Abstract
The psychological processes associated with HIV infection in long-term relationships differ from those operative in casual sexual encounters, and relatively little research has considered the aspects of personality applicable in the ongoing heterosexual relationships in which women are at greatest risk. Sensitivity to rejection has been linked with efforts to prevent rejection at a cost to the self and therefore may be relevant to the health risks that many women incur in relationships. We examined the association of rejection sensitivity with women’s sexual risk behavior in a sample of women at heightened risk for HIV exposure. Women in long-term heterosexual relationships (N = 159) were recruited for study participation in the hospital emergency room serving a low-income neighborhood in New York City, in 2001–2003. Rejection sensitivity and known HIV risk factors were assessed using verbally administered questionnaires. Rejection sensitivity was associated with lower perceived relationship power and in turn, more frequent unprotected sex with a partner perceived to be at risk for HIV. These results held when controlling for other HIV risk factors including partner violence, economic dependence, and substance use. Understanding the association of rejection concerns with lower perceived personal power in relationships may be important for HIV prevention.
Keywords: Rejection Sensitivity, HIV, Sexual Relationship Power
INTRODUCTION
Women currently account for approximately a quarter of all people living with HIV/AIDS in the United States, and sexual contact with male partners is the primary route of women’s HIV infection. In 2010, 84% of the 9500 women newly diagnosed with HIV were infected through heterosexual contact (CDC, 2013). Women’s risk for contracting HIV from their long-term heterosexual partner is increased when they have low power in their relationships and society, such as when they are financially dependent and lack control over sexual/reproductive decisions (Hirsch et al., 2010; Wingwood & Clemente, 2000). Under these circumstances, women may learn that assertiveness is often unhelpful and potentially dangerous when in a relationship with a more powerful male partner. Given the role of one’s own power to negotiate sexual behavior in HIV prevention (Pulerwitz, Amaro, De Jong, Gortmaker & Rudd, 2002), it is no wonder that worldwide, the HIV risk within relationships is heightened in the context of structural inequalities based on gender, race/ethnicity, and social class (Zierler & Krieger, 1997).
Risk factors operating at a societal level are clearly important, but because each woman draws upon her experiences and current goals to process, understand and cope actively with the circumstances she faces, psychological factors increase HIV risk for some more than for others. Risk behaviors, including sex with multiple partners and unprotected sex, have been modestly correlated with person-level factors (Hoyle, Fejfar, & Miller, 2000; Sheeran, Abraham & Orbell, 1999). Yet, the personality traits that have received most research attention, such as impulsivity, play a much larger role in the first sexual encounter with a particular partner than in any subsequent ones (Cooper, 2010). Little work has addressed psychological influences on HIV exposure in the long-term heterosexual relationships that put many women at risk, and specifically, the factors that may exacerbate or ameliorate the conditions of unequal relationship power associated with the disproportionately high HIV risk among economically disadvantaged, minority women.
One such psychological influence may be rejection sensitivity (RS; Downey & Feldman, 1996), the extent to which one expects and fears rejection in personally significant relationships. For more than a decade, research has linked RS with hostility, conflict, and instability in intimate relationships (see Romero-Canyas, Downey, Berenson, Ayduk & Kang, 2010). More recent studies also have suggested that high RS may be associated with a greater sense of dependence on intimate partners and of lower perceived power in relation to them. RS has correlated with self-silencing in women, defined by suppressing expression of one’s concerns to “keep the peace” in a relationship (Jack & Dill, 1992). For example, RS was associated with the extent to which female college students accommodated an internet dating partner by downplaying interests and characteristics that conflicted with the partner’s preferences (Romero-Canyas, Reddy, Rodriguez & Downey, 2013). Moreover, people with high RS will go to great lengths to please others to protect and/or repair their relationships from the rejection threats that they so readily anticipate and perceive (e.g., Romero-Canyas, Downey, Reddy, et al., 2010). These strands of research led us to hypothesize that RS may be significantly associated with meaningful individual differences in women’s HIV risk behavior in their long-term relationships.
RS and the dangers of prioritizing the prevention of rejection
Purdie and Downey’s (2000) longitudinal study of economically disadvantaged, minority middle school girls was the first to show that RS prospectively predicted involvement in high-risk relationships because of its association with self-silencing accommodations. Scores on a measure of RS administered before the girls entered relationships predicted more conflict and hostility in both the girls and their partners one year later. Highly rejection-sensitive girls also reported more worry about their partner’s commitment, and willingness to forgo their own values to maintain their relationships. For example, they were more likely to endorse statements like “I would do anything to keep my boyfriend with me, even if it’s things that I know are wrong.” Research suggests, then, that rejection-sensitive women are highly invested in preventing rejection and will do so even at a cost to themselves. When extended into the sexual domain of a close relationship, these patterns can be expected to compromise the ability to negotiate for the protection of one’s own health. Indeed, a recent survey study of college students (76% female; Edwards & Barber, 2010) found that RS was associated with lower rates of condom use among those who wanted to use condoms but believed that their partners did not.
No previous work of which we are aware has examined the implications of RS for sexual health in a sample characterized by high structural risk factors for HIV. However, a previous study (Kershaw et al., 2007) considered the association of conceptually related variables – adult attachment – with sexual risk behavior in a sample of young, urban pregnant women. Like RS, adult attachment reflects the degree to which people feel insecure about acceptance in a relationship, focusing on the extent to which they characteristically demonstrate anxiety and avoidance responses to rejection concerns. Both the anxiety and avoidance dimensions of adult attachment were associated with believing that the partner would be upset if asked to use condoms and with lower self-efficacy for negotiating and implementing condom use. Attachment anxiety was also associated with less frequent use of condoms during sexual acts and with having had unprotected sex with a partner reported to be at risk for acquiring sexually transmitted diseases. This prior study is notable because little research has addressed rejection concerns in samples at high sexual risk. Yet it remains unclear to what extent the findings may be specific to pregnant women or explained by unmeasured risk factors that may be correlated with rejection concerns, such as partner violence, and economic dependence on the partner.
