Abstract
Purpose: Transcatheter aortic valve replacement (TAVR) has emerged as a therapeutic option for severe aortic valvular stenosis (AS). To determine the indication for TAVR, it is mandatory to clarify the characteristics of the patients who were judged as inoperable for conventional aortic valve replacement (cAVR).
Methods: Of 185 patients newly diagnosed as severe AS from March 2010 to April 2011, we studied the characteristics of 61 (33%) patients (mean age, 86 ± 8 years) who were judged as inoperable.
Results: Younger patients (<85 years old, n = 22) had more major comorbidities and lower left ventricular ejection fraction than older patients (≥85 years old, n = 39). Mean estimated mortality for cAVR by Japan score was 7.0% ± 7.4%. Japan score did not correlate to age and was calculated relatively low in the older age group (6.2% ± 7.0%) than the younger age group (8.3% ± 8.1%).
Conclusion: One thirds of severe AS patients were judged as inoperable. In advanced age patients, age itself and other factors, which are not included in the conventional scoring systems, might have contributed to the decision making not to perform cAVR by cardiologists. Further study is necessary to define risk factors except for age.
Keywords: aortic valvular stenosis, aortic valve replacement, transcatheter aortic valve replacement, inoperable AS, frailty
Introduction
Aortic valvular stenosis (AS) is a common heart disease in the elderly.1) Although conventional aortic valve replacement (cAVR) is an established procedure, elderly patients have higher operative mortality.2) According to the previous clinical studies in the western countries, at least 30% of severe AS patients did not undergo AVR due to older age and multiple comorbidities.3–6) Transcatheter aortic valve replacement (TAVR) has emerged as a therapeutic option for patients with severe AS and high operative risk scores.7,8) TAVR was started in October 2009 in Japan and satisfactory early and mid-term results have been reported.9) In the early trial in western countries, high surgical risk score (Society of Thoracic Surgeons (STS) score >10%; EuroSCORE >20%) was employed as one of the inclusion criteria of TAVR.7) In determining the indication of TAVR, it is mandatory to understand the characteristics of the patients who are judged as inoperable for cAVR. Previous studies concerning inoperable patients have been mainly reported from US and European countries.3–8) This study was the first study that assessed the characteristics of inoperable patients with severe AS in Japan and could provide an insight into further investigation of candidates for TAVR.
Materials and Methods
Study subjects
Severe AS was defined based on the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease.10) We sent questionnaires about inoperable AS patients to 21 hospitals in Hokkaido and obtained the responses from 17. Of the total 185 patients who were newly diagnosed as severe AS from 2010 April to 2011 March, 61 patients (33%) were judged as inoperable by the cardiologists in each hospital. The patients who refused cAVR were excluded from the study. The present study was approved by the Institutional Review Board in Hokkaido University Hospital. The use of the medical records for the present study was approved by the institutional ethics review board in each hospital.
Patient characteristics and surgical risk scores
Patient characteristics data were collected from the cardiologists in each hospital by using a questionnaire to assess the surgical risk by STS11) and Japan score.12) The questionnaire included the following factors for each AS patient: demographics (age, gender, body surface area), medical history (hypertension, diabetes mellitus, serum creatinine level, hemodialysis, chronic obstructive pulmonary disease (COPD), peripheral vascular disease, cerebral vascular disease, carotid artery stenosis), cardiac complications (coronary artery disease, left main trunk disease, old myocardial infarction, angina, previous coronary artery bypass grafting, previous percutaneous coronary intervention, New York Heart Association (NYHA) class, left ventricular ejection fraction (LVEF), mitral stenosis, tricuspid valve regurgitation, active endocarditis, pulmonary hypertension, atrial fibrillation/ventricular tachycardia), and medical treatment (catecholamine, steroid). Based on the collected data, we estimated operative mortality and morbidity by using on line STS Risk calculator ver. 2.73 (http://riskcalc.sts.org/STSWebRiskCalc273/) and Japan score calculator (http://www.jacvsd.umin.jp). In these systems, operative mortality was defined as both all cause death occurring during the hospitalization, even if after 30 days and those after discharge from the hospital, but within 30 days of the operation. Morbidities were defined as permanent stroke, renal failure, prolonged ventilation over 24 h, deep sternal wound infection, and reoperation for any reasons.13) According to SURTAVI model,14) major comorbidities were defined as diabetes mellitus, COPD, peripheral vascular disease, carotid artery stenosis, cerebral vascular disease, previous cardiac surgery, LVEF <35%, pulmonary hypertension (>60 mmHg), and renal failure. When the patient’s data of height and weight were missing in the answer sheets, the age-derived average values in the Japanese population from National Health and Nutrition Examination survey report published by Ministry of Health, Labour, and Welfare were used.
