Abstract
Rhabdomyosarcoma arising in the female genital tract carries five-year survival in excess of 80%, but lifelong infertility may be a consequence of local control strategies. We present the technique and outcome for a fertility-sparing, radical abdominal trachelectomy in a 12-year-old girl with anaplastic, embryonal rhabdomyosarcoma involving the uterine cervix. The patient had presented to our center following the piecemeal resection of a uterine cervical mass; because of concern about microscopic residual disease, we classified her as group II-A according to the International Rhabdomyosarcoma Study (IRS) system. Staging studies excluded the presence of distant disease. The patient received four cycles of multiagent chemotherapy and then underwent radical abdominal trachelectomy, with removal of the uterine cervix, parametria, vaginal cuff, and regional lymph nodes. Microscopically, the specimen showed treatment effect and no residual tumor. Regional nodes were negative. Radical abdominal trachelectomy, which has not been previously reported for rhabdomyosarcoma, has appeared to secure local disease control in this case, while preserving the patient’s future fertility potential. In properly selected cases of rhabdomyosarcoma of the uterine cervix, where involvement of the uterus proper is not present, radical abdominal trachelectomy may be an attractive fertility-sparing alternative to radical hysterectomy.
Keywords: Rhabdomyosarcoma, Embryonal, Anaplasia, Uterus, Cervix, Trachelectomy
Rhabdomyosarcoma is the most common pediatric soft tissue sarcoma, and often arises from genitourinary sites [1,2]. Multi-modal treatment for this disease includes systemic chemotherapy, as well as surgery and/or radiotherapy for local control. Girls and young women with rhabdomyosarcoma of genital tract origin may now expect an overall five-year survival of 82% [3]. Long-term side effects, however, are common and may include infertility and/or sexual dysfunction. The likelihood of infertility is enhanced when radiotherapy to the vagina or cervix is utilized, and its likelihood is assured if hysterectomy is performed.
In response to this concern, clinicians have, in cases of clearly localized and purely embryonal rhabdomyosarcoma of the cervix (“sarcoma botryoides”), pursued less disabling operations including polypectomy and cervical conization [4-13]. Documentation of microscopically negative margins is a critical aspect of implementing such a limited surgical approach. Few data exist, however, as to how clinicians have handled cervical primaries with microscopic residual disease, which is classified as clinical group II in the Intergroup Rhabdomyosarcoma Study (IRS) system. There were no group II patients with cervical primaries in the IRS-I study (1972-1978) nor in the IRS-II study (1978-1984) [14,15]. The subsequent IRS-III study (1984-1991) and IRS-IV study (1991-1997) included only two such patients between them [3]. Because there are few prior published cases, clinicians must at present derive individualized treatment plans for any such patient.
We present a case referred to us in which a prior piecemeal resection was performed of an anaplastic, embryonal rhabdomyosarcoma of the uterine cervix. We selected a uterine-sparing option for local control and regional staging that included removal of the entire uterine cervix and parametria along with dissection of bilateral retroperitoneal lymph nodes, with reconstruction of the uterine isthmus to the vagina. Also known as fertility-sparing radical abdominal trachelectomy, this technique has not, to our knowledge, been previously applied to rhabdomyosarcoma of the uterine cervix.
1. METHODS
1.1. Clinical History
A previously healthy 12-year-old girl described a “grape-like” mass protruding from the vagina after swimming, which reportedly partially “fell off.” Several months later, after development of a vaginal odor and darkly-colored discharge, she was evaluated by a pediatrician and then a gynecologist. Antibiotics were prescribed. When no improvement was noted, ultrasonographic imaging was obtained and a limited internal exam, performed awake, demonstrated a cervicovaginal mass. A small biopsy was performed and was diagnostic for embryonal rhabdomyosarcoma.
She subsequently underwent an examination under anesthesia, during which an exophytic mass was found arising from the posterior lip of the cervix and filling the vaginal vault. A stalk apparently connecting the mass to the cervix was surgically transected and the resulting defect in the cervix sutured. The specimen was submitted to pathology in two components, each consisting of multiple, unoriented pieces measuring, in aggregate, 10 × 8 × 3 cm for the first specimen and 4 × 2.5 × 2 cm for the second specimen. A diagnosis of embryonal rhabdomyosarcoma with focal anaplastic features, arising in cervical stromal tissue, was rendered by the outside pathologist. Margin status was unknown. The patient was referred to our center.
