Abstract
Background and Aims:
A decision-to-delivery interval (DDI) of 30 min for category-one caesarean section (CS) deliveries is the standard of practice recommended by clinical guidelines. Our institution established a protocol for category-one (‘crash’) CS to expedite deliveries. The aim of this study is to evaluate DDI, factors that affect DDI and the mode of anaesthesia for category-one CS.
Methods:
This retrospective cohort study evaluated 390 women who underwent category-one CS in a tertiary obstetric centre. We analysed the factors associated with DDI, mode of anaesthesia and perinatal outcomes. Summary statistics were performed for the outcomes. The association factors were considered significant at P < 0.05.
Results:
The mean (standard deviation) DDI was 9.4 (3.2) min with all deliveries achieved within 30 min. The longest factor in the DDI was time taken to transfer patients. A shorter DDI was not significantly associated with improved perinatal outcomes. The majority (88.9%) of women had general anaesthesia (GA) for category-one CS. Of those who had an epidural catheter already in situ (34.4%), 25.6% had successful epidural extension. GA was associated with shorter DDI, but worse perinatal outcomes than regional anaesthesia (RA).
Conclusions:
Our ‘crash’ CS protocol achieved 100% of deliveries within 30 min. The majority (88.9%) of the patients had GA for category-one CS. GA was found to be associated with shorter anaesthesia and operation times, but poorer perinatal outcomes compared to RA.
Key words: Caesarean section, emergencies, general anaesthesia, local anaesthesia
INTRODUCTION
The incidence of caesarean section (CS) deliveries has been rising rapidly in many countries. In England, the CS rate has increased from 12% in 1990 to 25.5% in 2013.[1] In the US, the CS rate has reached 32.8% in 2013.[2] The urgency of CS is classified based on a four-grade system developed by Lucas et al. Category-one CS is defined when there is ‘immediate threat to the life of woman or foetus’ and delivery must be undertaken as quickly as possible after the decision.[3] In the UK, 10% of all CS performed have been classified as category-one.[4] Category-one CS has been associated with 15-times higher risk of maternal death compared to the less urgent category – three CS deliveries.[5]
A decision-to-delivery interval (DDI) of 30 min for category-one CS deliveries has been recommended as a standard of practice by several guidelines.[6] The DDI may also be used as an audit standard to measure the performance of an obstetric unit.[7]
In 1997, our institution established a protocol to expedite ‘crash’ (category-one) CS. A prospective audit carried out in 1999 found a mean DDI of 14.9 min.[8] Using public announcement system and dedicated category-one CS operating theatre (OT), the mean DDI was 7.7 min in a subsequent 1-year prospective audit conducted in 2004.[9] We conducted this retrospective cohort study to evaluate DDI, factors that affect DDI and the mode of anaesthesia for category-one CS.
METHODS
This study was reviewed and approved by Institutional Review Board (SingHealth Centralised Institutional Review Board CIRB reference: 2013/1043/D) and was conducted in a tertiary obstetric centre, with approximately 11,000 deliveries per year. A ‘crash’ CS protocol has been followed at our centre since 1997, where a public announcement system is used to activate a dedicated multidisciplinary team once a decision for ‘crash’ CS is made. The team consists of 24-h on-site obstetric, anaesthetic and neonatology teams supported by the OT staff. A dedicated OT is reserved for ‘crash’ CS located within 50 metres of the labour ward.
Women who delivered via category-one CS in our hospital between April 2010 and December 2013 with ‘crash’ CS were identified. The patient transfer time, the time taken to institute anaesthesia and to perform CS were assessed. Perinatal outcomes were compared between category-one CS deliveries within 10 min of decision and those with DDI more than 10 min. The incidence of the use of each type of anaesthesia for category-one CS and impact on the DDI and perinatal outcomes were investigated.
Relevant data were collected from the medical records. Characteristics assessed/noted were: Maternal - age (year), body mass index (BMI) (kg/m2), gravidity (week), parity (week), gestational age (week); neonatal - birth weight (g), Apgar score at 5 min, arterial cord pH, resuscitation via bag and mask (%), resuscitation via intubation (%), transfer time, anaesthesia time, operation time, DDI, indication(s) for category-one CS and mode of anaesthesia.
