Abstract
Recent evidence suggests that one possible cause of disparities in health outcomes for stigmatized groups is the implicit biases held by health care providers. In response, several health care organizations have called for, and developed, new training in implicit bias for their providers. This review examines current evidence on the role that provider implicit bias may play in health disparities, and whether training in implicit bias can effectively reduce the biases that providers exhibit. Directions for future research on the presence and consequences of provider implicit bias, and best practices for training to reduce such bias, will be discussed.
Keywords: health care, health disparities, implicit bias, bias reduction
A number of stigmatized social groups face broad and persistent health disparities. Many ethnic/racial groups, such as African Americans and American Indians, have shorter life expectancies than their White peers (e.g., Williams & Mohammed, 2009; but see Ruiz and colleagues (this issue) for an example of the “Hispanic Paradox”). Individuals with lower socio-economic statuses face increased risk of disease, and women are more likely to be the victims of rape and intimate partner violence and suffer from depression than men (e.g., Coker et al., 2002; Nolen-Hoeksema, 2001). Sexual orientation may also be another key factor in continued health disparities such that gay men, lesbian women, and bisexuals tend to have poorer health than their heterosexual counterparts (e.g., Dilley, Wynkoop Simmons, Boysun, Pizacani, & Stark, 2010).1
The causes for such disparities are linked to three broad factors: Genetic/biological antecedents, socioeconomic predictors, and psychological processes that contribute to biased health care (e.g., Adler & Rehkopf, 2008; Sankar et al., 2004; Schnittker & McLeod, 2005). Prominent among the psychological biases that have been discussed are the nonconscious or implicit prejudice and stereotypes held by health care providers. Despite their explicit commitment to providing equal care, some studies suggest that implicit prejudice and stereotyping can impact the judgment and behavior of health care providers when they interact with stigmatized patients (e.g., Green et al., 2007; see Chapman, Kaatz, & Carnes , 2013, for a review). To address this problem, several health care organizations have proposed, and in some cases tested, new approaches to raising awareness and providing skills for reducing implicit bias in patient care. Not surprisingly, most of the research on implicit bias in health care draws heavily from the theories and research methods developed by social psychology for the study of intergroup processes. Indeed, many social psychologists directly collaborate on the work being done to document and prevent implicit bias in health care.
The purpose of this paper is to provide an overview of the research on implicit bias among health care providers and the steps being taken to develop interventions to reduce such bias using articles found on the PsycINFO, PubMed, and Google Scholar search databases. We also highlight gaps in the scientific literature, and suggest future directions for research on the role of implicit bias in creating disparities for stigmatized patients.
Persistent Concerns About Bias in Health Care Delivery
One of the more troubling explanations for continuing health disparities is bias on the part of health care providers (Smedley, Stith, & Nelson, 2002; van Ryn & Fu, 2003). Although bias seems anathema to the profession, this has not always been the case. For example, the Tuskegee Syphilis Study of Untreated Syphilis in the Negro Male (1932 to 1972) was a long running study conducted by the United States Public Health Service in which hundreds of African American men infected with syphilis were studied to understand the life history of the disease. Not only were the men unaware that they had the disease, but they were never given treatment to cure it—even though the treatment had become commonplace while the study was being conducted. The effects of the Tuskegee Study can still be seen today in that African Americans who have knowledge of the study report greater medical and research mistrust (Freimuth et al., 2001; Shavers, Lynch, Burmeister, 2000).
Three converging lines of evidence make it difficult to dismiss provider bias as playing some role in creating or maintaining health disparities. First, ethnic/racial differences in care have been observed even after economic, educational, and access differences were accounted for, leading some to conclude that bias must be at work (e.g., Kressin & Petersen, 2001; Sheifer, Escarce, & Schulman, 2000). Second, careful examinations of providers’ perceptions of actual patients showed that African American patients were perceived in more negative terms than white patients (e.g., Finucane & Carrese, 1990; van Ryn & Burke, 2000). Finally, controlled experiments have found that providers’ perceptions and treatment recommendations for hypothetical Black patients differed significantly from those made for hypothetical White patients with the exact same symptoms (for a review see Paradies, Truong, & Priest, 2013).
Another source of evidence that cannot be ignored is the consistent finding that ethnic/racial minorities report greater dissatisfaction with their health care providers — especially when the providers are not of the same ethnicity (i.e., typically white) — and they perceive significantly more bias in health care compared to Whites (e.g., Cooper et al., 2003; Cooper-Patrick et al., 1999; LaVeist, Nickerson, & Bowie, 2000; Saha, Komaromy, Koepsell, & Bindman, 1999). A national survey by The Commonwealth Fund (Collins et al., 2002) found that compared to Whites, Hispanics and African Americans were nearly twice as likely to report problems communicating with their providers, 14 times more likely to believe that they would receive better health care if they were of a different ethnicity, and nearly twice as likely to feel that they had been treated with disrespect during a recent health care visit.
Based on this evidence and increasing awareness of the subtle ways in which bias may affect judgment and behavior, a ground-breaking report by the Institute of Medicine (IOM; Smedley et al., 2002) concluded that unrecognized or implicit bias among health care providers may contribute to health disparities, but additional research was needed to provide more direct evidence on the processes at work.
Direct evidence of biased attitudes and stereotypes among health care providers
The IOM report was based on inferences drawn from observational or survey data within the field of medicine, and evidence provided by (non-medical) social psychology studies. The latter providing the strongest evidence that implicit (if not explicit) intergroup bias is implicated in worse interpersonal interactions and biased behavior (e.g., Fazio, Jackson, Dunton, & Williams, 1995; Kawakami, Dovidio, & Gaertner, 2002). In the time since the IOM report was published, however, numerous studies have provided direct evidence on the attitudes and beliefs of health care providers.
