Abstract
The prevalence of metabolic syndrome, a clustering of three or more risk factors that include abdominal obesity, increased blood pressure, and high levels of glucose, triglycerides, and high-density lipoproteins, has reached dangerous and costly levels worldwide. Increases in morbidity and mortality result from a combination of factors that promote altered glucose metabolism, insulin resistance, and metabolic dysfunction. Although diet and exercise are commonly touted as important determinants in the development of metabolic dysfunction, other environmental factors, including circadian clock disruption and activation of the aryl hydrocarbon receptor (AhR) by dietary or other environmental sources, must also be considered. AhR binds a range of ligands, which prompts protein–protein interactions with other Per-Arnt-Sim (PAS)-domain-containing proteins and subsequent transcriptional activity. This review focuses on the reciprocal crosstalk between the activated AhR and the molecular circadian clock. AhR exhibits a rhythmic expression and time-dependent sensitivity to activation by AhR agonists. Conversely, AhR activation influences the amplitude and phase of expression of circadian clock genes, hormones, and the behavioral responses of the clock system to changes in environmental illumination. Both the clock and AhR status and activation play significant and underappreciated roles in metabolic homeostasis. This review highlights the state of knowledge regarding how AhR may act together with the circadian clock to influence energy metabolism. Understanding the variety of AhR-dependent mechanisms, including its interactions with the circadian timing system that promote metabolic dysfunction, reveals new targets of interest for maintenance of healthy metabolism.
Keywords: aryl hydrocarbon receptor, metabolic syndrome, circadian rhythms
AhR Ligands
The aryl hydrocarbon receptor (AhR) is an evolutionarily ancient protein, which first appeared within the vertebrate class ∼450 million years ago. Although historically most frequently studied in the context of regulating responsiveness to environmental toxicants, both the existence of AhR prior to industrialization and the presence of naturally occurring ligands provide evidence for its integral importance to animal physiology.1,2 AhR can be activated through binding an array of diverse ligands that can be endogenous, naturally occurring, and/or anthropogenic.3–5
AhR activation by environmental pollutants, leading to its dimerization with aryl hydrocarbon nuclear transporter (ARNT) and subsequent activation of xenobiotic metabolizing enzymes such as cytochrome P4501A1 (Cyp1A1), has been a primary focus of toxicology studies for decades. Industrially produced AhR ligands include halogenated aromatic hydrocarbons, which are toxic chemical contaminants of the global ecosystem produced as byproducts of pesticide production, bleaching, and combustion processes. Dioxins are members of the polyhalogenated aromatic hydrocarbon family, consisting of two benzene rings connected by two oxygen atoms, with four to eight chlorine atoms added. Contamination with dioxin and dioxin-like compounds is widespread throughout the biosphere, including air, water, fish, and mammals.6 The entire human population, especially those living in industrialized countries, is exposed to these toxicants that act as potent, long-acting agonists for AhR.7 Although the most toxic of these man-made compounds can enter through the skin or lungs, food is the most common source, and, once internalized, these fat-soluble compounds bioaccumulate in the food chain.8–10 AhR is highly expressed in tissues that are exposed to the environment, including the gut, lungs, and skin. As a biological sensor, AhR is structured to respond to chemical changes in the environment. The ubiquitous presence of ligands suggests a long-standing role in responding to the components of foreign materials, including substances that are inhaled, ingested, or in contact with skin. Thus, it seems a logical candidate not only to regulate responses to toxic substances but also to act as an integrator of energy metabolism.
Other exogenous AhR ligands are naturally occurring components of food and herbal medicines, including indole metabolites, stilbenes, carotenoids, and flavonoids.11–13 The indole derivatives indole-3-carbinol (I3C) and it metabolite 3,3′-diindolylmethane (DIM) are components of cruciferous vegetables, including broccoli and cabbage. The stilbene resveratrol is found in red wine. Carotenoids, the yellow, orange, and red pigments produced by plants, are present in a variety of vegetables. Flavonoids and curcumin are other dietary polyphenols that activate AhR. Although considered less toxic, these lower affinity ligands are capable of activating AhR-dependent signaling. The array of potential dietary ligands suggests that AhR activation may be commonplace and physiological.
