Abstract
The 2014 i2b2/UTHealth Natural Language Processing (NLP) shared task featured four tracks. The first of these was the de-identification track focused on identifying protected health information (PHI) in longitudinal clinical narratives. The longitudinal nature of clinical narratives calls particular attention to details of information that, while benign on their own in separate records, can lead to identification of patients in combination in longitudinal records. Accordingly, the 2014 de-identification track addressed a broader set of entities and PHI than covered by the Health Insurance Portability and Accountability Act – the focus of the de-identification shared task that was organized in 2006. Ten teams tackled the 2014 de-identification task and submitted 22 system outputs for evaluation. Each team was evaluated on their best performing system output. Three of the 10 systems achieved F1 scores over .90, and seven of the top 10 scored over .75. The most successful systems combined conditional random fields and hand-written rules. Our findings indicate that automated systems can be very effective for this task, but that de-identification is not yet a solved problem.
Graphical abstract
1. Introduction
The 2014 i2b21/UTHealth2 Natural Language Processing (NLP) shared task featured four tracks. The first of these was the de-identification track focused on identifying protected health information (PHI) in the clinical narratives. While identifying PHI for removal, it is important for de-identification to preserve the medically salient contents of the narratives so that this information can benefit downstream research and maintain the value of the record for the care of the patients.
The 2014 shared task data were selected to show the progression (or lack thereof) of heart disease in diabetic patients over time, the focus of Track 2 of the i2b2/UTHealth shared task (Stubbs et al, this issue). In order to reflect the progression over time, the records were longitudinal: the same patients were represented over multiple documents separated by weeks, months, or years. The inclusion of longitudinal records in a corpus presents a unique challenge for de-identification: Including more records from a patient's medical record provides important medical data for clinical research, but it also potentially puts the patient at greater risk of being identified.
America's Health Insurance Portability Accountability Act (HIPAA; 45 CFR 164.514) defines 18 categories of PHI, which must be removed from a medical record before it can be considered safely de-identified. These categories include patient names, contact information, ID numbers, and so on. However, a recent study in Canada showed that over an 11-year period, records of people's addresses alone could lead to their being identified (El Emam et al., 2011). Similarly, US citizens can be identified by their date of birth, ZIP code, and gender (Golle, 2006; Sweeney, 2000), yet the HIPAA PHI categories do not include gender, years, or full ZIP codes for sufficiently populated areas. In other words, while HIPAA provides a starting point for effective de-identification, it may not be sufficient for full de-identification.
While full de-identification may not be a realistic and attainable goal, expanding HIPAA categories to include a wider set of information can make de-identification more secure. Accordingly, the 2014 i2b2/UTHealth shared task data were de-identified to a more strict standard than what HIPAA defines (Stubbs and Uzuner, this issue; Stubbs et al., forthcoming), using additional categories for PHI, such as professions, full dates, and information about medical workers and facilities. We refer to this expanded set of PHI categories as i2b2-PHI categories (see Section 3).
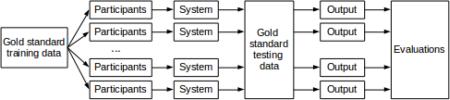
We defined the Track 1 shared task consistently with the de-identification that we performed for data release. We released 60% of the de-identified data, with the gold standard i2b2-PHI annotations (but after the authentic PHI were replaced with realistic surrogates) as the training corpus. We gave the participants three months to build systems that automated the de-identification task. At this point, we released the remaining data, without annotations, as test data, and gave the participants three days to submit up to three system runs on the test data. We evaluated the system runs on two sets of PHI categories: the 18 categories defined by HIPAA (HIPAA-PHI) and the i2b2-PHI. We ranked the systems primarily based on their performance on the i2b2-PHI.
This paper provides a brief overview of the de-identification task (Track 1) of the i2b2/UTHealth 2014 shared task, related work (Section 2), data (Section 3) and annotation (Section 4). Its focus is primarily on the evaluation metrics (Section 5), descriptions of participating systems (Section 6) and results of the shared task. To put this task into context, we compare these results to the results of the 2006 i2b2 de-identification task (Section 7) and close the paper with a discussion and conclusions (Sections 8 and 9).
2 Related work
There have been many shared tasks in NLP, but few are comparable to the 2014 de-identification task described here. Traditional named entity recognition (NER) is similar to de-identification, as the focus for both tasks is to identify information such as names, dates, and locations in texts. However, de-identification of medical records includes more categories of information than traditional NER, such as phone numbers, ID numbers, and ages. The 6th and 7th Message Understanding Conferences (MUCs) included shared tasks in NER. Specifically, the participants were asked to label entities (organizations, persons, locations), numbers (currencies and percentages), and temporal expressions (specific dates and times) (Sundheim, 1995; Chinchor, 1997). The MUC-6 NER task participants included 20 systems from 15 teams, and 96.42 as the highest f-measure (Sundheim, 1995). MUC-7 had 14 systems from 12 teams, with a top f-measure of 93.39 (Chinchor, 2001). However, both of the MUC tasks were run on newswire texts, rather than clinical notes, making a direct comparison to the 2014 i2b2/UTHealth de-identification challenge untenable.
NER-type shared tasks in the biomedical domain tend to focus on identifying information related to the field, rather than traditional named entities. BioCreAtIvE (Hirschman et al., 2005) participants identified and mapped gene and protein names, and the TREC Genomics tracks also focused on genes and diseases when looking for particular entities (Hersh and Vorhees, 2009). The BioNLP'09 (Kim et al., 2009) focused on protein and gene event extraction, which the BioNLP'11 (Pyysalo et al., 2012) and BioNLP'13 (Nédellec et al., 2013) tasks expanded upon. Each of these shared tasks used text from MEDLINE. Other biomedical shared tasks include the BioASQ tasks, which use data from PubMed (BioASQ, 2015).
To the best of our knowledge, the only other de-identification shared task made open to the public is the previous i2b2 event, held in 2006 (Uzuner et al., 2007). The 2006 task used 889 de-identified records, one record per patient, and fielded sixteen submissions from seven teams. The 2006 data used individual records for each patient. As we noted in the Introduction, longitudinal records may contain much more personal information about a patient than individual records. And this information, while perfectly HIPAA-compliant and ineffective for identifying the patient when found in individual records and on their own, can be used collectively to piece together the identity of the patient over several records. This makes de-identification of longitudinal records a potentially more intricate task.
2.1 De-identification tools
In order to provide context for comparing the i2b2 participants with other recently developed de-identification systems, here we discuss three recent systems and their results. A broader overview of de-id systems can be found in the recent review article by Meystre et al (2010), in which the authors describe 18 de-identification systems built between 1995 and 2010. Here, we focus on three recent tools: MIST, the MITRE Identification Scrubber Toolkit (Aberdeen et al., 2010), BoB, the “best of breed” tool from the Veteran's Health Administration (Ferrández et al., 2012), and an in-house tool from Cincinnati Children's Hospital Medical Center (Delager et al., 2014).