Transfer time was defined as the time taken from decision for category-1 CS to arrival in the OT. Anaesthesia time was the time from arrival in OT and immediate start of anaesthesia to skin incision. Operation time was the time from skin incision to the delivery of the foetus. DDI was the time from the decision for category-one CS to the time the foetus was delivered.
Data were summarised with continuous variables summarised using mean [standard deviation (SD)] and median [interquartile range (IQR)], while categorical variables were summarised using frequency (proportion). Comparisons between groups were based on pair-wise comparisons. Two sample t-test and Kruskal–Wallis test were used to compare continuous outcomes between groups. The associated factors were considered significant if P < 0.05. Differences in means or medians with corresponding 95% confidence intervals (95% CIs) were used to quantify the association between the groups and continuous outcomes. Categorical outcomes were compared between groups using Fisher's exact test. Odds ratios (95% CI) were used to quantify the respective associations. We analysed the subgroups of women categorised by the mean duration of DDI identified. The statistical tests were performed using the SAS version 9.2 software (SAS Institute, Cary, North Carolina, USA).
RESULTS
There were 390 cases of ‘crash’ CS between April 2010 and December 2013. Four medical records did not record the decision-to-delivery time. The maternal and neonatal demographic characteristics are shown in Table 1. Slightly more than half (58.9%) of all neonates born by ‘crash’ CS had a cord arterial pH ≤ 7.2.
Table 1.
Maternal and neonatal demographic characteristics (n=390)
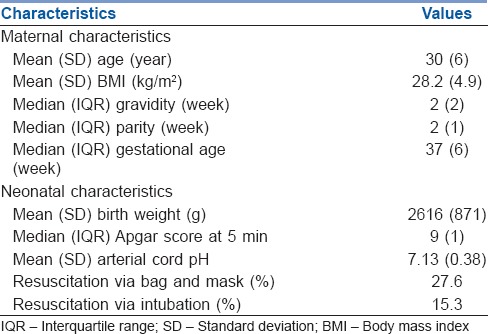
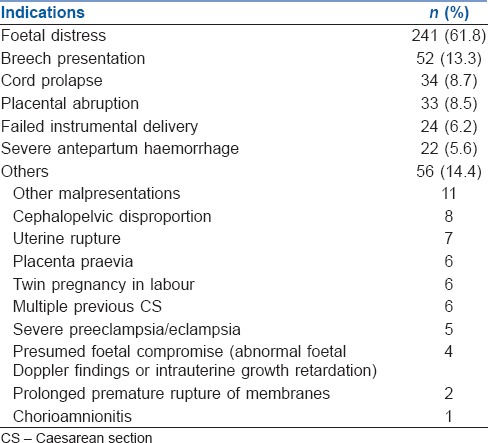
Table 2 shows the most common indications for category-one CS such as foetal distress, breech presentation, cord prolapse, placental abruption, failed instrumental delivery and severe antepartum haemorrhage. Other indications are also included in Table 2. Sixty-three patients had more than one indication.
Table 2.
Indications for category-1 caesarean sections (n=390)
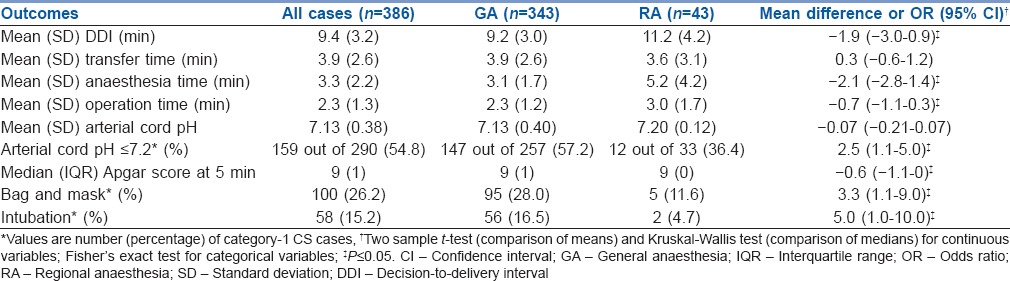
All the category-one CS were commenced within 30 min, with a mean (SD) DDI of 9.4 (3.2) min. Of these cases, 61.5% were achieved within 10 min, 37.3% within 20 min and 1.2% (4 cases) taking more than 20 min. The mean transfer, anaesthesia and operation time are shown in Table 3. The indications for the four cases with DDI > 20 min were foetal distress (2), breech presentation (1) and failed instrumental delivery (1). None of these cases needed neonatal resuscitation with bag and mask ventilation or intubation. Of all the category-one CS, 218 (63.6%) were performed out-of-hours (office hours as defined by timing between 0830 h and 1630 h with daytime coverage of emergency OT). Out-of-hour cases were associated with a longer mean (95% CI) DDI by 1.0 min (0.3 to 1.7, P = 0.004) and a longer mean (95% CI) operation time by 0.3 min (0.04 to 0.62, P = 0.024). There was no significant difference in the transfer time, the anaesthesia time or neonatal outcomes between category-one CS performed within and after office hours.