Phenotypic characteristics of mice that lack AhR provide further evidence of its physiological relevance. Germline AhR knockouts produced by three separate laboratories have demonstrated the importance of AhR for the physiological regulation of growth, fertility, and liver and cardiovascular development, as well as the expected decreased sensitivity to dioxin exposure.14 More recently, tissue-specific deletion models indicate that AhR is an important regulator of hepatic energy homeostasis, adipocyte and dendritic cell function, and cerebellar granule cell development.15–17 Although knockout studies are frequently cited as evidence for the activation of AhR in the absence of exogenous ligands, the range of molecules derived from food sources outlined above calls this idea into question. Nevertheless, knockout studies also prompted the search for endogenous ligands, and several have been identified. For example, ultraviolet light exposure produces tryptophan derivatives in the skin and liver in rodents and humans that bind AhR with high affinity.18,19 Activation of AhR by these compounds, although transient due to their rapid metabolism, potentially links AhR activity to daily oscillations in environmental illumination and to regulation of the circadian clock.20–22 A cocktail of tryptophan photo-products or the specific photoproduct 6-formylindolo[3,2-b] carbazole (FICZ) activates AhR and alters expression patterns of circadian clock genes in vivo in the liver, as well as in a cell line derived from the rat suprachiasmatic nucleus (SCN), the brain’s master clock.14 These data highlight the potential physiological functions of endogenous agonists, and demonstrate that AhR can interact with the circadian clock.
AhR Activation and Signaling
In the absence of a ligand, the inactive AhR is bound by a group of chaperone proteins that include heat shock protein 90 (HSP-90) and the AhR-interacting protein comprised PAS-A and prostaglandin E synthase (p23), and localizes within the cellular cytoplasm. PAS-B regions act as interactive surfaces for heterodimer and homodimer formation and function as the ligand-binding surface. Lipophilic AhR agonists enter the cell and bind specifically to the PAS-B region of the cytoplasmic AhR. Ligand binding causes a conformational change that exposes a nuclear localization sequence, and after phosphorylation by protein kinase C, the ligand-bound AhR complex subsequently translocates into the nucleus.23–25 In the nucleus, the PAS-A domain of AhR dimerizes with the aryl hydrocarbon receptor nuclear translocator (Arnt) through its PAS domain, and this heterodimer binds specific DNA sequences, identified as xenobiotic response elements within the promoters of target genes. Classical AhR target genes include phase I metabolizing enzymes, cytochrome P450, family 1, member 1A (Cyp1A1), cytochrome P450, family 1, member 2A (Cyp1A2), cytochrome P450, family 1, sub family B (Cyp1B1), phase II metabolizing enzymes, and AhR repressor, although many other genes may also be regulated by AhR/Arnt.26
Classical AhR signaling does not, however, account for all the cellular effects attributed to the activated AhR. AhR signaling may be influenced by the affinity of the ligand for the AhR, as well as by cell-type-specific properties and other environmental factors. Non-canonical signaling through AhR includes crosstalk with other nuclear receptors, regulation of cell cycle and MAP kinase cascades, modulation of the immune system, activation of immediate early genes, and interaction with the molecular circadian clock. Crosstalk between AhR and estrogen receptor (ER) signaling is perhaps the most well studied among the nuclear receptor interactions. Molecular processes that underlie these interactions remain under investigation, but are likely multifactorial. Proposed mechanisms include direct binding of liganded AhR to ER, competition between AhR and ER for the same transcriptional co-activators and co-repressors, enhanced estrogen metabolism resulting from inductions of phase I metabolizing enzymes, and proteosomal targeting of ER for degradation (reviewed in the studies by Shanle and Xu27 and Swedenborg and Pongratz28). Although AhR activation is most commonly anti-estrogenic, some AhR ligands are weakly estrogenic and the effects are context-dependent.27
AhR crosstalk with signaling pathways critical to cell-cycle progression highlights the involvement of AhR in tumorigenesis. The complex interface with the cell cycle is not completely delineated, but is dependent on protein–protein interactions with the retinoblastoma tumor suppressor protein (RB). This heterodimer acts transcriptionally to regulate both co-activation and co-repression during the G1 phase of the cell cycle. AhR also induces the p27 Kip1 cyclin/cdk inhibitor and the cyclin-dependent kinase inhibitor p21. Similarly, AhR is also an important regulator of immune cell compartments, especially in inflammation and autoimmunity.29 Clearly, AhR is a versatile receptor with a unique ability to sense chemical change in the environment. How it relates that chemical change into physiological adaptation remains a major topic for discovery.