MITRE's MIST tool (Aberdeen et al., 2010) is an open source de-identification system that also includes annotation and PHI replacement tools. The parts of the system that identify PHI use the Carafe engine (Wellner, 2009), a system that uses a Conditional Random Field (CRF) (Lafferty et al., 2001) model trained specifically for text processing. The Carafe engine is the only system used in MIST: it does not implement rules, though in the conclusions the authors note that some types of PHI may be better captured through rules. When run on the 2006 i2b2 data, MIST achieved precision of 0.978, recall of 0.951, and F1 of 0.965.
The VHA's BoB (Ferrández et al., 2012) is built on the Apache UIMA architecture (Apache, 2008) and uses cTAKES (Savova et al., 2010) to pre-process the documents. The system then uses a “stepwise hybrid” approach to removing PHI. In the first step, a “high sensitivity extraction component”, uses rules and a CRF model to identify all possible PHI in a document. In the second step, a “false positives filtering component” uses Support Vector Machine (SVM) (Boser et al, 1992) classifiers to remove inaccurate PHI tags generated in the first step. When tested against the 2006 i2b2 corpus, and implementing special rules to account for the differences in annotations, BoB achieved precision, recall, and F1 of 0.846, 0.965, and 0.902, respectively.
The Cincinnati Children's Hospital Medical Center's (CCHMC) in-house de-identification system (Delager et al., 2012) is based on the MALLET package (McCallum, 2002), which also uses CRF models. The CCHMC system also utilizes pre-processing in the form of an in-house and the TreeTagger3 part of speech processor, and post-processing in the form of rules that identify email addresses, match names to an external lexicon, and capture any names that the CRF module missed. When tested on the 2006 i2b2 corpus, with training data from other corpora, the system achieved precision, recall, and F1 of 0.9682, 0.9342, and 0.9509, respectively (Delager et al, 2014).
Overall, these systems perform quite well, and set a high standard for further research in de-identification. Many differences in the scores can be attributed to differences in training data, as each group had access to data that was unavailable to the others at the time.
3. Data
The data for this task are a newly de-identified corpus of longitudinal medical records, drawn from the Research Patient Data Repository of Partners Healthcare (Kumar et al., this issue). This corpus was used for all the tracks of the 2014 i2b2/UTHealth shared task. It consists of 1,304 medical records for 296 diabetic patients. All PHI in these records have been removed (Stubbs and Uzuner, this issue; Stubbs and Uzuner, forthcoming) and replaced with realistic surrogates (Stubbs et al., forthcoming). This shared task was open to all interested researchers from any country, and was announced on various mailing lists in the NLP community, as well as a mailing list of past i2b2 shared task participants. We released approximately two thirds of the training data in May 2014, and released the remaining third in June. In early July we released the test data, at which time participants were asked to stop developing their systems, and they were given three days to submit up to three system runs on the test data. The corpus was distributed to the shared task participants under a data use agreement and will be available to the rest of the community for research from https://www.i2b2.org/NLP/ in November 2015. Institutional review boards at Partners Healthcare, MIT, and SUNY Albany approved this study.
4. Annotation
As we described in the Introduction, due to the longitudinal nature of our data, we were aware that small amounts of information about the patients that would not be considered PHI under HIPAA could be pieced together to reveal a person's identity. Therefore, to ensure the patients’ protection as much as possible, we used HIPAA-PHI categories as our starting point, augmented and added sub-categories, and created the following i2b2-PHI categories with their “type” attributes:
NAME (types: PATIENT, DOCTOR, USERNAME)
PROFESSION
LOCATION (types: ROOM, DEPARTMENT, HOSPITAL, ORGANIZATION, STREET, CITY, STATE, COUNTRY, ZIP, OTHER)
AGE
DATE
CONTACT (types: PHONE, FAX, EMAIL, URL, IPADDRESS)
IDs (types: SOCIAL SECURITY NUMBER, MEDICAL RECORD NUMBER, HEALTH PLAN NUMBER, ACCOUNT NUMBER, LICENSE NUMBER, VEHICLE ID, DEVICE ID, BIOMETRIC ID, ID NUMBER)
Of these i2b2-PHI categories, only the following correspond to the HIPAA-PHI categories: NAME-PATIENT, LOCATION-STREET, LOCATION-CITY, LOCATION-ZIP, LOCATION-ORANIZATION, AGE, DATE, all ID sub-categories as well as CONTACT-PHONE, CONTACT-FAX, CONTACT-EMAIL
Given these PHI categories and types, we annotated the information in each record twice, and implemented a series of automatic and manual checks to ensure that all authentic PHI were annotated. We replaced all annotated authentic PHI with realistic surrogates, and re-checked the records for readability (Stubbs and Uzuner, this issue). We used these annotated data as the source of the training and testing data released to the participants, and as the gold standard against which we evaluated the system outputs, as we describe in the next section.
5. Evaluation
We used precision (Eq. 1), recall (Eq. 2 and F-measure (Eq. 3) scores to evaluate the participants’ results against the gold standard annotations. We checked the significance of the differences of the systems from each other using approximate randomization (Chinchor, 1992 and Noreen, 1989).
| Eq. 1 |
| Eq. 2 |
| Eq. 3 |
We calculated P, R, and F1 at both entity and token levels across the entire corpus. We used micro-averaged F1 as our primary metric. The evaluation scripts we used are freely available on GitHub: https://github.com/kotfic/i2b2_evaluation_scripts/tree/v1.2.1
Entity-based (also known as “instanced-based” (Uzuner et al., 2007)) evaluations require that system outputs match the beginning and end locations of each PHI tag exactly, as well as match the tag name and type attribute. Token-based evaluations must also match the tag's name and type attribute, but are evaluated on a per-token basis. In other words, if the gold standard has “Rayna De Angelis” annotated as NAME with type DOCTOR, and a system annotated “Rayna” and “De Angelis” as individual tags that each have NAME/DOCTOR annotations, the entity-based evaluation would not count that system's output as correct, though the token-based evaluation would. We perform both entity- and token-based evaluations because entity-based evaluations are the standard system for named entity recognition, where it is important for a phrase describing an entity to be captured whole. However, for the purposes of de-identification, it is less important for all parts of a single PHI to be identified together as long as all the parts are identified as PHI at some point. As long as “Rayna” and “De Angelis” are identified as PHI and removed from the corpus, it does not matter if that is the result of a single entity annotation or two token-based annotations.
Given these metrics, we take into consideration the differences in de-identification requirements of medical institutions for data release for our evaluations. For example, some institutions may want any possible PHI removed, while others may be only concerned with those categories specified by HIPAA. Therefore, we evaluated systems on both the i2b2-PHI and the HIPAA-PHI.
