Abstract
Bronchiolitis obliterans organizing pneumonia, now termed as cryptogenic organizing pneumonia (COP), is a fibrotic lung disease of the small airways with the potential to progress to end-stage lung disease. COP in pregnancy carries a high risk of maternal and neonatal complications and only two prior cases have been reported. This is the first case of pre-existing COP in pregnancy. We report a 16-year-old primigravid with COP who elected inpatient management and preterm delivery as a successful management option.
Keywords: cryptogenic organizing pneumonia, pregnancy complications, pregnancy outcome, premature birth
INTRODUCTION
Bronchiolitis obliterans organizing pneumonia, now termed as cryptogenic organizing pneumonia (COP), was first described by Epley and his colleagues in 1985.1 It is a fibrotic lung disease of the small airways which results from damage to the bronchiolar epithelium. The repair process often leads to excessive proliferation of granulation tissue that fills the terminal lumens and respiratory bronchioles. If granulation tissue extends continuously into the alveolar ducts and alveoli it is termed as bronchiolitis obliterans organizing pneumonia.1,2 The original terminology of bronchiolitis obliterans organizing pneumonia has been abandoned because the major process is organizing pneumonia with bronchiolitis obliterans being only a minor and accessory finding that may even be absent.3 COP remains a rare disease in pregnancy with only two prior cases reported in the literature. To our knowledge, we report the first case of pre-existing COP in pregnancy.
CASE REPORT
A 16-year-old primigravid Caucasian female with COP presented at 20 weeks gestation for prenatal care. The patient had a history of chronic respiratory failure secondary to bronchiolitis obliterans organizing pneumonia, severe end-stage lung disease, pulmonary hypertension, asthma and a partial right-lower lower-lobe resection. She had a baseline forced expiratory volume in the first second (FEV1) of 22–35%. Diagnosed at the age of six, her initial diagnostic work-up included bronchoscopy, serum immunglobulins and a sweat chloride test. At the age of 10, a 2D echocardiogram was conducted that showed levocardia, minimally elevated right ventricular systolic pressure of 29–30 mmHg and trace tricuspid insufficiency. At 14 years of age, her pulmonary function tests showed a forced vital capacity (FVC) of 1.55L (65% of predicted), an FEV1 of 0.75 L (35% of predicted), an FEV1/FVC ratio of 48%, a peak expiratory flow (PEF) of 1.71 L/second, a total lung capacity of 4.5 L (145% of predicted), a residual volume of 2.95 L and a functional residual capacity of 3.18 L (212% of predicted). Her tidal flow-volume curve showed severe obstructive lung disease. She was informed that she was a transplant candidate, but was lost to follow-up. Although the gold standard for pathological diagnosis of COP is an open or thoracoscopic lung biopsy,4 we were unable to obtain the histopathological report of the initial bronchoscopy or lower-lobe resection.
Pulmonary function tests at four months gestation revealed very severe obstruction with a suboptimal response to albuterol with pre-bronchodilator values of an FVC of 1.56 L (48% predicted), an FEV1 of 0.51 L (17% predicted) and an FEV1/FVC ratio of 32.72%. The patient was counselled extensively regarding the risks of continued pregnancy with limited pulmonary reserve. Due to the potential for maternal death and poor neonatal outcome, termination of pregnancy was recommended. The patient declined termination, electing to continue with the pregnancy.
At 22 weeks gestation she presented with increased shortness of breath, chest pain, night sweats, fatigue, tachycardia and paroxysmal nocturnal dyspnoea. On admission, her pulmonary function tests revealed an FEV1 of 0.51 L (17% of predicted). She improved following bronchodilator therapy up to 0.65 L, but remained at 27% of predicted lung function. An electrocardiogram showed sinus tachycardia. Her initial chest X-ray showed no acute cardiopulmonary disease. A chest computed tomography (CT) showed patchy ground glass infiltrates and a transthoracic echocardiography showed minimal evidence of pulmonary hypertension with a right ventricular systolic pressure of 30 mmHg. She was admitted to the antepartum unit for continuous hospitalized observation, oxygen therapy and intensive maternal and fetal surveillance.