Multiple risks for HIV in socioeconomically disadvantaged women
Low-income, urban women are often simultaneously faced with several inter-related obstacles to effective HIV prevention (El-Bassel et al., 2007), all of which operate, in part, by diminishing their power in their relationships. Therefore, when considering the potential association of RS with diminished perceived relationship power and more frequent unprotected sex with high-risk partners, it is crucial to rule out these other variables as alternative explanations. In other words, it is important to test whether associations with RS are present above and beyond other correlated risk factors -- including partner violence, economic dependence on the partner, and substance use.
Violence is a means of enforcing an imbalance of power within a couple, and the atmosphere of terror it creates can readily overshadow other personal concerns. Not surprisingly, then, partner violence increases exposure to HIV through multiple pathways (e.g., Gielen, McDonnell & O’Campo, 2002). The sexually coercive behavior that often accompanies physical violence increases the woman’s exposure to sexually transmitted diseases (Wingwood & Clemente, 1997). In addition, a woman who has experienced partner violence may realistically fear retaliation for requesting that her partner use condoms, because he may interpret this request as a signal of mistrust or infidelity. Consistent with this idea, prospective data indicate that women who have experienced partner violence show declining efforts at HIV prevention in their relationships over time (El-Bassel, Gilbert, Wu, Go, & Hill, 2005).
Like partner violence, economic dependence on a male partner reflects an imbalance of power in a couple in which fears of the potential consequences of displeasing the partner often eclipse personal concerns. Indeed, economic dependence is one of the primary reasons women give for feeling compelled to stay in high-risk relationships (Newman, Williams, Massaquoi, Brown, & Logie, 2008). A recent study demonstrated an association between economic dependence and less frequent condom use that was mediated by the women less frequently requesting that their partner use condoms (Biello, Sipsma, Ickovics & Kershaw, 2010).
Substance use is also associated with increased risk for HIV and other sexually transmitted diseases in multiple ways that include diminished power over sexual decisions. Women’s substance use is associated with greater risk of partner violence and other forms of exploitation (Gilbert, El-Bassel, Chang, Wu & Roy, 2012); the need to maintain a drug supply and involvement in illegal subcultures may make dangerous relationships more difficult to avoid or escape (El-Bassel et al., 2005). The effect of intoxication itself on judgment increases the likelihood for several types of sexual risk, including sex with a greater number of partners, and reduced ability to insist effectively upon sexual protection. Finally, people who are most vulnerable to developing substance use problems often have co-existing psychosocial stressors, personality traits, and psychiatric difficulties that could also contribute to HIV risk behavior (Leigh & Stall, 1993). Thus, even while sober, people with a vulnerability to substance use disorders may still have more difficulties negotiating interpersonal situations and regulating behavior (El-Bassel, Gilbert, Vinocur, Chang, & Wu, 2011).
Current Research
To examine the association of RS with HIV risk in ongoing heterosexual relationships, we included a measure of RS in a larger study of individual differences in HIV risk among economically disadvantaged urban minority women, a demographic group that has elevated rates of HIV infection (*MASKED REFERENCE*). Based on literature linking RS with accommodating others at a cost to the self, we hypothesized that there would be an association between RS and high-risk sexual behavior that would be mediated by lower perceived power in the sexual relationship. In other words, RS would be associated with lower power over relationship decisions, and in turn, lower relationship power would explain the association between RS with high-risk sex in relationships. In testing our hypotheses about high-risk sexual behavior, we focused on the frequency of unprotected sex with a long-term partner who was perceived as at risk for transmitting HIV. Although women who had unprotected sex with partners they perceived as having absolutely no HIV risk may also have been putting themselves in danger of contracting HIV, they lacked awareness that they were doing so. Only when the partner was perceived as at risk should the interpersonal patterns associated with RS have made a difference, because it was only in this circumstance that having unprotected sex conflicted with what women knew was best for their health. Previous research has similarly taken into account that not all unprotected sex is equally high-risk (e.g., Kershaw et al., 2007).
Finally, because the sample faced high levels of known risk factors for HIV (including intimate partner violence, economic dependence on the partner, and substance use), analyses were conducted to verify that these factors did not account for the associations with RS.
METHOD
Participants
Female participants were recruited for the study while awaiting overnight medical treatment at an urban hospital emergency department that served a low-income catchment area of 1.1 million residents. Data were collected between August 2001 and April 2003. Women were approached in the waiting room and invited to participate in an initial screening interview. Written informed consent to be screened was provided by 799 women. Female research assistants fluent in English and Spanish conducted the screening interviews in private rooms at the hospital. All study procedures were approved by the applicable Institutional Review Boards.
To be eligible for this study, the woman needed to be over 18 years old, admitted to the emergency department when screening interviews were taking place, engaged in a sexual relationship with a man (described as either her boyfriend, ex-boyfriend, spouse, ex-spouse, father of her children, or a regular non-paying heterosexual partner) for at least six months, and not diagnosed with HIV or AIDS. Of the 336 women who met these criteria, 178 (53.0%) agreed to participate by signing written documentation of informed consent. Full-length interviews were completed at the hospital by trained social workers one week later. Several structured questionnaires were embedded in these interviews for administration by reading the questions aloud and recording verbal answers in response to options shown on printed cards. A total of 159 (47.3% participation of all screened eligible) women provided valid responses to all of the measures of central interest to this study.
Measures
Frequency of unprotected sex with partner
The number of unprotected sexual acts in which the participant had engaged with her primary partner over the last six months was estimated from reports of the total number of sexual acts performed over this period and the proportion of acts for which a condom was used, assessed in selected questions from the Sexual Risk Behavior Questionnaire (El-Bassel et al., 1995). Participants were first asked how many times they had engaged in sexual intercourse with their partner in the last six months (e.g., “in the past six months, since last _____, how often did you have vaginal sex with (your partner) _____?”). This question was asked separately for vaginal and anal sex, and definitions of each sexual act were provided. Response options were: Never, Once a month or less, 2–3 days a month, Once a week, 2–6 days a week, Once a day, or Two or more times a day. Responses were coded for the average monthly frequency, using the estimates 0, 1, 2.5, 4, 14, 30 and 60 respectively.