While we are concerned with the correct recognition of specific PHI categories from the perspective of preserving the integrity of the data, even in the absence of correct identification of categories of PHI, de-identification can succeed. In other words, systems can effectively remove PHI and preserve patient privacy without correctly differentiating between PHI categories. For example, a system that incorrectly identifies patient names as doctor names will still successfully remove the identified names from the records and accomplish de-identification even if it gets to that correct outcome for the wrong reasons. In order to evaluate systems purely on PHI identification without categories, we performed a binary evaluation on the recognition of PHI vs non-PHI (binary PHI categories).
As a result, we evaluated performance in the following ways: (1) micro-averaged entity- and token-based P, R, F1 on i2b2-PHI categories. This evaluation determines how well each system did compared to the gold standard. (2) micro-averaged entity- and token-based P, R, F1 on only the HIPAA-PHI categories. We perform this evaluation to determine whether a system's performance is good enough for meeting HIPAA requirements. (3) micro-averaged entity- and token-based evaluation of binary PHI categories. We perform this evaluation to check whether the records are de-identified effectively, even if for the wrong reasons. We used the micro-averaged entity-based F1 over i2b2-PHI categories as our primary ranking metric.
Table 10 in the Appendix shows, for a given ground truth, whether it would be considered correct (marked with a +) or incorrect (marked with a −) under each of our evaluation metrics. As can be seen, the token-based evaluations are the most accepting of variations in the system outputs (marked with the highest number of +s), while entity-based analyses require much stricter adherence to the gold standard in terms of matching the starting and ending offsets of every tag exactly. The most difficult task is the entity-based evaluation over the i2b2-PHI. In contrast, the binary evaluations accept any annotation that identified PHI.
We calculated statistical significance between system runs using approximate randomization as outlined in Chinchor (1992) and Noreen (1989). Significance was tested for micro-averaged P, R and F1, with N = 9,999 and an alpha of 0.1. These values are consistent with MUC-3 and MUC-4 evaluations as well as previous i2b2 challenges (Uzuner et al., 2007).
6. Submissions
Each participating team submitted up to three system outputs for evaluation to the de-identification track of the 2014 i2b2/UTHealth shared task. Overall, we received 22 submissions from 10 teams (see Table 9 in the Appendix for details on participating teams, their members and affiliations). The most popular and successful approaches among the submissions were hybrids of Conditional Random Fields (CRFs) and hand-written rules, which processed the outputs of the two different systems into a coherent whole. We present the system overviews here alphabetically by team name. Two of the teams (East China Normal University and UC San Diego) did not submit system descriptions and are accordingly omitted from this overview.
The team from Harbin Institute of Technology (He et al., this issue) pre-processed their data with the OpenNLP4 system's sentence detector and tokenizer, along with some regular expressions to tokenize irregular phrases. They then trained a CRF system on the following features: lexical, orthographic, and syntactic. Unlike most other systems, they did not use any medical dictionaries to identify key words.
The Harbin Institute of Technology Shenzhen Graduate School (Liu et al., this issue) team used three systems to generate annotations. First, a CRF based on token-level features, which used MedEx (Xu et al, 2010) for tokenization, and included features such as bag-of-words, part of speech, orthographic features, section information, and word representation features. Second, a CRF based on character-level features to extract PHI represented by characters, which used similar features to the token-level classifier, but decomposed raw sentences into characters instead of tokens. Third, a rule-based system that used regular expressions to identify standardized PHI such as PHONE, FAX, MEDICAL RECORD NUMBER, etc. They used a rule-based system to merge the outputs of the three systems: non-overlapping PHI instances were included directly in the system output; overlapping output from the three systems was resolved in a hierarchy, with preference given first to the rule-based classifier, then the character-level classifier, then the token-level classifier.
The team from Kaiser Permanente (Torii et al. (this issue)) focused on adapting the MIST tool5 for the 2014 shared task data. They added their own annotated data to the 2014 shared task training medical records and augmented the MIST tool by providing additional rules that used lexicons (for LOCATION and PROFESSION categories) and regular expressions (for PHONE, ZIP, and ORGANIZATION categories). These rules also prevented certain types of non-PHI, such as font names, from being annotated. In addition to MIST, the team also trained a NER model on the 2014 shared task data using the Stanford NER system6. Their best run then merged the outputs of MIST and Stanford NER systems by taking the longest span of overlapping outputs from them.
The LIMSI-CNRS team (Grouin (this issue)) trained a CRF with different linguistic categories of features. Surface features represented information such as the token itself, token length, typographic case, presence of punctuation or digits. For morpho-syntactic features, they used part of speech categories obtained from Tree Tagger7 They identified semantic types by using trigger words from different categories (e.g., Dr., MD, Mr., Mrs., etc), as well as a list of professions from Wikipedia. They also used distributional analysis features, such as frequency in the corpus, document section, and cluster ID based on context. They then used 77 regular expressions to correct CRF outputs by, for example, identifying multi-word expressions and multi-token sequences by comparing them to a lexicon collected from the training corpus and fixing annotation spans for AGE and DOCTOR tags. They submitted three system runs: CRF only, CRF + rules without the lexicon from the training corpus, and CRF + rules with the lexicon. Their best run used the CRF + rules with the lexicon.
The UNIMAN team from Manchester (Dehghan et al., this issue) pre-processed the input data with cTAKES8 and GATE9 for tokenization, sentence splitting, part-of-speech tagging, and chunking. They built a combined knowledge- and data-driven system for identifying PHI. The knowledge-based component used dictionaries and a small set of rules (with orthographic, pattern, negation, lexical and context features, e.g., words from specialized vocabularies, symbols, and special characters). The data-driven component used a CRF model for each of the following categories: CITY, DATE, HOSPITAL, ORGANIZATION, PROFESSION, and PATIENT. Their CRF features included lexical (lemma, part of speech for the token and surrounding words), orthographic (capitalization, digits; orthographic patterns), semantic (matched to the dictionaries of related vocabulary), and positional features (position in line, presence of space between current and next token). They also proposed a two-pass approach for some categories (PATIENT, DOCTOR, HOSPITAL, CITY, MEDICAL RECORD, and ID_NUM): for each category, they extracted the initial annotations at the patient-level and created a run-time patient-specific dictionary. This dictionary was subsequently used for ‘second-pass’ dictionary matching on the same set of patient narratives in order to capture mentions not recognized in the initial pass. Finally, an integration step merged the outputs of the rule-based and CRF modules using different sets of rules for the different system runs. The most successful merging system used rules for DATEs and DOCTORs, and rules and lexicons for PATIENTs.
