Abstract
Objective
Little data is available to inform clinical expectations about course and prognosis of severe OCD. This information is necessary to guide clinicians and to inform criteria for invasive interventions for severe and intractable OCD. This study sought to examine course and prospective predictors of a chronic course in patients with severe OCD over five years.
Method
A selected subset of adults in the Brown Longitudinal Obsessive-Compulsive Study (BLOCS) was included. Adult BLOCS participants were enrolled between 2001 and 2006. All participants in the current study had DSM-IV OCD diagnosis, severe OCD symptoms at baseline, and at least one year of follow-up data.
Results
Cox proportional hazard models were used to examine the general pattern of course in the severe OCD sample based on Longitudinal Interval Follow-Up Evaluation (LIFE) psychiatric status ratings, as well as test predictors of chronically severe course. Results indicated that approximately half of patients with severe OCD at baseline drop to a moderate or lower range of severity during five-years of follow-up (50.4%) and that marked improvement is rare after three years of severe illness. The only unique predictor of a more chronically severe course was patient report of ever having been housebound for a week or more due to OCD symptoms (p < .05).
Conclusion
Findings of this study were threefold: 1) half of participants with severe OCD have symptom improvement over five years of follow-up, 2) the majority of participants that drop-out of the severe range of symptom severity do so within the first three years of follow-up, and 3) patient-reported history of being housebound for one week or more due to OCD is a significant predictor of remaining severe over the five-year follow-up.
Obsessive-compulsive disorder (OCD) is chronic and debilitating1–3. While well-established, efficacious treatments have been identified for OCD – most notably exposure/response prevention (ERP) and serotonin reuptake inhibitors (SRIs) – there remains a minority of OCD patients who do not benefit from available approaches. Such treatment-refractory cases can be particularly challenging when combined with very severe symptoms. Unfortunately, little data is available to inform clinical expectations about course and prognosis of severe OCD.
For patients with severe and intractable OCD – those with severe OCD who do not show improvement with standard first- and second-line treatment approaches – neurosurgical interventions such as lesion procedures and deep brain stimulation are sometimes considered. Due to the highly invasive nature of these procedures and the availability of highly effective non-invasive treatments, these procedures are only considered for patients with severe and intractable OCD. While these invasive procedures have been used for severe OCD for decades, data guiding clinicians in identifying ideal candidates remain limited. This is, in part, a circular problem. Eligibility criteria are stringent in order to prevent patients who may benefit from less invasive approaches from unnecessarily assuming the risks of these invasive procedures. These criteria include minimum thresholds for symptom severity, functional impairment, chronicity, and treatment approaches tried without substantial benefit. Keeping eligibility criteria conservative, however, results in a very small pool of patients who receive such procedures, which in turn limits data available to identify ideal candidates for these interventions and refine eligibility criteria. As a result, many existing eligibility criteria are based on expert consensus and have not been empirically validated.
One such criterion for eligibility for many of these procedures is that severe OCD persist for a minimum of five years. While data suggest that OCD is often chronic4–6, there is little information to guide clinicians in determining when a patient’s severe OCD is unlikely to improve. Similarly limited is empirical data to aid clinicians in predicting which patients are likely to remain severe over time. Treatment-refractory OCD has been associated with a more chronic course, more functional impairment, greater severity, lower socioeconomic status, presence of religious/sexual obsessions, and greater family accommodation7. However, to our knowledge, there is no longitudinal data to suggest which factors may predict a more severe course of the disorder for those with treatment-refractory OCD.
Studies in broader OCD samples suggest several variables which may be related to course of OCD. Greater functional impairment predicts lower probability of remission6,8, earlier age of onset6,9 relates to more chronic course, and longer duration predicts lower probability of remission4. Greater symptom severity has also been linked to lower probability of remission4,9. Specific comorbidities have been associated with worse course of OCD, though number of Axis I comorbidities does not predict course4,9. Comorbid major depressive disorder (MDD) has been associated with worse course8,10 and has been found to predict poor treatment response by some11–13, though not by others14–16. Features of obsessive-compulsive personality disorder (OCPD) have been tied to worse outcomes17, greater probability of relapse following remission of OCD4, and poorer response to behavior therapy for OCD18. However, others have found no impact of OCPD on outcomes8,19,20. Nevertheless, it remains unclear whether any of these correlates of outcome in OCD samples with broad ranges of severity differentiate between those with severe OCD who will improve and those who will face a more refractory course of severe symptoms.
