Abstract
Background: Medical economics have significant impact on the entire country. The explosion in surgical techniques has been accompanied by questions regarding actual improvements in outcome and cost-effectiveness, such as the da Vinci® Surgical System (dVS) compared with conventional video-assisted thoracic surgery (VATS).
Objective: To establish a medical fee system for robot-assisted thoracic surgery (RATS), which is a system not yet firmly established in Japan.
Methods: This study examines the cost benefit performance (CBP) based on medical fees compared with VATS and RATS under the Japanese National Health Insurance System (JNHIS) introduced in 2012.
Results: The projected (but as yet undecided) price in the JNHIS would be insufficient if institutions have less than even 200 dVS cases per year. Only institutions which perform more than 300 dVS operations per year would obtain a positive CBP with the projected JNHIS reimbursement.
Conclusion: Thus, under the present conditions, it is necessary to perform at least 300 dVS operations per year in each institution with a dVS system to avoid financial deficit with current robotic surgical management. This may hopefully encourage a downward price revision of the dVS equipment by the manufacture which would result in a decrease in the cost per procedure.
Keywords: robotic surgery, cost-benefit performance, Japanese National Health Insurance System
Introduction
For a long time medical costs have been a remarkably significant large factor determining the national budget. This is significant when a government decides the country’s future policies. The current globalization of economic distribution among countries surrounding the Pacific has attracted much international interest. Above all, medical economics has a particularly large implication in Japan which implements a uniform universal health insurance system for the entire country.
The explosion in surgical technological techniques has been accompanied by questions about actual improvements in outcome and cost-effectiveness. At present, the main procedures for which robotic surgery has been approved are limited to procedures requiring deft and accurate manipulations in limited spaces such as the uterus, and the prostate, since governmental and insurance agencies question the real outcome efficiency and cost benefit performance (CBP) of robot-assisted surgery (RAS) in comparison to video-assisted surgery (VAS) in larger organs.
While RAS has been approved for insurance compensation only in prostate surgery in Japan, robot-assisted thoracic surgery (RATS) has not yet been approved for reimbursement by the Japan National Health Insurance System (JNHIS).
The cost of RAS in Japan is of course greatly affected by the cost of the operator-controlled module, the ancillary equipment and maintenance costs, but not by the surgeon’s fee, since in university hospitals in Japan, surgeons are paid a salary determined by the Ministry of Health and Welfare, regardless of the number or types of surgical procedures they perform.
Methods
All patients who underwent RATS in our hospital provided written informed consent after full explanation of the investigational nature of the procedures, and the study was approved by the institutional review board. We performed this institution-funded trial in 20 cases of mediastinal tumors, chest wall tumors and lung cancer, in order to establish the technique of RAS procedures and determine its medicoeconomic aspects in thoracic diseases. All procedures were performed between March 2010 and July 2012 and all costs were borne by the hospital in all cases. All data included in the figures and tables are calculated at ¥80 = $1, which was the average exchange rate as between March 2010 and July 2012.
Instruments
We employed the da Vinci® Surgical System (dVS) (Intuitive Surgical, Inc., Sunnyvale, California, USA), as described in our previous reports.1–3) The techniques and costs of preoperative workup, anesthesia and postoperative management are essentially the same for RATS and video-assisted thoracic surgery (VATS). The establishment of the four access ports was similar in RATS and VATS. The uniquely different features of RATS are the use of the EndoWrist (the monopolar curved scissors for Arm #1, and Maryland bipolar forceps or Cadiere forceps for Arm #2) and inflation of the typically narrow working thoracic space with high-pressure CO2 (8–10 mmHg).
Role of the funding source
All medical expenses for actual medical examinations and treatment for patients were paid for by Tokyo Medical University Hospital. For research support for studies on robotic surgery, we used a grant from the Cancer Research Institute of Tokyo Medical University.
Results
We compared the costs for RATS and VATS, as decreed by the JNHIS, with RATS for each of the above-mentioned thoracic procedures in the US and Japan (Tables 1 and 2). Although the additional costs varied according to the type of procedure, in general the use of RATS increased costs by over $10000 per procedure in Japan (Table 1A). However, when we examine the costs according to procedure and according to whether the disease is benign or malignant, we can see that, while, in general, uniform non-RATS procedures cost less in Japan than in the US, perhaps because of the nationally implemented policy of the JNHIS, the use of RATS in Japan almost doubles the cost of open procedure due to the high cost of robotic equipment. Robot-assisted prostatectomy for prostate cancer now receives insurance reimbursement for use of support devices for endoscopic surgery, $6775 under the JNHIS, since April 2012. If the same standard amount were applied to various diseases in the field of general thoracic surgery, the additional cost for RATS, which would also require set-up of the support devices for endoscopic surgery, $6775 which is the same as robotic prostatectomy under the JNHIS, on the basic cost of open thoracotomy approach.