AhR and the Circadian Clock
The perpetual existence of daily oscillations of the 24-hour light/dark cycle has led to an integration of environmental diurnality with physiological function. The endogenous circadian clock that drives internal timing synchronizes with the cyclic changes of the external environment to regulate processes such as the sleep–wake cycle, locomotion, feeding, and temperature such that they coordinately function at the appropriate time of day.30,31 In mammals, the central oscillator resides in a region of the basal hypothalamus called SCN and receives and relays information from the external environment.30 Circadian rhythms are generated by core clock genes that form transcriptional and translational feedback loops, controlling their own mRNA and protein levels. Specifically, the PAS-containing proteins Clock and Bmal1 form a heterodimer and bind to enhancer-box (Ebox) regions upstream of the PAS domain containing clock genes, most notably the Period and Cryptochrome (Cry) families.32,33 Increased levels of Per and Cry form heterodimers that feed back to inhibit Clock and Bmal1 directed transcription. Posttranslational mechanisms of casein kinase 1 delta and 1 epsilon phosphorylate Per proteins and target them for polyubiquitination and degradation, releasing the inhibition of Clock and Bmal1, thereby maintaining the 24-hour cycle of clock genes.34 Although the circadian clock is self-regulating, it is capable of sensing and adapting to change. Similar to AhR-dependent mechanisms that sense xenobiotics through PAS regions, the circadian clock uses Clock, Bmal1, and Per, PAS domain-containing proteins to regulate the circadian period. PAS domains, comprised of two 70 amino acid repeats identified as PAS A and PAS B, allow these proteins to function as environmental sensors and communicate downstream signals through gene transcription.3,35 AhR and Arnt are members of the same protein family, both containing basic helix–loop–helix (bHLH) domains, composed of two α helices with an inner loop sequence, and PAS structural motifs. The bHLH-PAS proteins are a subfamily of the bHLH family.3
The PAS domain facilitates heterodimer and homodimer formation among family members.3–5 PAS-domain-containing proteins are promiscuous in both their ligand binding and the formation of heterodimers, which allows for varied combinations of protein–protein interactions and crosstalk among intracellular signaling pathways. This promiscuity suggests that AhR can interact with other PAS-containing proteins outside its established canonical pathway, enhancing the possibility of activation of myriad signaling pathways.36
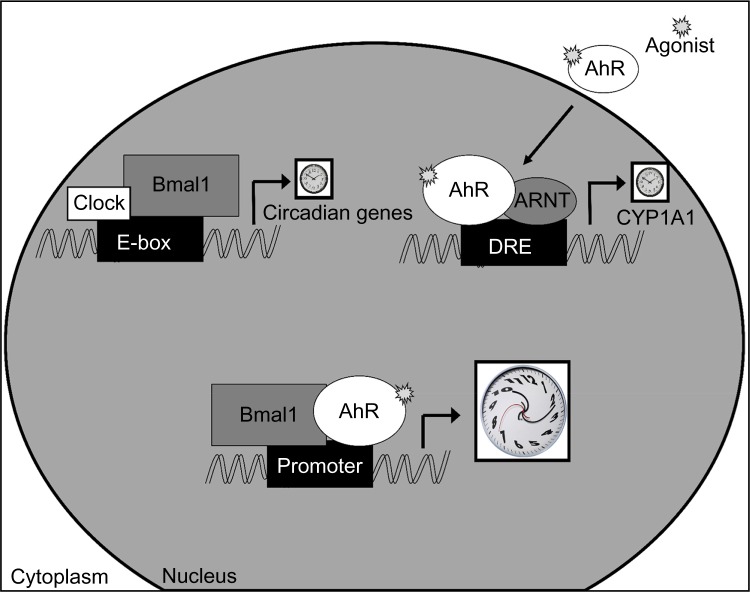
Following agonist-induced activation, AhR forms a heterodimer with the protein Arnt, which has a sequence homology similar to the clock protein Bmal1, including similar intron/exon splice patterns and conservation of five exons that compose the PAS domain.37 After ligand binding, the activated AhR enters the nucleus, where it can also form a heterodimer with Bmal1 in cultured hepatoma cells as well as in the ovary.38,39 This AhR/Bmal1 heterodimer disrupts the normal Clock/Bmal1 activation of Per1 on the Per1 promoter, resulting in the inhibition of Per1 transcription and dampened Per1 rhythm in liver (Fig. 1).39,40 Furthermore, Per1 and Bmal1 rhythms are altered in the SCN of mice exposed to 2,3,7,8-tetrachlorodibenzodioxin (TCDD).41 AhR is widely expressed in the central nervous system, including the hypo-thalamic SCN, the central circadian clock.42 Following intravenous injection of TCDD in rats, low levels of the dioxin are distributed in the brain, and the AhR target genes are upregulated.43,44 AhR activation in mice and hamsters alters rhythms of feeding and activity, gene expression, and the hormones prolactin, corticosterone, and melatonin.45–51 Human exposure to pesticides, which contain potent AhR agonists, increases the risk for idiopathic rapid eye movement sleep behavior disorder, further establishing a link between AhR, sleep, and circadian rhythms.52 Since AhR and Arnt are expressed within hypothalamic nuclei that regulate circadian rhythmicity, feeding behavior, and hormone secretion, and AhR activation alters gene expression in the hypothalamus, AhR-dependent mechanisms should be further explored.41,42,48,50
Figure 1.