Table 3.
Comparison of response times and perinatal outcomes between category-1 caesarean section performed under general anaesthesia versus regional anaesthesia
Based on the mean DDI of 9.4 min, we analysed the category-one CS with DDI ≥ 10 min (132) compared to those with DDI < 10 min (211). There were no significant differences in the perinatal outcomes between the two groups. Cases with DDI ≥ 10 min had a mean (95% CI) transfer time of 2.4 min (1.9 to 2.9, P ≤ 0.001) longer, a mean (95% CI) anaesthesia time of 1.5 min (1.1 to 1.9, P ≤ 0.001) longer and a mean (95% CI) operation time of 1.2 min (0.9 to 1.4, P ≤ 0.001) longer than the DDI <10 min group.
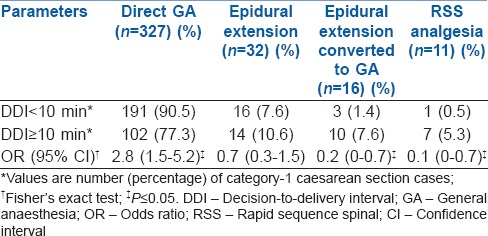
The majority (343, 88.9%) of the ‘crash’ CS were performed under general anaesthesia (GA). Rapid sequence spinal (RSS) anaesthesia was used in only 11 cases (2.8%). Of the women who arrived in the OT with epidural catheters in situ (133, 34.4%), extension of epidural analgesia was attempted in 48 (36.1%) of them, successful in 34 (25.6%). Conversion to GA was performed in the 16 cases of failed epidural extension. Women who had GA were more likely to have a DDI of <10 min; whereas those who had RSS or failed epidural extension were more likely to have DDI ≥ 10 min [Table 4]. Overall, GA was associated with a shorter mean DDI by 1.9 min, when compared to regional anaesthesia (RA) (RSS and epidural extension). Further comparisons revealed shorter anaesthesia and operation time, but worse perinatal outcomes in category-1 CS performed under GA [Table 3]. Women who had GA also had a lower mean (95% CI) BMI by 1.7 kg/m2 (0.0 to 3.3, P = 0.046) and a lower median (95% CI) gestational age by 2.2 weeks (0.5 to 3.9, P = 0.050).
Table 4.
Decision-to-delivery interval of category-1 caesarean section performed under each mode of anaesthesia (n=386)
Cord prolapse and placental abruption were found to be associated with significantly worse perinatal outcomes, with the former associated with a lower mean (95% CI) arterial cord pH by 0.24 (0.10 to 0.49, P ≤ 0.001) and the latter associated with a lower median (95% CI) Apgar score at 5 min by 1.3 (0.7 to 2.0, P ≤ 0.001), a 2.8 (95% CI of 1.3 to 5.8, P = 0.005) times higher risk of needing bag and mask resuscitation and a 2.9 (95% CI of 1.3 to 6.4, P = 0.008) times higher risk of needing neonatal intubation.
DISCUSSION
This retrospective cohort study showed a mean (SD) DDI of 9.4 (3.2) min and all cases were able to achieve delivery within 30 min. With previous studies suggesting difficulty in achieving the 30-min standard,[4,10,11] our hospital's ‘crash’ CS protocol is highly effective and is sustainable.