A multidisciplinary team including pulmonology, neonatology, obstetrics and maternal fetal medicine met to determine optimal management and treatment. Inpatient management included steroid and beta-agonist nebulizers, daily respiratory treatments using a hand-held nebulizer of a beta-2 agonist and corticosteroids, daily pulmonary function tests and weekly arterial blood gases (ABG). The patient also received beta-methasone at 24 weeks and began having daily non-stress tests and twice weekly biophysical assessments at this time. The optimal date of delivery remained open for discussion; however, due to the severity of the patient condition, a tentative plan was established to deliver at 28 weeks or earlier for maternal or fetal decompensation.
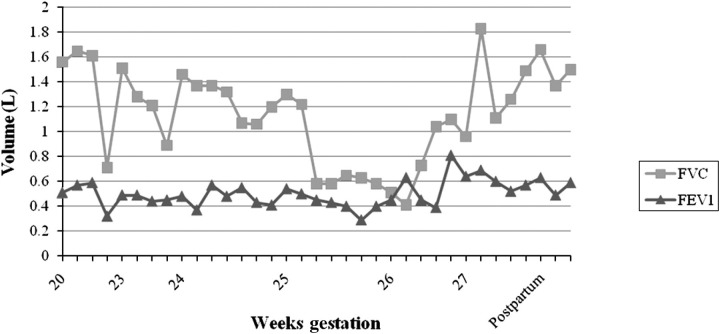
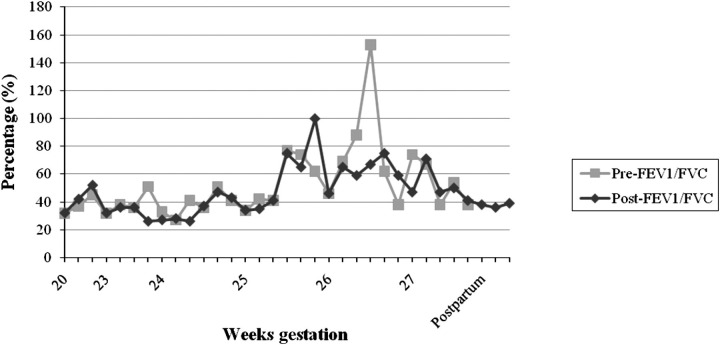
Throughout the inpatient stay, the patient required 2–4 L of continuous oxygen by nasal cannula to maintain an oxygen saturation of 94–100%. Daily pulmonary function tests showed an FVC of 0.41–1.83 L, an FEV1 of 0.29–0.81 L and a PEF of 29–71 L/minute (Figure 1). Weekly ABG levels showed pH values of 7.39–7.43, pCO2 of 38–47 mmHg, pO2 of 50–129 mmHg and HCO3 of 24.6–29.9 mmol/L. Weekly twice sonographic assessments confirmed fetal wellbeing throughout the pregnancy with no evidence of compromise. As shown in Figure 2, the patient experienced no further pulmonary deterioration during the inpatient stay; therefore, maternal fetal medicine, obstetrics and pulmonology agreed that advancing delivery until 30–32 weeks with continued expectant management was reasonable.
Figure 1.
Pulmonary function tests prior to bronchodilator treatment. FVC, forced vital capacity; FEV1, forced expiratory volume in the first second
Figure 2.
Pulmonary function tests pre- and postbronchodilator treatment. FVC, forced vital capacity; FEV1, forced expiratory volume in the first second
At 27+6 weeks gestation a multidisciplinary meeting was held and the risks and benefits of continued conservative management versus delivery were discussed. Despite the recommendation for continued expectant management, the patient elected to proceed with caesarean delivery. The patient also desired permanent sterilization given the severity of her current illness and a court order was obtained to allow a tubal ligation despite the patient's age of 16.
At 28 weeks of gestation, the patient was scheduled for a caesarean section. Prior to transfer to the operating room, she received a nebulizer of beta-agonist and corticosteroid. Neuraxial anaesthesia with supportive ventilation was used during the perioperative period in order to reduce the risk of postoperative mechanical ventilation. Full ventilatory support was available, should her respiratory status deteriorate.