The primary goal of this study is to examine the course of severe OCD in a longitudinal sample over five years to inform both refinement of neurosurgical criteria as well as clinical evaluation of prognosis for severe OCD. Using Cox proportional hazard regression, we sought to answer the following questions: (1) How long must a patient’s OCD remain severe before we can be reasonably certain that it will not remit? (2) Can we identify variables which will increase our ability to predict who is likely to remain severe over the five years? We hypothesized that measures of OCD severity, past and current functioning, cognitive behavior therapy (CBT) and medication use, age of OCD onset, and comorbid depression and OCPD at baseline would be meaningful predictors of remaining severe over the five years.
Methods
Participants
Our sample was a selected subset of adults participating in the Brown Longitudinal Obsessive-Compulsive Study (BLOCS5, primary outcomes of which have been published elsewhere4,9. For complete inclusion and exclusion criteria for the BLOCS, see Pinto, et al.5). Briefly, all adult participants were age 19 or older, had a primary diagnosis of DSM-IV OCD (defined as the disorder that participants considered their biggest problem overall across their lifetime), and had sought treatment for OCD within the five years prior to study entry. The only exclusion criterion was the presence of an organic mental disorder. Participants were recruited from a range of psychiatric treatment settings in Southeastern Massachusetts and Rhode Island. The study was approved by the Institutional Review Boards of Butler Hospital and Brown University.
For inclusion in the present analysis, all participants had OCD rated as “severe” or worse at baseline assessment and had at least 1 year of follow-up data. This represents approximately a third of the total adult BLOCS sample (n=113; 34.8%). The resulting subset was 54.0% female, 95.6% Caucasian, with a mean age of 38.5 years.
Measures
The Longitudinal Interval Follow-Up Evaluation (LIFE) is a semi-structured instrument designed to assess longitudinal course of Axis I disorders21. The LIFE generates a six-point OCD psychiatric status rating (PSR) based on OCD symptom severity, indicating whether participants meet criteria for OCD (at a moderate (PSR 4), severe (PSR 5), or extreme (PSR 6) level of distress and impairment), or are in partial (PSR 3) or full remission (PSR 2, PSR 1). PSRs are reliable and valid measures of symptom severity frequently used in longitudinal studies22, 23. Reliability and validity of the LIFE are reported elsewhere22. The LIFE was administered at baseline and annual follow-ups to assess severity of Axis I disorders, including OCD.
The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) – a 10-item, gold-standard, rater-administered severity scale – was administered at baseline to assess OCD severity24, 25. The OCD Database, semi-structured clinical interview developed to collect detailed demographic and clinical information, was used to assess age at OCD symptom onset, treatments received, and OCD-related functioning, including whether participants were ever housebound due to OCD for one week or more due to OCD symptoms26. The Global Assessment of Functioning (GAF), an evaluator-rated measure, was used to assess of overall functioning in the worst week over the past month27. A modified version of the Psychosocial Treatment Inventory was used to assess baseline patient report of CBT treatment received28. The Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I) and Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) were administered at baseline to establish baseline Axis I and II diagnoses29,30.
Procedures
Weekly OCD PSRs from the LIFE were used for each subject from study entry to five years (260 weeks). The dependent variable was whether a participant’s OCD remained in the severe range (PSR of 5 or greater). A patient was considered to have “dropped out” of the severe range if symptoms improved to a PSR of 4 (i.e., moderate) or lower for at least eight consecutive weeks. Using Cox proportional hazard models we first fit an unconditional model to examine the general pattern of course in the severe group. Next, we tested a model with potential predictors of chronically severe course, given severe OCD at baseline. Univariate analyses were first conducted to screen potential predictors for inclusion in the final prediction model, (see Collett31), and all predictors with a p-value of < .20 were included in the prediction model. Variables evaluated for inclusion in this model were selected based on both related literature and clinical experience, given the limited nature of literature focusing on severe OCD. Categorical predictors were evaluated using descriptive Kaplan-Meier curves and the log-rank test of equality across strata. Continuous predictors were evaluated for inclusion using Cox proportional hazard regression.
