Abstract
Background and Aims:
Laryngeal mask airway (LMA) cuff pressure increases when the air is used for the cuff inflation during oxygen: nitrous oxide (O2:N2O) anaesthesia, which may lead to various problems. We compared the effects of different gases for ProSeal LMA™ (PLMA) cuff inflation in adult patients for various parameters.
Methods:
A total of 120 patients were randomly allocated to four groups, according to composition of gases used to inflate the PLMA cuff to achieve 40 cmH2 O cuff pressure, air (Group A), 50% O2 :air (Group OA), 50% O2:N2O (Group ON) and 100% O2 (Group O). Cuff pressure, cuff volume and ventilator parameters were monitored intraoperatively. Pharyngolaryngeal parameters were assessed at 1, 2 and 24 h postoperatively. Statistical analysis was performed using ANOVA, Fisher's exact test and step-wise logistic regression.
Results:
Cuff pressure significantly increased at 10, 15 and 30 min in Group A, OA and O from initial pressure. Cuff pressure decreased at 5 min in Group ON (36.6 ± 3.5 cmH2 O) (P = 0.42). PLMA cuff volume increased in Group A, OA, O, but decreased in Group ON (6.16 ± 2.8 ml [P < 0.001], 4.7 ± 3.8 ml [P < 0.001], 1.4 ± 3.19 ml [P = 0.023] and − 1.7 ± 4.9 ml [P = 0.064], respectively), from basal levels. Ventilatory parameters were comparable in all four groups. There was no significant association between sore throat and cuff pressure, with odds ratio 1.002.
Conclusion:
Cuff inflation with 50% O2:N2O mixture provided more stable cuff pressure in comparison to air, O2 :air, 100% O2 during O2:N2O anaesthesia. Ventilatory parameters did not change with variation in PLMA cuff pressure. Post-operative sore throat had no correlation with cuff pressure.
Key words: Cuff pressure, pharyngolaryngeal morbidity, ProSeal LMA™, ventilatory parameters
INTRODUCTION
Laryngeal mask airway (LMA) is commonly used airway device for securing the airway during general anaesthesia. LMA cuff is usually inflated with air and the cuff pressure increases during oxygen: nitrous oxide (O2:N2O) anaesthesia.[1] Increased cuff pressure may lead to incorrect positioning of the LMA, inadequate seal, ineffective ventilation, airway contamination, decreased mucosal capillary perfusion and increased pharyngolaryngeal morbidity.[2,3,4]
Manufacturer of the LMA recommends to limit the LMA cuff inflation to achieve an adequate seal with minimal intracuff pressure (not exceeding 60 cmH2 O).[5] A number of studies suggested that manometer should be used to monitor cuff pressure intraoperatively.[6,7,8,9]
Different gases (O2:N2O mixture; O2:N2O and halothane mixture) used for the LMA cuff inflation resulted in decrease in the cuff pressure during O2:N2O anaesthesia.[10,11]
The study aimed to find out which gas or gas mixture used in anaesthesia could provide stable and better intracuff pressures with use of the PLMA.
METHODS
A prospective, randomised, double-blind, comparative study was conducted after obtaining the approval of the Institutional Ethics Committee registered with Clinical Trail Registry India CTRI/2013/08/003888 and written informed consent from 120 patients. Patients above 18 years scheduled for elective surgery, under general anaesthesia with PLMA were enrolled in the study. All the patients were examined in the preanaesthesia room and were informed about the questionnaire related sore throat, dysphagia and dysphonia. Patients with hiatus hernia, gastro-oesophageal reflux and procedures were excluded from the study.