Implicit attitudes among health care providers
Consistent with other populations, health care providers demonstrate implicit biases indicative of more negative attitudes toward African Americans than Whites (Blair et al., 2013a; Cooper et al., 2012; Green et al., 2007; Haider et al., 2011, 2015a, 2015b; Hausmann et al., 2015; Oliver, Wells, Joy-Gaba, Hawkins, & Nosek, 2014; Sabin, Nosek, Greenwald, & Rivara, 2009; Schaa, Roter, Biesecker, Cooper, & Erby, 2015; Stepanikova, 2012; for null effects, see Penner et al, 2010; Sabin, Rivara, & Greenwald, 2008), more negative attitudes toward Latinos than Whites (Blair et al., 2013a, 2013b; Stepanikova, 2012), and somewhat more negative attitudes toward Native Americans than Whites (Sabin, Moore, Noonan, Lallemand, & Buchwald, 2015). Health care providers also exhibit negative implicit biases against overweight/obese individuals (Phelan et al., 2014; Sabin, Marini, & Nosek, 2012; Teachman & Brownell, 2001; Waller, Lampman, & Lupfer-Johnson, 2012), gay and lesbian people (Burke et al., 2015; Sabin, Riskind, Nosek, 2015), lower social class (Haider et al., 2011, 2015a, 2015b), injecting drug users (von Hippel, Brener, & von Hippel, 2008), and wheelchair users with spinal cord injuries (Galli, Lenggenhager, Scivoletto, Molinari, & Pazzagila, 2015).
Implicit stereotypes among health care providers
Although the majority of the research has focused on attitudes (i.e., positive/negative associations), a handful of studies have explored specific implicit associations and stereotypes of stigmatized groups. Research suggests that health care providers implicitly hold associations that African American patients are less compliant and less cooperative in medical settings than White patients, despite the fact that the health care providers were not provided with evidence that African American patients are especially noncompliant or uncooperative (Green et al., 2007; Sabin & Greenwald, 2012; Sabin et al., 2008). What is more, research does not support the association that African American patients are more noncompliant in health care settings (e.g., Steiner et al., 2009). Diseases stereotypically associated with African Americans (e.g., sickle cell anemia, HIV, drug abuse) were also recognized faster by providers following subliminal presentation of Black than White faces (Moskowitz, Stone, & Childs, 2012). Although some diseases may possess a genetic component and thus reflect an accurate stereotype, physicians’ responses demonsrated inaccurate (e.g., drug abuse) as well as accurate (e.g., sickle cell anemia) disease stereotypes. Bean and colleagues (2013) further showed stereotypes of Hispanics among nursing and medical students, who were faster to respond to words associated with noncompliance and risky health behavior following subliminal images of Hispanics than Whites. Importantly, Bean and colleagues suggested that these stereotypes may stem from health care providers perceiving communication difficulties as a barrier when treating Hispanic patients (Lipton, Losey Giachello, Mendez, & Girotti, 1998). Health care providers, in the absence of any validating information, have also been found to implicitly stereotype obese people as more lazy, stupid, and worthless than thin people (Schwartz, O’Neal Chambliss, Brownell, Blair, & Billington, 2003).
Explicit attitudes and stereotypes among health care providers
Despite the numerous findings of health care providers showing implicit bias toward stigmatized groups, the findings on explicit or more controlled forms of bias generally show relatively low or even reversed bias. For example, Blair and colleagues (2013a) found that while doctors held implicit bias against Latino and African American patients, negative explicit attitudes against these groups were virtually nonexistent. In other research, health care providers explicitly reported that African American patients are no more likely than White patients to be noncooperative (Green et al., 2007). However, some studies have found indications of explicit bias by health care providers. Cooper at al. (2012) found that providers explicitly stereotyped African American patients as less cooperative than White patients, even though the providers had similar explicit attitudes toward both groups. When asked about what most health care providers believe, Bean et al. (2014) found that medical and nursing students perceived Hispanic and American Indian patients as engaging in more risky health behavior and as more noncompliant than White patients.
In general, then, health care providers appear to have many of the same attitudes and beliefs toward stigmatized groups as found in other populations, with higher levels of implicit than explicit bias (Blair et al., 2013a; Galli et al., 2015; but see Peris, Teachman, & Nosek, 2008, for an example of providers showing less implicit mental health bias than non-providers). Importantly, although health care providers show mean levels of bias against stigmatized groups, there is wide variance from provider to provider. For example, White, Hispanic, and Asian health care providers exhibited moderate levels of implicit bias toward African Americans whereas African American health care providers showed no such implicit bias (Sabin et al., 2009). Moreover, Sabin and colleagues found that, in general, male health care providers showed greater implicit racial bias than did female health care providers. Other findings show that higher BMI, as well as male, health care providers had less implicit bias toward obese individuals (Sabin et al., 2012; Schwartz et al., 2003), and providers with more contact with patients with spinal cord injuries showed less implicit biased toward wheelchair users (Galli et al., 2015).
Associations between implicit bias and medical judgments/treatment
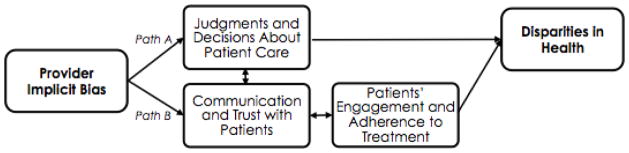
Does the level of bias of a particular provider matter in the perception and treatment of patients? As noted earlier, previous studies outside of health care have examined how implicit bias relates to biased judgment and behavior in other domains (e.g., Dovidio et al., 2002). Based on that work, researchers have developed a general model on the ways in which provider bias may contribute to health disparities (Blair, Steiner, & Havranek, 2011; Dovidio et al., 2008; van Ryn, 2002; van Ryn & Fu, 2003; see Figure 1). As shown in Figure 1, health care providers’ implicit bias may contribute to disparities through two paths. In Path A, providers’ implicit bias may affect their judgments and medical decisions regarding patients in their care (i.e., worse for stigmatized patients), with downstream consequences for health disparities. In Path B, providers’ implicit bias may negatively impact their communication and interaction with stigmatized patients, impacting the patients’ perceptions, judgments, and trust with their provider; this in turn would impact the patients’ engagement and adherence to treatment and increase health disparities. Importantly, these two paths may interact with one another such that the poor medical decision-making by the provider in Path A may undergird negative communication and mistrust with the patient (and visa versa).