Our evaluation included a repeat examination under anesthesia demonstrating a healing suture line in the uterine cervix, with no evidence of gross residual disease. Vaginal and cervical brush cytology were negative. However, the depth of involvement and depth of resection into the cervical stroma were difficult to assess, and the presence of microscopically positive margins could not be ruled out in the unoriented resection specimen. We classified her as IRS group II-A on this basis. Magnetic resonance imaging did not suggest the presence of macroscopic residual disease, and metastatic workup (CT scan of chest, abdomen, and pelvis; technetium bone scan; whole body positron emission tomography; and bilateral bone marrow aspirates and biopsies) was negative. Additional review of the pathology from the original specimen was performed, including a review by the Soft Tissue Sarcoma Pathology Committee of the Childrens’ Oncology Group (COG), which rendered a final diagnosis of embryonal rhabdomyosarcoma with diffuse anaplasia.
Based on the absence of distant metastases, a “favorable” site primary tumor, and embryonal histology, the patient was deemed to have “low-risk” disease (Stage 1, Group II), and, after informed consent was obtained from her mother, she was enrolled on COG protocol ARST 0331, subset A, regimen 1, a multiagent chemotherapy regimen consisting of vincristine, dactinomycin, and cyclophosphamide. This treatment schema calls for ten weeks of three-agent chemotherapy, followed at week 13 by local control maneuvers (for which we selected, in this case, radical abdominal trachelectomy), followed by an additional ten weeks of two-agent chemotherapy with vincristine and dactinomycin.
1.2. Operative Technique
At week 13 of treatment, the patient underwent resection. Our current technique for a fertility-sparing radical abdominal trachelectomy was reported previously [19] and the steps performed in this case are summarized as follows.
The patient received preoperative bowel preparation and perioperative intravenous antibiotics. An infraumbilical, vertical midline laparotomy to assess the pelvic organs and exclude intraperitoneal metastasis was performed. We found clinically enlarged lymph nodes (measuring up to 1.7 cm) in several of the pelvic lymphatic basins, so we proceeded with bilateral pelvic lymphadenectomy in a manner similar to that for patients undergoing radical hysterectomy. The limits of nodal dissection were the deep circumflex iliac vein caudally and the proximal common iliac artery cephalad. (If these nodes had proven histologically positive for disease, we would have given consideration to regional radiotherapy postoperatively.)
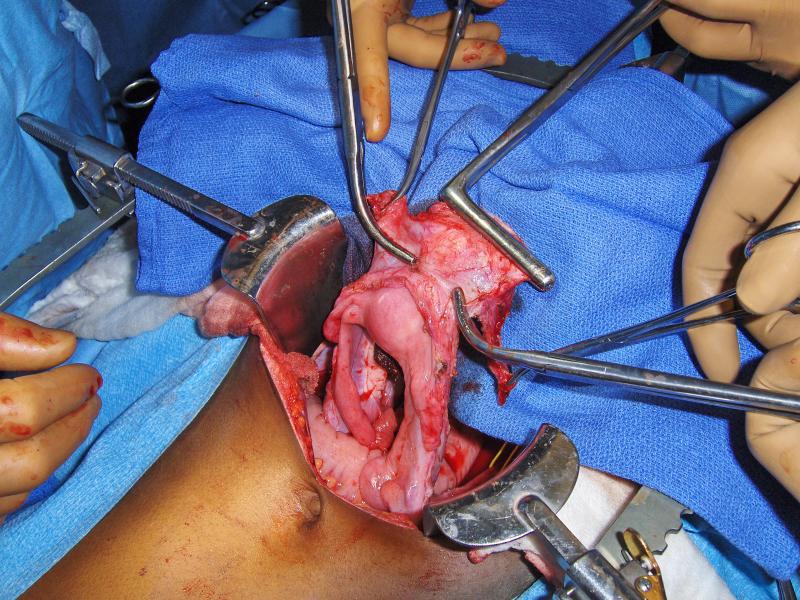
The intent of the radical abdominal trachelectomy was to resect the cervix, upper 1–2 cm of the vagina, parametrium, and paracolpos in a similar manner to a type II radical abdominal hysterectomy but sparing the uterine fundus or corpus (Fig. 1).