To estimate the percentage of sex acts that were unprotected, participants were asked about the proportion of times that they had used a condom during each type of sex (e.g., “In the past six months, altogether how many times did you use either a male or female condom during vaginal sex with your partner _____ ?”). Response options were: Never, Less than half the time, About half the time, More than half the time, or Always. These responses were coded in terms of an estimated percentage of unprotected sexual acts (1, .75, .50 .25 and 0, respectively).
Estimates of the monthly frequency of unprotected vaginal or anal sex were computed by multiplying the number of acts by the percentage of unprotected acts for each type of sex, and then these two numbers were summed. The resulting variable was multiplied by 6 to reflect the total number of unprotected sex acts with the partner in the last six months. A log transform was then applied to reduce the variable’s skew, and the result was multiplied by 244.48 to equate the mean and minimum possible values of the transformed scale with the original data and thereby make the units of the log transformed scale more readily interpretable. (Note that taking the product or sum of a scale with a constant has no effect on its relationships with other variables.) The transformed scale was normally distributed.
Perceived relationship power
The Sexual Relationship Power Scale (SRPS; Pulerwitz, Gortmaker, & DeJong, 2000) was developed to assess women’s ability to negotiate sexual practices that reduce HIV transmission risk effectively (Pulerwitz, et al., 2002). This measure addresses the power to make relationship decisions in sexual and non-sexual domains. The 15-item Relationship Control subscale (e.g., “If I asked my partner to use a condom, he would get angry,” “My partner tells me who I can spend time with”) has the response choices 1 = Strongly agree; 2 = Agree; 3 = Disagree; 4 = Strongly disagree. The 8-item Decision Making Dominance subscale (e.g., “Who usually has more to say about whether you have sex?” “Who usually has more to say about whether you use condoms?”) uses the response options: You; Your partner; Both of you equally; scored with the values 4, 1, and 2.5 respectively. Following the instructions provided by the scale authors, we computed the mean of each subscale and then averaged them together, α = 0.82. To normalize the skewed distribution, a log transform was applied to a reverse-scored version of the scale. We then multiplied each participant’s score by 5 and added 0.53, to set the mean and possible maximum values of the log transformed scale to equal those of the untransformed scale, and finally un-reversed the scale so that higher scores reflect more power in the relationship.
Rejection sensitivity (RS)
The Rejection Sensitivity Questionnaire is a valid and reliable measure of individual differences in the tendency to anxiously expect rejection in interpersonal situations (RSQ; Downey & Feldman, 1996). The measure presents hypothetical situations in which rejection is possible (e.g., “You ask a friend to do you a big favor”). Participants rate each situation, using six-point likert-type scales, on two dimensions. Their degree of anxiety and concern about the outcome (i.e., “How concerned or anxious would you be over whether or not your friend would do this favor?”) is rated from 1 = very unconcerned, to 6 = very concerned. Their expectation for a successful outcome (“I would expect that he/she would willingly do this favor for me”) is rated from 1 = very unlikely, to 6 = very likely. To compute an RS score for each situation, the expectation is reverse coded, such that a higher score indicates higher rejection expectancy, and the rejection expectancy score is multiplied by the anxiety score. Finally, the total RS score is the mean RS score across all the situations.
The original RSQ was designed for college students and contained items that would have been inappropriate for this sample. We therefore adapted the measure by eliminating those items. The adapted RSQ used in this sample included 8 situations, α =.88. Although the raw data were skewed, after applying a log transform the scale was normally distributed.
Perception of partner’s HIV risk
Participants were asked the current HIV status of their partner. To assess risk of HIV exposure in relationships with partners whose HIV status was currently negative or unknown, participants were asked “What would you say your partner’s chances are of getting HIV?”. Responses used a 5-point scale from 0 = Almost no chance to 5 = Almost certain chance. Those who perceived their partner as having almost no chance of HIV infection were coded 0, whereas those who reported that their partners were either HIV positive or at any risk of becoming HIV positive were coded 1.
Perception of own HIV risk
Participants were also asked “What would you say your chances are of getting HIV?” and responded using the same 5-point scale. Those who perceived themselves as having almost no chance of HIV infection were coded 0, whereas those who reported that they were at any risk of becoming HIV positive were coded 1.
Partner violence
We assessed the frequency with which participants were the target of physically or sexually coercive and/or injurious acts by their primary male partner in the last six months using the 15-item severe intimate partner violence subscale of the Revised Conflict Tactics Scales (CTS2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Seven items depict physically violent acts with potential for significant bodily harm (e.g., “Your partner choked you”); Five describe forced sexual acts (e.g., “Your partner used force, like hitting, holding down, or using a weapon, to make you have vaginal sex”); and three describe serious conflict-related physical injuries (e.g., “You passed out from being hit on the head by your partner in a fight”). Participants indicated how many times their partner had directed each act toward her in the last six months (0, 1, 2, 3–5, 6–10, 11–20 or more than 20). Participants who reported any such acts were coded 1, and the remainder were coded 0.
Economic dependence on partner
An interview item asking who held the lease on the participant’s place of residence was used as an index of financial dependence on the partner (as in El-Bassel et al., 2005). Responses indicating that the lease was held by the partner were coded 1, and all others were coded 0.
Substance use
Participants were asked how frequently they had used substances within the last 6 months. Response options for each substance type (alcohol, heroin, cocaine, crack, speedball, marijuana, uppers, downers, ecstasy and other) were never, once a month or less, 2–3 days a month, once a week, 2–6 days a week, once a day, 2 or more times a day. Daily consumption was reported for marijuana (n=19), cocaine and/or crack (n=8), five or more alcoholic drinks (n=5), heroin (n=5) and stimulants (n=1). Because all but one of the participants who endorsed daily consumption of five or more alcoholic drinks also endorsed daily use of one or more drugs, we created a combined daily substance use index rather than examining alcohol and drugs separately. Participants who reported daily substance use were coded 1, and those who reported no use or less frequent use were coded 0. Alcohol and drug use at less than daily frequencies were coded in additional dichotomous variables.