Results
Descriptive Analysis
An unconditional descriptive model was used to determine the likelihood that someone with severe OCD will drop out of the severe range over the five years and describe the pattern of patients with severe OCD at baseline leaving the severe range over time. This study included right- but not left-censored data and data coverage was acceptable (see Figure 1). 50.4% of the sample (n=57) dropped out of the severe range for eight weeks or more over the five years. Examination of the corresponding survival curve indicated the majority of these improvements occurred within the first two to three years, with a more gradual rate thereafter (Figure 1).
Figure 1.
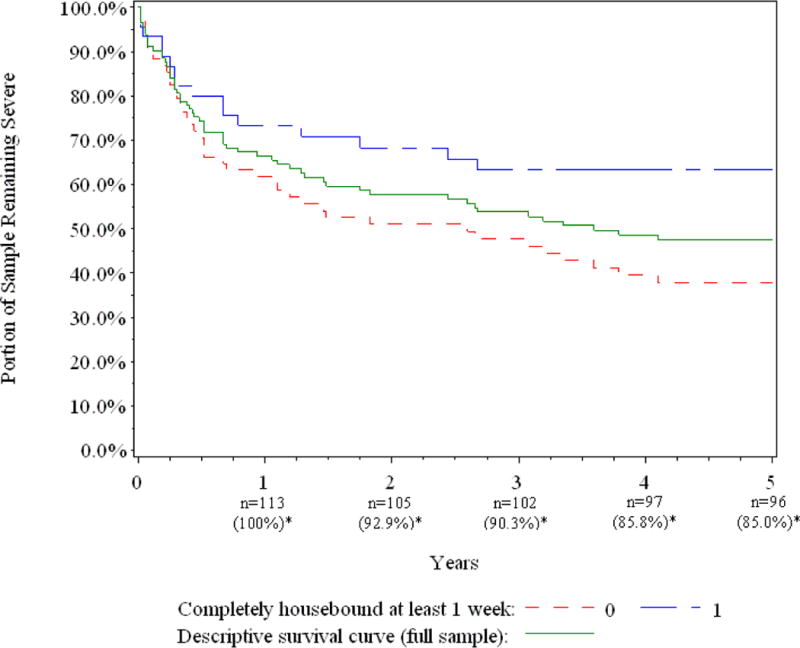
Survival Curves for Full Sample and “Houseboundedness”
*Sample sizes and percent at each year reflect the full sample; they do not necessarily reflect accurate values for the univariate or multivariate models. Censored data are not explicitly represented.
Prediction Model
To identify baseline predictors of whether or not a patient will drop from the severe range over five years, we used a Cox proportional hazard regression model. Variables considered for inclusion in the prediction model included: baseline symptom severity (Y-BOCS), age of onset of major OCD symptoms, clinician-rated baseline level of functioning (GAF), patient report of past severe functional impairment (whether or not patient had ever been housebound for a week or more due to OCD; Housebound) prior to baseline, OCPD as assessed by the SCID-II, current MDD at baseline (current MDD), patient report of lifetime number of CBT sessions at baseline (lifetime CBT sessions), patient report of trial of weekly CBT (minimum 13 sessions offered one to two times per week in single treatment episode) prior to baseline (weekly CBT trial), and total duration of psychotropic medication use at baseline (medication duration; see Table 1 for descriptive statistics). Five predictors met criteria for inclusion in the prediction model: Y-BOCS (χ2=4.07, p=.044), GAF (χ2=5.12, p=.024), Housebound (χ2=4.99, p=.026), lifetime CBT sessions (χ2=1.65, p=.199), and OCPD (χ2=3.48, p=.06). Age of onset (χ2=.19, p=.66), current MDD (χ2=0.95, p=.33), weekly CBT trial (χ2=.32, p=.57) and medication duration (χ2=.05, p=.82) did not meet criteria for entry into the final model.
Table 1.