The Newfoundland team (Chen (this issue)) used a non-parametric Bayesian (Orbanz and Teh, 2010) Hidden Markov Model (HMM) (Baum and Petrie, 1966). This model utilizes latent variables to organize words of the same label into more refined categories, which allows the model to capture subtle variations in the data. Instead of using a fixed number of latent variables, which makes a strong assumption of data, the model allows an infinite number of latent variables by implementing a Dirichlet process (Blei and Ng, 2003) as a prior and lets the data determine the optimum number of latent variables. The Newfoundland system implemented a Dirichlet process to identify PHI. They also implemented a set of features to identify words that did not appear in the training data.
The team from Nottingham (Yang and Garibaldi (this issue)) pre-processed the data via sentence splitting, tokenization, part of speech tagging, and shallow parsing. They then identified the following features: word-token (lemma, part of speech (POS), chunk), context (lemma, POS, chunk of nearby tokens), orthography (capitalization, punctuation, regex patterns for dates, usernames, etc.), sentence-level features (position of token in sentence, section headers), task-specific features (lists of names and acronyms of US states, countries, languages, and lexical clues such as presence of Dr. MD, etc). Their system is a hybrid one: they trained a CRF using the described features, and then used dictionaries and regular expressions to identify PHI with few sample instances. As a post-processing step, they performed entity extraction from identified PHI, and used a trusted PHI term list to uncover more potential terms. They generated the trusted PHI term list by making use of different types of relations between detected PHI terms.
The San Marcos (Guillen (this issue)) team built an entirely rule-based system. They performed an analysis of the data to determine the most frequently used tags, tokenized the texts, performed rule-based token classification based on whether the tokens were digits or non-digits, and analyzed the result to determine patterns for DATEs, AGEs, and IDs. They refined their rules with lexical clues.
Table 1 shows an overview of the different tools, rules, machine learning algorithms, features, and external resources used by these systems.
Table 1.
Overview of tools, rules, machine learning, and external resources used in systems.
| Team name | Tools | Rules and features | Machine learning systems and features | External resources |
|---|---|---|---|---|
| Harbin Institute of Technology | OpenNLP CRF++ | Regular expressions for tokenization | CRF: lexical, syntactic, orthographic | |
| Harbin Institute of Technology Shenzhen Graduate School | MedEx | Regular expressions for categories such as PHONE, FAX, MEDICAL RECORD, EMAIL and IPADDR | CRFs: bag-of-words; part-of-speech (POS) tags; combinations of tokens and POS tags; sentence information; affixes; orthographical features; word shapes; section information; dictionary features | |
| Kaiser Permanente | MIST Stanford NER | Regular expressions for categories such as PHONE, EMAIL, ZIP | MIST, Stanford NER; features not mentioned | Personal de-id corpus |
| LIMSI-CNRS | Tree Tagger MEDINA toolkit | Rules to correct output of CRF | CRF: surface features, morpo-syntactic, semantic, distributional | |
| UNIMAN | Pre-processing: CTAKES and GATE | JAPE system: orthographic, pattern, contextual, entity | CFR: lexical, orthographic, semantic, positional | Dictionaries collected from Wikipedia, GATE, and deid |
| Newfoundland | Python packages Numpy and Scipy | non-parametric Bayesian Hidden Markov Model: token, word token, number token | ||
| Nottingham | Pre-processing; CRF++ | Yes, for categories such as FAX, EMAIL, DEVICE, BIOID | CRF: Word-token, context, orthographic, sentence-level,task-specific | self-compiled dictionary |
| San Marcos | Used for all categories of PHI |
7. Results
We evaluated all systems on both i2b2-PHI and HIPAA-PHI categories, both based on entity- and token-level annotations. We ranked each team based on their top performing system run in terms of micro-averaged entity-based F1 on i2b2-PHI categories. The evaluations reported in this section are the results from the shared-task submissions; we report results only on the best-performing submission of each team. In their own papers in this supplement, the participants had the opportunity to present systems and results that improve upon their shared task submissions.
Table 2 shows the entity-based results for each team's best system run on i2b2-PHI, sorted by micro-averaged F1. Overall, the systems performed quite well on what is known to be a difficult task. Three systems achieved micro-averaged F1 measures of over .9, and eight of them scored over .58. Given that the entity-based, i2b2-PHI evaluation has the strictest rules for obtaining a true positive, these results will always compare less favorably to other evaluations in this paper. We also include the macro-averaged scores in this table, which show that for most teams the macro evaluation scores barely differ from the micro scores for most teams. As this difference continues throughout the other evaluations, we omit macro scores from the rest of the paper.
Table 2.
i2b2-PHI categories: micro- and macro-averaged entity-based evaluation. The micro-F1 scores are bolded, as they are the primary evaluation metric for this task.
| Rank | Team Name | Micro- averaged Precision |
Micro- averaged Recall |
Micro- averaged F1 |
Macro- averaged Precision |
Macro- averaged Recall |
Macro- averaged F1 |
|---|---|---|---|---|---|---|---|
| 1 | University of Nottingham | 0.9645 | 0.9092 | 0.9360 | 0.9653 | 0.9156 | 0.9398 |
| 2 | Harbin Institute of Technology: Shenzhen Graduate School | 0.9264 | 0.8988 | 0.9124 | 0.9282 | 0.9091 | 0.9185 |
| 3 | University of Manchester | 0.9306 | 0.8836 | 0.9065 | 0.9341 | 0.893 | 0.9131 |
| 4 | Harbin Institute of Technology | 0.9229 | 0.8505 | 0.8852 | 0.9228 | 0.8576 | 0.889 |
| 5 | Kaiser Permanente | 0.8731 | 0.7700 | 0.8183 | 0.8727 | 0.7627 | 0.814 |
| 6 | LIMSI–CNRS | 0.8937 | 0.7332 | 0.8055 | 0.8909 | 0.7272 | 0.8007 |
| 7 | Memorial University of Newfoundland | 0.7944 | 0.7191 | 0.7549 | 0.7963 | 0.7259 | 0.7595 |
| 8 | East China Normal University | 0.9344 | 0.4288 | 0.5878 | 0.9215 | 0.3951 | 0.5531 |
| 9 | California State University San Marcos | 0.7628 | 0.3526 | 0.4823 | 0.7217 | 0.3235 | 0.4467 |
| 10 | UC San Diego | 0.5271 | 0.3825 | 0.4433 | 0.5662 | 0.4011 | 0.4696 |
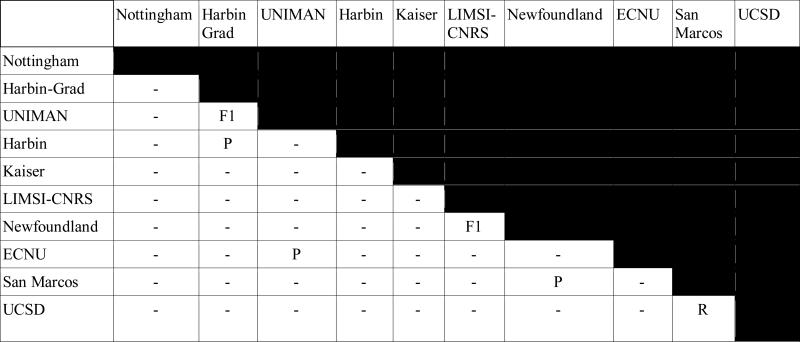
Table 3 shows the results of the significance tests between the top-ranking submissions of each team, as determined by micro-averaged entity-based F1 over i2b2-PHI categories (see Table 2). Cells with P, R, or F1 indicate that the two systems are not significantly different in P, R, or F1, respectively. Overall, we see that the majority of the systems are significantly different in terms of their output. Note that we only show half the table, as the upper diagonal would be symmetrically identical to the lower.