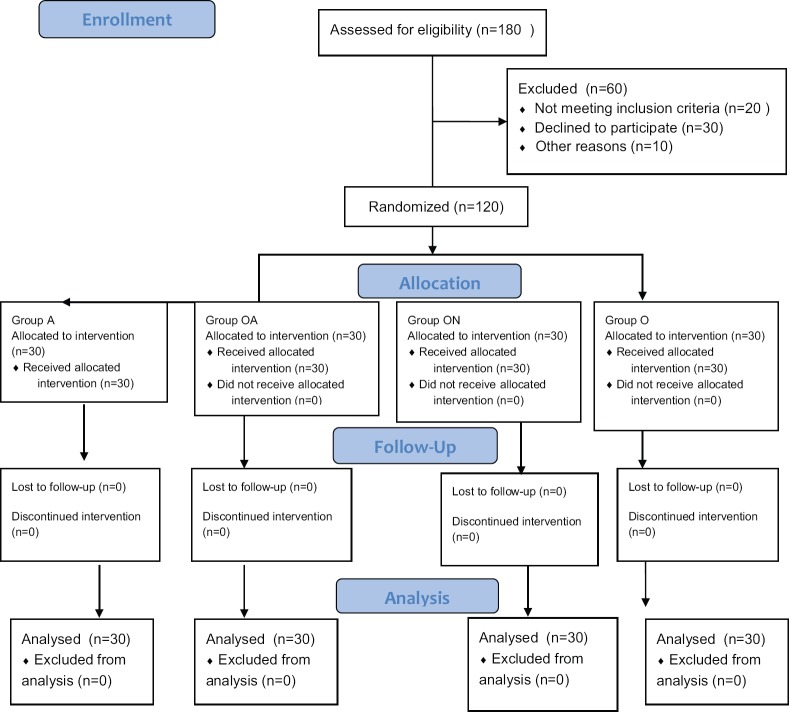
A random number table for 120 patients to be divided into four groups was generated using computer software and sequentially numbered opaque sealed envelopes were prepared [Figure 1]. To maintain the blinding, an anaesthesiologist not involved in the study opened the envelope just before the administration of general anaesthesia and prepared the appropriate gas-filled syringe according to the code to inflate the cuff and did not take part in management and observations. For Group A, room air was filled in 50 ml syringes. Gases of different composition were prepared just before induction in the pre-operative room by an anaesthesiologist not involved in the study. Ventimask tubing was attached to fresh gas outlet of Drager anaesthesia work station (Primus®) for desired composition of gas for different groups (air [Group A], O2 :air [50% O2] [Group OA], O2:N2O [50% O2] [Group ON] or 100% O2 [Group O]) according the group. The other end of the tubing was attached to 50 ml syringe via three-way assembly. The fresh gas flow was set at desired concentration and gas mixture at 5 L flow. Once desired gas is filled in the syringe, three-way was put in off position towards syringe and disconnected from the tubing.
Figure 1.
CONSORT flow diagram
In the operating room, routine monitors were attached to the patient. The size of the PLMA was decided according to the manufacturer guidelines. The PLMA cuff was checked for any leak. General anaesthesia was induced with intravenous fentanyl 2 μg/kg and propofol 1.5 mg/kg. After confirming adequate bag mask ventilation, atracurium 0.5 mg/kg was administered and ventilation was performed with 100% O2 at 5 L fresh gas flow for 3 min. A fully deflated PLMA was inserted by a single anaesthesiologist with more than 1 year of experience of PLMA insertion. The PLMA cuff was inflated by the specified syringe to obtain a cuff pressure of 40 cmH2 O with the help of aneroid cuff pressure manometer (Endotest®, Rusch, Germany), attached to the pilot balloon. The volume of gas inflated was noted. Successful insertion was assessed by chest expansion and capnography. At cuff pressure of 40 cmH2 O, oropharyngeal leak pressure (OLP) was checked by closing adjustable pressure limiting valve at fixed gas flow of 3 L/min. The airway pressure at which leak was heard (by stethoscope) was noted.[12,13] Volume controlled ventilation was initiated and initial ventilatory settings were adjusted to maintain end-tidal carbon dioxide (EtCO2) between 35 and 45 mmHg.