Descriptive statistics for predictors
| Baseline Predictor | Mean (sd) or % (n) |
|---|---|
| Y-BOCS | 27.5 (3.97) |
| Age of Onset | 17.1 (8.76) |
| GAF | 41.3 (6.48) |
| Lifetime CBT Sessions | 19.31 (34.93) |
| Psychotropic Medication Duration (Years) | 9.16 (8.26) |
| Housebound | 39.8% (45) |
| OCPD | 36.3% (41) |
| Current MDD | 30.1% (34) |
| Weekly CBT Trial | 18.6% (21) |
Results of the prediction model are presented in Table 2. This model only included 106 of the total 113 participants as seven participants had missing baseline data on one or more predictors. Tests for violations of the assumption of proportionality were nonsignificant. Only one predictor in the model uniquely predicted greater relative risk of remaining in the severe range over the five years: patient report of whether they had ever been housebound for a week or more due to OCD (p=.019; Figure 1). The hazard ratio indicated that patients who reported never being housebound for a week or more due to OCD were more than twice as likely as those who had been housebound to drop out of the severe range (assuming all other variables are constant).
Table 2.
Results of Proportional Hazards Regression Model
| Baseline Predictor | B (SE) | X2 | p-value | Hazard Ratio | 95% Confidence Interval* |
|---|---|---|---|---|---|
| Housebound | −0.79 (0.34) | 5.47 | 0.019 | 0.46 | 0.24–0.88 |
| OCD Severity (Y-BOCS) | −0.08 (0.04) | 3.65 | 0.056 | 0.93 | 0.86–1.00 |
| Lifetime CBT Sessions | −.005 (.005) | 0.82 | 0.366 | 1.00 | 0.99–1.01 |
| Functioning (GAF) | 0.04 (0.03) | 2.74 | 0.098 | 1.05 | 0.99–1.10 |
| OCPD Diagnosis | −0.55 (0.31) | 3.09 | 0.079 | 0.58 | 0.31–1.07 |
Wald’s confidence limits
Discussion
This study provides the first examination of predictors of five-year course in a prospective, longitudinal investigation of severe OCD. The main findings of the study were threefold: 1) half of participants with severe OCD experience noteworthy symptom improvement over five-year follow-up, with symptoms decreasing to or below the moderate range for a minimum of eight weeks, 2) the majority of participants that drop-out of the severe range do so within the first three years, and 3) history of being housebound for one week or more due to OCD is a more relevant predictor of remaining severe than traditional measures of symptom severity, global functioning, and comorbidity. This suggests that in addition to current levels of severity and functioning, more distal factors may have important predictive utility.
Results from this study suggest that approximately half who present with severe OCD remain chronically severe over five years of follow-up, consistent with the chronicity and persistent significant impairment reported with this disorder6. Importantly, however, 50% of our participants did improve to at least the moderate range during the course of the study, with the majority (89%) occurring during the first three years of evaluation. Indeed, 82% of participants that dropped out of the severe range did so within the first two years of observation, and another 7% between years two and three. This suggests that the likelihood of improvement to a moderate symptom level is rare for individuals with OCD who have been consistently severely ill for three years or more. This highlights a potential need to reconsider our treatment strategies for individuals with severe OCD. Surgery criteria requiring five years of severe symptoms may be on the whole too stringent.
Although research frequently highlights the influence of comorbid disorders on OCD prognosis, neither MDD nor OCPD were significant predictors of a chronic severe course. In contrast to our results, a recent, 15-year naturalistic prospective study of anxiety disorders found that OCD participants with comorbid MDD were significantly less likely to remit from OCD than those without MDD10. Differences between these studies may help reconcile the discrepancy. The impact of MDD on course may be less pronounced in the current investigation, as all participants were severely ill compared to Marcks and colleagues10 which had no lower bound on OCD severity. Individuals with comorbid MDD may present with more severe OCD symptoms32,33, making symptom improvement less likely. Alternatively, depression may influence OCD treatment. Although early studies found that comorbid MDD had a deleterious effect on OCD treatment outcome11–13, our lack of significant finding regarding MDD is consistent with more recent treatment studies finding no relationship between depression and OCD treatment response34. The role of MDD in the treatment of OCD remains an area for future exploration.