Analytic strategy
After examining the means and zero-order correlations of the study variables, we used regression analyses to test our hypotheses, standardizing all continuous risk factors for ease of interpretation. The first set of analyses focused on the association between frequency of unprotected sex in a long-term relationship with RS, perceived partner HIV risk and their interaction. The second set of analyses focused on the association of perceived relationship power with the same variables. Both sets of analyses focused on the hypothesized interaction between RS and perceived partner HIV risk, and were conducted in the same series of steps. Specifically, RS and perceived partner HIV risk were entered in the first step, and the interaction between these two variables was entered in the second step. Following the procedures recommended by Aiken and West (1991), we conducted simple slope analyses to further probe statistically significant interactions. The third step sought to establish whether the Step 2 results held when controlling for three known risk factors for HIV, specifically partner violence, economic dependence, and substance use. Thus, models were re-estimated with these three risk factors entered as controls.
In a fourth step we tested whether the Step 3 results held after controlling for the participant’s own perceived HIV risk and various demographic measures (age, race, educational attainment, marital status, and relationship duration). The change in R2 attributed to this step was not statistically significant in either set of analyses. Moreover, none of the added variables was significantly associated with unprotected sex frequency or perceived relationship power, and their inclusion did not change the reported results. The Step 4 models are therefore not presented.
A final set of analyses tested for mediation, estimating the indirect effect of RS via relationship power on unprotected sex with relationship partners perceived to be at risk for HIV.
RESULTS
Descriptive statistics
Participant characteristics were consistent with the composition of the urban, low-income community served by the hospital. Approximately one quarter (26.4%) of the sample held full-time jobs, and 60.4% were currently receiving some form of governmental financial assistance. Participants ranged in age from 18 to 61 years (Mean = 33.7, SD = 10.1 years) and were primarily from minority groups (52.2% Latina, 43.4% Black, and 4.4% White). They had completed a mean (SD) of 11.36 (1.39) years of education. Participants’ intimate relationships ranged in duration from 0.5 to 30 years (Mean (SD) = 6.45 (6.41) years); 20.75% were legal marriages. High levels of psychosocial stressors were faced by the participants. For example, 40.3% reported a history of homelessness, 36.0% reported a history of sexual assault, and 22.2% reported a history of incarceration.
The mean (SD) number of unprotected sexual encounters in the last six months was 82.98 (67.56). Relationship power and RS had scale means (SDs) of 2.77 (.40) and 7.06 (3.16), respectively. Forty-five participants reported that their partners were at risk for transmitting HIV (28.3%), including two participants whose partners had tested positive for the virus. (Excluding these two individuals did not yield any different results.) Forty-two participants reported being at risk for contracting HIV themselves (26.4%).
In terms of known HIV risk factors, severe partner violence was reported by 15.7%, economic dependence by 51.6%, and daily substance use by 19.5%. (Substance use at a less than daily frequency was reported by 27.7%, but when added to our models as a single variable, or as two separate variables for alcohol and drugs, less than daily substance use showed no significant associations nor changed the results that we report below.)
Zero-order correlations
The frequency of unprotected sex with the partner was correlated with lower perceived relationship power, and two of the three psychosocial risk factors (economic dependence and substance use) (Table 1). Although neither RS nor partner violence were significantly associated with unprotected sex frequency, they were correlates of lower perceived relationship power. Both unprotected sex frequency and relationship power were uncorrelated with perceived partner HIV risk, perceived own HIV risk, and demographic characteristics.
Table 1.
Correlations among study variables (N = 159)
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Frequency of unprotected sex with partner | --- | |||||||
| 2. Perceived relationship power | − 0.24* | --- | ||||||
| 3. Rejection sensitivity | 0.03 | − 0.23* | --- | |||||
| 4. Perceived partner HIV risk | 0.04 | − 0.10 | 0.08 | --- | ||||
| 5. Partner violence | 0.12 | − 0.32* | 0.25* | 0.15 | --- | |||
| 6. Economic dependence on partner | 0.26* | − 0.15 | − 0.14 | 0.02 | 0.00 | --- | ||
| 7. Substance use (daily) | 0.22* | − 0.14 | 0.05 | 0.04 | 0.05 | 0.00 | --- | |
| 8. Perceived own HIV risk | 0.04 | − 0.05 | 0.15 | 0.45* | 0.17* | − 0.02 | 0.07 | --- |
| 9. Age | − 0.07 | − 0.06 | 0.20* | 0.07 | − 0.05 | − 0.02 | − 0.04 | 0.03 |
| 10. Race (black) | 0.00 | − 0.03 | − 0.14 | 0.15 | 0.11 | −0.12 | 0.18* | 0.08 |
| 11. Educational attainment | 0.07 | 0.13 | − 0.11 | 0.14 | − 0.01 | −0.02 | − 0.06 | 0.11 |
| 12. Married | 0.15 | − 0.03 | − 0.13 | − 0.05 | − 0.05 | 0.25* | 0.06 | − 0.10 |
| 13. Relationship Duration | − 0.04 | 0.07 | − 0.17* | 0.03 | − 0.10 | 0.17* | − 0.03 | − 0.03 |
p < 0.05
RS and unprotected sex in relationships with high-risk partners
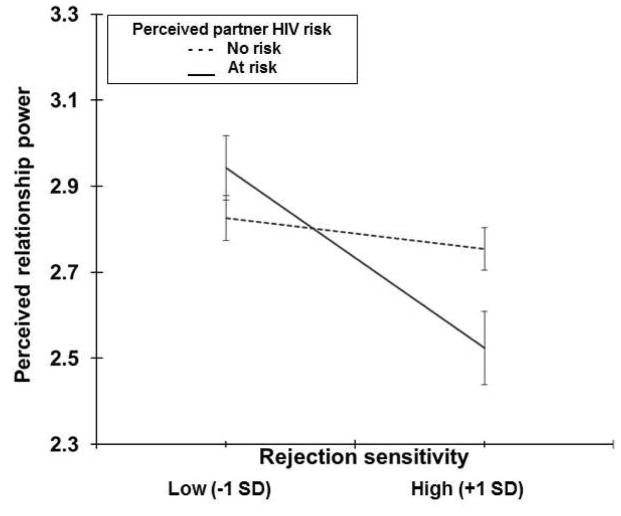
We conducted a series of linear regression analyses on the number of unprotected sexual acts with the partner in the last six months (Table 2). When entered together in the first step of our model, neither RS nor perceived partner HIV risk was significantly associated with frequency of unprotected sex. When the interaction between RS and perceived partner HIV risk was added to the model in Step 2, it was statistically significant as hypothesized (Figure 1). Simple slope analyses showed that women who perceived their partner as at risk for HIV engaged in significantly more frequent unprotected sex with him for every 1 SD increase in RS, B = 21.19, t = 2.32, p <0.05. When the partner was not perceived to be at risk, however, the frequency of unprotected sex with him was not significantly associated with RS, B = −6.31, t <1, ns.