FIG. 1.
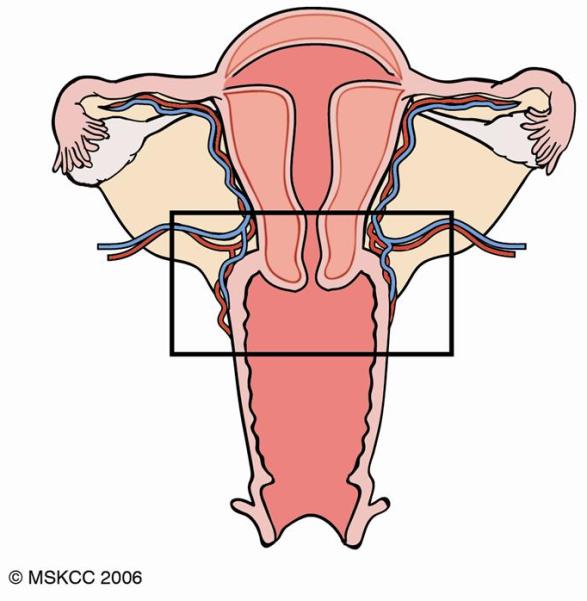
The intent of this radical abdominal trachelectomy was to resect the cervix, upper 1–2 cm of the vagina, parametrium, and paracolpos in a similar manner to a type II radical abdominal hysterectomy while sparing the uterine corpus.
The trachelectomy was begun by developing the paravesical and pararectal spaces and dissecting the bladder caudal to the mid-vagina. The round ligaments were divided and the uterus gently manipulated with an atraumatic Buxton-type uterine clamp. Care was taken not to destroy the cornu or the uteroovarian pedicles.
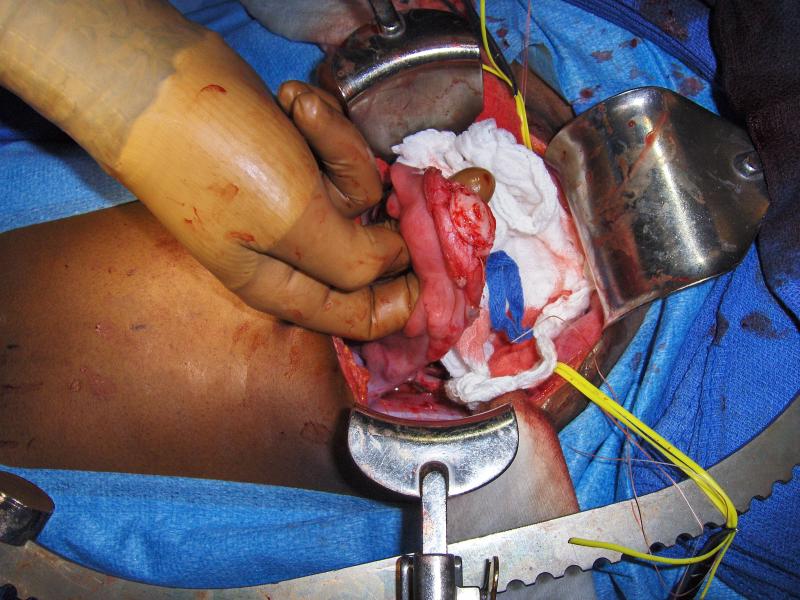
The infundibulopelvic ligaments with ovarian blood supply were kept intact. Care was also taken not to injure the fallopian tubes or disrupt the uteroovarian ligament. The uterine vessels were then ligated and divided at their origin from the hypogastric vessels. The parametria and paracolpos with uterine vessels were mobilized medially with the specimen, and a complete ureterolysis was performed similar to a type II radical abdominal hysterectomy. The posterior cul-de-sac peritoneum was incised and the uterosacral ligament divided; similarly, the parametria and paracolpos were divided. A Wertheim clamp was then placed below the cervix at the desired length of the upper vagina (1-2 cm) followed by two Zeppelin type clamps placed distally at each vaginal corner and the specimen separated (Fig. 2).
FIG. 2.
The uterine fundus and cervix with parametria and upper vagina have been resected with the only remaining blood supply from the bilateral uteroovarian ligaments. The curved clamps demonstrate the level of the internal cervical os where the abdominal trachelectomy incision will be made. The Wertheim clamp has been replaced to occlude the vaginal margin.