Statistical analysis
Continuous variables were presented as mean ± standard deviation. Categorical data were presented as number and percentages. χ2 test or Fisher’s exact test was used for the comparison of categorical data. Mann Whitney U test was used for the comparison of continuous values. Statistical analysis was performed using SPSS statistical software (version 15.0, SPSS, Inc., Chicago, Illinois, USA). A p value less than 0.05 was considered to be statistically significant.
Results
Characteristics of inoperable AS patients
The characteristics of severe AS patients judged as inoperable are shown in Table 1. The mean age was 86 years. Twenty two patients (36%) were less than 85 years old and 39 patients (64%) were 85 years old or more. Forty eight patients (79%) were more than 80 years old. In total, 29% of them had diabetes mellitus, 21% had COPD, 32% had coronary artery diseases, and 11% had renal failure on hemodialysis. Their mean serum creatinine value, excluding the patients on hemodialysis, was 1.3 ± 0.7 mg/dl. Compared with the older patients (≥85 years old), the younger patients (<85 years old) more frequently had diabetes mellitus (55% vs. 15%, p = 0.001), renal failure on hemodialysis (22% vs. 5%, p = 0.038), peripheral vascular disease (18% vs. 3%, p = 0.033), coronary artery disease (59% vs. 18%, p = 0.001), and pulmonary hypertension (32% vs. 8%, p = 0.015). The younger patients had lower LVEF than the older patients (55% ± 14% vs. 62% ± 13%, p = 0.044).
Table 1.
Characteristics of inoperable patients
| Total (n = 61) | Age <85 years (n = 22) | Age >85 years (n = 39) | P value | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 85.9 ± 7.8 | 77.6 ± 5.1 | 90.6 ± 4.3 | <0.001 |
| Male (%) | 44 (71) | 15 (68) | 29 (74) | 0.61 |
| Body surface area, m2 | 1.43 ± 0.15 | 1.52 ± 0.13 | 1.40 ± 0.13 | <0.001 |
| Medical history | ||||
| Hypertension (%) | 43 (69) | 17 (77) | 26 (67) | 0.38 |
| Diabetes mellitus (%) | 18 (29) | 12 (55) | 6 (15) | 0.001 |
| Serum creatinine (w/o HD), mg/dl | 1.3 ± 0.7 | 1.5 ± 0.9 | 1.2 ± 0.6 | 0.21 |
| Renal failure on hemodialysis (%) | 7 (11) | 5 (22) | 2 (5) | 0.038 |