Table 2.
Associations with the frequency of unprotected sex with partner (N=159)
| Model | Variable | B | (SE) | β | 95% CI | R2 | ΔR2 |
|---|---|---|---|---|---|---|---|
| 1. | (Constant) | 81.42 | 6.37 | [ 68.84,93.99] *** | .00 | --- | |
| Rejection sensitivity | 1.98 | 5.42 | 0.03 | [− 8.73, 12.69] | |||
| Perceived partner HIV risk | 5.53 | 12.00 | 0.04 | [−18.17, 29.23] | |||
|
| |||||||
| 2. | (Constant) | 80.98 | 6.28 | [ 68.58,93.39] *** | .04 | .04 * | |
| Rejection sensitivity | − 6.31 | 6.39 | − 0.09 | [−18.94, 6.32] | |||
| Perceived partner HIV risk | 3.42 | 11.86 | 0.02 | [−20.01, 26.85] | |||
| Rejection sensitivity x Perceived partner HIV risk | 27.49 | 11.65 | 0.22 | [4.49, 50.50] * | |||
|
| |||||||
| 3. | (Constant) | 55.22 | 8.36 | [38.71,71.72] *** | .15 | .12 *** | |
| Rejection sensitivity | − 4.49 | 6.24 | − 0.07 | [−16.82, 7.85] | |||
| Perceived partner HIV risk | − 0.46 | 11.34 | − 0.00 | [−22.87, 21.95] | |||
| Rejection sensitivity x Perceived partner HIV risk | 22.67 | 11.10 | 0.19 | [0.74, 44.60] * | |||
| Partner violence | 16.39 | 14.44 | 0.09 | [−12.14, 44.91] | |||
| Economic dependence on partner | 33.97 | 10.22 | 0.25 | [13.78, 54.15] *** | |||
| Substance use (daily) | 35.66 | 12.73 | 0.21 | [10.52, 60.81] ** | |||
p < 0.05,
p < 0.01,
p < 0.001
Figure 1.
Predicted six-month frequency of Unprotected sex with partner as a function of Rejection sensitivity x Perceived partner HIV risk.
In Step 3, we re-estimated the model adding three known risk factors for HIV in intimate relationships. Economic dependence and substance use were both significantly associated with more unprotected sex with the partner, whereas partner violence was not. Notably, the interaction between RS and perceived partner HIV risk remained significant.
RS and perceived power in relationships with high-risk partners
We next examined whether lower perceived power in relation to a partner at risk for transmitting HIV significantly explained the association of RS with more frequent unprotected sex in these relationships. We first repeated the regression analysis described previously, this time to examine variables associated with perceived relationship power (Table 3). RS was significantly associated with lower relationship power, but adding the interaction of RS with perceived partner HIV risk in Step 2 rendered the main effect of RS non-significant (Figure 2). Simple slope analyses indicated that women who perceived their partners as at risk for HIV reported significantly lower relationship power with every SD increase in RS (B = −0.21, t = −3.60, p < 0.001). No significant association was observed between RS and relationship power with partners not perceived to be at risk for HIV (B = −0.04, t = −1.01, ns).
Table 3.
Associations with perceived relationship power (N=159)
| Model | Variable | B | (SE) | β | 95% CI | R2 | ΔR2 |
|---|---|---|---|---|---|---|---|
| 1. | (Constant) | 2.79 | 0.04 | [2.72, 2.86]*** | .06 | --- | |
| Rejection sensitivity | − 0.09 | 0.03 | − 0.22 | [− 0.15, − 0.03] ** | |||
| Perceived partner HIV risk | − 0.07 | 0.07 | − 0.08 | [− 0.21, 0.07] | |||
|
| |||||||
| 2. | (Constant) | 2.79 | 0.04 | [ 2.72, 2.86] *** | .10 | .04** | |
| Rejection sensitivity | − 0.04 | 0.04 | − 0.09 | [− 0.11, 0.04] | |||
| Perceived partner HIV risk | − 0.06 | 0.07 | − 0.06 | [− 0.19, 0.08] | |||
| Rejection sensitivity x Perceived partner HIV risk | − 0.17 | 0.07 | − 0.24 | [− 0.31, − 0.04] ** | |||
|
| |||||||
| 3. | (Constant) | 2.91 | 0.05 | [ 2.82, 3.00] *** | .20 | .10*** | |
| Rejection sensitivity | − 0.03 | 0.04 | − 0.07 | [− 0.10, 0.04] | |||
| Perceived partner HIV risk | − 0.02 | 0.07 | − 0.02 | [− 0.15, 0.10] | |||
| Rejection sensitivity x Perceived partner HIV risk | − 0.15 | 0.06 | − 0.20 | [− 0.27, − 0.02] * | |||
| Partner violence | − 0.27 | 0.08 | − 0.25 | [− 0.44, − 0.11] *** | |||
| Economic dependence on partner | − 0.13 | 0.06 | − 0.16 | [− 0.24, − 0.01] * | |||
| Substance use (daily) | − 0.11 | 0.07 | − 0.11 | [− 0.26, 0.03] | |||
p < .05,
p < .01,
p < .001
Figure 2.