The 30-min standard for category-one CS is based on expert opinion, with most studies finding no correlation between DDI and maternal morbidity.[12,13,14] Several studies showed the improvement of perinatal outcomes with shortened DDI[14] while others showed worse outcomes with faster DDI.[6,11,15] More recent studies did not show correlation of perinatal outcomes with DDI.[10,12,14,16] A recent meta-analysis on DDI for category-one CS found no correlation between DDI and adverse perinatal outcomes.[17]
Patient transfer was the main time limiting factor to deliver the foetus. In addition, we found that ‘crash’ CS performed out-of-hours were associated with longer DDI, in contrast to the study in 2004 by Lim et al., which found no such association.[9] The longer out-of-hours mean DDI may not be clinically relevant given the small difference. Our finding of a mean DDI of 9 min could be due to different data collection methods and retrospective data analysis.
This study did not show significantly better perinatal outcomes in category-one CS cases with shorter DDI (i.e., DDI < 10 min). This finding is in agreement with several studies that found no evidence that faster deliveries may improve perinatal outcomes.[10,12,14,16] The reason for this is two-fold. First, time has the most value in the most urgent cases. Being a category-one CS case does not necessarily equate to the highest degree of urgency.[18] For example, having a breech presentation in active labour might not be imminent threat to the life of the foetus, provided that there is no concomitant cord prolapse. On the other hand, ‘true’ category-one emergencies will benefit more from a speedy delivery. In a retrospective study on women presenting with clinically overt placental abruption, neonates delivered within 20 min were shown to have substantially reduced morbidity and mortality compared to those delivered between 20 and 30 min.[19]
Second, the DDI might not be an accurate measure of the duration of foetal compromise. If the foetus has been compromised for a long duration before the decision for category-one CS is made, the perinatal outcomes will be poor even with a very short DDI. In a retrospective study on urgent caesarean delivery for foetal bradycardia, Leung et al. showed that in the group with an irreversible underlying cause of foetal distress, the arterial cord pH decreased with bradycardia-to-delivery interval, but not DDI, at a rate of 0.011 per min.[20] Bradycardia-to-delivery times correlate better with perinatal outcomes than DDI as this is a more accurate reflection of the duration of foetal compromise. The use of RA or GA in foetal distress in obstetrics may be dependent on hospital and clinical situation.[21] Therefore, to better appreciate the real effect of an expedited delivery on perinatal outcomes, future studies should focus on the most urgent cases (e.g., overt placental abruption and cord prolapse with cord compression) and employ a more accurate measure of the duration of foetal compromise (e.g., bradycardia-to-delivery interval).
We were not able to conduct a comparison with pre-protocol period as the data were not available. In a study conducted by Weiner et al., DDI and neonatal outcomes were compared before (−27 months) and after (+27 months) the implementation of a departmental programme designed to shorten the DDI for emergency CS for non-reassuring foetal heart rate.[13] After the programme implementation, the mean (SD) DDI decreased from 21.7 (9.1) min to 12.3 (3.8) min (P < 0.001), associated with significant reductions in the rates of cord pH ≤ 7.1 and 5 min Apgar score ≤7 (P = 0.016 and P = 0.031, respectively).[13]
GA using rapid sequence induction and cricoid pressure has been the ‘gold standard’ due to the rapidity of achieving surgical anaesthesia. Regional anaesthetic techniques using RSS and extension of existing epidural anaesthesia have also been suggested. GA has been reported to be faster than RSS,[22,23,24] but GA is associated with an increased risk of difficult intubation.[25] GA could also lead to an increase in maternal blood loss[26] and possibly worse the neonatal outcomes.[27] RA should be considered whenever time and situation may allow.[4,17] The majority of category-one CS in our institution were performed under GA in the previous audit.[9]
However, we found that women who had GA after failed epidural extension had significantly longer DDI than those with successful extension of epidural block. We also found that GA was associated with a shorter DDI, but a lower median Apgar score at 5 min, a higher percentage of neonates with arterial cord pH ≤ 7.2 and a higher risk for neonatal resuscitation using bag and mask or intubation compared to RA. Our findings are similar to that of an observational study, which showed that GA led to an increased risk of Apgar score <7 and for neonatal resuscitation at birth.[27] Patients who had GA were associated with a lower BMI and gestational age. Patients with higher BMI may have higher risk of difficult airway, hence higher chance of receiving RA instead. Preterm pregnancies could be more complicated and urgent, necessitating the use of GA to achieve timely deliveries. Ultimately, the choice regarding the type of anaesthesia for category-one CS should be individualised, being a considered balance between achieving a rapid delivery and minimising potential anaesthetic complications.