Fresh gas flow composition was changed to O2:N2O (50:50) with isoflurane (1 minimum alveolar concentration) at 3 L for initial 5 min, then subsequently, flow was reduced to 1 L/min (500 ml O2 :500 ml N2 O). Attempts for PLMA insertion, use of Guedel's airway (due to difficult mask ventilation or to relieve post-operative upper airway obstruction), volume of gas injected in the PLMA cuff, initial tidal volume (inspiratory/expiratory), respiratory rate (RR), peak inspiratory airway pressure and EtCO2 were noted after the insertion of PLMA. The cuff pressure and ventilator parameters were noted every 5 min for the first 30 min and then every 10 min till N2 O was switched off and 100% O2 was given to the patient.
At the end of surgery, when the patient was awake and following commands, PLMA was removed, inflated. The presence of blood stain on the cuff was noted. Gas from the PLMA cuff aspirated and the volume noted. Oral suction was avoided as far as possible and if done was noted. The patient was shifted to the post-anaesthesia care unit.
Postoperatively, sore throat, dysphonia and dysphagia were assessed by a questionnaire at 1, 2 and 24h. Sore throat was defined as constant pain or discomfort in the throat independent of swallowing, dysphonia; as difficulty in speaking or pain on speaking, and dysphagia; as difficulty or pain on swallowing.[7]
The primary outcome was to compare the changes in cuff pressure intraoperatively with different gas composition used to inflate PLMA by cuff pressure monitor. The secondary outcome was to compare the effect of PLMA cuff pressure change on intraoperative ventilator parameters and post-operative pharyngolaryngeal morbidity. A pilot study with five patients in each group was conducted before the study. The mean ± standard deviation cuff pressure till 30 min was 74.6 ± 6.4, 79 ± 8, 43.6 ± 6, and 33.2 ± 4 cmH2 O in Group A, Group OA, Group O and Group ON, respectively. Twenty-seven needed to be enrolled in each group to have α of 5% and power of 90%. Thirty patients in each group were enrolled in this study to allow 10% dropout, i.e., exclusion from the study.
The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS™), Windows version 15.0 (South Wacker Drive, Chicago, IL, USA). The results were analysed using one-way ANOVA for continuous variable and Fisher's exact test for categorical variables. Statistical significance between the groups was analysed using post hoc comparison (multiple comparisons) by Bonferroni's method. Apart from univariate analyses, potential predictors of sore throat were analysed with a step-wise logistic regression. The value of P < 0.05 was considered statistically significant.
RESULTS
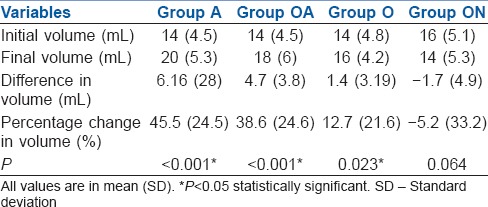
The demographic characteristics, types of surgeries, PLMA sizes, PLMA insertion attempts, OLP and duration of low flow anaesthesia were comparable in between the groups [Table 1]. In Group A, cuff pressure started to increase at 5 min and became statistically significant at 10 min, and continued to increase till 90 min. In Group OA, cuff pressure increase started at 5 min and became statistically significant at 10 min till 30 min then again decreased gradually till 90 min. In Group ON, an insignificant decrease in cuff pressure was observed till 15 min which again increased till 80 min. In Group O, there was increase in cuff pressure at 5 min which became statistically significant from 15 min till maximum at 90 min [Figure 2].
Table 1.
