Abstract
The delivery of a 25-year-old Jehovah's Witness was complicated by postpartum haemorrhage with a nadir haematocrit of 3%. To improve oxygen delivery without blood transfusion, FiO2 was increased to maximize dissolved oxygen delivery. Central venous oxygen saturation was used to assess tissue oxygenation. When blood products are refused, successful management of severe anaemia is possible with supportive medical care to achieve haemostasis, optimize oxygen delivery and promote haematopoiesis.
Keywords: postpartum haemorrhage, ScvO2, blood product refusal
CASE HISTORY
A 25-year-old primipara dedicated to Jehovah's Witness faith developed preeclampsia at 37 weeks with a haematocrit of 35%. She received magnesium sulphate and delivered a 2555 g infant via vacuum. Her postpartum course was complicated by postpartum haemorrhage due to uterine atony and retained products of conception for which she was treated with operative curettage and uterotonics. Her postoperative haematocrit was 6.2%. She was transferred to the ICU and received vitamin K, iron sucrose and hespan. She became increasingly hypotensive and received norepinephrine, dopamine and albumin. She demonstrated acute neurological changes, was intubated and transferred to our facility.
The patient's record documented a 21-year recognition of Jehovah's Witness practice and an advanced directive executed during pregnancy. Her family confirmed these sentiments. The office of the Attorney General reviewed the directive and concluded its execution while pregnant acted as a surrogate expression of her preferences including her consideration of her pregnancy. Medical providers approached her case respecting her advanced directive.
Initial laboratory values included an elevation of troponin of 5.43 ng/mL (<0.4), ALT of 266 U/L (8–49), AST of 210 U/L (10–44) and serum creatinine of 1.2 mg/dL (0.3–1.2), venous lactate of 10.7 mmol/L (0.5–2.1), platelet count of 156,000/μL (150–400) and HCO3 of 17 mEq/L (22–32). Blood draws were obtained from peripheral and peripherally inserted central catheter (PICC) line access. Her electrocardiogram demonstrated sinus tachycardia with a heart rate of 130 beats per minute. A transthoracic echo obtained on postpartum day 3 revealed normal ventricular size and function without detectable regional wall motion abnormality, normal valve function and a very small, circumferential pericardial effusion.
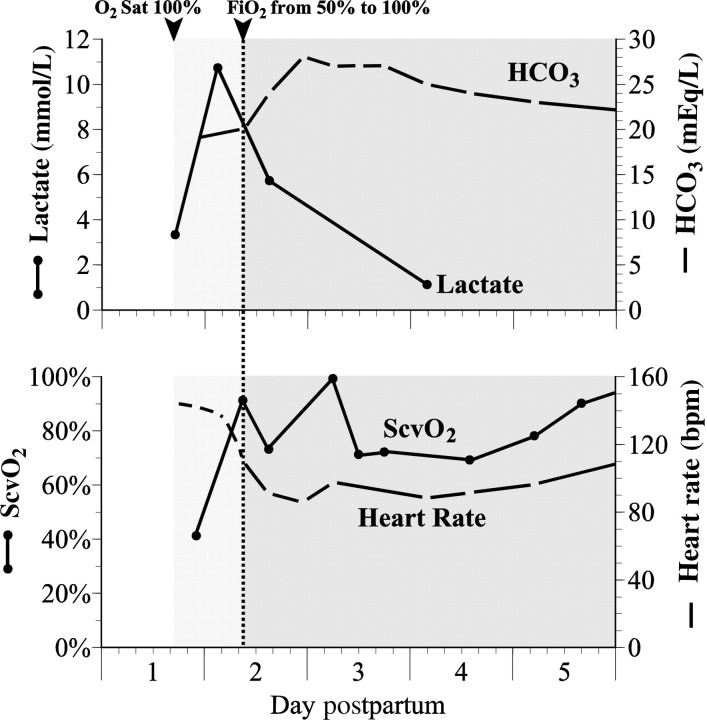
To decrease oxygen consumption, she remained mechanically ventilated with spontaneous assist control and positive end-expiratory pressure of 5 cm H2O. Her FiO2 (fraction of inspired oxygen) was increased from 50% to 100% despite O2 saturations of 100% to optimize oxygen carrying capacity (Figure 1). Tissue oxygenation was assessed with central venous oxygen saturations (ScvO2) obtained via a PICC with the line tip in the superior vena cava just above the cavoatrial junction. At a FiO2 of 100%, ScvO2 improved from 40% to 90%, lactate and HCO3 normalized, each suggesting improved oxygen delivery. Her PaO2 ranged from 126 to 180 at FiO2 of 40%. No measurements were obtained after the FiO2 change. She received antibiotics for ventilator-associated pneumonia. Paralytics were considered but not utilized. She was extubated on postpartum day 16.
