Abstract
Background and Aims:
Intra-operative identification and preservation of extraocular motor nerves is one of the main goals of surgeries for skull base tumours and this is done by monitoring the extraocular movement (EOM). Intra-operative electromyographic monitoring has been reported, but it is a complex and skilful process. Electrooculography (EOG) is a simple and reliable technique for monitoring EOMs. We aimed to assess the utility of EOG monitoring in preventing extraocular motor nerve dysfunction during skull base surgeries.
Methods:
In this retrospective cohort study, intra-operative EOG recordings were obtained using disposable needle electrodes placed on the periorbital skin and the polarity of the waves noted for interpretation. Triggered as well as continuous EOG responses were recorded after monopolar electrode stimulation of cranial nerve (CN) during tumour removal which helped the surgeon with careful dissection and avoiding potential nerve injuries.
Results:
Of the 11 cases monitored, oculomotor and abducent nerves were identified in all cases, but the trochlear nerve could not be definitively identified. Six patients had no pre- or post-operative extraocular motor nerve dysfunction. The other five patients had pre-existing deficits before surgery, which recovered completely in two, significantly in one, and did not improve in two patients at 3–6 months follow-up.
Conclusions:
EOG was found to be a simple and reliable method of monitoring extraocular motor nerves (CNs III and VI) intraoperatively.
Key words: Extraocular motor nerves, extraocular movements, intra-operative electrooculographic monitoring, skull base surgery
INTRODUCTION
Intra-operative preservation of extraocular motor nerves is one of the main goals of skull base tumour surgeries.[1] Intra-operative electromyographic (EMG) monitoring of these nerves has been reported previously,[1,2,3,4,5] most of which require complex and skilful placement of recording electrodes. Electrooculographic (EOG) technique is a simple and reliable method for monitoring the extraocular movements (EOM).[6] However, literature reports are few and do not present any definitive suggestions regarding the same. The present study describes the experience in our centre with EOG monitoring in skull base surgeries. The primary aim of this retrospective study was to analyse the utility of EOG monitoring in preventing extraocular motor nerve dysfunction during surgeries on tumours of the skull base. The secondary aim was to find out whether EOG monitoring would help in preventing injury to extraocular motor nerves translating as good clinical outcome, with better functional preservation of the nerves.
METHODS
Collection of the patient and monitoring data and analysis was done retrospectively for which ethics committee waiver of patient consent was obtained. Informed consent for intra-operative neurophysiological monitoring was obtained as part of the anaesthesia and surgical consents. Informed patient consent was obtained for publication of image with identification details. Intra-operative EOG monitoring was done in eleven patients with skull base tumours over a period of 2 years (October 2011 to December 2013), in whom there was a risk of injury to extraocular motor nerves during surgery. All patients were operated in our centre after detailed clinical and radiological diagnosis. The data were collected from the patient records regarding anaesthesia and surgical details, perioperative course of the patient, and the follow-up details were collected from the computerised records and outpatient written notes. The intra-operative neurophysiological recordings were retrieved from the historical recorded waveforms, annotated during live monitoring, from the monitoring system (described below).
Anaesthesia was induced with propofol 2 mg/kg and fentanyl 2 μg/kg. Maintenance was with total intravenous anaesthetic technique and no muscle relaxant (after rocuronium used for endotracheal intubation at 0.6 mg/kg). Morphine 0.1 mg/kg was given to all patients at skin incision and repeated at 0.05–0.1 mg/kg every 4 h for analgesia and better endotracheal tube tolerance along with continuous propofol infusion (8–10 mg/kg/h) and ventilation was with air-oxygen mixture (50:50).