Patient characteristics, size of ProSeal laryngeal mask airway, type and duration of low flow anaesthesia
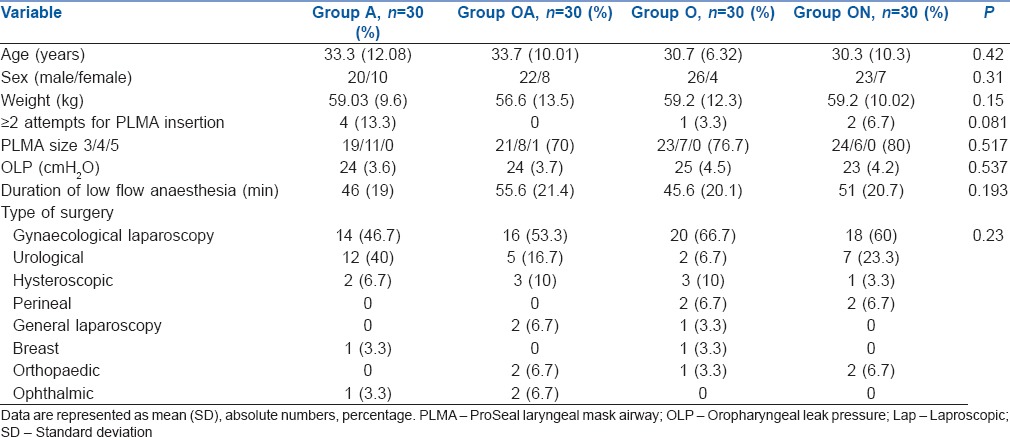
Figure 2.
Change in mean pressure (cmH2O) with time in Group A, OA, O and ON
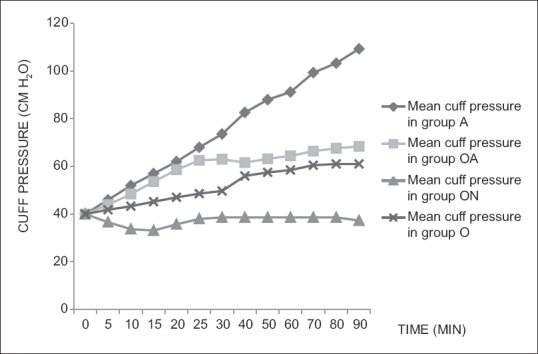
There was statistically significant increase in the gas volume in the PLMA cuff in the Group A, Group OA and O (P: <0.001, <0.001 and 0.023, respectively). There was insignificant decrease in the gas volume (P = 0.064) in Group ON [Table 2].
Table 2.
ProSeal LMA™ cuff volume variation
There was no significant difference in the ventilator parameters, i.e., inspired and expired tidal volume, RR and peak inspired pressure at any point of time in all the groups. Guedel's airway was not used in any patient. The blood on PLMA after removal was noted in four (13.3%) patients in Group A and two (6.7%) patients in Group ON, which was not statistically significant. Number of patients requiring oral suctioning was not statistically significant.
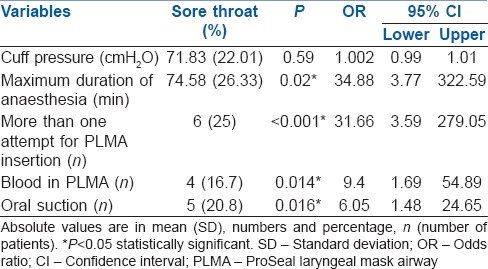
The incidence of sore throat, dysphagia, and dysphonia were not statistically significant at any point of time till 24 h in between the groups [Table 3]. Sore throat did not have a statistically significant correlation with cuff pressure (P = 0.59). Sore throat had statistical significant correlation with duration of anaesthesia (P = 0.02), with more than one attempt of LMA insertion (P < 0.001), blood on LMA (P = 0.014), oral suctioning (P = 0.016) [Table 4]. None of the predictors showed correlation with dysphagia and dysphonia.
Table 3.