AhR-induced circadian clock disruption. PAS-domain-containing family members are organized into class 1 and class 2 proteins. Class 1 proteins (white) can form either homodimers or heterodimers and bind to promoter sites to regulate transcription. Class 2 proteins (gray) cannot form homodimers but heterodimerize with other proteins. In the circadian system, the class 1 protein Clock binds to the class 2 protein Bmal1 and through Enhancer-box (Ebox) regions regulates circadian gene expression. AhR is a class 1 protein that binds the class 2 protein Arnt, regulating xenobiotic metabolism through DREs. PAS-domain-containing proteins can bind a variety of ligands and form diverse heterodimers, allowing for varied combinations of protein–protein interactions with other PAS-domain-containing proteins and crosstalk among signaling pathways.3 AhR and Bmal1 heterodimer formation disrupts downstream circadian signaling, promoting metabolic disorder.
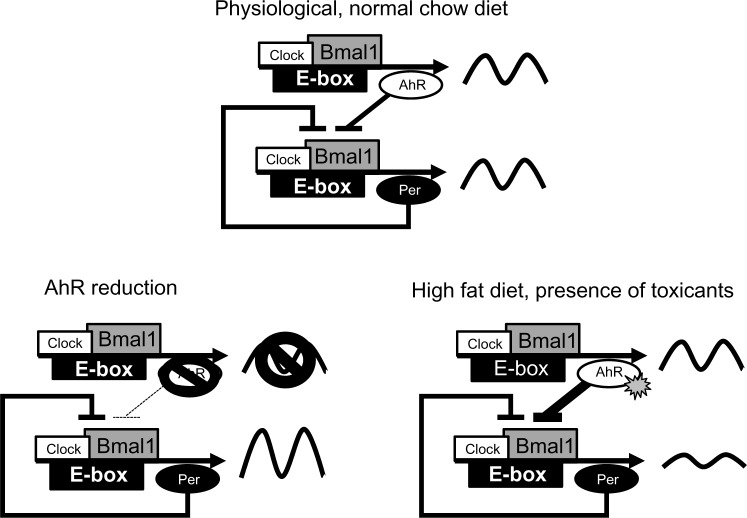
Activation of AhR alters the expression patterns of circadian clock genes and suppresses circadian rhythms. Reciprocally, genetic alteration of the circadian clock influences AhR signaling and sensitivity to agonist-induced activation of AhR and AhR target genes.40,53–55 Rhythmic expression of AhR mRNA and protein levels is regulated by an Ebox DNA-binding region within the AhR promoter, influencing rhythmic control of AhR expression through Clock/Bmal1-induced transcription.56–59 AhR is rhythmically expressed in the SCN and peripheral tissues.41 AhR target gene expression of Cyp1A1, Cyp1B1, and ARNT, although expressed at low levels under basal conditions, has a diurnal expression pattern with a peak that occurs during the day.41,57,58,60 In response to agonist exposure, Cyp1A1, a key target gene and indicator of AhR activation, has a rhythmic sensitivity that peaks during the night. However, in Per1/2 mutant mice, rhythmic sensitivity to agonist-induced Cyp1A1 expression is abolished, and overall Cyp1A1 levels are enhanced.53–55 Additionally, rhythmic oscillation of AhR mRNA and time-dependent sensitivity of target gene upregulation are absent in CLOCK mutant mice.61 Rhythmic expression of AhR and AhR target genes under basal conditions and time-dependent variations in sensitivity of AhR activation imply that the circadian system influences both physiological and exogenous AhR mechanisms. Overall, the circadian clock acts as a check on AhR sensitivity to ligands. Without an intact circadian clock, rhythmic expression of AhR is abolished, and, not surprisingly, the rhythm in sensitivity of the AhR to ligand-induced activation is also suppressed. However, without Per1, overall levels of Cyp1A1 are enhanced in response to agonist treatment. An examination of rhythmic expression patterns suggests that highest levels of AhR, with likely highest levels of sensitivity to agonist activation, occur when Per levels are near their trough. Thus, Per may act to suppress AhR protein, likely through an influence on CLOCK:BMAL1 transcriptional activity (Fig. 2). An influence of Per1 on Cyp1A1 stability must also be considered.