While a connection between OCPD and OCD is well-established, few studies have investigated the influence of OCPD on OCD course. Comorbid OCPD approached significance in both the univariate and final model (ps = .06 and .08, respectively), providing measured support for future investigations into the potential impact of OCPD on severe OCD course. Notably, in our larger sample of individuals with primary OCD4, while OCPD did not emerge as a significant predictor of remission, it did predict relapse. Though our sample size here did not allow for the examination of predictors of subsequent worsening following improvement in a severe sample, future research should clarify if OCPD also differentiates between those with severe OCD who are unable to sustain improvement and those that remain improved.
Consistent with prior research with more broadly defined samples, baseline OCD severity and global functioning were significant univariate predictors of OCD course4,6. However, neither of these variables remained significant in the presence of houseboundedness. Patient report of ever being housebound due to OCD for one week or more was the only significant predictor of leaving the severe range during the five-year period in our prediction model. This finding, if replicated, has significant implications for both assessment and treatment of OCD. It suggests the need to not only consider current severity and overall functioning, but also the utility of assessing past or worst-ever functioning. Nearly 40% of our severe sample reported a history of being housebound for one week or more due to OCD symptoms, highlighting the frequency of what is arguably a marker of extreme functional impairment. The reasons a patient with OCD may become housebound should also be investigated in future work. Past houseboundedness may indicate a tendency to engage in extreme avoidance strategies or high levels of illness accommodation by family members. Assessment of these factors may be informative above and beyond a history of being housebound. If our finding is confirmed in other work, asking about houseboundedness due to OCD may be a useful addition to the duration criteria in refining criteria for neurosurgical interventions.
Beyond the implications for neurosurgical entry criteria, candidates for which are few35, these findings also have important implications for treatment planning for OCD patients more broadly. Clinicians who assess for a history of impairment significant enough to result in houseboundedness will quickly learn a key predictor of prognosis which may allow them to plan treatment more appropriately and aggressively. For example, a clinician may wish to plan (or refer) for an intensive course of ERP, schedule more frequent medication follow-ups, and perhaps recommend case management or involve social workers in the treatment to ensure a focus not only on symptoms, but also on functioning and management of activities of daily living.
Limitations of this investigation also warrant consideration. First, participants were all treatment-seeking and predominantly Caucasian, limiting generalizability. Second, because of the naturalistic study design, treatments were not controlled, precluding examination of treatment effects on severe OCD course. Relatedly, while this design allowed thorough characterization of the sample during the study, we cannot say how long patients experienced severe OCD prior to enrollment. This is an important caveat and a reason these findings should be confirmed in other samples. Third, we examined only a limited number of predictors in the present study. While we included those predictors we believed to be the best candidates, additional predictors should be examined in future work (e.g., family accommodation). Moreover, use of a priori power analyses in future studies will ensure adequate power, as survival analyses often require large samples to be adequately powered. It is possible that with a larger sample in the present study other predictors may have reached statistical significance. Fourth, although the LIFE is a well-validated and frequently used measure of longitudinal course22,36,37, PSRs lack the precision of other symptom rating scales, making the distinction between moderate and severe OCD a broad one. A related point is that the definition of symptom improvement used here and in other BLOCS publications (i.e., eight consecutive weeks) was selected to reflect a clinically meaningful time period of symptom change, but does not formally reflect DSM, nor does it imply that all individuals who improved remained improved indefinitely. In this study, 50.9% of the subsample who dropped from the severe range did re-enter the severe range for at least one week during the remainder of the five year period. However, the majority of those who experienced a return to the severe range following symptom improvement did not remain “chronically” severe: This group (n=29) spent an average of only 26% of their remaining weeks in the severe range (from the week of their initial drop below the severe range), and only four of the 29 spent more than half of their remaining weeks in the severe range. Finally, data on age of onset, past functional impairment, and symptoms over the follow-up intervals were retrospective and therefore subject to memory bias. However, this study represents one of the few prospective investigations of OCD and, to our knowledge, the first to examine course of severe OCD.
In summary, this study examined course and prospective predictors of a chronic course in severe OCD. Our results suggest that marked improvement is rare after three years of severe illness. Nevertheless, half of those with severe OCD do, in fact, remit to a moderate symptom level. History of being housebound for a week or more due to OCD was the single strongest predictor of remaining severe throughout the five years. These findings highlight the need to consider more basic markers of functional impairment and history of functional impairment.
Clinical Points.
Little data has been available to inform clinical expectations about course and prognosis of severe OCD.