Pharyngolaryngeal morbidity at 1, 2 and 24 h
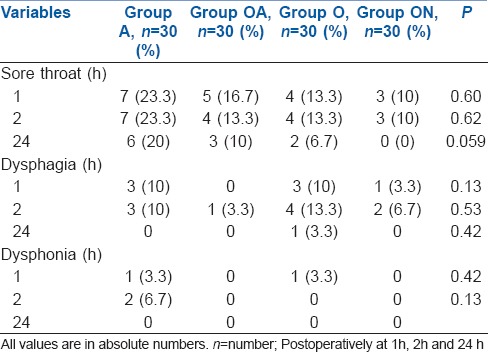
Table 4.
Univariate predictors of sore throat
DISCUSSION
In this study, increase in cuff pressure and final aspirated volume was significant in Group A, OA and O. This increase was more in Group A in comparison to Group OA and O. Although cuff pressure remained fairly stable in Group ON, the final aspirated volume was also decreased in Group ON. LMA silicon cuff acts as a semi-permeable membrane which results in diffusion of different gases between the cuff and inspired air. The amount and direction of the diffusion depend on the partial pressure gradient.[14] There was a continuous increase in PLMA cuff pressure in Group A from 40 cmH2 O to final mean cuff pressure of 109 cmH2 O. The blood gas coefficient of N2 O is 0.46, which is thirty times greater than nitrogen, present in the air. It is therefore possible that N2 O diffuses inside the cuff quickly, whereas nitrogen diffuses out slowly.[15] The increase in cuff pressure when the air is used for inflating the cuff was documented both in vivo and in vitro from 40 cmH2 O to 80 cmH2 O in 60 min.[1,14] It was also observed that the mean cuff pressure started increasing within 5 min of N2 O exposure to reach a plateau after 45 min till 115 min.[12] The continuous increase in cuff pressure from 20 to 200 cmH2 O at 350 min with N2 O anaesthesia has also been demonstrated.[16]
In Group ON, decrease in cuff pressure was observed at 15 min which again gradually increased to near initial pressures. Studies have revealed decrease in cuff pressure when mixtures of N2 O, O2, halothane or enflurane or isoflurane have been used to inflate the cuff during O2 and N2 O anaesthesia, as diffusion of N2 O inside the cuff is prevented.[2,10,11,17] When PLMA cuff is inflated with 50% N2 O, it creates a pressure above the atmospheric pressure at 40 cmH2 O which leads to a pressure gradient between the inside and outside of the cuff resulting in the diffusion of N2 O out of the cuff resulting in an initial decrease in pressure and volume.[18]
In Group OA, cuff pressure increased till 30 min and then gradually decreased. There has been no study till date to evaluate the effect of O2 and air mixture on cuff pressure with N2 O anaesthesia. We hypothesize that the decrease in concentration of nitrogen due to dilution of air with 50% O2 may lead to lesser degree of diffusion of N2 O inside the cuff resulting in more gradual rise in cuff pressure than that of air only.
In Group O, increase in cuff pressure up to 61 cmH2 O was observed. Since N2 O is more soluble than O2, there is diffusion of N2 O inside the cuff. In vitro study showed O2 diffusion across the cuff is <10% of N2 O.[14] N2 O being more permeable than O2 and nitrogen could have led to the rise in cuff pressure in this group. However, increase is lesser than that of air and air: O2 mixture because of relatively lesser permeability of N2 O with O2 in comparison to nitrogen.
In this study, fresh gas flows were kept constant in all the patients. The rate of diffusion of N2 O across the cuff is affected by the area available for diffusion, the cuff material and the number of time LMA is autoclaved.[1,8] The change in cuff pressure and volume can occur with the warming of gases inside the cuff.[18] The LMA size, position and head manipulation might also influence the cuff pressure.[12] To avoid this bias, in this study head of the patient was kept at the neutral position and cuff pressure recording was started after positioning the patient.