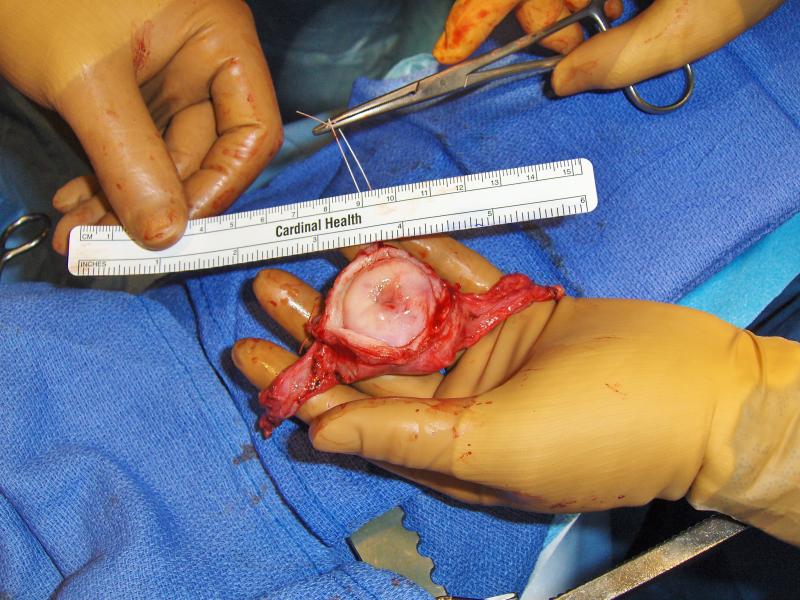
The lower uterine segment was then estimated, and clamps were placed at the level of the internal os (Fig. 2). Using a knife, the radical trachelectomy was completed by separating the fundus from the isthmus or upper endocervix at approximately 5 mm below the level of the internal os. The specimen, consisting of radical trachelectomy, upper vagina, and parametria with suture marking the vaginal cuff at 12 o’clock, was sent for frozen-section evaluation of its endocervical margin (Fig. 3).
FIG. 3.
Specimen of radical abdominal trachelectomy.
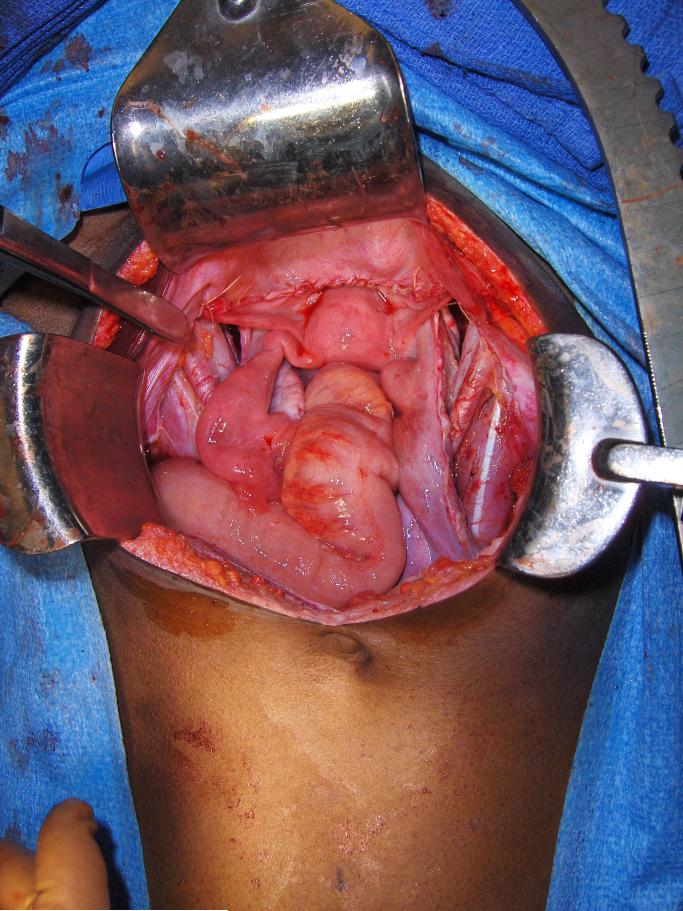
The uterine fundus was inspected (Fig. 4) and curettage of the endometrial cavity was performed as well as a shave disc margin on the remaining cervical tissue, which was sent for frozen-section analysis. This was performed to ensure that the reconstructed uterus to vagina was disease free. (A frozen-section analysis may also be obtained on the distal vaginal margin if clinically indicated.) The uterus was then reconstructed to the upper vagina with interrupted #2-0 absorbable sutures and the continuation of the uterus to the upper vagina restored (Fig. 5). No cervical cerclage was utilized.