Table 3.
Significance tests for de-identification systems using entity-based evaluations over i2b2-PHI categories
Table 4 shows the token-level evaluations of the i2b2-PHI categories. As we discussed, this is a less restrictive evaluation, as it counts each PHI token separately. All the teams’ scores are higher using this evaluation metric, suggesting that some of the errors in the entity-based evaluations are from not capturing the entire PHI entity.
Table 4.
i2b2-PHI categories: micro-averaged token-based evaluation
| Rank | Team Name | Micro-averaged Precision | Micro-averaged Recall | Micro-averaged F1 |
|---|---|---|---|---|
| 1 | University of Nottingham | .9815 | .9414 | .9611 |
| 2 | University of Manchester | .9722 | .9250 | .9480 |
| 3 | Harbin Institute of Technology: Shenzhen Graduate School | .9564 | .9366 | .9464 |
| 4 | Harbin Institute of Technology | .9571 | .9051 | .9304 |
| 5 | Kaiser Permanente | .9397 | .8609 | .8986 |
| 6 | LIMSI–CNRS | .9321 | .7783 | .8483 |
| 7 | Memorial University of Newfoundland | .8629 | .8038 | .8323 |
| 8 | East China Normal University | .9498 | .5399 | .6885 |
| 9 | California State University San Marcos | .9010 | .4753 | .6223 |
| 10 | UC San Diego | .7164 | .4939 | .5847 |
For comparison, Tables 5 and 6 show the results when the systems are evaluated on only the HIPAA-PHI categories at the entity and token levels, respectively. Table 4 shows that the token-based HIPAA-PHI evaluation resulted in the highest scores for each team. Again, as we would expect, the token-based evaluations result in higher scores, and overall the token-based HIPAA-PHI scores are the highest of all.
Table 5.
HIPAA-PHI categories only: micro-averaged entity-based evaluation
| Rank | Team Name | Micro-averaged Precision | Micro-averaged Recall | Micro-averaged F1 |
|---|---|---|---|---|
| 1 | University of Nottingham | .9763 | .9390 | .9573 |
| 2 | Harbin Institute of Technology: Shenzhen Graduate School | .9513 | .9307 | .9409 |
| 3 | University of Manchester | .9437 | .9213 | .9323 |
| 4 | Harbin Institute of Technology | .9414 | .8957 | .9180 |
| 5 | Kaiser Permanente | .8850 | .8047 | .8429 |
| 6 | LIMSI–CNRS | .9137 | .7666 | .8337 |
| 7 | Memorial University of Newfoundland | .8494 | .7535 | .7985 |
| 8 | East China Normal University | .9335 | .6117 | .7391 |
| 9 | California State University San Marcos | .7758 | .4571 | .5753 |
| 10 | UC San Diego | .5384 | .3900 | .4524 |
Table 6.
HIPAA-PHI categories only: micro-averaged token-based evaluation
| Rank | Team Name | Micro-averaged Precision | Micro-averaged Recall | Micro-averaged F1 |
|---|---|---|---|---|
| 1 | University of Nottingham | 0.9889 | 0.9629 | 0.9757 |
| 2 | University of Manchester | 0.9797 | 0.9542 | 0.9668 |
| 3 | Harbin Institute of Technology Shenzhen Graduate School | 0.9748 | 0.9578 | 0.9662 |
| 4 | Harbin Institute of Technology | 0.9708 | 0.9371 | 0.9536 |
| 5 | Kaiser Permanente | 0.9548 | 0.8914 | 0.9221 |
| 6 | Memorial University of Newfoundland | 0.9037 | 0.8365 | 0.8688 |
| 7 | LIMSI–CNRS | 0.9514 | 0.7972 | 0.8675 |
| 8 | East China Normal University | 0.9496 | 0.7273 | 0.8237 |
| 9 | California State University San Marcos | 0.9085 | 0.6039 | 0.7255 |
| 10 | UC San Diego | 0.7439 | 0.5089 | 0.6043 |
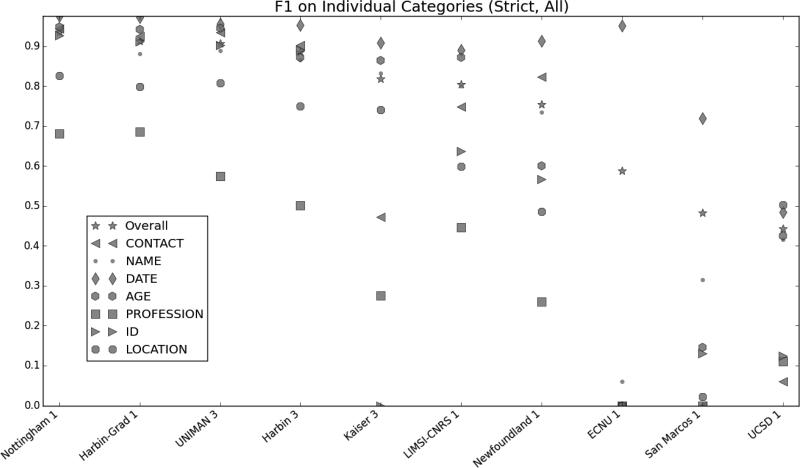
Figure 1 shows the entity-based micro-averaged F1 scores for the individual i2b2-PHI categories. Overall, the PROFESSION and LOCATION categories proved to be the most difficult. There are multiple factors that contribute to this. First, the phrases labeled as PROFESSION, LOCATION-ORGANIZATION and LOCATION-OTHER vary widely in content, form, and structure, from simple phrases such as “firefighter” or “Cape Cod” to complex descriptions such as “Ground Transit Operators Supervisor” or “Fountain Of The Four Rivers”. Additionally, not all PROFESSIONs are nouns or noun phrases, making syntactic cues harder to use. For example, “nurse” and “nursing” are both labeled as PROFESSION because “she is a nurse” and “he works in nursing” both refer to a person's job. Lack of training data also contributes to the problem for these tags: there are only 413 PROFESSION, 206 LOCATION-ORGANIZATION and 17 LOCATION-OTHER tags in the entire i2b2/UTHealth shared task corpus (Stubbs and Uzuner, this issue), and the tags do not exist in other de-identified corpora, such as the i2b2 2006 challenge data (Uzuner et al., 2007).