We inflated PLMA cuff till 40 cmH2 O as lower cuff pressures result in a better seal, optimal fibreoptic position, optimal functioning and efficacious positive pressure ventilation.[19,20,21,22,23] OLP was between 23 and 25 mmHg in all the groups and the mean calculated leak volume was <10 ml. The change in the cuff pressure in different groups did not affect ventilatory parameters and leak volume. Higher leak volume was observed with cuff pressure of 60 cmH2 O (0.65 ml/kg) than 40 cmH2 O (0.42 ml/kg) and 20 cmH2 O (0.51 ml/kg), but it was not associated with air leakage in any patient.[20]
In this study, the post-operative pharyngolaryngeal morbidity was comparable in all the groups. The incidence of post-operative sore throat with LMA ranges from 17.5% to 45.6%.[7,22,24] LMA cuff pressure rise has been implicated as a primary reason for post-operative pharyngolaryngeal morbidity.[2,6,8,9,13] However, in this study, PLMA cuff pressure had no correlation with the incidence of pharyngolaryngeal morbidity. This could be attributed to the initial low cuff pressure (40 cmH2 O). Therefore, even with the pressure up to 110 cmH2 O in some cases, the duration was not prolonged enough to cause decrease in mucosal perfusion. No difference in post-operative sore throat was observed with cuff pressure of 30 mmHg and 180 mmHg during O2:N2O anaesthesia (50% vs. 42%).[25] Increase in cuff pressure (35 vs. 50 mmHg) also had no correlation with post-operative pharyngolaryngeal complications.[26]
Low incidence of post-operative pharyngolaryngeal morbidity in this study may be due to the administration of neuromuscular blockers. Higher incidence of sore throat have been reported with spontaneous ventilation in comparison to controlled ventilation, owing to increased pharyngeal muscle tone.[22]
In this study, the volume of gas inflated was also less than the maximum recommended volume (50-70% less) for PLMA size, which could be the additional factor for decreased pharyngolaryngeal morbidity in the studied patients. Brimacombe et al. also reported reduced pharyngolaryngeal morbidity at 18-24 h postoperatively with low cuff volume than higher volume (20% vs. 42%).[24] Other causes of pharyngolaryngeal morbidity are anaesthesiologist's skill, the level of insertion difficulty, the number of insertion attempts, the LMA size, dry and cold gas, the duration of anaesthesia.[22,27] In this study, there was a significant correlation of sore throat with more than one attempt of PLMA insertion. Nott et al. also quoted that multiple insertion attempts can lead to sore throat.[28]
Prolonged duration of anaesthesia also had a positive correlation with sore throat. This could be due to the pressure on the pharyngeal mucosa for a prolonged period, leading to decreased mucosal perfusion.[22]
The presence of blood on PLMA and use of oral suction were also significantly related to sore throat in the post-operative period. This may be due to oropharyngeal trauma.
Limitations of the study were exact composition of gas mixture was not analysed before inflation of cuff and the correct position of the LMA were not confirmed by fibreoptic bronchoscopy. Analysis of gas composition after deflation of cuff might have provided information regarding the diffusion of different gases through LMA cuff.