Monitoring equipment used for EOG was the commercially available neurophysiological monitoring system (Protektor, Xltek®, Canada). It was used to detect the effects induced by intra-operative stimulation and manipulation of the cranial nerves (CNs) related to EOM, in addition to EMG of 5th, 7th and lower CNs and evoked potential monitoring in some cases. The decision on the modality of monitoring was based on tumour location and the surgical approach, in coordination with the surgeon. The recording was done from two channels horizontal and vertical by inserting disposable subdermal needle electrodes along the periorbital area [Figure 1]. All electrodes were secured in position by use of adhesive tapes. For horizontal channel, the active electrode was placed near the medial canthus and the reference near the lateral canthus for the monitored eye. For vertical channel, the active electrode was placed on the upper and the reference electrode on the lower side of the orbital margin. Ground (anodal) electrode was placed on the mentum. Bilateral EOG recording was done in midline and brainstem lesions. Cathodal stimulation was done by the surgeon using monopolar electrodes to stimulate the CNs during surgery. Rectangular pulses with a frequency of 4.7 Hz, pulse duration of 0.2 ms and intensity of 1 mA were applied. Stimulator settings were: Sensitivity 100 μv/div, time base 2 ms/div, low-frequency filter 10 Hz and high-frequency filter 1 kHz. Responses were recorded as positive or negative wave on the monitor as well as simultaneous acoustic feedback transmitted via a loudspeaker. The responses could be interpreted by the anaesthesiologist and did not demand the constant presence of neurologist or neurophysiology technician in the operating room. However, they were immediately available in the hospital for any technical snag or difficulty in interpretation. Whenever a response was recorded upon surgical site stimulation, the surgeon proceeded with dissection carefully with repeated stimulation and assessment of EOG response to avoid injury to the extraocular motor nerves. Immediate post-operative clinical evaluation of the patient was done to assess any change from the pre-existing extraocular motor nerve dysfunction and for any new onset dysfunction. The outcome was assessed in terms of change in extraocular motor nerve function from the post-operative status to that at 6 months.
Figure 1.
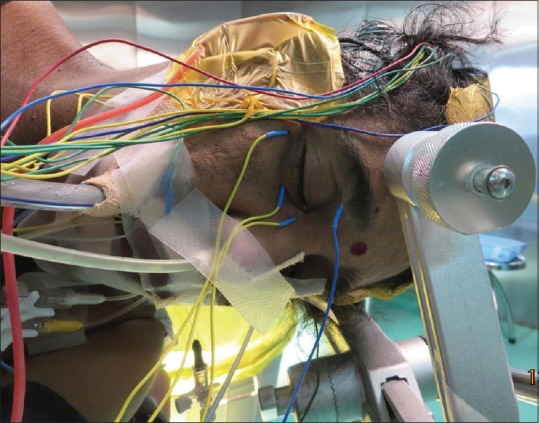
Patient positioned for excision of right petroclival meningioma. Subdermal needle electrodes inserted along right periorbital area depicted
RESULTS
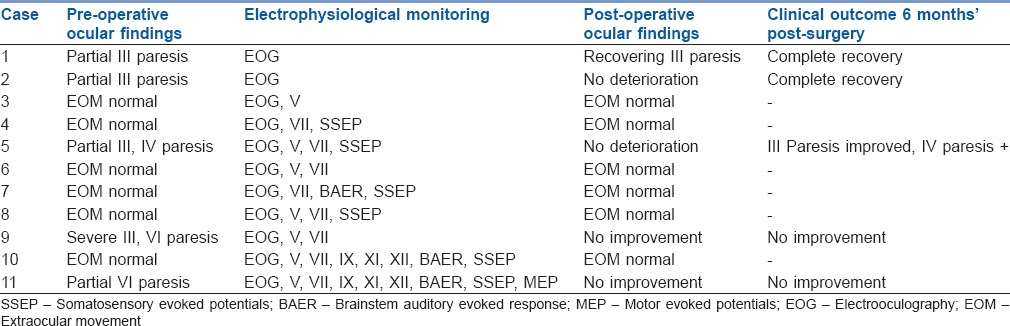
Demographic data, diagnoses, ocular findings, surgical approach and clinical outcome at the end of 6 months after surgery for the 11 patients are summarised in Tables 1 and 2. The EOG responses observed were electrical stimulation triggered responses and mechanically induced responses as monitored by continuous recording.