In this study, half of patients with severe OCD at baseline improved to a moderate, or lower, level of severity over the course of five years.
Assessment of past functioning, particularly whether someone has ever been housebound for a week or more due to OCD, may be useful in determining prognosis for patients with severe OCD.
Acknowledgments
Financial support for the project came from a grant from the National Institute of Mental Health R01MH060218. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
None of the authors has any financial conflicts of interest to disclose.
Portions of these data were presented at the International Obsessive-Compulsive Disorder Foundation 2013 annual conference.
References
- 1.Huppert JD, Simpson HB, Nissenson KJ, Liebowitz MR, Foa EB. Quality of life and functional impairment in obsessive-compulsive disorder: a comparison of patients with and without comorbidity, patients in remission, and healthy controls. Depress Anxiety. 2009;26:39–45. doi: 10.1002/da.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eisen JL, Mancebo MA, Pinto A, et al. Impact of obsessive-compulsive disorder on quality of life. Compr Psychiatry. 2006;47:270–275. doi: 10.1016/j.comppsych.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bystritsky A, Liberman RP, Hwang S, et al. Social functioning and quality of life comparisons between obsessive-compulsive and schizophrenic disorders. Depress Anxiety. 2001;14:214–218. doi: 10.1002/da.1069. [DOI] [PubMed] [Google Scholar]
- 4.Eisen JL, Sibrava NJ, Boisseau CL, et al. Five-year course of obsessive-compulsive disorder: predictors of remission and relapse. J Clin Psychiatry. 2013;74:233–239. doi: 10.4088/JCP.12m07657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA. The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. J Clin Psychiatry. 2006;67:703–711. doi: 10.4088/jcp.v67n0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skoog G, Skoog I. A 40-year follow-up of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56:121–127. doi: 10.1001/archpsyc.56.2.121. [DOI] [PubMed] [Google Scholar]
- 7.Ferrao YA, Shavitt RG, Bedin NR, et al. Clinical features associated to refractory obsessive-compulsive disorder. J Affect Disord. 2006;94:199–209. doi: 10.1016/j.jad.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 8.Steketee G, Eisen J, Dyck I, Warshaw M, Rasmussen S. Predictors of course in obsessive-compulsive disorder. Psychiatry Res. 1999;89:230–238. doi: 10.1016/s0165-1781(99)00104-3. [DOI] [PubMed] [Google Scholar]
- 9.Eisen JL, Pinto A, Mancebo MC, Dyck IR, Orlando ME, Rasmussen SA. A 2-year prospective follow-up study of the course of obsessive-compulsive disorder. J Clin Psychiatry. 2010;71:1033–1039. doi: 10.4088/JCP.08m04806blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marcks BA, Weisberg RB, Dyck I, Keller MB. Longitudinal course of obsessive-compulsive disorder in patients with anxiety disorders: a 15-year prospective follow-up study. Compr Psychiatry. 2011;52:670–677. doi: 10.1016/j.comppsych.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cottraux J, Mollard E, Bouvard M, Marks I. Exposure therapy, fluvoxamine, or combination treatment in obsessive-compulsive disorder: one-year followup. Psychiatry Res. 1993;49:63–75. doi: 10.1016/0165-1781(93)90030-k. [DOI] [PubMed] [Google Scholar]
- 12.Foa EB. Failure in treating obsessive-compulsives. Behav Res Ther. 1979;17:169–176. doi: 10.1016/0005-7967(79)90031-7. [DOI] [PubMed] [Google Scholar]
- 13.Foa EB, Grayson JB, Steketee GS, Doppelt HG, Turner RM, Latimer PR. Success and failure in the behavioral treatment of obsessive-compulsives. J Consult Clin Psychol. 1983;51:287–307. doi: 10.1037//0022-006x.51.2.287. [DOI] [PubMed] [Google Scholar]
- 14.Basoglu M, Lax T, Kasvikis Y, Marcks YM. Predictors of improvement in obsessive-compulsive disorder. J Anxiety Disord. 1988;2:309–317. [Google Scholar]
- 15.Abramowitz J, Foa EB. Does Comorbid Major Depressive Disorder Influence Outcome of Exposure and Response Prevention for OCD? Behavior therapy. 2000;31:795–800. [Google Scholar]