Figure 1.
Lactate concentration, HCO3 concentration, central venous oxygen saturation (ScvO2) and heart rate are plotted against time demonstrating improvement in maternal condition after increasing the patient's FiO2 to 100% to increase dissolved oxygen and oxygen delivery
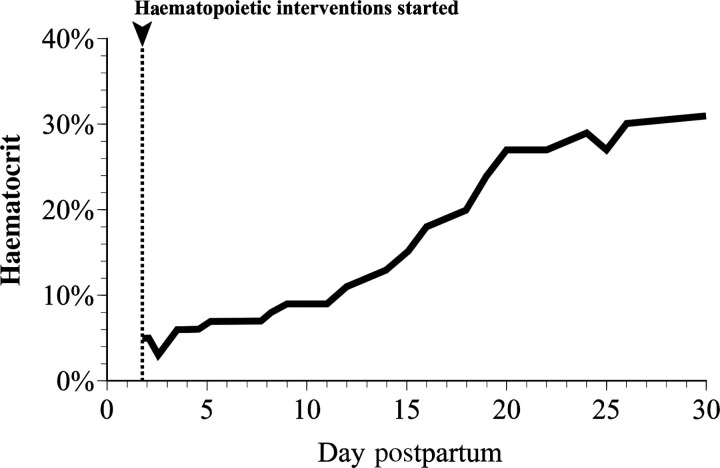
The haematocrit reached a nadir of 3% on postpartum day 4 with an undetectable haemoglobin. Blood draws collected in paediatric tubes were minimized. She received erythropoietin 40,000 units intravenously every other day × five doses, iron sucrose intravenously 100 mg daily × six doses, vitamin B12 0.2 mg intramuscularly × one dose and 1 mg per feeding tube daily × 10 days and folic acid 1 mg per feeding tube orally × 20 days to stimulate haematopoiesis. On postpartum day 5 her reticulocyte count was 20%. Her haematocrit increased at a rate of approximately 1% per day (Figure 2).
Figure 2.
Haematocrit is plotted against time demonstrating a rise in haematocrit of approximately 1% per day with haematopoietic support
After extubation, the patient was oriented and verbal but demonstrated global deconditioning, bilateral lower extremity weakness and right foot clonus. Computed tomography and magnetic resonance imaging revealed left frontal-parietal vasogenic oedema without restricted diffusion to suggest infarct. The findings were attributed to preeclampsia and were consistent with an atypical presentation of posterior reversible leukoencephalopathy syndrome.1 Her strength and coordination rapidly improved with in-hospital physical and occupational therapy. She was discharged on postpartum day 38 with improving short-term memory deficits and ambulating with a cane. Prior to discharge she was lactating and had no evidence of Sheehan's syndrome with normal cortisol and adrenocorticotropin levels.
DISCUSSION
Postpartum patients refusing blood transfusion after haemorrhage represent distinctive medical and ethical challenges for health-care providers. Obstetrical patients who refuse blood products appear to have an increased rate of mortality. In New York City, a cohort of Jehovah's Witness obstetric patients experienced a maternal mortality rate of 512/100,000 relative to 12/100,000 for controls.2 In the Netherlands, Jehovah's Witness patients demonstrated a 130 times increased risk for maternal death associated with major obstetrical haemorrhage.3 The medical management of patients with severe anaemia refusing blood transfusion requires: (1) haemostasis, (2) maximizing oxygen delivery to the tissues, (3) reducing oxygen consumption, (4) promoting haematopoiesis and (5) reviewing advanced directives.4–6 While not an option for this case, the use of cell salvage is acceptable to Jehovah's Witnesses and should be offered when appropriate. Blood substitutes remain in experimental stages and donated blood is of limited supply in some areas, thus these principles may be applied to all severely anaemic patients.