Figure 1.
Micro-averaged entity-based micro-averaged F1 measures by category: i2b2-PHI categories
7.1 Comparison to 2006 i2b2 de-identification shared task
The existence of the 2006 i2b2 de-identification challenge (Uzuner et al., 2007) raises the question of whether de-identification systems have improved significantly in the past eight years. However, differences in the data sets, annotation schemes, and evaluation software make the comparison between participating systems somewhat tricky.
To begin with, the data from the 2006 shared task were tokenized before the organizers shared it with the task participants. However, for the 2014 data we chose to not make any such modifications, preferring instead to share the data in the same form they were found in the Partners data repository. The lack of tokenization makes the 2014 task more difficult, and somewhat changes the evaluation metric, as the “token-based” evaluation simply uses whitespace to determine tokenization, rather than using an automated tokenizing system. The 2006 data consisted of 889 discharge summaries (669 training, 220 test), while the 2014 data contained a wider variety of clinical records, including discharge summaries, admission notes, and correspondences between doctors.
Additionally, the 2006 annotation scheme was based more closely on the HIPAA-PHI categories, using only PATIENT, DOCTOR, LOCATION, HOSPITAL, DATE, ID, and PHONE. In part, the smaller number of categories in the 2006 data was due to the lack of any examples of the other PHI categories, such as fax numbers, emails, etc. As shown in the earlier sections, the 2014 data contained some PHI categories with less representation (such as PROFESSION and ORGANIZATION). The 2006 data annotated only the day and month of dates, while the 2014 data annotated all parts of dates, including years.
Finally, during surrogate generation, the 2006 data included ambiguous terms (substituting procedure and device names for people and locations) and out-of-vocabulary terms (i.e., deliberately introduced misspellings). While the 2014 data do include misspellings, they do not introduce deliberately ambiguous terms as PHI.
Despite these differences, the two tasks are similar enough that we can still perform some basic comparisons. We performed binary (PHI vs. non-PHI) entity- and token-based evaluations on the 2014 data, looking only at the HIPAA-PHI categories, for this purpose.
Table 7 shows the best micro-averaged token-based P, R, and F1 scores from the top run for each 2006 and 2014 team using the binary evaluation on only the HIPAA-PHI categories. Best team run was selected based on F1. Table 8 shows the same information at the entity level.
Table 7.
Comparison of 2006 and 2014 team results: precision, recall, and F1 of token-based binary HIPAA-PHI. Top result for each team selected by F1.
| 2006 teams | 2014 teams | ||||||
|---|---|---|---|---|---|---|---|
| Team name/run | P | R | F1 | Team name/run | P | R | F1 |
| Wellner 3 | 98.7 | 97.5 | .981 | Nottingham 1 | .9900 | .9640 | .9768 |
| Szarvas 2 | 99.3 | 96.9 | .980 | Harbin-Grad 2 | .9776 | .9629 | .9702 |
| Aramaki 1 | 99.1 | 94.9 | .970 | Manchester 3 | .9825 | .9567 | .9694 |
| Hara 3 | 96.1 | 93.8 | .949 | Harbin 3 | .9747 | .9408 | .9575 |
| Wrenn 3 | 94.9 | 94.3 | .946 | Kaiser 3 | .9692 | .8999 | .9333 |
| Guo 1 | 93.8 | 88.2 | .909 | Newfoundland 1 | .9207 | .8522 | .8851 |
| Guillen 1 | 92.8 | 70.5 | .801 | LIMSI-CNRS 3 | .9605 | .8048 | .8758 |
| ECNU 1 | .9666 | .7404 | .8385 | ||||
| San Marcos 1 | .9095 | .6045 | .7263 | ||||
| UCSD 1 | .7591 | .5161 | .6144 | ||||
Table 8.
Comparison of 2006 and 2014 team results: precision, recall, and F1 of entity-based binary HIPAA-PHI
| 2006 teams | 2014 teams | ||||||
|---|---|---|---|---|---|---|---|
| Team name/run | P | R | F1 | Team name/run | P | R | F1 |
| Szarvas 3 | .978 | .957 | .967 | Nottingham 1 | .9776 | .9403 | .9586 |
| Wellner 3 | .967 | .959 | .963 | Harbin-Grad 1 | .9557 | .9350 | .9452 |
| Aramaki 1 | .951 | .931 | .941 | Manchester 3 | .9459 | .9234 | .9345 |
| Hara 3 | .910 | .896 | .903 | Harbin 3 | .9459 | .9000 | .9224 |
| Wrenn 3 | .887 | .918 | .902 | Kaiser 3 | .8919 | .8076 | .8477 |
| Guo 1 | .87 | .798 | .813 | LIMSI-CNRS 3 | .9219 | .7736 | .8413 |
| Newfoundland 1 | .8628 | .7654 | .8112 | ||||
| ECNU 1 | .9342 | .6122 | .7397 | ||||
| San Marcos 1 | .7780 | .4584 | .5769 | ||||
| UCSD 1 | .5403 | .3914 | .4540 | ||||
For P, R, and F1, both the token-based and entity-based comparisons show that the top 2006 systems perform slightly better, though the differences are relatively small. Given the aforementioned differences between the two corpora, we can conclude that overall the systems from 2014 are at least on par with the 2006 systems.
8. Discussion
In the overview paper for the 2006 i2b2 de-identification shared task, the authors posed the following questions: “1. Does success on this challenge problem extrapolate to similar performance on other, untested data sets? 2. Can health policy makers rely on this level of performance to permit automated or semi-automated de-identification of health data for research purposes without undue risk to patients?” (Uzuner et al., 2007)
In general, it remains difficult to say whether the systems built for this challenge will perform as well on other data. While the data for the 2014 shared task included a wider variety of document types than the 2006 data, both sets were drawn from the Partners HealthCare and so share a certain degree of similarity. In order to truly determine if the performance will extrapolate to other data sets, we will need data sets from other medical institutions that have PHI identified and replaced with surrogates in a similar fashion.
The answer to the second question is similarly difficult to determine, for similar reasons. However, for institutions that use a data format similar to that of Partners, the answer could be positive. While we are not aware of an industry-wide standard, 95% has been suggested as a rule-of thumb for determining whether a system can reliably de-identify a data set for safe distribution. Table 2 shows that, looking at HIPAA-PHI only and using a token-based evaluation, the top 4 systems satisfy this requirement. A related consideration is whether perfect de-identification (100% precision and recall) is a realistic goal. Given the performance of the participating systems in this challenge, as well as other recently developed de-identification software, it may be that perfect de-identification is unachievable, with the best performances we can expect being around .95 or slightly higher.