Table 1.
Patient demographics at admission and surgical approach
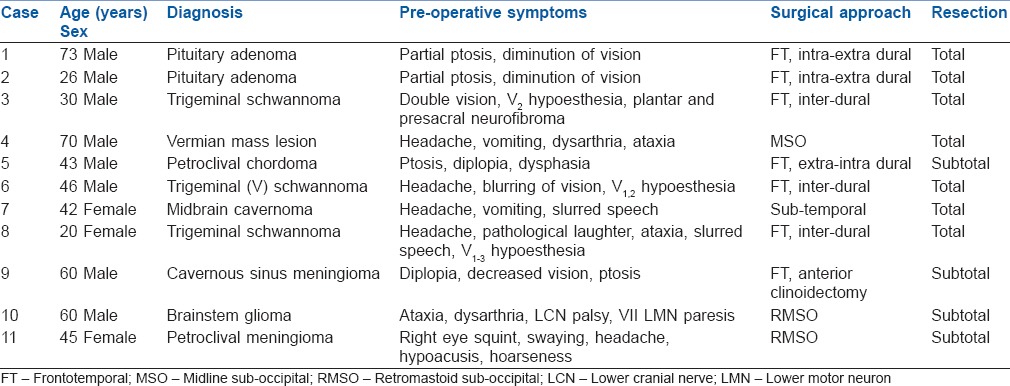
Table 2.
Perioperative findings and clinical outcome data at 6 months
Oculomotor (III) and abducent (VI) nerves could be identified in all the cases during surgical exposure. Electrical stimulation of the III CN yielded a positive monophasic response in horizontal channel traces, indicating movements of the eyeball towards the active electrode [Figure 2]. Electrical stimulation of the VI CN yielded a negative monophasic response in horizontal channel traces, indicating movements of the eyeball away from active electrode [Figure 3]. Trochlear (IV) nerve could be identified in only two patients. Electrical stimulation of IV nerve yielded a biphasic wave in the vertical channel traces.
Figure 2.
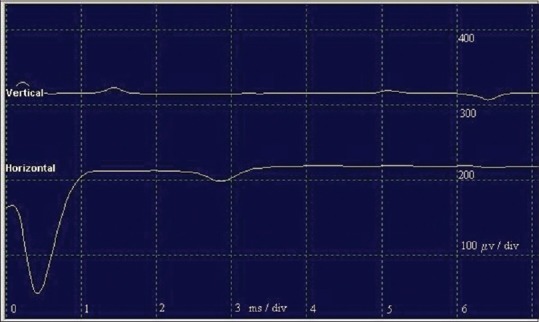
A positive monophasic response (negative deflection) in the horizontal traces, indicating movement of the eyeball towards the active electrode at the medial canthus, in response to III cranial nerve stimulation
Figure 3.
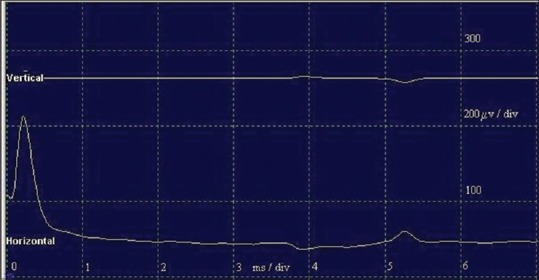
A negative monophasic response (positive deflection) in the horizontal traces, indicating movement of the eyeball away from the active electrode at the medial canthus, in response to VI cranial nerve stimulation
Mechanically induced responses were recorded as spikes during continuous monitoring at the time of surgical manipulation/dissection of the tumour tissue close to the nerves.
The surgical tumour removal was total in seven patients and subtotal in four patients. Six out of 11 patients had no pre- or post-operative extraocular motor nerve dysfunction. The other five patients had pre-existing deficits before surgery, which remained the same in the immediate post-operative period but recovered completely in two, significantly in one and showed no improvement in two patients at 6 months follow-up [Table 2].