FIG. 4.
The remaining uterine fundus is demonstrated without evidence of ischemia.
FIG. 5.
At the end of the procedure, the uterus was reconstructed to the upper vagina and the pelvic anatomy restored. The fundus was viable without evidence of ischemia with the remaining blood supply from bilateral uteroovarian ligaments.
2. RESULTS
2.1. Pathologic Analysis
The specimen consisted of a 3.0 × 2.7 × 2.3 cm uterine cervix with attached parametria and vaginal cuff. Microscopically, the cervical stroma showed edema, hemorrhage, and fibrosis. No residual tumor was present. The parametrial tissues, bilateral external and internal iliac lymph nodes, common iliac lymph nodes, obturator lymph nodes, as well as the endocervical curettage, were all benign.
2.2. Postoperative Course and Follow-up
The patient was discharged home on the fifth postoperative day. Her Foley catheter was removed at follow-up on the eleventh postoperative day. She resumed chemotherapy that day. Based upon the finding of no residual disease in the trachelectomy specimen, no radiotherapy was prescribed.
Vaginal examination at postoperative week eight demonstrated a neo-cervix that was pink and healthy in appearance and that admitted passage of a probe to demonstrate patency. Pap smear at postoperative week ten was normal. Follow-up imaging, performed three months after surgery, demonstrated the healed anastomosis (Fig. 6) and no evidence of disease.
FIG. 6.
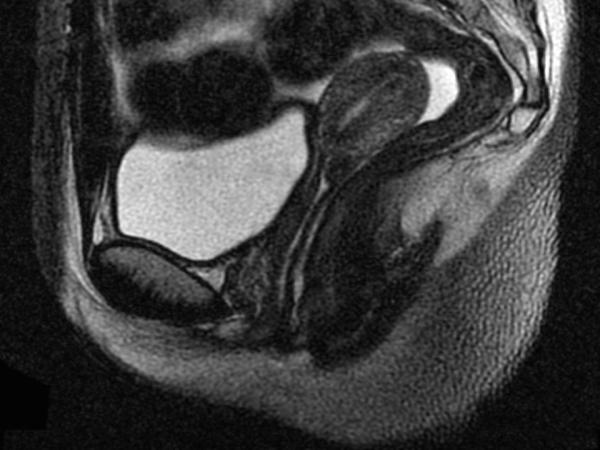
Sagittal T2-weighted magnetic resonance image demonstrating the healed uterine-vaginal anastomosis.
3. DISCUSSION
The treatment for rhabdomyosarcoma of the uterine cervix should always be multimodal and should include multiagent chemotherapy [16]. While radical hysterectomy, combined with pelvic lymphadenectomy, was previously the rule rather than the exception [17,18], the implementation of multimodal therapy has now often enabled the performance of less disfiguring and less disabling surgical procedures.
Surgical approaches need to place local control of disease as a primary goal. However, while ultra-minimally-invasive procedures such as simple polypectomy for an exophytic, botryoid sarcoma have been reported, they carry the hazard of leaving behind residual gross or microscopic disease. Of three patients reported by Zanetta and colleagues who underwent simple polypectomy for cervical sarcoma botryoides, one suffered a local recurrence and a second was found to have an additional focus of disease in the endocervical canal [8]. Most recurrences of rhabdomyosarcoma of the female genital tract are locoregional [3]. It cannot be emphasized strongly enough that polypectomy without histopathologic assessment of the cervical margin is not an oncologically sound operation for this disease.