Figure 1.
Model of paths through which provider implicit bias may contribute to health disparities.
Most of the research that has been conducted to test Path A has presented health care providers with hypothetical clinical cases that, randomly assigned, vary in the patients’ social group membership (e.g., White vs. Black). The researchers then examine the extent to which providers’ implicit biases correlate with judgments and decisions, according to the patients’ group membership. Consider, for example, a highly cited study by Green and colleagues (2007), who found that medical residents with greater implicit racial bias were less likely to recommend thrombolysis (“clot-busting”) treatment for a Black patient suffering from chest pain in a hypothetical scenario; implicit racial bias did not relate to treatment recommendations for a White patient with the same symptoms.
Research published since Green et al. (2007), however, has revealed a more complex picture. Studies show that providers’ implicit bias predicts some, but not all, medical judgments. For example, Sabin and Greenwald (2012) found that providers’ implicit race bias predicted less prescribed postsurgical pain medication for African American than White patients, but implicit race bias did not predict race differences in decisions for other medical issues, such as treatment of urinary tract infections, attention deficit hyperactivity disorder, and asthma. Many other studies have failed to find any association between providers’ implicit race or class biases and their medical judgments (Haider et al., 2011, 2015a, 2015b; Oliver et al., 2014; Sabin et al, 2008).
Only one study has investigated providers’ implicit bias and actual medical treatment, rather than responses to a hypothetical scenario. Blair and colleagues (2014) assessed implicit bias among experienced providers and then examined the medical records of a random sample of patients diagnosed with hypertension (stratified by ethnicity/race). An analysis of patients’ medications showed that increases in treatment intensification — physicians’ decisions to start a new medication or increase medication dosage when hypertension persists — for minority (versus White) patients bore no relation to providers’ implicit biases. Furthermore, although hypertension control was worse among African American than White patients, this difference was also unrelated to their providers’ implicit biases.
Considering the evidence thus far, it appears that provider bias may play only a limited role in explaining ethnic/racial health disparities through providers’ medical judgments and decisions (Pathway A in Figure 1). This finding is consistent with laboratory research that shows stronger associations between implicit bias and nonverbal behavior than explicit statements or judgments (Dovidio et al., 2002; Fazio et al., 1995). Many decisions about specific medications and treatment options are based on practice guidelines that leave little room for the influence of providers’ feelings and beliefs. Additional research is needed that directly compares these types of decisions with those that allow for more discretion in providers’ decision-making (e.g., giving narcotics for pain management, recommending a novel treatment that may be more effective but requires strict adherence and follow-up).
In addition, the majority of research on bias in medical decision-making has been conducted through hypothetical scenarios. Although a hypothetical scenario may accurately reflect some types of decision scenarios (i.e., careful consideration of written information, no time limit, and judgments that one knows will be carefully analyzed by researchers), other decisions are made under more stressful and ambiguous conditions (e.g., addressing pain complaints in a busy, understaffed emergency department). The one study to date that examined real patient care by Blair and colleagues (2014) was conducted under conditions that are likely to mitigate bias: a primary care setting in which patients and providers developed working relationships over the course of many years; processes and outcomes that were made over time, with many opportunities for adjustment; strong organizational expectations for meeting hypertension control guidelines and awareness of the problem of uncontrolled hypertension, particularly among African Americans. Implicit bias may be more likely to affect care delivered outside of established relationships, or in decisions made under time pressure, with limited information and without the benefit of clear guidelines (Burgess et al., 2007; Stepanikova, 2012).
Evidence on associations between implicit bias and patients’ perceptions and behavior
The second pathway (B) through which provider bias may contribute to health disparities, as shown in Figure 1, focuses on the effect of implicit bias on interpersonal communication. As noted previously, a number of lab studies have shown that people with more implicit ethnic/racial bias have poorer interpersonal interactions with minority individuals, often in very subtle ways (e.g., Dovidio et al., 2002). In the medical context, such interactions may impact the providers’ ability to accurately assess the patients’ views on treatment plans and curtail productive discussion, especially if the topic is sensitive (e.g., the need for lifestyle changes or the use of drugs and alcohol). On the patient side, a poor interaction due to provider bias could undermine trust and engagement in care, leading to less follow-up and worse adherence to the treatment plan.
Several studies have shown that African American patients report less positive clinical interactions with providers who have higher levels of implicit bias favoring Whites over Blacks (Blair et al., 2013b; Cooper et al., 2012; Penner et al., 2010). For example, Blair and colleagues (2013b) examined the association between providers’ implicit ethnic/racial bias and their patients’ perceptions of the “patient centeredness” of their provider during medical visits. African American patients in this study consistently rated their providers lower on interpersonal treatment, communication, trust, and knowledge of the patient to the extent that the providers had more implicit bias. However, the study found no association between Latino patients’ perceptions of their providers and their providers’ implicit bias against Latinos, suggesting that implicit bias may not be expressed or may not be perceived in the same way with different groups.