| COPD (%) | 13 (21) | 4 (18) | 9 (23) | 0.65 |
| Peripheral vascular disease (%) | 5 (8) | 4 (18) | 1 (3) | 0.033 |
| Cerebral vascular disease (%) | 9 (15) | 5 (23) | 4 (10) | 0.19 |
| Carotid artery stenosis (%) | 1 (2) | 1 (5) | 0 (0) | 0.18 |
| Cardiac complications | ||||
| Coronary artery disease (%) | 20 (32) | 13 (59) | 7 (18) | 0.001 |
| Left main disease (%) | 4 (7) | 3 (14) | 1 (3) | 0.09 |
| NYHA class | 2.5 ± 0.7 | 2.5 ± 0.9 | 2.5 ± 0.7 | 0.85 |
| Old myocardial infarction (%) | 8 (13) | 3 (14) | 5 (13) | 0.93 |
| Angina (%) | 16 (26) | 7 (32) | 9 (23) | 0.46 |
| CABG (%) | 3 (5) | 1 (5) | 2 (5) | 0.92 |
| PCI (%) | 7 (11) | 5 (23) | 2 (5) | 0.038 |
| Ejection fraction, % | 59 ± 14 | 55 ± 14 | 62 ± 13 | 0.044 |
| Mitral stenosis (%) | 3 (5) | 1 (5) | 2 (5) | 0.92 |
| Tricuspid valve regurgitation (%) | 34 (56) | 14 (64) | 20 (51) | 0.35 |
| Pulmonary hypertension >60 mmHg (%) | 10 (16) | 7 (32) | 3 (8) | 0.015 |
| Atrial fibrillation (%) | 17 (27) | 7 (32) | 10 (26) | 0.61 |
| Medical treatment | ||||
| Catecholamine use (%) | 4 (7) | 2 (9) | 2 (5) | 0.55 |
| Steroid use (%) | 2 (3) | 1 (5) | 1 (3) | 0.68 |
| Estimated operative mortality | ||||
| STS score | 10.6 ± 7.9 | 9.0 ± 9.3 | 11.5 ± 7.0 | 0.23 |
| Japan SCORE | 7.0 ± 7.4 | 8.3 ± 8.2 | 6.2 ± 7.0 | 0.29 |
Values are mean ± SD; the differences were examined between patients <85 years old and patients ≥85 years old. AVR: aortic valve replacement; HD: hemodialysis; COPD: chronic obstructive pulmonary disease; CABG: coronary artery bypass grafting; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; STS: Society of Thoracic Surgeons
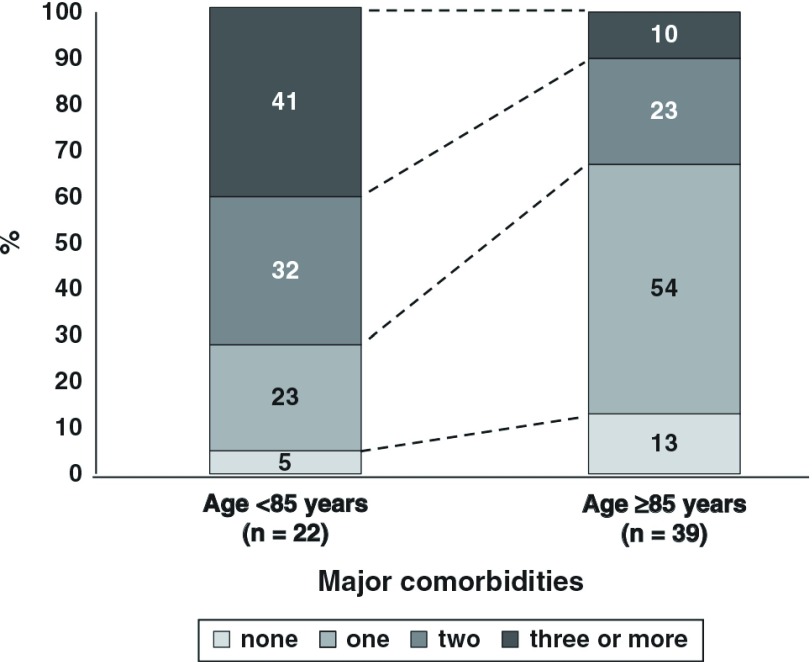
Figure 1 shows the prevalence of the number of major comorbidities according to SURTAVI model14) in the older (≥85 years) and younger (<85 years) groups. In the younger age group, over 70% of the patients had two or more major comorbidities. On the other hand, in the older age group, almost 70% had no or only one major comorbidity. Most of the older patients would have been considered inoperable because of age itself or other factors which are not in the scoring systems.