Predicted Perceived relationship power as a function of Rejection sensitivity x Perceived partner HIV risk.
We next re-estimated the model controlling for partner violence, the woman’s economic dependence on her partner and her substance use (see Table 3, Step 3). The woman’s perceived relationship power was inversely associated with the partner’s physical/sexual violence toward her as well as her economic dependence on him. The woman’s use of substances was not significantly associated with her relationship power. Importantly, the interaction between RS and the partner’s perceived HIV risk remained significantly associated with lower relationship power after the other risk factors were taken into account.
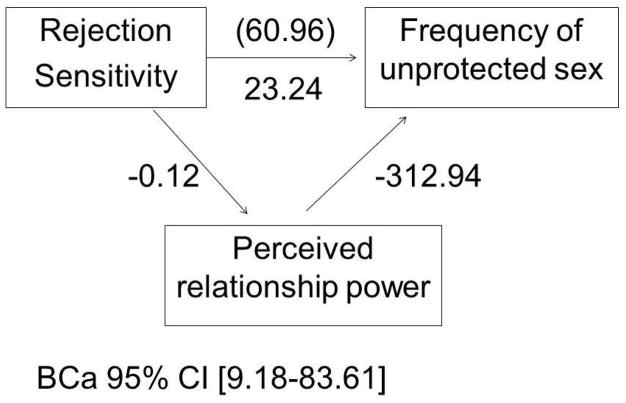
Test of mediation
To estimate the indirect effect of perceived relationship power on high-risk sexual activity within relationships, we used a nonparametric bootstrapping approach as is recommended for testing the significance of mediators in small samples (see Preacher & Hayes, 2004; Shrout & Bolger, 2002). We randomly sampled observations with replacement from the set of women who perceived their partners to be at risk for HIV (n = 45) to create a sample of 1,000, and calculated a bias-corrected and accelerated (BCa) 95% confidence interval. When relationship power was included in the model, the association of RS with unprotected sex was reduced from 60.96 (c) to 23.24 (c′) and no longer significant (p > 0.05). The true indirect effect was estimated to lie between 9.18 and 83.61 with 95% confidence, indicating that mediation significantly differed from zero at p < 0.05 (Figure 3). When this analysis was repeated taking into account partner violence, economic dependence and substance use, the indirect effect remained significant (between 1.13 and 68.26 with 95% confidence, p < 0.05).
Figure 3.
Mediation model for women who perceive their partners to be at risk for HIV. Perceived relationship power significantly mediates the association between Rejection sensitivity and the Frequency of unprotected sex with partner.
DISCUSSION
When a woman perceived her long-term male partner to be at risk for HIV, the extent to which she had high RS was associated with lower perceived power in the relationship and having engaged in significantly more unprotected sex with him. Moreover, her perceived lack of relationship power significantly explained such potentially dangerous sexual activity. Importantly, this pattern of associations was present even when other known risk factors for HIV exposure were controlled. That is, even though past research has suggested that women may have had more difficulty negotiating condom use if they were afraid of their partner’s violent reactions, economically dependent on him or frequently using substances, the association we found between high-risk unprotected sex frequency and RS was not explained by these other factors. The observed associations with RS were also independent of the woman’s own perceived HIV risk and demographic variables. This study adds to our understanding of RS as a relationship-centered vulnerability for health and wellbeing (Purdie & Downey, 2000) and demonstrates its relevance to the high HIV risk faced by marginalized women.
Limitations and future research directions
The present study lays the groundwork for further longitudinal and experimental research to understand preventable mechanisms of HIV susceptibility among women in long-term relationships. However, several limitations of this study should be rectified in future research.
First, participants facing high levels of psychosocial stressors completed a lengthy interview about their risk factors for HIV. Though fortunate to be able to conduct an investigation of RS in this context, we were limited in the number of questions we could ask without overtaxing the participants. Regrettably, we were not able to ask follow-up questions about whether the women wanted to use condoms, or why women with high RS more frequently had unprotected sex with a partner they believed could expose them to HIV. We were also unable to include additional personality questionnaires. Hence, the mechanisms of the associations that we found warrant further study.
Our evidence that the association of RS with the frequency of unprotected sex with a partner perceived to be at risk for HIV was mediated by lower perceived relationship power is consistent with the explanation that those with high RS prioritized the prevention of rejection over other goals and therefore more readily saw themselves as needing to accommodate their partner’s decisions, needs, and desires. Yet other reasons are also possible. For example, romantic attachment anxiety has been associated with increased sexual motivation when feeling insecure about a relationship (Davis, Shaver & Vernon, 2004) and a greater tendency to interpret sex as having implications for relationship status and quality (Birnbaum, Reis, Mikulincer, Gillath & Orpaz, 2006). Perhaps RS similarly motivated women to have unprotected sex with their partners for internal (rather than interpersonal) reasons, such as increasing feelings of intimacy and security, or increased desire to conceive a child. Future research should further examine why women high in RS engaged in more high-risk sex.
Although RS showed significant associations with lower perceived relationship power and having unprotected sex independent of central psychosocial and sociocultural risk factors for HIV exposure, we were unable to test whether these associations were independent of other personality variables, such as romantic attachment anxiety, fear of negative evaluation, low self-esteem, or neuroticism. While correlated with these other personality constructs, RS has repeatedly been shown to be associated with specific outcomes even when these other constructs are controlled (e.g., Berenson et al., 2009; Downey & Feldman, 1996; Romero-Canyas, Downey, Reddy, et al., 2010), but analyses of this sort were not conducted in the present study.