Other researchers have attempted to assess provider behaviors more objectively. For example, Cooper and colleagues (2012) measured providers’ implicit prejudice and stereotyping of African Americans and then audio-recorded their clinical visits with African American and White patients. These recordings were subsequently coded for possible behavioral indicators of bias, such as verbal dominance, amount of patient-centered communication, and length of the clinical visit. Although providers’ implicit race bias showed some associations to these behavioral indicators with African American patients, the same bias also predicted similar outcomes with White patients. Interestingly, African American and White patients differed in their perceptions of providers with greater implicit bias, with African American patients reporting worse interactions with biased providers than White patients. Thus, providers’ implicit bias may have a negative impact on clinical visits with both African American and White patients, but the providers’ implicit bias may especially damage the perceptions of African American patients.
Another study found a similarly complex view of providers’ implicit bias predicting more objective behaviors. In a partial re-analysis of the Penner et al. (2010) data, Hagiwara and colleagues (2013) measured the amount of time that providers talked during the clinical interaction compared to the amount of time that the patients talked (i.e., talk-time ratio). Results revealed that providers with more implicit bias had higher talk-time ratios (greater dominance) with African American patients. However, this dominance during the interaction was positively related to patient adherence with medications 16 weeks later. As speculated by Hagiwara and colleagues, this pattern may reflect the influence of a third variable (past experiences with discrimination) that could have affected how much the patients asserted themselves during the interaction and their subsequent (lower) adherence. Note that while Cooper et al. (2012) provided a White patient reference group, there was no such comparison group included in Hagiwara and colleague’s analysis.
To summarize, research shows that providers’ implicit bias is a relatively consistent predictor of ethnic/racial differences in patients’ subjective experiences with their health care providers, at least for African American patients. However, objective indicators of specific provider behaviors involved in these experiences have been more difficult to pin down (but see Hagiwara et al., this issue). One may certainly argue that the patients’ perception of the situation is more important than objective events when it comes to trust and willingness to follow treatment recommendations or engage further with the health care system. Indeed, a vast amount of research shows that perceived discrimination may undermine health among stigmatized groups (for a review see Pascoe & Richman, 2009).
Importantly, additional work is needed on the conditions under which provider bias is more or less likely to affect communication with patients. Basic research suggests a number of moderating conditions that have yet to be mapped on to medical practice (see Perugini, Richetin, & Zogmaister, 2010). Similarly, little is known about the ways in which the effects of provider bias may be exacerbated by patient characteristics. Patients who have experienced many prior episodes of bias in other settings (e.g., school or work) may be particularly sensitive to implicit bias in the medical setting (Hagiwara et al., this issue); or, a patient who is assertive or challenges the providers’ judgment may be more likely to activate provider bias. We turn next to examine the work being done to help providers understand the experiences of stigmatized patients.
Reducing implicit bias among health care providers
In response to the evidence that health care providers exhibit implicit bias, and that it may affect patients’ perceptions of their care, health care organizations and faculty are developing and testing new training in implicit bias for health care providers. Several papers describe best practices for helping students in health care learn about their biases, and emerging research indicates that adopting approaches developed for reducing implicit bias in STEM and other fields show promise for reducing implicit bias in health care.
Research suggests that contemporary approaches to teaching cultural competence and minority health are generally insufficient to reduce implicit bias among health care providers. Several reviews, including the section above, indicate that implicit prejudice and stereotyping is present when students begin training in health care, and that the level of implicit bias remains constant or increases as students matriculate through their training (see Chapman et al., 2013). Rubineau and Kang (2012) reported significant increases in medical students’ disparate behaviors toward Black standardized patients between their first and second years of medical school. Results from the CHANGES project, a four-year longitudinal study that tracked implicit and explicit bias among 3959 students across 49 medical schools in the United States, revealed similar shortcomings in medical training. For example, Phelan and colleagues (2014) found that whereas implicit bias toward obese patients remained constant, explicit bias increased during the four years of medical school. Also using the CHANGES data set, van Ryn and colleagues (2015) identified several factors that predicted increases in implicit bias during medical school, such as having heard negative comments from supervising medical staff about African American patients, and having had unfavorable contact with African American physicians. Although the van Ryn paper reported that formal training in minority health or cultural competence showed small, but significant, relationships to reduced implicit bias during medical school, these effects were eliminated after controlling for other variables.
Most educational interventions designed to reduce implicit bias appear to use a two-step approach that includes (1) making the students aware of their implicit biases, and (2) providing instruction on strategies they can use to either reduce the activation of implicit associations, or control how those associations influence judgment and behavior (Burgess, van Ryn, Dovidio, & Saha, 2007; Blair et al., 2011; Stone & Moskowitz, 2011; Teal et al., 2012). At this writing, only a handful of studies have examined whether teaching single or multiple strategies for reducing implicit bias is effective among health care providers.
Bias awareness strategies
Self-reflection activities that challenge self-perceptions are a common educational tool for helping students in health care become aware of bias (Teal et al., 2012). However, research suggests that awareness, by itself, may not always change the way health care providers think about stigmatized patient groups (Chapman et al., 2013). For example, Teal and colleagues (2010) had medical students complete a Black/White race Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998) and then participate in peer discussion groups to discuss their experience with the IAT and their observations about implicit bias during ongoing clinical experiences. The results suggested that whereas students improved their awareness of provider-focused strategies for reducing implicit bias, they reported less interest in using patient-focused strategies like perspective-taking. In a similar approach, Gonzalez and colleagues (2014) exposed medical students to a single session about the role of provider implicit bias in health disparities. Participants read papers on the topic, completed an IAT and self-reflection exercises, and discussed their perspectives in class. Whereas the majority of students reported positive attitudes and beliefs about implicit bias, 22% of the sample doubted the validity of the IAT and the existence of health disparities overall. In contrast, van Ryn and colleagues (2015) reported that having completed an IAT (with feedback) was a significant predictor of decreases in implicit bias after controlling for instruction in cultural competence and minority health. Overall, these results suggest that being made aware of implicit bias through self-reflection activities, like feedback from an IAT, may motivate health care providers to address their implicit biases, but perhaps only if the feedback and reflection activity does not induce the defensiveness that can lead them to deny their bias, or counter-argue the issue of disparities.