- 16.Foa EB, Kozak MJ, Steketee GS, McCarthy PR. Treatment of depressive and obsessive-compulsive symptoms in OCD by imipramine and behaviour therapy. Br J Clin Psychol. 1992;31(Pt 3):279–302. doi: 10.1111/j.2044-8260.1992.tb00995.x. [DOI] [PubMed] [Google Scholar]
- 17.Cavedini P, Erzegovesi S, Ronchi P, Bellodi L. Predictive value of obsessive-compulsive personality disorder in antiobsessional pharmacological treatment. Eur Neuropsychopharmacol. 1997;7:45–49. doi: 10.1016/s0924-977x(96)00382-3. [DOI] [PubMed] [Google Scholar]
- 18.Pinto A, Liebowitz MR, Foa EB, Simpson HB. Obsessive compulsive personality disorder as a predictor of exposure and ritual prevention outcome for obsessive compulsive disorder. Behav Res Ther. 2011;49:453–458. doi: 10.1016/j.brat.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castle DJ, Deale A, Marks IM, Cutts F, Chadhoury Y, Stewart A. Obsessive-compulsive disorder: prediction of outcome from behavioural psychotherapy. Acta Psychiatr Scand. 1994;89:393–398. doi: 10.1111/j.1600-0447.1994.tb01535.x. [DOI] [PubMed] [Google Scholar]
- 20.Orloff LM, Battle MA, Baer L, et al. Long-term follow-up of 85 patients with obsessive-compulsive disorder. AJ Psychiatry. 1994;151:441–442. doi: 10.1176/ajp.151.3.441. [DOI] [PubMed] [Google Scholar]
- 21.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 22.Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 23.Skodol AE, Pagano ME, Bender DS, et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med. 2005;35:443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 25.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- 26.Rasmussen SA. Genetic studies of obsessive-compulsive disorder. Ann Clin Psychiatry. 1993;5:241–247. doi: 10.3109/10401239309148823. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association., American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 28.Steketee G, Perry JC, Goisman RM, et al. The psychosocial treatments interview for anxiety disorders: a method for assessing psychotherapeutic procedures in anxiety disorders. J Psychother Pract Res. 1997;6:194–210. [PMC free article] [PubMed] [Google Scholar]
- 29.First M, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) Washington, D.C: American Psychiatric Press, Inc; 1997. [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) Washington, D.C: American Psychiatric Press, Inc; 1996. [Google Scholar]
- 31.Collett D. Modeling survival data in medical research. London, UK: Chapman and Hall; 1994. [Google Scholar]
- 32.Besiroglu L, Uguz F, Saglam M, Agargun MY, Cilli AS. Factors associated with major depressive disorder occurring after the onset of obsessive-compulsive disorder. J Affect Disord. 2007;102:73–79. doi: 10.1016/j.jad.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Hong JP, Samuels J, Bienvenu OJ, 3rd, et al. Clinical correlates of recurrent major depression in obsessive-compulsive disorder. Depress Anxiety. 2004;20:86–91. doi: 10.1002/da.20024. [DOI] [PubMed] [Google Scholar]
- 34.Anholt GE, Aderka IM, van Balkom AJ, et al. The impact of depression on the treatment of obsessive-compulsive disorder: results from a 5-year follow-up. J Affect Disord. 2011;135:201–207. doi: 10.1016/j.jad.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 35.Garnaat SL, Greenberg BD, Sibrava NJ, et al. Who qualifies for deep brain stimulation for OCD? Data from a naturalistic clinical sample. J Neuropsychiatry Clin Neurosci. 2014;26:81–86. doi: 10.1176/appi.neuropsych.12090226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Solomon DA, Keller MB, Leon AC, et al. Recovery from major depression. A 10-year prospective follow-up across multiple episodes. Arch Gen Psychiatry. 1997;54:1001–1006. doi: 10.1001/archpsyc.1997.01830230033005. [DOI] [PubMed] [Google Scholar]
- 37.Gunderson JG, Daversa MT, Grilo CM, et al. Predictors of 2-year outcome for patients with borderline personality disorder. AJ Psychiatry. 2006;163:822–826. doi: 10.1176/ajp.2006.163.5.822. [DOI] [PubMed] [Google Scholar]