Figure 2.
Working model of AhR regulation of the clock. Under physiological conditions (top), some level of AhR activation may occur by endogenous ligands, exposure to UV light, or the presence of ligands in the diet. AhR is regulated by the clock, and its expression pattern shows diurnal rhythmicity. AhR acts as a brake on the clock, inhibiting the ability of Clock and Bmal1 to drive transcription. When AhR is reduced (lower left), in animals with genetic deletion of one or both alleles, the brake is removed and the amplitude of clock oscillations is enhanced. When AhR is overactivated (lower right) by the presence of toxicants, or a HFD, the inhibitory actions are increased, which contributes to the dampening of the circadian oscillation. Dampened circadian oscillations are strongly associated with systemic metabolic dysfunction.
Conversely, AhR also influences circadian integrity. Under control conditions, mice exposed to a 30-minute light pulse early during the lights-off period perceive this nocturnal light exposure as an extension of the lights-on period. In response, the circadian clock is delayed on subsequent days, which can be observed as an activity onset that occurs later than predicted on the following days. However, this light-induced phase delay in activity onset is severely attenuated in mice treated with either TCDD or β-napthoflavone (BNF), both AhR agonists.41 This effect holds when AhR agonists are applied to SCN-containing brain slices in vitro. Application of the neurotransmitter glutamate to SCN-containing brain slices mimics the effects of light, causing the same phase delay described above. Pretreatment of SCN slices with the AhR agonist FICZ blocks glutamate-induced phase resetting of the SCN electrical activity rhythm.22 These data suggest that AhR activation directly within the SCN impacts the ability of the clock to respond to phase-resetting stimuli. In addition to behavioral and electrical activity changes, circadian clock genes Per1 and Bmal1 in liver and SCN are altered in response to AhR agonists.40,41,62 AhR activation with BNF attenuates light-induced induction of Per1 in the SCN, providing an essential mechanism for the effects of AhR activation on light-induced changes in behavioral rhythmicity.
Furthermore, activation of the AhR by FICZ in the SCN cell line SCN2.2 alters the expression of the clock genes Per1, Cry1 and Cry2.22 Collectively, the data suggest that AhR expression, even under basal conditions, influences circadian rhythm strength. Overall, AhR expression and activation dampens the response of the circadian clock to perturbations in light and dampens the rhythmicity of clock gene rhythms. In contrast, when AhR is deleted, there is a tendency for the clock to have enhanced responsiveness to light at night and for increased amplitude of the Per1 rhythm.39,41,63 Further experimentation in AhR-null mice is needed for confirmation. Generally, the aggregate data suggest that AhR may act as a gain control on the circadian clock; activation of AhR suppresses rhythm amplitude, whereas inhibition of AhR strengthens rhythm amplitude (Fig. 2).
AhR and the Circadian Clock in Metabolic Disruption
Obesity and type 2 diabetes continue to burden society as a result of lifestyle choices, chemical exposures, genetics, and other contributing factors. In 2011, The World Health Organization predicted that 347 million people suffer from type 2 diabetes.64 Both circadian disruption and dioxin exposure promote metabolic dysfunction through parallel and overlapping mechanisms. Epidemiological evidence links circadian disruption, by shift work, to higher body mass index, increased triglycerides, glucose dysregulation, obesity, and higher incidence of metabolic syndrome, defined by the National Cholesterol Education Program as the presence of three or more of the following criteria: high waist circumference, blood pressure, fasting triglyceride levels, fasting high-density lipoprotein, or high fasting glucose levels.65–68 Mouse models of circadian disruption produce altered rhythms in core circadian genes as well as clock-controlled genes to include numerous rate-limiting metabolic genes, disrupted rhythms in lipid and glucose metabolism, and hepatic ste-atosis.69,70 AhR status influences circadian rhythm strength, even under controlled conditions. Rhythms of the clock genes Per1 and Bmal1 are significantly enhanced in the liver of AhR−/− mice compared to wild-type mice.41 Genetic manipulation to reduce AhR expression in mice enhances the ability of mice to adjust their behavior in response to an alteration in the timing of the light/dark cycle (Jaeger and Tischkau, unpublished results, April 2016). Together, these data suggest that the circadian timing system is more robust, both in terms of amplitude of oscillation and in adaptability to environmental change, when the AhR is inhibited or reduced.