Control strategies
One way to reduce provider resistance to learning about implicit bias is by instructing them in strategies for controlling their automatic responses to stigmatized patients, such as affirming egalitarian goals, seeking common-group identities, perspective-taking, and individuation via counter-stereotyping (Burgess et al., 2007; Blair et al., 2011; Stone & Moskowitz, 2011). A recent study by Lai and colleagues (2014) comparing these and other strategies suggests that seeking counter-stereotypic and common-identity information (e.g., shifting group affiliations or boundaries) may be especially effective for reducing implicit bias among a non-health care sample (also see Prati and colleagues (this issue) for an example of cross-categorization as a tool to garner majority support for immigrant access to health services). The authors also concluded that the success of any approach requires active involvement or engagement when using the strategy.
Perspective-taking strategies
Perspective-taking is a common clinical skill taught in most health care training programs. Instruction in perspective-taking shows positive effects on implicit bias in laboratory studies (Todd & Galinsky, 2012) and among health care providers (Drwecki et al., 2011). For example Blatt and colleagues (2010) showed that training medical students in perspective-taking improved African American patient satisfaction relative to control training. The authors suggest that learning about perspective-taking increased patient satisfaction across medical schools, clinical disciplines, and for interactions between racially diverse students and patients.
Use of multiple strategies
Other research outside of the health care domain suggests that exposing providers to multiple strategies could attenuate implicit bias both immediately after training, and in some cases, the effects might last for several weeks (Rudman, Ashmore, & Gary, 2001). Devine and colleagues (2012) developed a two-step intervention for college undergraduates in which, after making the participants aware of their implicit prejudice toward African Americans through IAT feedback, they instructed participants in the use of stereotype-replacement thinking, counter-stereotypic imaging, seeking individuating information, perspective-taking, and how to increase positive contact with out-group members. The results showed that participants who completed the intervention reported significantly lower implicit prejudice toward African Americans at 4 and 8 weeks, compared to participants in a control intervention group.
Stone and colleagues (2015) tested a similar two-step approach in a series of workshops with first-year medical students. The students first completed a Hispanic-White/non-compliance IAT (without feedback) and read an article about implicit bias in medicine. The next week, all attended a lecture on implicit bias and learned about their own implicit biases by completing a classroom IAT demonstration. Two days later, the students participated in a team learning activity during which they discussed and developed implementation intentions for activating egalitarian goals, seeking common-identity and counter-stereotypic information, and for taking their patient's perspective during a clinical encounter. When they completed the same IAT three to seven days following the workshops, the results showed that participants demonstrated significantly less implicit stereotyping of Hispanics. The lasting effect of this and the intervention in Devine et al. (2012) supports the call for developing training modules that, in addition to making providers aware of their biases, provide instruction in how to control implicit bias, and features active learning exercises for practicing the new skills.
Promoting bias reduction at an institutional level
Finally, health care institutions can make changes that facilitate implicit bias reduction. Recent research indicates that positive intergroup contact is associated with reduction in implicit bias in a health care context (Burke et al., 2015; van Ryn et al., 2015). These studies suggest that implicit bias may fade when health care training features opportunities for positive contact across group boundaries (provider — patient; student — faculty).
Suggestions for future reduction strategies
While the research above suggests that interventions can reduce implicit bias among health care providers, more empirical work is needed. One area to investigate is how to provide information and feedback about implicit bias without causing defensive resistance to the issue. The available data suggest that simply confronting providers with evidence of their implicit biases may not, in and of itself, be sufficient to motivate them to change the way they think about, and interact with, stigmatized patients. Students in training may perceive information and feedback about implicit bias as assigning blame and responsibility for health disparities, which is likely inconsistent with their egalitarian goals to provide the best care possible to all patients (Burgess et al., 2007). However, research suggests that students may be more open to learning about their own biases, and accepting responsibility for changing them, if instructors start by activating and affirming their egalitarian goals and commitment to provide equal care, before having them engage in self-reflection activities or receive feedback from an IAT (Harris, Mayle, Mabbott, & Napper, 2007; Howell & Sheppard, 2012). Emphasizing from the start that reducing disparities is a shared responsibility, and that providers can learn to control their implicit responses to stigmatized patients, may also encourage openness and acceptance of the information (Moss-Rascusin et al., 2014)
It is also important to examine how best to train health care providers in the use of strategies for reducing implicit bias. The current literature suggests that there are two key elements for success: (1) instructors need to translate the abstract, theoretical concepts and processes that support the effectiveness of the strategies into practical, concrete clinical skills, and (2) instructors need to develop active learning exercises that allow students the opportunity to practice the skills before they use them in the clinic. But it is not clear which strategies, either in isolation or combination, work best for reducing implicit bias in patient care (Lai et al., 2012; Devine et al., 2012). It may be that some strategies (e.g., seeking counter-stereotypic information; perspective-taking) are relatively easy to use and more effective in a clinical setting than others (e.g., stereotype-replacement), but that there are clinical settings in which using any strategy would be difficult to employ (e.g., during an emergency room triage). Moreover, examining reduction strategies for patient groups who are not stigmatized due to race/ethnicity (e.g., obese individuals, gay and lesbian people, individuals with physical disabilities) may lend further insight into which type of strategies are more effective for treatment of different patient groups. Understanding the parameters to using implicit bias reduction strategies in a clinical setting and toward a variety of stigmatized patient groups is vital for helping providers adopt them in their practices.