Rather than relying solely on retrospective self-reports of behavior over a 6-month period, future studies should aim to reduce recall bias and social acceptability bias through alternative assessment methods, such as implicit measures, diary methods, confirmatory partner reports, official police/hospital records, and/or direct observation of couples’ interactions. In addition, verbal administration of measures by computer might have advantages over a face-to-face interview for collecting sensitive and stigmatized information.
We also caution against drawing any causal conclusions from cross-sectional, retrospective self-report studies of this nature. Although previous research has shown that RS can prospectively predict the outcome of a relationship (Downey, Freitas, Michaelis & Khouri, 1998), as well as accommodation and aggression in relationships (Purdie & Downey, 2000), further research is necessary to determine whether RS played a causal role in the lower perceived relationship power and more frequent high-risk sex that we found to be associated with it.
Finally, the present study had a small sample with limited statistical power and generalizability. One of the strengths of this study was that it focused on socioeconomically disadvantaged women at high risk for HIV, thereby extending work focusing on RS and HIV risk in college students (e.g., Edwards & Barber, 2010), but further work in larger, more diverse samples is warranted. Because this study only included women in heterosexual relationships for at least 6 months, it did not address the potential health risks that might be linked with RS among single women, women in new relationships, gay women, or men.
Of the forty-two participants who perceived themselves as at risk for HIV, fifteen reported having had unprotected intercourse with a male partner that they viewed as having no HIV risk. Therefore, while the sexual risk faced by male partners in the relationship was not the focus of our study, it was certainly present in some cases. An additional twenty-five participants reported unprotected intercourse within relationships in which they perceived both themselves and their partners to be mutually at risk for HIV, though it is unknown whether they considered the possibility of virus transmission within the relationship when estimating that HIV risk was mutual. Importantly, for physiological reasons it is easier for a woman to contract HIV from a male partner during heterosexual vaginal or anal intercourse than it is for her to transmit HIV to him (CDC, 2013).
Implications for intervention
One major issue for the prevention of HIV transmission in close relationships is the tendency for long-term partners to underestimate each other’s potential HIV risk (Kershaw et al., 2003; Misovich, Fisher & Fisher, 1997). But the results of the present study indicated that increasing awareness of risk with long-term partners was unlikely to be effective in reducing HIV exposure for women who had high RS. In fact, it was specifically among the women who did acknowledge their partner’s potential risk that the associations of RS with lower relationship power and more frequent unprotected sex were found.
For women who are highly rejection-sensitive, interventions to reduce HIV risk in long-term relationships should address both the maladaptive pattern of lower perceived relationship power and the unspoken fears that promote it. Of course, because RS typically develops as an adaptation to experiences in which one was painfully uncertain of acceptance in crucial family or social relationships (Downey, Khouri & Feldman, 1997), and perceived dependency may be fostered by deprivation and victimization, it will be important to recognize and validate women’s efforts to cope with adversity as part of any intervention to foster more assertive patterns with less personal cost.
Concluding comments
Among women in relationships with high-risk partners, RS was associated with lower perceived relationship power and in turn, more unprotected sex, thereby exacerbating the already high HIV risk women in this sample faced due to structural inequalities. Interventions to foster more assertive responses to danger signals in close relationships may be vital for rejection-sensitive women struggling against stress and disadvantage.
Acknowledgments
This work was supported by two grants from the National Institute of Mental Health: R01 MH05829 (El-Bassel) and R01 MH69703 (Downey).
Contributor Information
Kathy R. Berenson, Department of Psychology, Gettysburg College
Christine Paprocki, Department of Psychology, University of North Carolina at Chapel Hill
Marget Thomas Fishman, Department of Psychology, Columbia University
Devika Bhushan, Department of Psychology, Columbia University
Nabila El-Bassel, School of Social Work, Columbia University
Geraldine Downey, Department of Psychology, Columbia University
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications; 1991. [Google Scholar]
- Berenson KR, Gyurak A, Ayduk O, Downey G, Garner MJ, Mogg K, Bradley BP, Pine DS. Rejection sensitivity and disruption of attention by social threat cues. Journal of Research in Personality. 2009;43:1064–1072. doi: 10.1016/j.jrp.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biello KB, Sipsma HL, Ickovics JR, Kershaw T. Economic Dependence and Unprotected Sex: The Role of Sexual Assertiveness among Young Urban Mothers. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2010;87:416–425. doi: 10.1007/s11524-010-9449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum GE, Reis HT, Mikulincer M, Gillath O, Orpaz A. When Sex Is More Than Just Sex: Attachment Orientations, Sexual Experience, and Relationship Quality. Journal of Personality and Social Psychology. 2006;91:929–943. doi: 10.1037/0022-3514.91.5.929. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS surveillance report, 2011. Vol. 23. Atlanta: US Department of Health and Human Services, CDC; 2013. Retrieved from http://www.cdc.gov/hiv/topics/surveillance/resources/reports. Published Feb. 2013. [Google Scholar]
- Cooper ML. Toward a person x situation model of sexual risk-taking behaviors: Illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology. 2010;98:319–341. doi: 10.1037/a0017785. [DOI] [PubMed] [Google Scholar]
- Davis D, Shaver PR, Vernon ML. Attachment style and subjective motivations for sex. Personality and Social Psychology Bulletin. 2004;30:1076–1090. doi: 10.1177/0146167204264794. [DOI] [PubMed] [Google Scholar]