Fig. 1.
Prevalence of the number of major comorbidities in the older (≥85 years) and younger (<85 years) age groups. Major comorbidities were defined as diabetes mellitus, chronic obstructive pulmonary disease (COPD), peripheral vascular disease, carotid artery stenosis, cerebral vascular disease, previous cardiac surgery, left ventricular ejection fraction (LVEF) <35%, pulmonary hypertension (>60 mmHg), and renal failure.
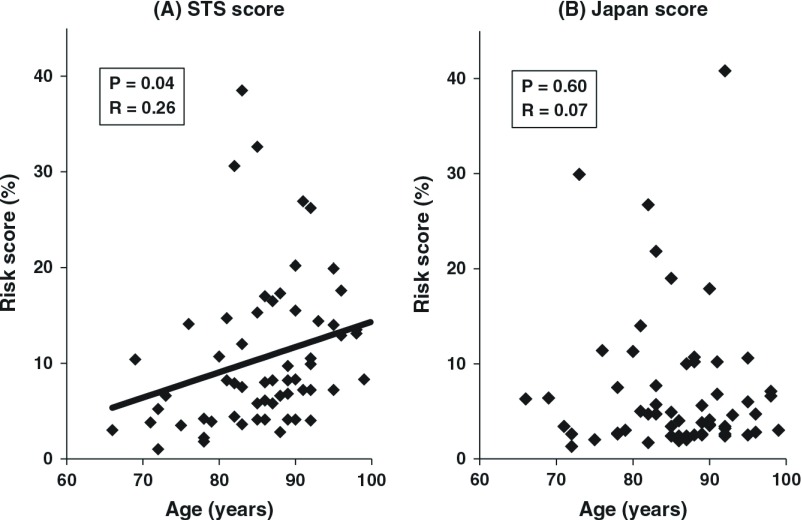
Estimated risk scores
In total, the estimated risk scores of operative mortality for cAVR were quite high: 10.6% ± 7.9% by STS score and 7.0% ± 7.4% by Japan score (Table 1). STS and Japan scores (operative mortality) in the two different age groups were not statistically different. Although the younger patients had more comorbidities than the older patients, the estimated operative mortality for cAVR was comparable between the two age groups. Figure 2 shows the estimated operative mortality as a function of age. The correlation coefficient between the STS and Japan scores and age was 0.26 (p = 0.04) and 0.07 (p = 0.60), respectively. Taken together, it is suggested that “older age” has greater influence on the risk score by STS than by Japan score system. Estimated mortality for cAVR by Japan score was calculated relatively low in the older age group (6.2% ± 7.0%) than the younger age group (8.3% ± 8.1%).
Fig. 2.
Estimated operative mortality (A, STS score; B, Japan score) as a function of age. STS: Society of Toracic Surgeons.
Discussion
The present study demonstrated that about 30% of severe AS patients were judged as inoperable by cardiologists. They were quite “high-risk” patients (STS score, 10.6% ± 7.9%), which was comparable to the reported value from European countries (3%–12%)6,7) (Table 2). In very old patients (≥85 years old), Japan score was calculated to be relatively low (6.2%). The factors other than “age”, such as dementia and frailty not included in the current scoring systems available for cAVR, might affect to the decision not to perform cAVR by cardiologists. Further study is necessary to define these risk factors especially in very old patients in the era of TAVR.
Table 2.