A viable female infant weighing 2 pounds 12 ounces (1.25 kg) with Apgar scores of 8 and 9 at 1 and 5 minutes, respectively, was delivered by caesarean section, followed by bilateral tubal ligation. The surgery was uncomplicated with haemodynamic stability and no respiratory compromise. Physical examination of the infant revealed respiratory distress requiring intubation to provide one dose of surfactant. The infant was immediately extubated to high flow-nasal cannula and transferred to the neonatal intensive care unit (NICU). Cord blood gas showed a pH of 7.32, pCO2 of 48 mmHg, pO2 of 31 mmHg, HCO3 of 24.9 mmol/L, a base excess of −1 mmol/L and an O2 sat of 54%. She was weaned to room air by day 13. The NICU course was complicated by feeding issues that were resolved prior to discharge. The infant was developing normally and was discharged at an adjusted gestational age of 36+4 weeks.
The patient was transferred to the postoperative anaesthesia care unit (PACU) on 2 L of oxygen which was increased to 4 L due to dyspnoea and tachypnoea. Once stable, she was transferred to the postpartum unit on 4 L of oxygen by nasal cannula with an O2 saturation of 98%. Oxygen was reduced to 2 L by nasal cannula over a two-day period and postpartum pulmonary function tests showed an FVC range of 1.37–1.50 L and an FEV1 of 0.49–0.59 L. The patient had an uneventful postpartum stay and had returned to her baseline by day three postpartum. The patient was discharged home on day three on beta-agonist inhalation therapy, corticosteroids and supplemental oxygen. The severity of the patient's pulmonary status and potential for future lung transplantation were stressed prior to discharge and outpatient follow-up with obstetrics and pulmonology were scheduled for two weeks postpartum. Unfortunately, the patient has again been lost to follow-up.
COMMENT
Pregnancy alters lung function causing physiological changes such as increased minute volume, compensated respiratory alkalosis and a reduction in expiratory reserve volume. Vital capacity and forced expiratory reserve volume are preserved.5–7 Pulmonary disorders during pregnancy carry a high risk of maternal and neonatal complications. Respiratory disease in pregnancy has been associated with an increased risk of maternal and neonatal mortality, preterm delivery, small for gestational age and intrauterine growth retardation, hypertensive disorders of pregnancy, increased risk of obstetrical complications and caesarean section.5–7
The primary objective of this case was to avoid termination of pregnancy prior to the age of viability while optimizing maternal and neonatal outcomes in a patient with pre-existing COP. A MEDLINE search for articles published between 1985 and 2010 was conducted using MeSH terms and keywords ‘bronchiolitis obliterans’, ‘bronchiolitis obliterans organizing pneumonia’, ‘cryptogenic organizing pneumonia’, ‘respiratory insufficiency’ and ‘pregnancy’. Only two prior cases of COP in pregnancy were identified in the literature. Gestational age at presentation included 38 weeks with complicating diagnoses of idiopathic thrombocytopenia and asthma8 and 26.5 weeks with a complicating diagnosis of HIV.9 Diagnosis of the first case of bronchiolitis obliterans organizing pneumonia in pregnancy was made during the postpartum period following a bronchoalveolar lavage, transbronchial lung biopsy and CT.8 In the second case, the diagnosis of bronchiolitis obliterans organizing pneumonia was made at 29 weeks gestation following a bronchoscopy and open-lung biopsy.9 The initial differential diagnosis in each case was of infectious aetiology and therefore initial treatment included antibiotics. Symptomatic treatment included bronchodilators, corticosteroids and oxygen therapy. No pulmonary function parameters were reported in either case. One patient had an emergent delivery at 38 weeks due to severe respiratory distress, significant leukocytosis and fetal tachycardia,8 whereas the second patient delivered at 34 weeks due to premature rupture of membranes.9 Both delivered viable infants via caesarean section.
At 28 weeks gestation our patient elected preterm delivery rather than continued antenatal management in order to avoid the potential for further respiratory compromise. Assessment of the two prior case reports of COP in pregnancy may give the impression that delivery is possible at an advanced gestational age. Neither case reported pulmonary function tests documenting the severity of patient respiratory compromise.