Table 1A.
Costs per robotic surgery case in Japan
| Contents | Items | Cost: US $ |
|---|---|---|
| Surgeon’s fee | Surgeons receive only their basic salary | 0 |
| dVS equipment fee; based on 100 procedures/year (all specialties) | $5859* | |
| Medical materials | Cadiere forceps (Usable in 10 procedures) | $578 |
| Monopolar curved scissors (Usable in 10 procedures) | $853 | |
| Maryland bipolar forceps (Usable in 10 procedures) | $780 | |
| Permanent cautery spatula (Usable in 10 procedures) | $578 | |
| Drape, instrument arm (Disposable) | $404 | |
| Drape, camera arm (Disposable) | $114 | |
| Drape, camera (Disposable) | $96 | |
| Cannula seals (Disposable) | $173 | |
| Total for da Vinci instrument items | $3575# | |
| Maintenance cost | $2250** | |
| Total ( = Cost/one robotic surgery case) | $11684*** | |
Table 1A shows the cost for the da Vinci® Surgical System (dVS) operation on the assumption of 100 cases in 1 institution per year with the projected Japanese National Health Insurance System (JNHIS) reimbursement system. *repayment cost/operation, **running cost/operation, ***cost/one-robotic case operation, #medical materials cost for the dVS/operation
Table 2.
Cost for RATS with the Japanese public health insurance system since April 2012
| Procedure | Change in cost of procedures performed in USA | Change in cost of procedures performed in Japan $1 = ¥80, average exchange rate Mar.2010-Jul.2012 | |||||
|---|---|---|---|---|---|---|---|
| Excluding robot | Including robot | Excluding robot | Including robot (price of "the Excluding robot + $6775) | ||||
| Benign | Malignant | Benign | Malignant | ||||
| Thymectomy | Thymectomy | $179837) | $24007) | $4625 | Simple resection $4625 | $11400 | Simple resection $11400 |
| Extended thymectomy | NA | $35618) | Extended resection $7003 | Extended resection $13778 | |||
| Resection of tumor A. Mediastinal B. Chest wall |
Open surgical procedures | NA | NA | A. $2313 B. $1325 |
A. $4425 B. $2713 |
A. $9088 B. $8100 |
A. $11200 B. $9488 |
| VATS | $7031 | NA | |||||
| Lobectomy | Open surgical procedures | $83689) | $54609) | $7294 | $9080 | $14069 | $15855 |
| VATS | $14799) | $7369 | $11500 | ||||
Table 2 shows the cost for dVS-surgery for 100 robotic cases per year at 1 institution with the projected JNHIS reimbursement system. RATS: robot-assisted thoracic surgery; VATS: video-assisted thoracic surgery; JNHIS: Japanese National Health Insurance System
Calculations of costs associated with robotic medical care for institutions which perform dVS-operations 100 times (A), 200 times (B) or 300 times (C) annually, are shown in Table 1B. In the JNHIS, reimbursement is based on the insurance point number awarded for a given procedure or the equipment used. The difference of cost for dVS surgery in Table 3 varies on the assumption of between 100, 200 or 300 robotic cases in a year at one institution with the JNHIS (Table 3).
Table 1B.