- Downey G, Feldman SI. Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology. 1996;70:1327–1343. doi: 10.1037//0022-3514.70.6.1327. [DOI] [PubMed] [Google Scholar]
- Downey G, Freitas AL, Michaelis B, Khouri H. The self-fulfilling prophecy in close relationships: Rejection sensitivity and rejection by romantic partners. Journal of Personality and Social Psychology. 1998;75:545–560. doi: 10.1037//0022-3514.75.2.545. [DOI] [PubMed] [Google Scholar]
- Downey G, Khouri H, Feldman S. Early interpersonal trauma and later adjustment: The mediational role of rejection sensitivity. In: Cicchetti D, Toth SL, editors. Rochester symposium on developmental psychology. Developmental perspectives on trauma: Theory, research and intervention. Vol. 8. Rochester, NY: University of Rochester Press; 1997. pp. 85–114. [Google Scholar]
- Edwards GL, Barber BL. The relationship between rejection sensitivity and compliant condom use. Archives of Sexual Behavior. 2010;39:1381–1388. doi: 10.1007/s10508-009-9520-8. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Vinocur D, Chang M, Wu E. Posttraumatic Stress Disorder and HIV Risk Among Poor, Inner-City Women Receiving Care in an Emergency Department. Am J Public Health. 2011;101(1):120–127. doi: 10.2105/AJPH.2009.181842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Chang M, Gomes C, Vincour D, Spevack T. Intimate partner violence prevalence and HIV risks among women receiving care in emergency departments: Implications for IPV and HIV screening. Emergency Medicine. 2007;24:255–259. doi: 10.1136/emj.2006.041541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Go H, Hill J. Relationship Between Drug Abuse and Intimate Partner Violence: A Longitudinal Study Among Women Receiving Methadone. Am J Public Health. 2005;95:465–470. doi: 10.2105/AJPH.2003.023200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Ivanoff A, Schilling RF, Gilbert L, Borne D, Chen DR. Preventing HIV/AIDS in drug-abusing incarcerated women through skills building and social support enhancement: Preliminary outcomes. Social Work Research. 1995;19:131–141. [PubMed] [Google Scholar]
- Gielen AC, McDonnell KA, O’Campo PJ. Intimate partner violence, HIV status, and sexual risk reduction. AIDS and Behavior. 2002;6:107–116. [Google Scholar]
- Gilbert L, El-Bassel N, Chang M, Wu E, Roy L. Substance use and partner violence among urban women seeking emergency care. Psychology of Addictive Behaviors. 2012;26:226–235. doi: 10.1037/a0025869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JS, Wardlow H, Smith DJ, Phinney HM, Parikh S, Nathanson CA. The Secret: Love, Marriage and HIV. Vanderbilt University Press; Nashville, TN: 2010. [Google Scholar]
- Hoyle RH, Fejfar MC, Miller JD. Personality and sexual risk taking: A quantitative review. Journal of Personality. 2000;68:1203–1231. doi: 10.1111/1467-6494.00132. [DOI] [PubMed] [Google Scholar]
- Jack DC, Dill D. The silencing the self scale: Schemas of intimacy associated with depression in women. Psychology of Women Quarterly. 1992;16:97–106. [Google Scholar]
- Kershaw TS, Ethier KA, Niccolai LM, Lewis JB, Ickovics JR. Misperceived risk among female adolescents: social and psychological factors associated with sexual risk accuracy. Health Psychology. 2003;22:523–532. doi: 10.1037/0278-6133.22.5.523. [DOI] [PubMed] [Google Scholar]
- Kershaw TS, Milan S, Westdahl C, Lewis J, Schindler Rising S, Fletcher R, Ickovics J. Avoidance, anxiety and sex: The influence of romantic attachment on HIV-risk among pregnant women. AIDS and Behavior. 2007;11:299–311. doi: 10.1007/s10461-006-9153-z. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV: Issues in methodology, interpretation and prevention. Am Psychologist. 1993;48:1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misovich SJ, Fisher JD, Fisher WA. Close relationships and elevated HIV risk behavior: Evidence and possible underlying psychological processes. Review of General Psychology. 1997;1:72–107. [Google Scholar]
- Newman PA, Williams CC, Massaquoi N, Brown M, Logie C. HIV prevention for Black women: structural barriers and opportunities. J Health Care Poor Underserved. 2008;19:829–41. doi: 10.1353/hpu.0.0043. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, Gortmaker SL, DeJong W. Measuring relationship power in HIV/STD research. Sex Roles. 2000;42:637–660. [Google Scholar]
- Pulerwitz J, Amaro H, De Jong W, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14:789–800. doi: 10.1080/0954012021000031868. [DOI] [PubMed] [Google Scholar]
- Purdie V, Downey G. Rejection Sensitivity and adolescent girls’ vulnerability to relationship-centered difficulties. Child Maltreatment. 2000;5:338–349. doi: 10.1177/1077559500005004005. [DOI] [PubMed] [Google Scholar]
- Romero-Canyas R, Downey G, Berenson KR, Ayduk O, Kang NJ. Rejection sensitivity and the rejection-hostility link in romantic relationships. Journal of Personality. 2010;78:119–148. doi: 10.1111/j.1467-6494.2009.00611.x. [DOI] [PubMed] [Google Scholar]
- Romero-Canyas R, Downey G, Reddy KS, Rodriguez S, Cavanaugh TJ, Pelayo R. Paying to Belong: When Does Rejection Trigger Ingratiation? Journal of Personality and Social Psychology. 2010;99:802–823. doi: 10.1037/a0020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero-Canyas R, Reddy KS, Rodriguez S, Downey G. After all I have done for you: Self-silencing accommodations fuel women’s post-rejection hostility. Journal of Experimental Social Psychology. 2013;49:732–740. doi: 10.1016/j.jesp.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psychological Bulletin. 1999;125:90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflicts tactics scales (CTS2): Development and Preliminary Psychometric Data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Wingwood GM, DiClemente RJ. The effects of an abusive primary partner on the condom use and sexual negotiation practices of African-American women. American Journal of Public Health. 1997;87:1016–1018. doi: 10.2105/ajph.87.6.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingwood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27:539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- Zierler S, Krieger N. Reframing women’s risk: Social inequalities and HIV infection. Annual Rev Public Health. 1997;18:401–43. doi: 10.1146/annurev.publhealth.18.1.401. [DOI] [PubMed] [Google Scholar]