Toxic responses to dioxins are mediated through the ligand-activated transcription factor AhR and upregulation of target genes that regulate xenobiotic metabolism.60,71 Chronic low-level exposure to dioxins is linked to insulin resistance and development of type 2 diabetes. Activation of AhR alters glucose metabolism, glucose tolerance, and insulin levels, and increases the risk of diabetes mellitus.72–76 AhR activation specifically within adipose tissue promotes inflammation and impairs glucose and insulin tolerance.16,77–79 Additionally, signaling downstream of tumor necrosis factor α–nuclear factor-kβ, which decreases glucose transporter type 4 expression and contributes to insulin resistance, is increased in adipose tissue of Vietnam veterans exposed to dioxins.80,81 AhR activation alters hepatic genes involved in fatty acid, lipid, and cholesterol metabolism pathways, including the peroxisome proliferator-activated receptor (PPAR) pathway, all of which mediate glucose and lipid homeostasis.62,82,83 Additionally, AhR activation induces an inflammatory response, which is implicated in the pathogenesis of metabolic disorders.78,84 This evidence points to a clear interaction between activated AhR and systemic energy metabolism. It seems likely that AhR plays a role in maintaining physiological balance in energy metabolism and that constant pathological activation of AhR upsets this balance, thereby contributing to metabolic disease. Perhaps most importantly, mechanisms that underlie physiological regulation of metabolism by AhR provide an opportunity to increase our understanding of how the body reacts to environmental stimulation.
Around 90% of human exposure to dioxins occurs through our diet, primarily through animal fat consumption.8 Besides TCDD and toxic pollutants, many compounds that influence AhR activity exist as natural components of fruits and vegetables.11,85,86 Additionally, the arachidonic acid metabolite, lipoxin A4, prostaglandins, specifically prostaglandin G2, and an arachidonic acid metabolite produced in inflammatory disease conditions, namely, 12(R)-hydroxy-5(Z),8(Z),10E, 14(Z)-dicosatetraenoic acid (12(R)-HETE), can act as AhR agonists.87–89 Lipid and lipid derivatives, such as oxidized low-density lipoproteins (OxLDL), have been identified as AhR agonists.90 OxLDL and saturated fatty acids contained in a Western diet activate AhR and contribute to obesity and inflammation in C57Bl/6 J mice.91 AhR activation also occurs through exposure to flavonoids and metabolites from fruits and vegetables, indole-3-carbinol, and herbal supplements including ginseng.12,92,93 Additionally, the consumption of fish and shrimp, which bioaccumulate organohalogens, increases potential dietary exposure.94 With a wide variety of AhR agonists present within food, or present due to secondary effects of diets that increase inflammatory mediators, exposure to AhR activation and its consequences are prevalent. Rather than focusing on the contribution of a single AhR ligand to AhR activation and downstream sequelae, it may be more important to consider the overall activation of AhR in response to the constellation of ligands, in terms of the overall metabolic consequences.
Mice lacking AhR expression have enhanced insulin sensitivity and improved glucose tolerance, although improved metabolism may differ depending on age, sex, housing, diet, and possible genetic drift.63,95–97 Mice with a low-affinity AhR allele fed a high-fat diet (HFD) are less susceptible to obesity, exhibiting differences in fat mass, liver physiology, and liver gene expression compared to mice with high-affinity AhR.98 AhR−/− and AhR+/− mice are resistant to the harmful effects of diet-induced obesity through protection against hepatic steatosis, insulin resistance, and inflammation. AhR-deficient mice fed an HFD have enhanced energy expenditure resulting from increased brown adipose tissue activity compared to AhR+/+ mice fed an HFD.99
HFD consumption disrupts circadian rhythms by altering circadian regulation of gene expression through inhibition of Clock/Bmal1 recruitment to chromatin, resulting in lost oscillation or phase advances of genes. A large number of metabolites in carbohydrate, lipid, metabolic, and xenobiotic pathways are regulated by Clock/Bmal1 binding to their promoter regions.100,101 Genes that lose rhythmic expression following HFD consumption often peak during the time period when Clock/Bmal1 is recruited to chromatin, which also coincides with peak the expression of AhR.41,102,103 Persistent activation of AhR alters circadian rhythm, primarily through inhibition of Clock/Bmal1-mediated target genes.39–41 Therefore, AhR-induced disruption of Clock/Bmal1 activity may play a role in HFD-induced disruption of metabolic rhythms. Furthermore, even deletion of a single AhR allele (AhR+/−) protects mice against diet-induced changes in transcriptional oscillations and also against glucose and metabolic gene rhythm disruption (Jaeger and Tischkau, unpublished results, April 2016). The persistence of the phenotype in the AhR heterozygote mice suggests a dosage effect. These studies highlight the involvement of AhR and the clock in the regulation of energy metabolism and provide interesting opportunities to explore novel therapies to combat poor metabolic health.