Japanese national guidelines for the calculation of the costs of advanced medical care10)
| • $3255000 (purchase price of the dVS) × 0.9 = $2929500 (repayment cost) |
| $2929500/5 years (service life) = $585900/year (repayment cost/year) |
| At an institution which perform the dVS operation A: 100 times, B: 200 times and C: 300 times in a year |
| A: ¥ 46872000/100 times (annual use) = $5859* (repayment cost/operation) |
| B: ¥ 46872000/200 times (annual use) = $2930* (repayment cost/operation) |
| C: ¥ 46872000/300 times (annual use) = $1953* (repayment cost/operation) |
| • Amount of maintenance cost/5 years = $1250000 |
| $1250000 × 0.9 = $1125000 → $1125000/5 year = $225000 (maintenance cost/year)† |
| A: $225000/100 times = $2250**(running cost/operation) |
| B: $225000/200 times = $1125**(running cost/operation) |
| C: $225000/300 times = $750**(running cost/operation) |
| • Pattern A: $3575# (medical materials cost/operation) + $2250** (running cost/operation) + $5859* (repayment cost/operation) |
| = $11684***/one-robotic case operation |
| • Pattern B $3575# (medical materials cost/operation) + $1125** (running cost/operation) + $2930* (repayment cost/operation) |
| = $7630***/one-robotic case operation |
| • Pattern C: $3575# (medical materials cost/operation) + $750** (running cost/operation) + $1953* (repayment cost/operation) |
| = $6278***/one-robotic case operation |
Table 1B shows a tentative calculation for the basis of costs associated with robotic medical care for institutions which perform the da Vinci® Surgical System (dVS) procedures 100 times (pattern A), 200 times (pattern B) and 300 times (pattern C) in a year, respectively. *repayment cost/operation, **running cost/operation, ***cost/one-robotic case operation, #medical materials cost for the dVS/operation; †Reduced by Intuitive Surgical to US$90000 (maintenance cost/year) from July 2012.
Table 3.
The difference of cost for RATS with the Japanese public health insurance system since April 2012
| Procedure | Change in cost in procedures performed in Japan $1 = ¥80, average exchange rate Mar.2010-Jul.2012 |
||||||
|---|---|---|---|---|---|---|---|
| The dVS operation was performed 100 times in a year | The dVS operation was performed 200 times in a year | The dVS operation was performed 300 times in a year | |||||
| Including robot (price of "Excluding robot + $11675) | Including robot (price of "Excluding robot + $7625) | Including robot (price of "Excluding robot + $6275) | |||||
| Benign | Malignant | Benign | Malignant | Benign | Malignant | ||
| Thymectomy | Thymectomy | $16300 | Simple resection $16300 | $12250 | Simple resection $12250 | $10900 | Simple resection $10900 |
| Extended thymectomy | Extended resection $18678 | Extended resection $14628 | Extended resection $13278 | ||||
| Resection of tumor A. Mediastinal B. Chest wall |
Open surgical procedures | A. $13988 | A. $16100 | A. $9938 | A. $12050 | A. $8588 | A. $10700 |
| VATS | B. $13000 | B. $14388 | B. $8950 | B. $10338 | B. $7600 | B. $8988 | |
| Lobectomy | Open surgical procedures | $18969 | $20755 | $14919 | $16705 | $13569 | $15355 |
| VATS | |||||||
Table 3 shows the differences in cost for dVS surgery for 100, 200 or 300 robotic cases per year at 1 institution with the projected JNHIS reimbursement system. RATS: robot-assisted thoracic surgery; dVS: da Vinci® Surgical System; VATS: video-assisted thoracic surgery; JNHIS: Japanese National Health Insurance System
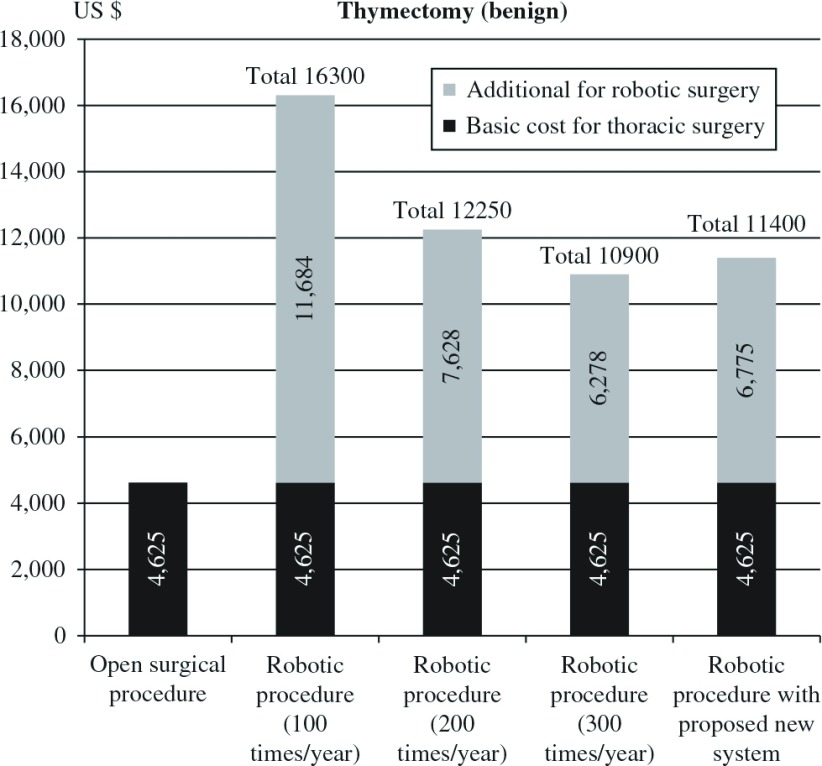
Figure 1 shows the difference between open thoracotomy procedures and RATS procedures, when institutions performed the dVS operation 100, 200 or 300 times per year, and the projected JNHIS additional insurance reimbursement for endoscopic surgery ($6775), for thymectomy for benign disease. The anticipated reimbursement by the JNHIS ($11400) shows the price insufficiency (100 times/year; $ –4900, 200 times/year; $ –85 per procedure) calculated on the basis of the projected reimbursement. Only institutions performing 300 procedures per year would show a positive CBP under the projected reimbursement system.