DISCUSSION
The key findings of the present study are that the extraocular motor nerves (mainly III, VI) could be identified in all cases during the skull base surgery with the help of EOG monitoring. The follow-up showed good clinical outcome in the form of no extraocular motor nerve deficits or no worsening from the pre-operative deficits.
Skull base tumours are known to invade the cavernous sinus and can damage the extraocular motor nerves. These tumours tend to be large at the time of detection and often distort the anatomy; hence, intra-operative monitoring of these nerves aids the surgeon in identifying the anatomical location and preventing iatrogenic injury.[7,8] The EMG technique of intra-operative monitoring has not been widely utilised for these nerves unlike other CNs because the extraocular muscles are small (around 2-3 mm diameter) and located deep inside the orbital cavity and therefore lead to technical difficulty. Hence, EOG technique, which is a simple method with easy setup of the monitoring system, was used in our patients.
The EOG is based on the working principle that the eyeball represents an electrical dipole with the positive pole at the cornea and negative at the retina and axial eye movements lead to changes in the corneoretinal resting potential. It was first described by Geoffrey Arden in 1962 and has since been used to evaluate oculomotor abnormalities and in the diagnosis of retinal and macular pathologies with newer applications being developed such as sleep pattern studies and human computer interface systems for persons with motor impairment.[9,10] EOG is the response recorded at the periorbital skin using surface electrodes placed around both eyes whenever the eyeball moves following electrical stimulation or surgical manipulation.
The electrical stimulation used in our cases was through monopolar stimulating electrode. Monopolar stimulation provides a radial diffusion of current that covers an approximately spherical space around the stimulating electrode with a relatively high volume of tissue activated during stimulation, hence requiring lower current intensity. We used monopolar stimulation since it is useful in a focused and deep operative field, easy to manipulate and can also be used as a tumour dissector.
Most of the investigators have used EMG technique using needle electrodes or a specially designed ring electrode to monitor the extraocular nerves.
A group of investigators developed a ring electrode and stimulated the ocular motor nerves electrically in 22 patients and recorded compound muscle action potentials from the extraocular muscles with the electrode placed epiconjunctivally.[1] However, the fixation of this ring electrode requires invasive microsurgical procedure by attaching the electrode with the help of sutures through the ring and into the extraocular muscles.
Another group of investigators has used EMG of extraocular muscles by placing transcutaneous needle electrodes near the orbital muscles to monitor III, IV and VI nerves. They showed that it was useful in aggressive surgical approach to the cavernous sinus tumours to facilitate total resection. Among the seven patients, pre-operative CN deficits improved in three, two other patients had transient palsy of III, IV, VI and one had only VI nerve paresis.[3]
Intra-operative EMG was monitored in 18 patients in another study by placement of single shafted bipolar electrodes in the extraocular muscles under the guidance of B-mode ultrasound. There was no distinct relationship between ocular motor nerve function and neurophysiological parameters and the predictive value for the clinical outcome was poor.[4]
In yet another method of insertion of needle electrodes, a group of authors in a study have utilised neuronavigation method. They utilised this method to monitor the oculomotor system in 10 patients. With the optical tracking system, percutaneous needle electrodes were inserted into the lateral rectus, inferior rectus and superior oblique muscle along the axis of a hand-held pointer or by means of an electrode applicator. EMG monitoring of III, IV and VI nerve function was done successfully with this method.[5]
Intra-operative EOG monitoring was initially utilised in an innovative study; wherein, it was applied to 12 cases of skull base tumour surgeries.[11] Surface electrodes were placed along the periorbital skin. The active and reference electrodes were placed in horizontal and vertical orientation constituting two channels. Total intravenous anaesthesia was employed for maintenance. Depending on the eye movement and polarity of the wave in the EOG recording, the III and VI nerves could be identified in the horizontal orientation channel. Since the stimulation of IV nerve did not yield consistent response in any channels, the vertical orientation channel was used in only initial four cases. Mechanical manipulation yielded polyphasic waves with polarity opposite to that of electrical EOG response. The authors have mentioned normal pre-operative and post-operative findings of EOM in the two illustrative cases and excellent results in the other cases also.