9. Conclusion
This paper presents an overview of the de-identification track (Track 1) from the 2014 i2b2/UTHealth NLP shared task. Due to the different needs differing institutions might have for de-identifying records, this task investigates performance on de-identification at both entity and token levels, for various definitions of PHI: i2b2-PHI, which match the gold standard; HIPAA-PHI, which adhere strictly to the HIPAA guidelines for de-identification; and binary PHI, which consider only whether a PHI is identified as PHI at all. Of these, the entity-based i2b2-PHI de-identification was the most difficult, with the highest-ranked team achieving a micro-averaged F1 of 0.9360.
In its most strict form, de-identification remains a task that cannot yet be handled perfectly by automated systems; however, the performances of the systems are encouraging and can solve a significant portion of the task. Whether this performance is “good enough” remains a topic of debate and depends on the PHI types that are missed (e.g., doctor names vs patient names would have different significance for perfect identification). Until these debates are resolved, we expect most data will be distributed with data use agreements that tackle the problem from the policy end, thus strengthening the solutions provided by the automated systems.
Highlights.
First de-identification shared task on clinical narratives
10 teams participated, submitting 22 system output
Top-performing system achieved micro-averaged F1 measure of .936 using strictest evaluation metric
Acknowledgements
We would like to thank the program committee for the 2014 i2b2/UTHealth NLP Shared Task, along with everyone who participated in the task and workshop. We would also like to that the JBI editor and reviewers, for their thoughtful comments and feedback.
Funding for this project was provided by:
NIH NLM 2U54LM008748, PI: Isaac Kohane
NIH NLM 5R13LM011411, PI: Ozlem Uzuner
NIH NIGMS 5R01GM102282, PI: Hua Xu
Appendix
Table A1.
Participants in Track 1 of the 2014 i2b2/UTHealth NLP shared task
| Team name | Affiliations | # of members | Countries |
|---|---|---|---|
| Nottingham | University of Nottingham | 2 | UK |
| UNIMAN | University of Manchester University of Novi Sad Health eResearch Centre | 5 | UK Serbia |
| Harbin | Harbin Institute of Technology | 5 | China |
| Harbin-Grad | Harbin Institute of Technology Shenzhen Graduate School | 5 | China |
| ECNU | East China Normal University | 1 | China |
| Kaiser | Kaiser Permanente Southern California | 7 | USA |
| LIMSI-CNRS | Centre National de la Recherche Scientifique | 1 | France |
| San Marcos | California State University San Marcos | 1 | USA |
| Newfoundland | Memorial University of Newfoundland | 1 | Canada |
| UCSD | University of California San Diego | 5 | USA |
Table A2.
A set of variations of system output, and how they would be compared to the gold standard using the different levels of evaluation. A + indicates that the evaluation method would result in a true positive, a - indicates that the input would result in a false positive.
| Gold standard: <LOCATION type=“HOSPITAL”>Brooks Infirmary</LOCATION> | ||||||
|---|---|---|---|---|---|---|
| Instance-based | Token-based | |||||
| i2b PHI categories and types |
HIPAA PHI categories only |
PHI/not PHI |
i2b2 PHI categories and types |
HIPAA PHI categories only |
PHI/not PHI |
|
| <LOCATION type=“HOSPITAL”>Brooks Infirmary</LOCATION> | + | + | + | + | + | + |
| <LOCATION type=“ORGANIZATION”>Brooks Infirmary</LOCATION> | − | + | + | + | + | + |
| <NAME type=“DOCTOR”>Brooks Infirmary</NAME> | − | − | + | − | − | + |
| <LOCATION type=“HOSPITAL”>Brooks</LOCATION> | − | − | − | + | + | + |
| <LOCATION type=“ORGANIZATION”>Brooks</LOCATION> | − | − | − | − | + | + |
| <NAME type=“DOCTOR”>Brooks</NAME> | − | − | − | − | − | + |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Informatics for Integrating Biology and the Bedside
University of Texas Health Science Center at Houston
Works cited
- Aberdeen John, Bayer Samuel, Yeniterzi Reyyan, Wellner Ben, Clark Cheryl, Hanauer David, Malin Bradley, Hirschman Lynette. The MITRE Identification Scrubber Toolkit: Design, training, and assessment. International Journal of Medical Informatics. 2010 Dec;79(12):849–59. doi: 10.1016/j.ijmedinf.2010.09.007. doi: 10.1016/j.ijmedinf.2010.09.007. [DOI] [PubMed] [Google Scholar]
- [May 2015];Apache UIMA. 2006 http://uima.apache.org.
- Baum LE, Petrie T. Statistical Inference for Probabilistic Functions of Finite State Markov Chains. [28 November 2011];The Annals of Mathematical Statistics. 1966 37(6):1554–1563. doi:10.1214/aoms/1177699147. [Google Scholar]
- [January 7, 2015];BioASQ project. Data. http://www.bioasq.org/participate/data.
- Blei David M, Ng Andrew Y, Jordan Michael I. Latent dirichlet allocation. The Journal of Machine Learning research. 2003;3:993–1022. [Google Scholar]
- Boser BE, Guyon IM, Vapnik VN. A training algorithm for optimal margin classifiers. Proceedings of the fifth annual workshop on Computational learning theory - COLT '92. 1992:144. doi:10.1145/130385.130401. [Google Scholar]
- Chen Tao. Hidden Markov Model using Dirchilet Process for De-Identification. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) doi: 10.1016/j.jbi.2015.09.004. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinchor Nancy (a) Named Entity Scores – English. [January 6, 2015];Message Understanding Conference Proceedings. http://www.itl.nist.gov/iaui/894.02/related_projects/muc/proceedings/ne_english_score_report.html Updated January 12, 2001.
- Chinchor Nancy. [January 6, 2015];MUC-7 Named Entity Task Definition version 3.5. 1997b http://www.itl.nist.gov/iaui/894.02/related_projects/muc/proceedings/ne_task.html.