There are limitations in this study: minor incomplete documentation in the medical records (e.g., absence of ‘crash’ CS activation time and missing cord blood gas results) could have also contributed to reporting bias; we used Apgar score at 5 min and arterial cord pH as measures of perinatal outcomes instead of more sensitive indicators (neonatal intensive care unit stay and presence of complications such as encephalopathy) as these were not available in the database. The decision-making process of type of anaesthesia by the anaesthetists was also not recorded in the database.
CONCLUSION
We were able to achieve the international standard DDI of 30 min in all category-1 CS deliveries. Patient transfer was the main contributing factor for DDI. A shorter DDI was not significantly associated with better perinatal outcomes. The majority (88.9%) of the patients had GA for category-1 CS. Among the parturients who arrived in the OT with epidural catheters in situ, 25.6% of them had successful extension of the epidural block. Compared to regional anaesthetic techniques, GA was found to be associated with shorter anaesthesia and operation times, but poorer perinatal outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hospital Episode Statistics: NHS Maternity Statistics, England 2012-13. 2013 Published by Health and Social Care Information Centre. [Google Scholar]
- 2.Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Mathews TJ. Births: Final Data for 2013. National Vital Statistics Reports. 2015;64:1–65. [PubMed] [Google Scholar]
- 3.Lucas DN, Yentis SM, Kinsella SM, Holdcroft A, May AE, Wee M, et al. Urgency of caesarean section: A new classification. J R Soc Med. 2000;93:346–50. doi: 10.1177/014107680009300703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinsella SM, Walton B, Sashidharan R, Draycott T. Category-1 caesarean section: A survey of anaesthetic and peri-operative management in the UK. Anaesthesia. 2010;65:362–8. doi: 10.1111/j.1365-2044.2010.06265.x. [DOI] [PubMed] [Google Scholar]
- 5.Lewis G, Drife J. The Fifth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. London: Royal College of Obstetricians and Gynaecologists Press; 2001. Why Mothers Die 1997-1999. [Google Scholar]
- 6.Hillemanns P, Strauss A, Hasbargen U, Schulze A, Genzel-Boroviczeny O, Weninger E, et al. Crash emergency cesarean section: Decision-to-delivery interval under 30 min and its effect on Apgar and umbilical artery pH. Arch Gynecol Obstet. 2005;273:161–5. doi: 10.1007/s00404-005-0045-7. [DOI] [PubMed] [Google Scholar]
- 7.Soltanifar S, Russell R. The National Institute for Health and Clinical Excellence (NICE) guidelines for caesarean section, 2011 update: Implications for the anaesthetist. Int J Obstet Anesth. 2012;21:264–72. doi: 10.1016/j.ijoa.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Yeap ML, Tan KH, Tee CS. Book of Abstracts of XVI FIGO World Congress of Gynecology and Obstetrics. Washington, D.C.: USA; 2000. Emergency Caesarean Section: An Analysis of Maternal and Fetal Outcome. [Google Scholar]
- 9.Lim Y, Shah MK, Tan HM. Evaluation of surgical and anaesthesia response times for crash caesarean sections – An audit of a Singapore hospital. Ann Acad Med Singapore. 2005;34:606–10. [PubMed] [Google Scholar]
- 10.Chauhan SP, Roach H, Naef RW, 2nd, Magann EF, Morrison JC, Martin JN., Jr Cesarean section for suspected fetal distress. Does the decision-incision time make a difference? J Reprod Med. 1997;42:347–52. [PubMed] [Google Scholar]
- 11.MacKenzie IZ, Cooke I. What is a reasonable time from decision-to-delivery by caesarean section? Evidence from 415 deliveries. BJOG. 2002;109:498–504. doi: 10.1111/j.1471-0528.2002.01323.x. [DOI] [PubMed] [Google Scholar]