Fig. 1.
Differences between open surgical procedure and robot-assisted thoracic surgery (RATS) procedure for thymectomy. The financial differences are shown among institutions performing RATS procedures, in which institutions performed the da Vinci® Surgical System (dVS) operation 100, 200 or 300 times per year. Figures are based on data contained in Tables 1A, 1B, 2 and 3. Since the purchase price and 5-year service life cost are set by the government, the cost per RATS procedure in the institution obviously decreases with the number of procedures performed annually.
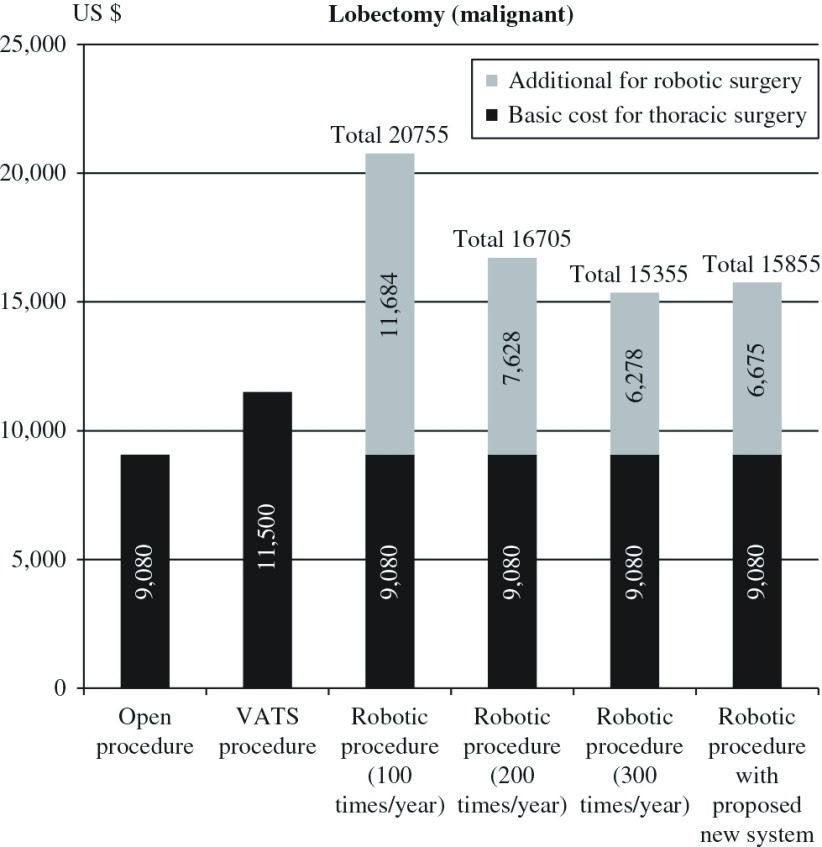
Figure 2 shows the cost of lobectomy for malignant disease. The differences between open thoracotomy, VATS and RATS procedures are shown in Tables. The projected reimbursement with the JNHIS ($15855) still show a loss (as with benign tumors) if the institution performs only 100 or 200 procedures for year. This pattern also shows that only institutions performing 300 procedures per year would show a profit.
Fig. 2.