- Chinchor Nancy. The statistical significance of the MUC-4 results. Proceedings of the 4th conference on Message understanding. 1992:30–50. [Google Scholar]
- Dehghan Azad, Kovačević Aleksandar, Karystianis George, Keane John A., Nenadic Goran. Combining Knowledge- and Data-driven Methods for De-identification of Clinical Narratives. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) doi: 10.1016/j.jbi.2015.06.029. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deleger Louise, Lingren Todd, Ni Yizhao, Kaiser Meghan, Stoutenborough Laura, Marsolo Keith, Kouril Michal, Molnar Katalin, Solti Imre. Preparing an annotated gold standard corpus to share with extramural investigators for de-identification research. Journal of Biomedical Informatics. Aug. 2014;50:173–83. doi: 10.1016/j.jbi.2014.01.014. doi: 10.1016/j.jbi.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deleger L, Molnar K, Savova G, Xia F, Lingren T, Li Q, et al. Large-scale evaluation of automated clinical note de-identification and its impact on information extraction. J Am Med Inform Assoc. 2012 doi: 10.1136/amiajnl-2012-001012. doi:10.1136/amiajnl-2012-001012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Emam K, Buckeridge D, Tamblyn R, Neisa A, Jonker E, Verma A. The re-identification risk of Canadians from longitudinal demographics. BMC Medical Informatics Decision Making. 2011;11:46. doi: 10.1186/1472-6947-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrández Oscar, South Brett R, Shen Shuying, Friedlin F Jeffrey, Samore Matthew H, Meystre Stéphane M. BoB, a best-of-breed automated text de-identification system for VHA clinical documents. Journal of the American Medical Informatics Association. 2013 Jan 1;20(1):77–83. doi: 10.1136/amiajnl-2012-001020. doi: 10.1136/amiajnl-2012-001020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golle P. Revisiting the uniqueness of simple demographics in the US population. Workshop on Privacy in the Electronic Society. 2006 [Google Scholar]
- Grouin Cyril. Clinical records de-identification using CRF and rule-based approaches. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement)(this issue) [Google Scholar]
- Guillen Rocio. An Approach to De-Identifying Electronic Medical Records. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) this issue. [Google Scholar]
- He Bin, Cheng Jianyi, Guan Yi, Cen Keting, Hua Wenlan. A CRF-based Approach to De-identification in Medical Records. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) doi: 10.1016/j.jbi.2015.08.012. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschman L, Yeh A, Blaschke C, Valencia A. Overview of BioCreAtIvE: critical assessment of information extraction for biology BMC Bioinformatics. 2005;v6:s1. doi: 10.1186/1471-2105-6-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafferty J, McCallum A, Pereira F. Conditional random fields: Probabilistic models for segmenting and labeling sequence data. Proc. 18th International Conference on Machine Learning. 2001 [Google Scholar]
- Liu Zengjian, Tang Buzhou, Chen Qingcai, Wang Xiaolong, Li Haodi. De-identification of electronic medical records – HITSZ's system for track 1 of the 2014 i2b2 NLP challenge. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) this issue. [Google Scholar]
- Kim Jin-Dong, Ohta Tomoko, Pyysalo Sampo, Kano Yoshinobu, Tsujii Jun'ichi. Proceedings of the Workshop on BioNLP: Shared Task. Association for Computational Linguistics; Boulder, Colorado: Jun, 2009. Overview of BioNLP’09 Shared Task on Event Extraction. pp. 1–9. [Google Scholar]
- Kumar Vishesh, Stubbs Amber, Shaw Stanley, Uzuner Ozlem. Creation of a new longitudinal corpus of clinical narratives. Journal of Biomedical Informatics. doi: 10.1016/j.jbi.2015.09.018. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCallum AC. MALLET: a Machine Learning for Language Toolkit. 2002 [Google Scholar]
- Meystre Stephane M., Friedlin F Jeffrey, South Brett R, Shen Shuying, Samore Matthew H. Automatic de-identification of textual documents in the electronic health record: a review of recent research. BMC medical research methodology. 2010;10(1):70. doi: 10.1186/1471-2288-10-70. doi: 10.1186/1471-2288-10-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nédellec C, Bossy R, Kim J-D, Kim J-J, Ohta T, Pyysalo S, Zweigenbaum P. Overview of BioNLP Shared Task 2013 Proceedings of the BioNLP Shared Task 2013 Workshop. Association for Computational Linguistics; 2013. pp. 1–7. [Google Scholar]
- Noreen EW. Computer-intensive methods for testing hypotheses: an introduction. Wiley; New York: 1989. [Google Scholar]
- Orbanz P, Teh YW. Bayesian Nonparametric Models. Article in Encyclopedia of Machine Learning. Springer. 2010 [Google Scholar]
- Pyysalo S, Ohta T, Rak R, Sullivan D, Mao C, Wang C, Sobral B, Tsujii J, Ananiadou S. Overview of the ID, EPI and REL tasks of BioNLP Shared Task 2011 BMC Bioinformatics. 2012;13 doi: 10.1186/1471-2105-13-S11-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savova GK, Masanz JJ, Ogren PV, et al. Mayo clinical Text Analysis and Knowledge Extraction System (cTAKES): architecture, component evaluation and applications. Journal of the American Medical Informatics Association. 2010;17:507–13. doi: 10.1136/jamia.2009.001560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs A, Kotfila C, Xu H, Uzuner O. Identifying risk factors for heart disease over time. Journal of Biomedical Informatics. doi: 10.1016/j.jbi.2015.07.001. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs A, Uzuner O. De-identifying longitudinal medical records. Journal of Biomedical Informatics. this issue. [Google Scholar]
- Stubbs A, Uzuner Ö. De-identification of Medical Records Through Annotation. In: Ide Nancy, Pustejovsky James., editors. Chapter in Handbook of Linguistic Annotation. Springer; 2015. Submitted, anticipated publication. [Google Scholar]
- Stubbs A, Uzuner Ö, Kotfila C, Goldstein I, Szolovitz P. Challenges in Synthesizing Replacements for PHI in Narrative EMRs. In: Gkoulalas-Divanis Aris, Loukides Grigorios., editors. Chapter in Medical Data Privacy Handbook. Springer; 2015. Anticipated publication. [Google Scholar]
- Sundheim B. Overview of results of the MUC-6 Evaluation. Proceedings of the Sixth Message Understanding Conference (MUC-6) 1995 [Google Scholar]
- Sweeney L. Uniqueness of Simple Demographics in the U.S. Population. Carnegie Mellon University, School of Computer Science, Data Privacy Laboratory, Technical Report LIDAP-WP4; Pittsburgh: 2000. [Google Scholar]
- Torii Manabu, Fan Jung-wei, Yang Wei-li, Lee Theodore, Wiley Matthew T., Zisook Daniel, Huang Yang. De-Identification and Risk Factor Detection in Medical Records. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) doi: 10.1016/j.jbi.2015.08.011. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzuner O, Luo Y, Szolovits P. Evaluating the State-of-the-Art in Automatic De-identification. Journal of the American Medical Informatics Association. 2007;14(5):550–563. doi: 10.1197/jamia.M2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellner Benjamin. Sequence Models and Ranking Methods for Discourse Parsing [Ph.D. Dissertation] Brandeis University; Waltham, MA: 2009. [Google Scholar]
- Xu H, Stenner SP, Doan S, Johnson KB, Waitman LR, Denny JC. MedEx: a medication information extraction system for clinical narratives. Journal of the American Medical Informatics Association. JAMIA. 2010;17(1):19–24. doi: 10.1197/jamia.M3378. doi:10.1197/jamia.M3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Hui, Garibaldi Jonathan. A Hybrid System for Automatic De-identification in Patient Discharge Summaries. Journal of Biomedical Informatics. 2014;(i2b2 NLP supplement) this issue. [Google Scholar]