We were faced, in the present case, with the inability to rule out microscopic residual disease in the cervix, given the piecemeal nature of the patient’s original resection. Of necessity, we classified the tumor as an IRS group IIA lesion (microscopic residual disease following initial gross total resection). For the Children’s Oncology Group protocol ARST 0331, in which the patient was enrolled, local control options for a uterine cervical primary such as this include surgery or radiation therapy; chemotherapy alone, with monitoring of the primary site, is permissible only for IRS group I lesions. The recommended surgical option is hysterectomy to convert the patient to group I, but after consideration, this was felt to be incongruous with the particular clinical situation—namely, that of an exophytic cervical tumor without apparent uterine body involvement. If hysterectomy is not performed, ARST 0331 allows local resections less extensive than hysterectomy for uterine/cervical group IIa lesions (in which case subsequent external beam radiotherapy or endocavitary brachytherapy are given or withheld according to margin and nodal status), or alternatively, radiation therapy. In this instance, we could not assure the patient’s family with any degree of confidence that cervical conization or a more limited resection of the cervix would result in microscopically negative margins and therefore obviate the need for local radiotherapy. We also thought that radiotherapy, whether applied alone or following additional cervical resection, would likely result in long-term side effects including dyspareunia and infertility. After comprehensive discussion of all these options with the family as well as in our multidisciplinary tumor board, the fertility-sparing option of radical trachelectomy was agreed upon by the patient’s family. We felt it was likely that this approach could avert the morbidity of, and indeed the need for, radiation therapy.
Radical abdominal trachelectomy has been reported by our group [19] and others [20] for cervical carcinoma among adult patients. Recently, we have described its use in two pediatric patients with clear cell carcinoma of the cervix [21]. Successful pregnancy and cesarian delivery has been reported in adult patients following radical abdominal trachelectomy [22,23], and it is our hope that patients undergoing this procedure in childhood and adolescence may have the same success.
Surgical treatment for genitourinary rhabdomyosarcoma in children must place local control as a primary objective with the recognition that this group of patients has a favorable prognosis for cure. A comprehensive assessment of the impact of various local control options on subsequent sexual and reproductive health and function is, therefore, an integral part of the multidisciplinary care of these children. In properly selected cases of rhabdomyosarcoma of the uterine cervix, where involvement of the uterus proper is not present, radical trachelectomy may be an attractive option. In the present case, it has appeared to secure local control of disease while preserving the patient’s future potential for fertility.
REFERENCES
- 1.Chintagumpala MM. Soft-tissue sarcomas. In: McMillan JA, Feigin RD, DeAngelis CD, Jones MD Jr, editors. Oski’s Pediatrics: Principles and Practice. Fourth Edition Lippincott, Williams & Wilkins; Philadelphia, PA: 2006. pp. 1781–1786. [Google Scholar]
- 2.Rodeberg D, Paidas C. Childhood rhabdomyosarcoma. Semin Pediatr Surg. 2006;15:57–62. doi: 10.1053/j.sempedsurg.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Arndt CAS, Donaldson SS, Anderson JR, et al. What constitutes optimal therapy for patients with rhabdomyosarcoma of the female genital tract? Cancer. 2001;91:2454–2468. [PubMed] [Google Scholar]
- 4.Daya DA, Scully RE. Sarcoma botryoides of the uterine cervix in young women: a clinicopathological study of 13 cases. Gynecol Oncol. 1988;29:290–304. doi: 10.1016/0090-8258(88)90228-4. [DOI] [PubMed] [Google Scholar]
- 5.Gordon AN, Montag TW. Sarcoma botryoides of the cervix: excision followed by adjuvant chemotherapy for preservation of reproductive function. Gynecol Oncol. 1990;36:119–124. doi: 10.1016/0090-8258(90)90121-z. [DOI] [PubMed] [Google Scholar]