Cost of pulmonary lobectomy for malignant disease among open thoracotomy, video-assisted thoracic surgery (VATS) and robot-assisted thoracic surgery (RATS) procedures, in institutions which performed the da Vinci® Surgical System (dVS) operation 100, 200 or 300 times in a year. Figures are based on data contained in Tables 1A, 1B, 2 and 3.
Discussion
In Japan, prostectomy for prostate cancer using the dVS is the only application recognized for reimbursement by the JNHIS of the Ministry of Health, Labour and Welfare, and this has been only since April 2012. We are still waiting for recognition by the Ministry of Health, Labour and Welfare for reimbursement of dVS operations in other clinical fields, such as gastrectomy, uterectomy, pulmonary lobectomy and thymectomy. Nevertheless, dVS operations are now increasing rapidly in Japan. The total number of dVS operations in Japan was 209 in 2009, 498 in 2010, and 971 in 2011. Rapid decisions concerning JNHIS applications for dVS operations are necessary for many other procedures.
Good long-term outcomes from robotic surgery for thymectomy with nonthymomatous myasthenia gravis and lobectomy for non-small cell lung cancer have recently been reported.4–6) These reports also show satisfactory outcomes for RATS. In the near future, these reports will encourage many thoracic surgeons to attempt to widen the indications of robotic surgery in Japan.
As for the clinical hypothesis in Japan, it appears that no final conclusion can be reached unless the number of cases of RATS increases. Past reports4,5) are retrospective investigations in the field of thoracic surgery. However, such clinical evidence is not yet shown even in other fields, particularly in urology, and evidence showing a significant difference is only available for thymectomy by RATS for myasthenia gravis. We consider that RATS, if fairly priced, would be worth performing for thoracic disease in Japan. It appears that randomize prospective studies in RATS are necessary in the future. Such studies are essential because the medical cost is high, which is the first practical issue that needs to be addressed to solve this clinical problem. As a result, accumulation of sufficient number of cases evaluated by randomized prospective studies is expected to bring about medico-economic improvement. These series of studies enable cost-benefit analysis leading to the reduction of the medical cost which can finally pave the way for the extension of the benefits of robotic surgery to many patients.
The clinical use of a dVS in Japan began in 2006, and even today only a few hospitals and institutions possess it. As of April 2012, 45 dVS systems were being used for clinical or educational purposes in Japan. Because only a few hospitals can afford it, even for government-sanctioned procedures such as prostatectomy, only those relatively few hospitals will accumulate many more patients, at the expense of other hospitals and perhaps to the detriment of some patients.
The JNHIS has covered the whole nation of Japan since 1961. Now the medical copayment the patients have to pay is 30%, with all their other medical expenses being paid by the government. Regardless of the lower per capita medical costs for Japan in comparison with other countries, because all prices are fixed by the government, the tendency of medical costs to increase annually continues to be a point of much political disagreement. The background is complicated and includes Japan’s rapidly aging society, advanced medical developments and the increasing cost of drugs. To limit the national health care financial burden as much as possible, the Japanese Government must always consider improving and controlling the medical insurance system which means that the costs of robotic surgery are problematic.
The Japanese medical reimbursement assignment revision by the Ministry of Health, Labour and Welfare in April 2012 did not accept the dVS robotic system as a basic medical instrument. Instead, dVS robot-assisted surgery was approved, under several detailed conditions, for example, the experience of the users, as additional technical support in the insurance system, that is, it was considered medical technology supporting a surgical procedure.
However, despite the enormous potential for the spread and development of robotic surgery in various fields, including the field of telemedicine, the single greatest negative feature preventing this, at least in Asia, is the hugely greater cost of the equipment in Japan, Korea and Taiwan.
The cost of a dVS system in Japan is US$3255000 (November 2012 exchange rate), despite the fact that Japan only applies a 7% sales tax, but no import tax. The cost in Korea is similar. Thus, as of September 2011 the cost in Japan was 2.17 times that in the US (US$1500000), 1.46 times that in the UK and 1.59 times that in Germany and France. Despite repeated requests for an explanation for this from the manufacturer, no satisfactory answer has been forthcoming.
One possible related factor is that Intuitive Surgical Inc. is the sole manufacturer of the dVS device and there are as yet no other comparable competitive systems on the market.7) Despite our ignorance of the intricacies of patent law that are related to the present situation, we are sanguine that, as competition for such devices spreads, the attendant lower prices might stimulate increases in the applications of and education in RAS.