- 12.Nasrallah FK, Harirah HM, Vadhera R, Jain V, Franklin LT, Hankins GD. The 30-minute decision-to-incision interval for emergency cesarean delivery: Fact or fiction? Am J Perinatol. 2004;21:63–8. doi: 10.1055/s-2004-820513. [DOI] [PubMed] [Google Scholar]
- 13.Weiner E, Bar J, Fainstein N, Ben-Haroush A, Sadan O, Golan A, et al. The effect of a program to shorten the decision-to-delivery interval for emergent cesarean section on maternal and neonatal outcome. Am J Obstet Gynecol. 2014;210:224e.1–6. doi: 10.1016/j.ajog.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Gabbay-Benziv R, Ashwal E, Lahav-Ezra H, Rabinerson D, Wiznitzer A, Ben-Haroush A, et al. Decision-to-delivery interval in suspected placental abruption-association with pregnancy outcome. J Matern Fetal Neonatal Med. 2014;27:1680–3. doi: 10.3109/14767058.2013.871703. [DOI] [PubMed] [Google Scholar]
- 15.Roemer VM, Heger-Römermann G. What factors modify the condition of the newborn infant in emergency cesarean section? Z Geburtshilfe Perinatol. 1992;196:141–51. [PubMed] [Google Scholar]
- 16.Roy KK, Baruah J, Kumar S, Deorari AK, Sharma JB, Karmakar D. Cesarean section for suspected fetal distress, continuous fetal heart monitoring and decision to delivery time. Indian J Pediatr. 2008;75:1249–52. doi: 10.1007/s12098-008-0245-9. [DOI] [PubMed] [Google Scholar]
- 17.Tolcher MC, Johnson RL, El-Nashar SA, West CP. Decision-to-incision time and neonatal outcomes: A systematic review and meta-analysis. Obstet Gynecol. 2014;123:536–48. doi: 10.1097/AOG.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 18.Levy DM. Emergency Caesarean section: Best practice. Anaesthesia. 2006;61:786–91. doi: 10.1111/j.1365-2044.2006.04711.x. [DOI] [PubMed] [Google Scholar]
- 19.Kayani SI, Walkinshaw SA, Preston C. Pregnancy outcome in severe placental abruption. BJOG. 2003;110:679–83. [PubMed] [Google Scholar]
- 20.Leung TY, Chung PW, Rogers MS, Sahota DS, Lao TT, Hung Chung TK. Urgent cesarean delivery for fetal bradycardia. Obstet Gynecol. 2009;114:1023–8. doi: 10.1097/AOG.0b013e3181bc6e15. [DOI] [PubMed] [Google Scholar]
- 21.Jadon A. Complications of regional and general anaesthesia in obstetric practice. Indian J Anaesth. 2010;54:415–20. doi: 10.4103/0019-5049.71039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kathirgamanathan A, Douglas MJ, Tyler J, Saran S, Gunka V, Preston R, et al. Speed of spinal vs general anaesthesia for category-1 caesarean section: A simulation and clinical observation-based study. Anaesthesia. 2013;68:753–9. doi: 10.1111/anae.12290. [DOI] [PubMed] [Google Scholar]
- 23.Popham P, Buettner A, Mendola M. Anaesthesia for emergency caesarean section, 2000-2004, at the Royal Women's Hospital, Melbourne. Anaesth Intensive Care. 2007;35:74–9. doi: 10.1177/0310057X0703500110. [DOI] [PubMed] [Google Scholar]
- 24.Beckmann M, Calderbank S. Mode of anaesthetic for category 1 caesarean sections and neonatal outcomes. Aust N Z J Obstet Gynaecol. 2012;52:316–20. doi: 10.1111/j.1479-828X.2012.01457.x. [DOI] [PubMed] [Google Scholar]
- 25.McDonnell NJ, Paech MJ, Clavisi OM, Scott KL ANZCA Trials Group. Difficult and failed intubation in obstetric anaesthesia: An observational study of airway management and complications associated with general anaesthesia for caesarean section. Int J Obstet Anesth. 2008;17:292–7. doi: 10.1016/j.ijoa.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 26.Lertakyamanee J, Chinachoti T, Tritrakarn T, Muangkasem J, Somboonnanonda A, Kolatat T. Comparison of general and regional anesthesia for cesarean section: Success rate, blood loss and satisfaction from a randomized trial. J Med Assoc Thai. 1999;82:672–80. [PubMed] [Google Scholar]
- 27.Ong BY, Cohen MM, Palahniuk RJ. Anesthesia for cesarean section – Effects on neonates. Anesth Analg. 1989;68:270–5. [PubMed] [Google Scholar]