In our centre, we employed EOG technique in 11 cases with skull-base tumours. We used disposable needle electrodes instead of surface electrodes because of the need for stable recordings for long duration and fewer chances of dislodgement after patient positioning. III and VI CNs could be consistently identified in all the cases in horizontal channel and IV nerve could be identified in two cases in vertical channel recordings. Mechanical responses were identified as spikes in horizontal channels with no relationship to EOG response to electrical stimulation or their polarity. No complications were attributed to the needle electrode insertion or the EOG technique.
EOG technique has also been used during transsphenoidal surgeries for pituitary adenoma to prevent post-operative extraocular motor nerve dysfunction. In a study by a group of clinicians, 100 patients were monitored and the rate of transient diplopia was 1% in the monitoring group versus 4.8% in the control but this did not reach statistical significance. However, they concluded that EOG was a novel, efficient and simple method to prevent post-operative extraocular motor nerve palsy.[12]
Trochlear nerve stimulation recordings are difficult to obtain and lack reproducibility either by EMG or EOG technique.[13] In EMG technique, it is difficult to access the superior oblique because it is small in size and lies deep between superior and medial rectus in the orbital cavity and in some studies have necessitated orbital osteotomy for electrode placement in superior oblique muscle.[1,13] In EOG method, since the trochlear nerve causes intorsion in the abducted eye and depression in the adducted eye, it is difficult to elicit those movements. Furthermore, the movements are primarily around the anteroposterior axis and torsional movements around the axis do not cause much change in the potential difference and cannot be recorded on the vertical monitoring channel.[14] Another noteworthy point is that in distinction to all other CNs, the trochlear nerve exits from the dorsal surface of the brainstem and crosses the midline before emerging from the brainstem to innervate the superior oblique muscle on the contralateral side. Hence, in lesions affecting the midline and brainstem, bilateral recordings have to be done.
Functional impairment of IV nerve leads to less significant interference with the use of eye than impairment of the III and VI nerves.[7] Cranial nerve III deficit essentially leads to functional blindness of the affected eye since it leads to severe impairment of the eye movement, ptosis and pupillary dilatation. Thus, the main utility is in monitoring III and VI nerves, the dysfunction of which leads to more serious complications.
The strengths of this study arises from the fact that EOG monitoring is a simple and easy to interpret method, useful in identifying the extraocular motor nerves during skull base surgeries with good results in the follow-up. This method could be useful in facilitating more complete resection of skull base tumours by preserving these nerves. The limitations of the study are the retrospective nature of the study, small sample size, absence of a control group without electrophysiological monitoring and absence of a control group with EMG monitoring. In addition, statistical analysis was not possible because of the limited number of patients. This precludes us from commenting on the prognostic value of this type of monitoring.
The available studies in literature employing EOG monitoring are scarce and EMG is considered to be the gold standard for monitoring extraocular motor nerves. However, the EMG of these CNs is not monitored as frequently as other CNs in most centres, considering the complexity involved in inserting the needle electrodes into small and deeply situated extraocular muscles. This has led to underutilization of these CNs monitoring. Although the present study was done in a smaller population, it is easy to monitor and could be done using the same neurophysiological monitoring system used to monitor other CNs and evoked potentials. Further prospective clinical research comparing EOG and EMG methods and evaluating the clinical outcomes would provide important information on the prognostic value of these methods.