Summary of previous studies regarding inoperable severe AS patients
| Authors | Year | Country (No. of centers) | Patients analyzed | Mean age (years) | Percentage of patients ≥80 years | Risk scores | Percentage of inoperable patients |
|---|---|---|---|---|---|---|---|
| Bouma, et al.3) | 1999 | Netherland (3) | 205 | 78 | 46% | NA | 41% |
| Iung, et al.4) | 2005 | Europe (92) | 216 | 82 | 54% | Euro 9% | 33% |
| Charlson5) | 2006 | US (2) | 124 | 85 | NA | NA | 61% |
| Bach, et al.6) | 2009 | US (3) | 369 | 73 | 39% | STS 2.7% | 52% |
| Leon, et al.7) | 2010 | mainly US (21) | NA | 83 | NA | STS 12%; Euro 30% | NA |
| Present study | 2014 | Japan (17) | 61 | 86 | 79% | STS 11% | 33% |
Euro: EuroSCORE; NA: not applicable; STS: Society of Thoracic Surgeons score; US: United States
Comparison with previous studies regarding inoperable patients
Table 2 shows a summary of previous multicenter studies regarding the characteristics of patients judged as inoperable. Most of the studies have been reported from European countries and US.3–8) In the current study, the mean age of the patients was the oldest (86 years) and the percentage of patients more than 80 years old was the highest (79%). The risk score in the current study was relatively high (STS score 11%), which corresponded well to that in PARTNER trial.7,8) The percentage of inoperable patients was relatively low in our study compared with those in the other previous studies (33% vs. 33%–61%).
Is older age an operative risk for cAVR?
Hannan, et al. have reported higher age as the significant risk factor of early mortality for isolated cAVR.15) They suggested that the mortality gradually increased with each year after age of 55. Florath, et al. have reported that age especially more than 71 years old was the independent predictor for operative mortality in cardiac surgery.16) Di Eusanio, et al. reported that octogenarians had significant higher incidence of both hospital mortality and postoperative complications such as renal failure, stroke, atrial fibrillation, and third degree atrioventricular block.17) Handa, et al. recently examined 7883 Japanese patients who underwent cAVR by using the Japanese Adult Cardiovascular Surgery Database to assess the risk stratification for potential TAVR candidates and reported that the early mortality in the patients over 80 years old was significantly higher than those under 70 years old (5.2% vs. 2.1%).2)
Age is an important negative factor for decision making in performing cAVR. Iung, et al. reported that older age was the major reason for not considering cAVR.4) In our study, 64% of the inoperable patients were over 85 years old and their mean Japan score was relatively low (6.2% vs. 8.3% in the younger group). It is possible that cardiologists considered not only age itself but other factors not included in the scoring systems in decision making for cAVR.
Possible risk factors not included in the conventional scoring systems
There exist some criticisms for adapting the same risk scores for TAVR as cAVR. Several important comorbid conditions associated with adverse surgical outcomes are not included in Euro, STS, and Japan scores; porcelain aorta, chest radiation, liver cirrhosis, dementia, cancer, cachexia, and frailty.18) It is suggested that we should establish a new “TAVR score” to estimate operative mortality and quality of life after surgery.14)
In PARTNER trial cohort, Makkar, et al. reported that atherosclerosis and porcelain aorta were the main reasons for technical inoperability.19) cAVR may cause cerebral embolism, aortic dissection, mural laceration, and hemorrhage by using aortic cross-clamping.20) In a review of 221 patients having cardiac procedures on cardiopulmonary bypass, Blauth, et al. reported that 22% of patients had atheroembolic event after surgery. In patients with severe atherosclerosis, the risk of atheroembolic event increased to 37%.21) While ascending aorta replacement using deep hypothermic circulatory arrest is one method for establishing conventional cross-clamping and full-flow perfusion, the operative mortality of this strategy ranges from 6.8% to 10%22) and this procedure may increase surgical invasiveness for those patients.
Irradiation can affect all of the structures in the heart, including the three layers of the heart (pericardium, myocardium and endocardium) as well as the coronary vessels, the valvular and subvalvular apparatus, and the conduction systems. Pericardial adhesion is the most common manifestation and presents clinically in 60% to 70% of patients receiving mediastinal irradiation.23) The patients who received mediastinal irradiation therapy would have higher mortality and morbidity than the others due to higher incidence of bleeding and accidental damage of the heart structures.