Finally, the ultimate goal of training providers to reduce implicit bias is to reverse the disparities in care that many stigmatized patient groups receive. It is therefore critical to examine if any reductions in implicit bias, observed after providers receive training in bias reduction, subsequently translate into more positive outcomes for stigmatized patient groups. Indeed, real changes in patient care may not occur with a one-time training in the first year of medical or nursing school; students may need continued exposure to an implicit bias curriculum in each year of their training in order to fully integrate the information into the other knowledge and skills they learn for patient care. Naturally, extended training will require a relatively high level of commitment, in terms of instruction time and resources, by health care training programs (Penner, Blair, Albrecht, & Dovidio, 2014). Nevertheless, integrating instruction on implicit bias into existing health care training appears necessary to address the role that providers may play in creating disparate care for stigmatized patients.
Conclusions
The evidence in this review suggests that, similar to the general population, health care providers in the U.S. have implicit negative attitudes and stereotypes about many stigmatized groups. Only recently have efforts been made to directly investigate whether provider implicit bias contributes to the health disparities experienced by these groups. Whereas some studies suggest that provider bias may negatively impact clinical interactions with stigmatized patients, provider bias has not been consistently linked to worse medical judgment and decisions. More research is needed to document the conditions under which these processes play out in different clinical settings, with different patient populations.
Research on best practices for addressing and reducing implicit bias in health care is also underway. While recent papers describe several interventions that may effectively translate when training future and current providers, there is an urgent need for more research to test the extent to which these interventions are effective, both immediately and during the course of health care delivery. A stronger understanding of how provider implicit bias influences clinical care, and how to motivate providers to adopt strategies for controlling implicit bias, could play an important role in the reduction of disparities in health care for stigmatized patient groups.
Acknowledgments
This publication was supported in part by the American Heart Association in an award to the second author (15SFDRN24180024) and by The National Institute on Minority Health and Health Disparities of the National Institutes of Health in an award to the last author (R01MD008940).
Footnotes
Although the problem of health disparities affect a variety of groups, much of this review will focus on ethnic/racial groups because there is very little research on health care bias with other groups. We include research with other groups where it exists.
Contributor Information
Colin A. Zestcott, University of Arizona
Irene V. Blair, University of Colorado Boulder
Jeff Stone, University of Arizona.
References
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2006;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Bean MG, Focella ES, Covarrubias R, Stone J, Moskowitz GB, Badger TA. Documenting nursing and medical students’ stereotypes about Hispanic and American Indian patients. Journal of Health Disparities Research and Practice. 2014;7:14–22. [PMC free article] [PubMed] [Google Scholar]
- Bean MG, Stone J, Badger TA, Focella ES, Moskowitz GB. Evidence of nonconscious stereotyping of Hispanic patients by nursing and medical students. Nursing Research. 2013;62:362–367. doi: 10.1097/NNR.ob013e31829e02ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair IV, Havaranek EP, Price DW, Hanratty R, Fairclough DL, Farley T, Hirsh HK, Steiner JF. Assessment of biases against Latinos and African Americans among primary care providers and community members. American Journal of Public Health. 2013a;103:92–98. doi: 10.2105/AJPH.2012.300812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair IV, Steiner JF, Hanratty R, Price DW, Fairclough DL, Daugherty SL, Bronsert M, … Havranek EP. An investigation of associations between clinicians’ ethnic and racial bias and hypertension treatment, medical adherence and blood pressure control. Journal of General Internal Medicine. 2014;29:987–995. doi: 10.1007/s11606-014-2795-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair IV, Steiner JF, Havranek EP. Unconscious (implicit) bias and health disparities: where do we go from here? The Permanente Journal. 2011;15:71–78. doi: 10.7812/tpp/11.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair IV, Steiner JF, Fairclough DL, Hanratty R, Price DW, Hirsh HK, Wright LA, … Havranek EP. Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Annals of Family Medicine. 2013b;11:43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blatt B, LeLacheur SF, Galinsky AD, Simmens SJ, Breenberg L. Does perspective-taking increase satisfaction in medical encounters? Academic Medicine. 2010;85:1445–1452. doi: 10.1097/ACM.0b013e3181eae5ec. [DOI] [PubMed] [Google Scholar]
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: Lessons from social-cognitive psychology. Journal of General Internal Medicine. 2007;22:882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, Nelson DB, van Ryn M. Do contact and empathy mitigate bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Academic Medicine. 2015;90:645–651. doi: 10.1097/ACM.0000000000000661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. Journal of General Internal Medicine. 2013;28:1504–1510. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2000;24:260–268. doi: 10.1016/S0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Collins KS, Hughes DL, Doty MM, Ives BL, Edwards JN, Tenney K. Findings from the Commonwealth Fund 2001 Health Care Quality Survey. New York, NY: The Commonwealth Fund; 2002. Diverse communities, common concerns: Assessing health care quality for minority Americans. [Google Scholar]