- 6.Lin J, Lam SK, Cheung TH. Sarcoma botryoides of the cervix treated with limited surgery and chemotherapy to preserve fertility. Gynecol Oncol. 1995;58:270–273. doi: 10.1006/gyno.1995.1225. [DOI] [PubMed] [Google Scholar]
- 7.Marana HRC, Andrade JM, Llorach-Velludo MA, et al. Sarcoma botryoides of the female genital tract: long-term results of conservative treatment followed by pregnancy. A case report. Eur J Gynaecol Oncol. 1999;20:122–3. [PubMed] [Google Scholar]
- 8.Zanetta G, Rota SM, Lissoni A, et al. Conservative treatment followed by chemotherapy with doxorubicin and ifosfamide for cervical sarcoma botryoides in young females. Br J Cancer. 1999;80:403–406. doi: 10.1038/sj.bjc.6690370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Porzio G, Toro G, Paris I, et al. Cervical sarcoma botryoides treated with conservative surgery and adjuvant chemotherapy: a case report. Eur J Gynaecol Oncol. 2000;21:499–500. [PubMed] [Google Scholar]
- 10.Bernal KL, Fahmy L, Remmenga S, et al. Embryonal rhabdomyosarcoma (sarcoma botryoides) of the cervix presenting as a cervical polyp treated with fertility-sparing surgery and adjuvant chemotherapy. Gynecol Oncol. 2004;95:243–246. doi: 10.1016/j.ygyno.2004.06.049. [DOI] [PubMed] [Google Scholar]
- 11.Gruessner SEM, Omwandho COA, Dreyer T, et al. Management of stage I cervical sarcoma botryoides in childhood and adolescence. Eur J Pediatr. 2004;163:452–456. doi: 10.1007/s00431-004-1469-y. [DOI] [PubMed] [Google Scholar]
- 12.Caruso RA, Napoli P, Villari D, et al. Anaplastic (pleomorphic) subtype embryonal rhabdomyosarcoma of the cervix. Arch Gynecol Obstet. 2004;270:278–280. doi: 10.1007/s00404-003-0504-y. [DOI] [PubMed] [Google Scholar]
- 13.Stankovic ZB, Djurićić S, Stanković DS, et al. Minimal invasive treatment of cervical rhabdomyosarcoma in an adolescent girl. J BUON. 2007;12:121–123. [PubMed] [Google Scholar]
- 14.Hays DM, Shimada H, Raney RB, Jr, et al. Sarcomas of the vagina and uterus: the Intergroup Rhabdomyosarcoma Study. J Pediatr Surg. 1986;20:718–724. doi: 10.1016/s0022-3468(85)80032-4. [DOI] [PubMed] [Google Scholar]
- 15.Hays DM, Shimada H, Raney RB, Jr, et al. Clinical staging and treatment results in rhabdomyosarcoma of the female genital tract among children and adolescents. Cancer. 1988;61:1893–1903. doi: 10.1002/1097-0142(19880501)61:9<1893::aid-cncr2820610929>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 16.Vlahos NP, Matthews R, Veridiano NP. Cervical sarcoma botryoides: a case report. J Reprod Med. 1999;44:306–308. [PubMed] [Google Scholar]
- 17.Ghavimi F, Herr H, Jereb B, et al. Treatment of genitourinary rhabdomyosarcoma in children. J Urol. 1984;132:313–319. doi: 10.1016/s0022-5347(17)49607-8. [DOI] [PubMed] [Google Scholar]
- 18.Montag TW, D’Ablaing G, Schlaerth JB, et al. Embryonal rhabdomyosarcoma of the uterine corpus and cervix. Gynecol Oncol. 1986;25:171–194. doi: 10.1016/0090-8258(86)90098-3. [DOI] [PubMed] [Google Scholar]
- 19.Abu-Rustum NR, Sonoda Y. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma. Gynecol Oncol. 2007;104:S56–S59. doi: 10.1016/j.ygyno.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 20.Smith JR, Boyle DCM, Corless DJ, et al. Abdominal radical trachelectomy: a new surgical technique for the conservative management of cervical carcinoma. Br J Obstet Gynaecol. 1997;104:1196–1200. doi: 10.1111/j.1471-0528.1997.tb10946.x. [DOI] [PubMed] [Google Scholar]
- 21.Abu-Rustum NR, Su W, Levine DA, et al. Pediatric radical abdominal trachelectomy for cervical clear cell carcinoma: a novel surgical approach. Gynecol Oncol. 2005;97:296–300. doi: 10.1016/j.ygyno.2004.12.050. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez M, Guimares O, Rose PG. Radical abdominal trachelectomy and pelvic lymphadenectomy with uterine conservation and subsequent pregnancy in the treatment of early invasive cervical cancer. Am J Obstet Gynecol. 2001;185:370–374. doi: 10.1067/mob.2001.115866. [DOI] [PubMed] [Google Scholar]
- 23.Palfalvi L, Ungar L, Boyle DCM, et al. Announcement of healthy baby boy born following abdominal radical trachelectomy. Int J Gyncol Cancer. 2003;13:250. doi: 10.1046/j.1525-1438.2003.13049.x. [DOI] [PubMed] [Google Scholar]