Severe anaemia limits adequate oxygen delivery to tissues and may initiate anaerobic metabolism, lactate production and metabolic acidosis. Total oxygen delivery (DO2) is dependent on cardiac output (Q) and oxygen content (CaO2). CaO2 reflects O2 carried by haemoglobin (1.39[Hb]SaO2) and dissolved O2 (0.003PaO2):
Ninety-eight percent of the oxygen content of blood is bound to haemoglobin and 2% is unbound (dissolved). With adequate haemoglobin, increasing the dissolved component of oxygen does not significantly change the total oxygen content. For example, with a haemoglobin of 15 mg/dL, increasing the PaO2 from 90 to 300 mmHg increases the total content by only 3%. However, in the context of severe anaemia, the relative contribution of dissolved oxygen is significant. With a haematocrit of 3% (haemoglobin of 1.3 mg/dL), the same PaO2 change increases the total oxygen content by 30%.
To maximize the potential for oxygen delivery, we increased the FiO2 from 50% to 100% despite 100% saturation at 50% FiO2. Clinical improvement with this intervention was supported by improvement in labs and vital signs (Figure 1). It is unlikely increases in cardiac output played a major role in her increase in oxygen delivery given she had a 60% decrease in heart rate (rather than increase). PaO2 was not measured after the FiO2 was increased, thus an actual total oxygen content calculation is not available.
Mixed venous oxygen saturation (SvO2) measures the balance between oxygen delivery and oxygen consumption but requires placement of a pulmonary artery catheter. Alternatively, ScvO2 sampling from the SVC is accessible with a PICC and reflects the degree of oxygen extraction from the brain and the upper body.7 ScvO2 >75% represents normal oxygen extraction. While there is good but imperfect correlation between SvO2 and ScvO2, changes of both parameters occur in parallel.7 The advantages and limitations of venous oximetry are well reviewed in the literature.7 As seen in Figure 1, after FiO2 was increased to 100%, ScvO2 improved in concert with improvement in lactate and HCO3 suggesting that the changes in ScvO2 reflect improvement in tissue oxygenation.
Pregnant and postpartum patients refusing blood products provide a unique resuscitative challenge and medical–ethical dilemma. After concluding that the patient had a valid advanced directive, we initiated care to minimize oxygen consumption and improve oxygen delivery. These efforts included: (1) mechanical intubation and sedation to decrease oxygen requirements, (2) maximizing dissolved oxygen delivery with a FiO2 of 100% and (3) an aggressive haematopoiesis regimen that resulted in a 1% haematocrit increase per day. In this case, venous oximetry measurements via a less invasive central line appeared to correlate with clinical improvement after specific interventions to improve oxygenation were employed.
DECLARATIONS
The authors have no conflicts of interest to declare.
REFERENCES
- 1. Servillo G, Striano P, Striano S, et al. Posterior reversible encephalopathy syndrome (PRES) in critically ill obstetric patients. Intensive Care Med 2003;29:2323–6 [DOI] [PubMed] [Google Scholar]
- 2. Singla AK, Lapinski RH, Berkowitz RL, Saphier CJ. Are women who are Jehovah's Witnesses at risk of maternal death? Am J Obstet Gynecol 2001;185:893–5 [DOI] [PubMed] [Google Scholar]
- 3. Van Wolfswinkel M, Zwart J, Schutte J, Duvekot J, Pel M, Van Roosmalen J. Maternal mortality and serious maternal morbidity in Jehovah's witnesses in the Netherlands. BJOG 2009;116:1103–10 [DOI] [PubMed] [Google Scholar]
- 4. Remmers P, Speer A. Clinical strategies in the medical care of Jehovah's Witnesses. Am J Med 2006;119:1013–8 [DOI] [PubMed] [Google Scholar]
- 5. Mannucci P, Levi M. Prevention and treatment of major blood loss. N Engl J Med 2007;356:2301–11 [DOI] [PubMed] [Google Scholar]
- 6. Gyamfi C, Gyamfi M, Berkowitz R. Ethical and medicolegal considerations in the obstetric care of a Jehovah's witness. Obstet Gynecol 2003;102:173–80 [DOI] [PubMed] [Google Scholar]
- 7. Marx G, Reinhart K. Venous oximetry. Curr Opin Crit Care 2006;12:263–8 [DOI] [PubMed] [Google Scholar]