In establishing its policy regarding remuneration for RAS techniques, the Japanese government decided, for whatever reason, that RAS is not a basic medical technique, but rather an “add-on” technological support system. In defense of this policy, it can only be said that with a population of 127570000, of whom 30740000 are over 65 and 16650000 are under 16, the Japanese government is constantly caught in a conundrum whereby they must seek to provide best possible care but yet not pay exorbitant amounts.
The fact remains that, under the present system, any given institution in Japan would have to be able to perform 300 or more procedures annually to break even financially, and few institutions are willing to take on that responsibility.
There are several limitations to this study. The first two concern financial matters: i.e., the pricing policy of the dVS manufacturer is absolutely opaque, while the second is that the remuneration policy of the Japanese government is equally murky. Thirdly, unless it is made possible for clinicians to explore possible wider indications of the equipment, as well as the true value of RAS and RATS for patients, institutions and health systems, it may take a long time for these procedures to be understood and implemented.
We believe that it is essential for these primarily financial concerns to be clearly addressed in order for the benefits of RAS to reach the public.
Conclusion
Because of the high cost of the system in Japan, it is necessary to perform dVS surgery at least 300 times in a year at one institution to prevent a deficit in income. We hope that marked competition will eventually reduce the cost of robot-related devices. Without a large decrease in cost of the system, it is difficult to envision rapid spread and development of RAS even in countries with highly developed national insurance systems.
Acknowledgements
The authors are grateful to Tom Lang, MA, Tom Lang Communications and Training International, Professor Farhad Alinaghizadeh Mollasaraie, Department of Medical Sciences, Occupational and Environmental Medicine, Uppsala University, and Ms. Maya Vardaman and Associate Professor Edward F. Barroga of the Department of International Medical Communications, Tokyo Medical University, for reviewing this manuscript.
We appreciate the financial support for research on robotic surgery from the Cancer Research Institute of Tokyo Medical University.
Disclosure Statement
The authors have no conflict of interest to disclose with respect to this article.
References
- 1).Kajiwara N, Kakihana M, Usuda J, et al. Extended indications for robotic surgery for posterior mediastinal tumors. Asian Cardiovasc Thorac Ann 2012; 20: 308-13. [DOI] [PubMed] [Google Scholar]
- 2).Kajiwara N, Taira M, Yoshida K, et al. Early experience using the da Vinci Surgical System for the treatment of mediastinal tumors. Gen Thorac Cardiovasc Surg 2011; 59: 693-8. [DOI] [PubMed] [Google Scholar]
- 3).Kajiwara N, Kakihana M, Kawate N, et al. Appropriate set-up of the da Vinci Surgical System in relation to the location of anterior and middle mediastinal tumors. Interact Cardiovasc Thorac Surg 2011; 12: 112-6. [DOI] [PubMed] [Google Scholar]
- 4).Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg 2011; 141: 673-7. [DOI] [PubMed] [Google Scholar]
- 5).Park BJ, Melfi F, Mussi A, et al. Robotic lobectomy for non-small cell lung cancer (NSCLC): long-term oncologic results. J Thorac Cardiovasc Surg 2012; 143: 383-9. [DOI] [PubMed] [Google Scholar]
- 6).Louie BE, Farivar AS, Aye RW, et al. Early experience with robotic lung resection results in similar operative outcomes and morbidity when compared with matched video-assisted thoracoscopic surgery cases. Ann Thorac Surg 2012; 93: 1598-604; discussion 1604-5. [DOI] [PubMed] [Google Scholar]
- 7).Barbash GI, Glied SA. New technology and health care costs—the case of robot-assisted surgery. N Engl J Med 2010; 363: 701-4. [DOI] [PubMed] [Google Scholar]
- 8).Bodner J, Augustin F, Wykypiel H, et al. The da Vinci robotic system for general surgical applications: a critical interim appraisal. Swiss Med Wkly 2005; 135: 674-8. [DOI] [PubMed] [Google Scholar]
- 9).Park BJ, Flores RM. Cost comparison of robotic, video-assisted thoracic surgery and thoracotomy approaches to pulmonary lobectomy. Thorac Surg Clin 2008; 18: 297-300, vii. [DOI] [PubMed] [Google Scholar]
- 10).Summary of Advanced Medical Care; Home page of Ministry of Health, Labour and Welfare in Japan (in Japanese)