- Cooper LA, Johnson RDL, Ford DE, Steinwache DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Thi Vu H, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Devine PG, Forscher PS, Austin AJ, Cox WTL. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology. 2012;48:1267–1278. doi: 10.1016/j.jesp.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilley JA, Wynkoop Simmons K, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific Northwest. American Journal of Public Health. 2010;100:460–467. doi: 10.2105/AJPH.2007.130336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. Journal of Personality and Social Psychology. 2002;82:62–68. doi: 10.1037/0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Drwecki BB, Moore CF, Ward SE, Prkachin KM. Reducing racial disparities in pain treatment: the role of empathy and perspective taking. Pain. 2011;152:1001–1006. doi: 10.1016/j.pain.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Fazio RH, Jackson JR, Dunton BC, Williams CJ. Variability in automatic activation as an unobtrusive measure of racial attitudes: A bona fide pipeline? Journal of Personality and Social Psychology. 1995;69:1013–1027. doi: 10.1037/0022-3514.69.6.1013. [DOI] [PubMed] [Google Scholar]
- Finucane TE, Carrese JA. Racial bias in presentation of cases. Journal of General Internal Medicine. 1990;5:120–121. doi: 10.1007/BF02600511. [DOI] [PubMed] [Google Scholar]
- Freimuth VS, Quinn SC, Thomas SB, Cole G, Zook E, Duncan T. African Americans’ views on research and the Tuskegee syphilis study. Social Science & Medicine. 2001;52:797–808. doi: 10.1016/S0277-9536(00)00178-7. [DOI] [PubMed] [Google Scholar]
- Galli G, Lenggenhager B, Scivoletto G, Molinari M, Pazzagila M. Don’t look at my wheelchair! The plasticity of longlasting prejudice. Medical Education. 2015;49:1239–1247. doi: 10.1111/medu.12834. [DOI] [PubMed] [Google Scholar]
- Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: A teaching program and survey of medical students. Teaching and Learning in Medicine. 2014;26:64–71. doi: 10.1080/10401334.2013.857341. [DOI] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its prediction of thrombolysis decisions for blacks and white patients. Journal of General Internal Medicine. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology. 1998;74:1464–1480. doi: 10.1037/0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Hagiwara N, Penner LA, Gonzalez R, Eggly S, Dovidio JF, Gaertner SL, West T, Albrecht TL. Racial attitudes, physician-patient talk time ratio, and adherence in racially discordant medical interactions. Social Science & Medicine. 2010;87:123–131. doi: 10.1016/j.socscimed.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider AH, Schneider EB, Sriram N, Dossick DS, Scott VK, Swoboda SM, Losonczy L, … Freischiag JA. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decision. Journal of the American Medical Association: Surgery. 2015a;150:457–464. doi: 10.1001/jamasurg.2014.4038. [DOI] [PubMed] [Google Scholar]
- Haider AH, Schneider EB, Sriram N, Scott VK, Swoboda SM, Zogg CK, Dhlman N, … Cooper LA. Unconscious race and social class bias among registered nurses: Vignette-based study using implicit association testing. Journal of the American College of Surgeons. 2015b;220:1077–1086. doi: 10.1016/j.jamcollsurg.2015.01.065. [DOI] [PubMed] [Google Scholar]
- Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, Swohoda S, Villegas CV, … Cornwell EE. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. Journal of the American Medical Association. 2011;306:942–951. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PR, Mayle K, Mabbott L, Napper L. Self-affirmation reduces smokers’ defensiveness to graphic on-pack cigarette warning labels. Health Psychology. 2007;26:437–446. doi: 10.1037/0278-6133.26.4.437. [DOI] [PubMed] [Google Scholar]
- Hausmann LRM, Myaskovsky L, Niyonkuru C, Oyster ML, Switzer GE, Burkitt KH, Fine MJ, … Boninger ML. Examining implicit bias of physicians who care for individuals with spinal cord injury: A pilot study and future directions. The Journal of Spinal Cord Medicine. 2015;38:102–110. doi: 10.1179/2045772313Y.0000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell JL, Shepperd JA. Reducing information avoidance through affirmation. Psychological Science. 2012;23:141–145. doi: 10.1177/0956797611424164. [DOI] [PubMed] [Google Scholar]
- Kressin NR, Peterson LA. Racial differences in the use of invasive cardiovascular procedures: Review of the literature and prescription for future research. Annals of Internal Medicine. 2001:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- Lai CK, Marini M, Lehr SA, Cerruti C, Shin JL, Joy-Gaba JA, Ho AK, … Nosek BA. Reducing implicit racial preferences: I. A comparative investigation of 17 interventions. Journal of Experimental Psychology: General. 2014;143:1765–1785. doi: 10.1037/a0036260. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Medical Care Research and Review. 2000;57:146–161. doi: 10.1177/1077558700574007. [DOI] [PubMed] [Google Scholar]
- Lipton RB, Losey LM, Giachello A, Mendez J, Girotti MH. Attitudes and issues in treating Latino patients with type 2 diabetes: Views of healthcare providers. The Diabetes Educator. 1998;24:67–71. doi: 10.1177/01457219802400109. [DOI] [PubMed] [Google Scholar]
- Moskowitz GB, Stone J, Childs A. Implicit stereotyping and medical decisions: Unconscious stereotype activation in practitioners’ thoughts about African Americans. American Journal of Public Health. 2012;102:996–1001. doi: 10.2105/AJPH.2011.300591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss-Racusin CA, van der Toorn J, Dovidio JF, Brescoll VL, Graham MJ, Handelsman J. Scientific diversity interventions. Science. 2014;343:615–616. doi: 10.1026/science.1245936. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10:173–176. doi: 10.1111/1467-8721.00142. [DOI] [Google Scholar]
- Oliver MN, Wells KM, Joy-Gaba JA, Hawkins CB, Nosek BA. Do physicians’ implicit views of African Americans affect clinical decision making? Journal of the American Board of Family Medicine. 2014;27:177–188. doi: 10.3122/jabfm.2014.02.120314. [DOI] [PubMed] [Google Scholar]
- Paradies Y, Truong M, Priest N. A systematic review of the extent and measurement of healthcare provider racism. Journal of General Internal Medicine. 2013;20:364–387. doi: 10.1007/s11606-013-2583-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, Richman LS. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Blair IV, Albrecht TL, Dovidio JF. Reducing racial health care disparities: A social psychological analysis. Policy Insights From the Behavioral and Brain Sciences. 2014;1:204–212. doi: 10.1177/2372732214548430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Teachman BA, Nosek BA. Implicit and explicit stigma of mental illness: Links to clinical care. The Journal of Nervous and Mental Disease. 2008;196:752–760. doi: 10.1097/NMD.0b013e3181879dfd. [DOI] [PubMed] [Google Scholar]