CONCLUSION
O2:N2O (50% O2) mixture provides a relatively stable cuff pressure in comparison to air, O2 :air (50% O2) and 100% O2 during O2:N2O anaesthesia. Ventilatory parameters are not affected with change in LMA cuff pressure and volume. Post-operative sore throat had no correlation with increased cuff pressure. However, postoperative sore throat had strong correlation with more than one attempt of LMA insertion, and prolonged duration of anaesthesia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Maino P, Dullenkopf A, Bernet V, Weiss M. Nitrous oxide diffusion into the cuffs of disposable laryngeal mask airways. Anaesthesia. 2005;60:278–82. doi: 10.1111/j.1365-2044.2004.04072.x. [DOI] [PubMed] [Google Scholar]
- 2.O’Kelly SW, Heath KJ, Lawes EG. A study of laryngeal mask inflation. Pressures exerted on the pharynx. Anaesthesia. 1993;48:1075–8. [PubMed] [Google Scholar]
- 3.Marjot R. Laryngeal mask cuff pressures. Anaesthesia. 1994;49:447. doi: 10.1111/j.1365-2044.1994.tb03488.x. [DOI] [PubMed] [Google Scholar]
- 4.Keller C, Brimacombe J. Mucosal pressure and oropharyngeal leak pressure with the ProSeal versus laryngeal mask airway in anaesthetized paralysed patients. Br J Anaesth. 2000;85:262–6. doi: 10.1093/bja/85.2.262. [DOI] [PubMed] [Google Scholar]
- 5.LMA™ airway instruction manual. San Diego: LMA North America Inc.; 2005. [Last accessed on 2015 Apr 27]. Available from: http://documents.mx/documents/lmaairways-manual.html . [Google Scholar]
- 6.Wong JG, Heaney M, Chambers NA, Erb TO, von Ungern-Sternberg BS. Impact of laryngeal mask airway cuff pressures on the incidence of sore throat in children. Paediatr Anaesth. 2009;19:464–9. doi: 10.1111/j.1460-9592.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 7.Seet E, Yousaf F, Gupta S, Subramanyam R, Wong DT, Chung F. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: A prospective, randomized trial. Anesthesiology. 2010;112:652–7. doi: 10.1097/ALN.0b013e3181cf4346. [DOI] [PubMed] [Google Scholar]
- 8.Jeon YS, Choi JW, Jung HS, Kim YS, Kim DW, Kim JH, et al. Effect of continuous cuff pressure regulator in general anaesthesia with laryngeal mask airway. J Int Med Res. 2011;39:1900–7. doi: 10.1177/147323001103900534. [DOI] [PubMed] [Google Scholar]
- 9.Burgard G, Möllhoff T, Prien T. The effect of laryngeal mask cuff pressure on postoperative sore throat incidence. J Clin Anesth. 1996;8:198–201. doi: 10.1016/0952-8180(95)00229-4. [DOI] [PubMed] [Google Scholar]
- 10.Algren JT, Gursoy F, Johnson TD, Skjonsby BS. The effect of nitrous oxide diffusion on laryngeal mask airway cuff inflation in children. Paediatr Anaesth. 1998;8:31–6. doi: 10.1046/j.1460-9592.1998.00696.x. [DOI] [PubMed] [Google Scholar]
- 11.Tekin M, Kati I, Tomak Y, Yuca K. Comparison of the effects of room air and N2O + O2 used for ProSeal LMA cuff inflation on cuff pressure and oropharyngeal structure. J Anesth. 2008;22:467–70. doi: 10.1007/s00540-008-0654-y. [DOI] [PubMed] [Google Scholar]
- 12.van Zundert T, Brimacombe J. Comparison of cuff-pressure changes in silicone and PVC laryngeal masks during nitrous oxide anaesthesia in spontaneously breathing children. Anaesthesiol Intensive Ther. 2012;44:63–70. [PubMed] [Google Scholar]
- 13.Keller C, Pühringer F, Brimacombe JR. Influence of cuff volume on oropharyngeal leak pressure and fibreoptic position with the laryngeal mask airway. Br J Anaesth. 1998;81:186–7. doi: 10.1093/bja/81.2.186. [DOI] [PubMed] [Google Scholar]
- 14.Lumb AB, Wrigley MW. The effect of nitrous oxide on laryngeal mask cuff pressure. In vitro and in vivo studies. Anaesthesia. 1992;47:320–3. doi: 10.1111/j.1365-2044.1992.tb02173.x. [DOI] [PubMed] [Google Scholar]