Summary and Future Studies
AhR is widely expressed throughout the body.104,105 Peripheral AhR activation and interaction with circadian signaling in metabolic tissues such as liver, adipose, and muscle has the potential to alter metabolism, but further studies are required to elucidate their detailed mechanisms. To study AhR signaling in vitro, use of the mouse Hepa-1c1c7 cell line (high AhR expression) and the Hepa-1c1c7-derived Hepa-1c1c12 (low AhR expression) allows comparison between varied levels of AhR expression.40 In addition to liver-derived Hepa-1c1c7 cells, cell lines derived from lung epithelia, keratinocytes, and fibroblasts can be used to study AhR signaling.106 In dispersed cells, however, the circadian clock frequently becomes desynchronized because of the lack of synchronizing signals provided in vivo by the SCN, the endocrine and autonomic nervous systems, and diet. Short exposure to high concentrations of serum (serum shock) can provide a synchronizing stimulus for circadian gene expression in mammalian tissue cultures. The mechanism of serum shock is hypothesized to mimic light-induced immediate early genes and synchronize circadian cycles, inherent within individual cells, to the population of cells in the dish.107 Thus, knowledge of the circadian system and its behavior in cultured cells, together with cell lines that differentially express the AhR, provide unique, yet underutilized opportunities to study the interaction between circadian rhythms and AhR signaling.
AhR and circadian signaling pathways regulate metabolic homeostasis through lateral and superimposed pathways. In addition to sharing PAS domain structure with circadian proteins, AhR demonstrates a rhythmic expression of transcription and sensitivity to activation by the AhR agonist TCDD.41,57,58 Reciprocally, AhR activation influences rhythmic strength of circadian clock genes, hormones, and behavioral responses to light-induced phase shifts.41,47,50 Correlations between AhR variants in mouse models and humans allow us to study how altered AhR affinity affects downstream signaling pathways.108 Epidemiological studies that explore the link between AhR polymorphisms and obesity may provide important information regarding the influence of AhR on physiological metabolism.
Decreasing AhR levels in mice by either knocking it out completely (AhR−/−) or knocking it down by at least 50% (AhR+/−) seems to enhance rhythms and bolster metabolism. In addition, the broad ligand-binding capacity of AhR suggests that manipulation of the receptor by an antagonist may promote healthier metabolism. The dietary component curcumin, a natural phenol found in spices, and resveratrol, a natural phenol found in red wine, along with synthetic compounds CH-223191, 6,2,4-trimethoxyflavone, and GNF351, have been reported as AhR antagonists.109–114 Given its importance in xenobiotic metabolism, complete blockade of AhR may not be desirable. Thus, partial inhibition of AhR, or specific inhibition of AhR-induced effects on Clock/Bmal1 and nuclear receptors PPARα and PPARγ and their downstream target genes that regulate glucose metabolism, may provide benefits while minimizing undesirable effects. It is becoming more evident that multiple mechanisms of AhR activation and downstream interaction with circadian rhythms and metabolism exist, but not all AhR-dependent consequences can be explained through dioxin response element (DRE)-dependent mechanisms. Understanding the variety of mechanisms by which AhR exerts its effects on metabolism may reveal new targets of interest for the conservation of homeostasis and reinforces the significance of AhR in clock disruption and metabolic disorder.
Footnotes
ACADEMIC EDITOR: Timothy Kelley, Editor in Chief
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1254 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE). Provenance: the authors were invited to submit this paper.