Prior reports in patients with pulmonary disease due to cystic fibrosis have suggested that an FEV1 of >70% is required for successful pregnancy outcome, and give further recommendations for termination if the FEV1 is <50%.10 Our patient continued to have severe pulmonary insufficiency with an FEV1 as low as 17% giving evidence to the possibility of a successful pregnancy. However, contrary to the current literature, she did not experience a reduction in FEV1/FVC, FEV1 or FVC. In retrospect, continued close antepartum care and careful management of respiratory function may have allowed delivery to be delayed. In addition, increased patient education regarding the severity of her condition may have helped to ensure adequate postpartum follow-up.
Further studies are needed to determine the effects of pregnancy on the progression of pulmonary disorders such as COP. Efforts are needed to determine the minimum parameters of pulmonary function that predict satisfactory maternal and neonatal outcomes. Research is also needed to further assess the risks and benefits of advancing gestation, the timing and route of delivery and the type of anaesthesia in such cases. We suggest that efforts be made to objectively assess the risks and benefits of continued gestation, with consideration of preterm delivery as a viable management option in patients with pulmonary disorders who desire to avoid termination of the pregnancy.
CONCLUSION
Management of COP in pregnancy requires aggressive treatment from a multidisciplinary team including maternal-fetal medicine, obstetrics, neonatology, pulmonology and respiratory therapy and anaesthesia specialists. Our patient had minimal pulmonary reserve throughout pregnancy, but with close inpatient management she experienced no further respiratory compromise. This case provides relevant information to the literature given the limited published research on the management of COP in pregnancy; however, it remains difficult to determine whether pregnancy alters the clinical progression of COP given our patient's elected preterm delivery at 28 weeks gestation and limited pulmonary decline. In summary, this case report reviews the first case of pre-existing COP in pregnancy and illustrates the complex decision-making process with regard to its management, the importance of a multidisciplinary approach to patient care and the role of elective preterm delivery in respiratory insufficiency.
REFERENCES
- 1. Epler GR. Bronchiolitis obliterans organizing pneumonia. Arch Inter Med 2001;161:158–64 [DOI] [PubMed] [Google Scholar]
- 2. Epler GR, Colby TV, McLoud TC, Carrington CB, Gaensler EA. Bronchiolitis obliterans organizing pneumonia. N Eng J Med. 1985;312:152–8 [DOI] [PubMed] [Google Scholar]
- 3. Cordier JF. Cryptogenic organizing pneumonia. Eur Respir J 2006; 28:422 [DOI] [PubMed] [Google Scholar]
- 4. Lamont J, Verbeken E, Verschakelen J, Demedts M. Bronchiolitis obliterans organising pneumonia. A report of 11 cases and a review of the literature. Acta Clin Belg 1998;53:328–36 [DOI] [PubMed] [Google Scholar]
- 5. Bhatia P, Bhatia K. Pregnancy and the lungs. Postgrad Med J 2000;76: 683–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cohen R, Talwar A, Efferen L. Exacerbation of underlying pulmonary disease in pregnancy. Crit Care Clin 2004;20:713–30 [DOI] [PubMed] [Google Scholar]
- 7. Wise R, Polito A, Krishnan V. Respiratory physiologic changes in pregnancy. Immunol Allergy Clin North Am 2006;26:1–12 [DOI] [PubMed] [Google Scholar]
- 8. Futagami M, Sakamoto T, Sakamoto A, et al. Bronchiolitis obliterans organizing pneumonia in pregnancy. J Obstet Gynecol 2003;23:309 [DOI] [PubMed] [Google Scholar]
- 9. Ghidini A, Mariani E, Patregnani C, Marinetti E. Bronchiolitis obliterans organizing pneumonia in pregnancy. Obstet Gynecol 1999;94:843 [DOI] [PubMed] [Google Scholar]
- 10. Canny GJ, Corey M, Livingstone RA, et al. Pregnancy and cystic fibrosis. Obstet Gynecol 1991;77:850–85 [PubMed] [Google Scholar]