- 15.Stanley TH, Liu WS. Tracheostomy and endotracheal tube cuff volume and pressure changes during thoracic operations. Ann Thorac Surg. 1975;20:144–51. doi: 10.1016/s0003-4975(10)63868-4. [DOI] [PubMed] [Google Scholar]
- 16.Moon BE, Kim MS, Lee JR. A simple method of partial inflation of the LMA cuff before insertion in children to allow cuff pressure without adjustment after insertion. Korean J Anesthesiol. 2012;62:524–8. doi: 10.4097/kjae.2012.62.6.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ong M, Chambers NA, Hullet B, Erb TO, von Ungern-Sternberg BS. Laryngeal mask airway and tracheal tube cuff pressures in children: Are clinical endpoints valuable for guiding inflation? Anaesthesia. 2008;63:738–44. doi: 10.1111/j.1365-2044.2008.05486.x. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell V, Adams T, Calder I. Choice of cuff inflation medium during nitrous oxide anaesthesia. Anaesthesia. 1999;54:32–6. doi: 10.1046/j.1365-2044.1999.00646.x. [DOI] [PubMed] [Google Scholar]
- 19.Licina A, Chambers NA, Hullett B, Erb TO, von Ungern-Sternberg BS. Lower cuff pressures improve the seal of pediatric laryngeal mask airways. Paediatr Anaesth. 2008;18:952–6. doi: 10.1111/j.1460-9592.2008.02706.x. [DOI] [PubMed] [Google Scholar]
- 20.Hockings L, Heaney M, Chambers NA, Erb TO, von Ungern-Sternberg BS. Reduced air leakage by adjusting the cuff pressure in pediatric laryngeal mask airways during spontaneous ventilation. Paediatr Anaesth. 2010;20:313–7. doi: 10.1111/j.1460-9592.2010.03277.x. [DOI] [PubMed] [Google Scholar]
- 21.Wallace CJ, Chambers NA, Erb TO, von Ungern-Sternberg BS. Pressure volume curves of paediatric laryngeal mask airways. Anaesthesia. 2009;64:527–31. doi: 10.1111/j.1365-2044.2008.05819.x. [DOI] [PubMed] [Google Scholar]
- 22.Grady DM, McHardy F, Wong J, Jin F, Tong D, Chung F. Pharyngolaryngeal morbidity with the laryngeal mask airway in spontaneously breathing patients: Does size matter? Anesthesiology. 2001;94:760–6. doi: 10.1097/00000542-200105000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Okuda K, Inagawa G, Miwa T, Hiroki K. Influence of head and neck position on cuff position and oropharyngeal sealing pressure with the laryngeal mask airway in children. Br J Anaesth. 2001;86:122–4. doi: 10.1093/bja/86.1.122. [DOI] [PubMed] [Google Scholar]
- 24.Brimacombe J, Holyoake L, Keller C, Barry J, Mecklem D, Blinco A, et al. Emergence characteristics and postoperative laryngopharyngeal morbidity with the laryngeal mask airway: A comparison of high versus low initial cuff volume. Anaesthesia. 2000;55:338–43. doi: 10.1046/j.1365-2044.2000.01285.x. [DOI] [PubMed] [Google Scholar]
- 25.Rieger A, Brunne B, Striebel HW. Intracuff pressures do not predict laryngopharyngeal discomfort after use of the laryngeal mask airway. Anesthesiology. 1997;87:63–7. doi: 10.1097/00000542-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Figueredo E, Vivar-Diago M, Muñoz-Blanco F. Laryngo-pharyngeal complaints after use of the laryngeal mask airway. Can J Anaesth. 1999;46:220–5. doi: 10.1007/BF03012599. [DOI] [PubMed] [Google Scholar]
- 27.Rieger A, Brunne B, Hass I, Brummer G, Spies C, Striebel HW, et al. Laryngo-pharyngeal complaints following laryngeal mask airway and endotracheal intubation. J Clin Anesth. 1997;9:42–7. doi: 10.1016/S0952-8180(96)00209-7. [DOI] [PubMed] [Google Scholar]
- 28.Nott MR, Noble PD, Parmar M. Reducing the incidence of sore throat with the laryngeal mask airway. Eur J Anaesthesiol. 1998;15:153–7. [PubMed] [Google Scholar]