CONCLUSIONS
EOG was found to be a simple and reliable method of monitoring extraocular motor nerves intraoperatively. However, only mapping of the oculomotor and abducent nerves can be done but quantitative evaluations cannot be derived from the EOG data. It is difficult to monitor oblique extraocular muscles and it would be worthwhile to develop a simple method for this.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sekiya T, Hatayama T, Iwabuchi T, Maeda S. Intraoperative recordings of evoked extraocular muscle activities to monitor ocular motor nerve function. Neurosurgery. 1993;32:227–35. doi: 10.1227/00006123-199302000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Sekiya T, Hatayama T, Iwabuchi T, Maeda S. A ring electrode to record extraocular muscle activities during skull base surgery. Acta Neurochir (Wien) 1992;117:66–9. doi: 10.1007/BF01400639. [DOI] [PubMed] [Google Scholar]
- 3.Sekhar LN, Møller AR. Operative management of tumors involving the cavernous sinus. J Neurosurg. 1986;64:879–89. doi: 10.3171/jns.1986.64.6.0879. [DOI] [PubMed] [Google Scholar]
- 4.Schlake HP, Goldbrunner R, Siebert M, Behr R, Roosen K. Intra-operative electromyographic monitoring of extra-ocular motor nerves (Nn. III, VI) in skull base surgery. Acta Neurochir (Wien) 2001;143:251–61. doi: 10.1007/s007010170105. [DOI] [PubMed] [Google Scholar]
- 5.Alberti O, Sure U, Riegel T, Bertalanffy H. Image-guided placement of eye muscle electrodes for intraoperative cranial nerve monitoring. Neurosurgery. 2001;49:660–3. doi: 10.1097/00006123-200109000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Marmor MF, Zrenner E. Standard for clinical electro-oculography. International Society for Clinical Electrophysiology of Vision. Arch Ophthalmol. 1993;111:601–4. doi: 10.1001/archopht.1993.01090050035023. [DOI] [PubMed] [Google Scholar]
- 7.Møller AR, editor. Intraoperative Neurophysiological Monitoring. 3rd ed. Totowa, New Jersey: Humana Press; 2011. Practical aspects of monitoring cranial motor nerves; pp. 235–60. [Google Scholar]
- 8.Doglietto F, Radovanovic I, Gentili F. Indications and technology of neurophysiologic monitoring in meningioma surgery. In: Pamir MN, Black PM, Fahlbusch R, editors. Meningiomas: A Comprehensive Text. Philadelphia: Saunders/Elsevier Inc.; 2010. pp. 311–23. [Google Scholar]
- 9.Ingster-Moati I, Bui Quoc E, Pless M, Djomby R, Orssaud C, Guichard JP, et al. Ocular motility and Wilson's disease: A study on 34 patients. J Neurol Neurosurg Psychiatry. 2007;78:1199–201. doi: 10.1136/jnnp.2006.108415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melek NB, Blanco S, Garcia H. Electro-oculography of smooth pursuit and optokinetic nystagmus eye movements in type I Duane's retraction syndrome. Binocul Vis Strabismus Q. 2006;21:37–44. [PubMed] [Google Scholar]
- 11.Fukaya C, Katayama Y, Kasai M, Kurihara J, Yamamoto T. Intraoperative electro-oculographic monitoring for skull base surgery. Skull Base Surg. 2000;10:11–5. doi: 10.1055/s-2000-6788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawamata T, Ishii N, Amano K, Namioka T, Hori T, Okada Y. A novel simple real-time electrooculographic monitoring system during transsphenoidal surgeries to prevent postoperative extraocular motor nerve dysfunction. Neurosurg Rev. 2013;36:371–6. doi: 10.1007/s10143-012-0438-6. [DOI] [PubMed] [Google Scholar]
- 13.Kawaguchi M, Ohnishi H, Sakamoto T, Shimizu K, Touho H, Monobe T, et al. Intraoperative electrophysiologic monitoring of cranial motor nerves in skull base surgery. Surg Neurol. 1995;43:177–81. doi: 10.1016/0090-3019(95)80131-y. [DOI] [PubMed] [Google Scholar]
- 14.Heide W, Koenig E, Trillenberg P, Kömpf D, Zee DS. Electrooculography: Technical standards and applications. The International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1999;52:223–40. [PubMed] [Google Scholar]