Patients with liver cirrhosis undergoing heart surgery with cardiopulmonary bypass have an extremely high mortality risk. Arif, et al. reported 30-day mortality was 26% in patients with liver cirrhosis.24) Patients categorized as CHILD classification B and C had a significantly high 30-day mortality (33% and 40%, respectively) compared with CHILD A (20%). Modi, et al. reported estimated mortality rates of 5% for patients categorized as CHILD A, 32% for CHILD B, and 67% for CHILD C.25) Postoperative liver dysfunction, coagulation abnormalities, and difficulty in intravascular volume management would be the reasons for the worse outcome in patients with liver cirrhosis.24)
Frailty has been recently recognized as a significant factor to be taken into account when selecting patients for TAVR. Frailty is considered to be a distinct clinical syndrome characterized by a decrease in muscle mass and energy expenditure as well as mal-nutrition, leading to extreme vulnerability to adverse events.18) Frailty would also have a significant influence on postoperative quality of life in very old patients. Sumi, et al. reported that in octogenarians with independent activities of daily living before surgery, cardiac valvular surgery was safe and postoperative quality of life was satisfactory.26) It would be necessary for us to discuss the benefit of surgery for each patient in a heart team including cardiologists, cardiac surgeons, and other healthcare professionals.
Conclusion
One thirds of severe AS patients were considered inoperable. In very old patients, such factors other than “age” as frailty would have contributed to the decision making not to perform cAVR by cardiologists. Further study is necessary to establish a new risk scoring system in the era of TAVR.
Acknowledgements
We would like to thank the cardiologists in the participating hospitals for providing the patient data; Kazusuke Ito, Noriyoshi Kato, Kouichi Kanda, Naoya Matsumura, Isao Sato, Izumi Yoshida, Hiroshi Okamoto, Tetsurou Kouya, Shigeo Kakinoki, Takayuki Hirabayashi, Hisashi Matsuo, Kazushi Urasawa, Hideyuki Takano, Hiroshi Asajima, Takehiro Yamashita, Eiichirou Imamura, Masaharu Machida, Ichirou Yoshida, Takahiko Saitou, Hidetsugu Sakai.
Disclosure Statement
The authors have no conflict of interest in the publication of this manuscript.
References
- 1).Sakata R, Fujii Y, Kuwano H. Thoracic and cardiovascular surgery in Japan during 2008: annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2010; 58: 356-83. [DOI] [PubMed] [Google Scholar]
- 2).Handa N, Miyata H, Motomura N, et al. Procedure- and age-specific risk stratification of single aortic valve replacement in elderly patients based on Japan Adult Cardiovascular Surgery Database. Circ J 2012; 76: 356-64. [DOI] [PubMed] [Google Scholar]
- 3).Bouma BJ, van Den Brink RB, van Der Meulen JH, et al. To operate or not on elderly patients with aortic stenosis: the decision and its consequences. Heart 1999; 82: 143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Iung B, Cachier A, Baron G, et al. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery. Eur Heart J 2005; 26: 2714-20. [DOI] [PubMed] [Google Scholar]
- 5).Charlson E, Legedza AT, Hamel MB. Decision-making and outcomes in severe symptomatic aortic stenosis. J Heart Valve Dis 2006; 15: 312-21. [PubMed] [Google Scholar]
- 6).Bach DS, Siao D, Girard SE, et al. Evaluation of patients with severe symptomatic aortic stenosis who do not undergo aortic valve replacement: the potential role of subjectively overestimated operative risk. Circ Cardiovasc Qual Outcomes 2009; 2: 533-9. [DOI] [PubMed] [Google Scholar]
