sciences; 2013. [Google Scholar]
- 13.Nascimento AF, McMenamin ME, Fletcher CD. Liposarcomas/atypical lipomatous tumors of the oral cavity: A clinicopathologic study of 23 cases. Ann Diagn Pathol. 2002;6:83–93. doi: 10.1053/adpa.2002.32375. [DOI] [PubMed] [Google Scholar]
- 14.Nakahara H, Shirasuna K, Terada K. Liposarcoma of the floor of the mouth: A case report. J Oral Maxillofac Surg. 1994;52:1322–4. doi: 10.1016/0278-2391(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 15.Crago AM, Singer S. Clinical and molecular approaches to well differentiated and dedifferentiated liposarcoma. Curr Opin Oncol. 2011;23:373–8. doi: 10.1097/CCO.0b013e32834796e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeWitt J, Heidelman J, Summerlin DJ, Tomich C. Atypical lipomatous tumors of the oral cavity: A report of 2 cases. J Oral Maxillofac Surg. 2008;66:366–9. doi: 10.1016/j.joms.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 17.Aleixo PB, Hartmann AA, Menezes IC, Meurer RT, Oliveira AM. Can MDM2 and CDK4 make the diagnosis of well differentiated/dedifferentiated liposarcoma? An immunohistochemical study on 129 soft tissue tumours. J Clin Pathol. 2009;62:1127–35. doi: 10.1136/jcp.2009.070201. [DOI] [PubMed] [Google Scholar]
- 18.Nikitakis NG, Lopes MA, Pazoki AE, Ord RA, Sauk JJ. MDM2/CDK4/p53 oral liposarcoma: Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:194–201. doi: 10.1067/moe.2001.116815. [DOI] [PubMed] [Google Scholar]
- 19.Sandberg AA. Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors: Lipoma. Cancer Genet Cytogenet. 2004;150:93–115. doi: 10.1016/j.cancergencyto.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 20.Hasanabadi MS, Amiri M, Tajedini A, Yazdi AK, Heidarali M, Amali A, et al. Huge myxoid liposarcoma of the esophagus: A case report. Acta Med Iran. 2011;49:118–21. [PubMed] [Google Scholar]