- Perugini M, Richetin J, Zogmaister C. Prediction of behavior. In: Gawronski B, Payne BK, editors. Handbook of implicit social cognition: Measurement, theory, and applications. New York, NY: The Guildford Press; 2010. pp. 255–277. [Google Scholar]
- Phelan SM, Dovidio JF, Puhl RM, Burgess DJ, Nelson DB, Yeazel MW, … van Ryn M. Implicit and explicit weight bias in a national sample of 4,732 medical students: The medical student CHANGES study. Obesity. 2014;22:1201–1208. doi: 10.1002/oby.20687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubineau B, Kang Y. Bias in white: A longitudinal natural experiment measuring changes in discrimination. Management Science. 2012;58:660–677. doi: 10.1287/mnsc.1110.1439. [DOI] [Google Scholar]
- Rudman LA, Ashmore RD, Gary ML. “Unlearning” automatic biases: The malleability of implicit prejudice and stereotypes. Journal of Personality and Social Psychology. 2001;81:856–868. doi: 10.1037/0022-3514.81.5.856. [DOI] [PubMed] [Google Scholar]
- Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American Journal of Public Health. 2012;102:988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS ONE. 2012;7:e48448. doi: 10.1371/1/journal.pone.0048448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Moore K, Noonan C, Lallemand O, Buchwald D. Clinicians’ implicit and explicit attitudes about weight and race and treatment approaches to overweight for American Indian children. Childhood Obesity. 2015;11:456–465. doi: 10.1089/chi.2014.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin LA, Nosek BA, Greenwald AG, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Health Care for the Poor and Underserved. 2009;20:896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Riskind RG, Nosek BA. Health care providers’ implicit and explicit attitudes toward lesbian women and gay men. American Journal of Public Health. 2015;105:1831–1841. doi: 10.2105/AJPH.2015.302631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Medical Care. 2008;46:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Sankar P, Cho MK, Condit CM, Hunt LM, Koenig B, Marshall P, Lee SS, Spicer P. Genetic research and health disparities. Journal of the American Medical Association. 2004;291:2985–2989. doi: 10.1001/jama.291.24.2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaa KL, Roter DL, Biesecker BB, Cooper LA, Erby LH. Genetic counselors’ implicit racial attitudes and their relationship to communication. Health Psychology. 2015;34:111–119. doi: 10.1037/hea0000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheifer SE, Escarce JJ, Schulman KA. Race and sex differences in the management of coronary artery disease. American Heart Journal. 2000;139:846–857. doi: 10.1016/S0002-8703(00)90017-6. [DOI] [PubMed] [Google Scholar]
- Schnittker J, McLeod JD. The social psychology of health disparities. Annual Review of Sociology. 2005;31:75–103. doi: 10.1146/annurev.soc.30.012703.110622. [DOI] [Google Scholar]
- Schwartz MB, O’Neal Chambliss H, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obesity Research. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- Shavers VL, Lynch CF, Burmeister LF. Knowledge of the Tuskegee study and its impact on the willingness to participate in medical research studies. Journal of the National Medical Association. 2000;92:563–572. [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. National Academy Press; Washington, D.C: 2002. [PubMed] [Google Scholar]
- Steiner JF, Ho PM, Beaty BL, Dickinson LM, Hanratty R, Zeng C, … Estacio RO. Sociodemographic and clinical characteristics are not clinically useful predictors of refill adherence in patients with hypertension. Circulation Cardiovascular Quality and Outcomes. 2009;2:451–457. doi: 10.1161/CIRCOUTCOMES.108.841635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepanikova I. Racial-ethnic biases, time pressure, and medical decisions. Journal of Health and Social Behavior. 2012;53:329–343. doi: 10.1177/0022146512445807. [DOI] [PubMed] [Google Scholar]
- Stone J, Moskowitz GB. Non-conscious bias in medical decision making: What can be done to reduce it? Medical Education. 2011;45:768–776. doi: 10.1111/j.1365-2923.2011.04026.x. [DOI] [PubMed] [Google Scholar]
- Stone J, Moskowitz GB, Zestcott CA. A brief, active learning workshop for reducing implicit bias among medical students. 2015 doi: 10.1037/sah0000179. Manuscript in preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: Is anyone immune? International Journal of Obesity. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- Teal CR, Shada RE, Gill AC, Thompson BM, Fruge E, Villarreal GB, Haidet P. When best intentions aren’t enough: Helping medical students develop strategies for managing bias about patients. Journal of General Internal Medicine. 2010;25(Suppl 2):115–118. doi: 10.1007/s11606-009-1243-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd AR, Galinsky AD. Perspective-taking as a strategy for improving intergroup relations: Evidence, mechanisms, and qualifications. Social and Personality Psychology Compass. 2014;8:374–387. doi: 10.1111/spc3.12116. [DOI] [Google Scholar]
- van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine. 2000;50:813–828. doi: 10.1016/S0277-9536(99)00338-X. [DOI] [PubMed] [Google Scholar]
- van Ryn M, Fu SS. Paved with good intentions: Do public health and human service providers contribute to racial/ethnic disparities in health? American Journal of Public Health. 2003;93:248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M, Hardeman R, Phelan SM, Dovidio JF, Herrin J, Burke SE, … Przedworski JM. Medical school experiences associated with change in implicit racial bias among 3547 students: A medical student CHANGES study report. Journal of General Internal Medicine. 2015;30:1748–1756. doi: 10.1007/s11606-015-3447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Hippel W, Brener L, von Hippel C. Implicit prejudice toward injecting drug users predicts intentions to change jobs among drug and alcohol nurses. Psychological Science. 2008;19:7–11. doi: 10.1111/j.1467-9280.2008.02037.x. [DOI] [PubMed] [Google Scholar]
- Waller T, Lampman C, Lupfer-Johnson G. Assesing bias against overweight indiiduals among nursing and psychology students: An implicit association test. Journal of Clinical Nursing. 2012;21:3504–3512. doi: 10.111/j.1365-2702.2012.04226.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–57. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]