- 7).Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010; 363: 1597-607. [DOI] [PubMed] [Google Scholar]
- 8).Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011; 364: 2187-98. [DOI] [PubMed] [Google Scholar]
- 9).Maeda K, Kuratani T, Mizote I, et al. Early experiences of transcatheter aortic valve replacement in Japan. Circ J 2013; 77: 359-62. [DOI] [PubMed] [Google Scholar]
- 10).American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation 2006; 114: e84-231. [DOI] [PubMed] [Google Scholar]
- 11).Edwards FH, Peterson ED, Coombs LP, et al. Prediction of operative mortality after valve replacement surgery. J Am Coll Cardiol 2001; 37: 885-92. [DOI] [PubMed] [Google Scholar]
- 12).Motomura N, Miyata H, Tsukihara H, et al. Risk model of valve surgery in Japan using the Japan Adult Cardiovascular Surgery Database. J Heart Valve Dis 2010; 19: 684-91. [PubMed] [Google Scholar]
- 13).Shroyer AL, Coombs LP, Peterson ED, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg 2003; 75: 1856-64; discussion 1864-5. [DOI] [PubMed] [Google Scholar]
- 14).van Mieghem NM, Head SJ, van der Boon RM, et al. The SURTAVI model: proposal for a pragmatic risk stratification for patients with severe aortic stenosis. EuroIntervention 2012; 8: 258-66. [DOI] [PubMed] [Google Scholar]
- 15).Hannan EL, Racz MJ, Jones RH, et al. Predictors of mortality for patients undergoing cardiac valve replacements in New York State. Ann Thorac Surg 2000; 70: 1212-8. [DOI] [PubMed] [Google Scholar]
- 16).Florath I, Rosendahl UP, Mortasawi A, et al. Current determinants of operative mortality in 1400 patients requiring aortic valve replacement. Ann Thorac Surg 2003; 76: 75-83. [DOI] [PubMed] [Google Scholar]
- 17).Di Eusanio M, Fortuna D, De Palma R, et al. Aortic valve replacement: results and predictors of mortality from a contemporary series of 2256 patients. J Thorac Cardiovasc Surg 2011; 141: 940-7. [DOI] [PubMed] [Google Scholar]
- 18).Arai T, Lefèvre T. Who is the right patient for TAVI. J Cardiol 2014; 63: 178-81. [DOI] [PubMed] [Google Scholar]
- 19).Makkar RR, Jilaihawi H, Mack M, et al. Stratification of outcomes after transcatheter aortic valve replacement according to surgical inoperability for technical versus clinical reasons. J Am Coll Cardiol 2014; 63: 901-11. [DOI] [PubMed] [Google Scholar]
- 20).Daitoku K, Fukui K, Ichinoseki I, et al. Radiotherapy-induced aortic valve disease associated with porcelain aorta. Jpn J Thorac Cardiovasc Surg 2004; 52: 349-52. [DOI] [PubMed] [Google Scholar]
- 21).Blauth CI, Cosgrove DM, Webb BW, et al. Atheroembolism from the ascending aorta. An emerging problem in cardiac surgery. J Thorac Cardiovasc Surg 1992; 103: 1104-11; discussion 1111-2. [PubMed] [Google Scholar]
- 22).Girardi LN, Krieger KH, Mack CA, et al. No-clamp technique for valve repair or replacement in patients with a porcelain aorta. Ann Thorac Surg 2005; 80: 1688-92. [DOI] [PubMed] [Google Scholar]
- 23).Veeragandham RS, Goldin MD. Surgical management of radiation-induced heart disease. Ann Thorac Surg 1998; 65: 1014-9. [DOI] [PubMed] [Google Scholar]
- 24).Arif R, Seppelt P, Schwill S, et al. Predictive risk factors for patients with cirrhosis undergoing heart surgery. Ann Thorac Surg 2012; 94: 1947-52. [DOI] [PubMed] [Google Scholar]
- 25).Modi A, Vohra HA, Barlow CW. Do patients with liver cirrhosis undergoing cardiac surgery have acceptable outcomes. Interact Cardiovasc Thorac Surg 2010; 11: 630-4. [DOI] [PubMed] [Google Scholar]
- 26).Sumi M, Ariyoshi T, Miura T, et al. Are octogenerians in good condition after cardiac valvular surgery? Ann Thorac Cardiovasc Surg. 2014 doi: 10.5761/atcs.oa.13-00241. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]