Author Contributions
Conceived and designed the experiments: CJ, SAT. Analyzed the data: CJ, SAT. Wrote the first draft of the manuscript: CJ, SAT. Contri buted to the writing of the manuscript: CJ, SAT. Agree with manuscript results and conclusions: CJ, SAT. Jointly developed the structure and arguments for the paper: CJ, SAT. Made critical revisions and approved final version: CJ, SAT. Both authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Hahn A, Poland E, Glover E, Stegeman J. Photoaffinity labeling of the Ah receptor: phylogenetic survey of diverse vertebrate and invertebrate species. Arch Biochem Biophys. 1994;310:218–28. doi: 10.1006/abbi.1994.1160. [DOI] [PubMed] [Google Scholar]
- 2.Hahn M. Aryl hydrocarbon receptors: diversity and evolution. Chem Biol Interact. 2002;141:131–60. doi: 10.1016/s0009-2797(02)00070-4. [DOI] [PubMed] [Google Scholar]
- 3.Gu Y, Hogenesch J, Bradfield C. The PAS superfamily: sensors of environmental and developmental signals. Annu Rev Pharmacol Toxicol. 2000;40:519–61. doi: 10.1146/annurev.pharmtox.40.1.519. [DOI] [PubMed] [Google Scholar]
- 4.McGuire J, Okamoto K, Whitelaw M, Tanaka H, Poellinger L. Definition of a dioxin receptor mutant that is a constitutive activator of transcription: delineation of overlapping repression and ligand binding functions within the PAS domain. J Biol Chem. 2001;276:41841–9. doi: 10.1074/jbc.M105607200. [DOI] [PubMed] [Google Scholar]
- 5.Reisz-Porszasz S, Probst M, Fukunaga B, Hankinson O. Identification of functional domains of the aryl hydrocarbon receptor nuclear translocator protein (ARNT) Mol Cell Biol. 1994;14:6075–86. doi: 10.1128/mcb.14.9.6075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rappe C, Buser H, Bosshardt HP. Dioxins, Dibenzofurans and Other Polyhalogenated Aromatics: Production, Use, Formation, and Destruction. The New York Academy of Sciences; New York: 1979. [Google Scholar]
- 7.Bohonowych J, Denison M. Persistent binding of ligands to the aryl hydrocarbon receptor. Toxicol Sci. 2007;98:99–109. doi: 10.1093/toxsci/kfm085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United States Environmental Protection Agency . Exposure and Human Health Reassessment of2,3,7,8-Tetrachlorodibenzo-p-Dioxin and Related Compounds. National Academy of Sciences Review Draft National Center for Environmental Assessment, Office of Research and Development; Washinton, DC: 2004. [Google Scholar]
- 9.United States Environmental Protection Agency Persistent Organic Pollutants: A Global Issue, a Global Response. 2015. https://www.epa.gov/international-cooperation/persistent-organic-pollutants-global-issue-global-response.
- 10.World Health Organization . Polychlorinated Biphenyls: Human Health Aspects (Concise International Chemical Assessment Document; 55) Geneva: World Health Organization; 2003. [Google Scholar]
- 11.Denison M, Nagy S. Activation of the aryl hydrocarbon receptor by structurally diverse exogenous and endogenous chemicals. Annu Rev Pharmacol Toxicol. 2003;43:309–34. doi: 10.1146/annurev.pharmtox.43.100901.135828. [DOI] [PubMed] [Google Scholar]
- 12.Bjeldanes L, Kim J, Grose K, Bartholomew J, Bradfield C. Aromatic hydrocarbon responsiveness-receptor agonists generated from indole-3-carbinol in vitro and in vivo: comparisons with 2,3,7,8-tetrachlorodibenzo-p-dioxin. Proc Natl Acad Sci U S A. 1991;88:9543–7. doi: 10.1073/pnas.88.21.9543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ciolino H, Daschner P, Yeh G. Dietary flavonols quercetin and kaempferol are ligands of the aryl hydrocarbon receptor that affect CYP1 A1 transcription differentially. Biochem J. 1999;340:715–22. [PMC free article] [PubMed] [Google Scholar]
- 14.Barouki R, Coumoul X, Fernandez-Salquero P. The aryl hydrocarbon receptor, more than a xenobiotic-interacting protein. FEBS Lett. 2007;581:3608–15. doi: 10.1016/j.febslet.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 15.Girer N, Murray I, Omiecinski C, Perdew G. Hepatic aryl hydrocarbon receptor attenuates fibroblast growth factor 21 expression. J Biol Chem. 2016;291(29):15378–87. doi: 10.1074/jbc.M116.715151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker N, Shoemaker R, English V, et al. Effects of adipocyte aryl hydrocarbon receptor deficiency on PCB-induced disruption of glucose homeostasis in lean and obese mice. Environ Health Perspect. 2015;123:944–50. doi: 10.1289/ehp.1408594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dever D, Adham Z, Thompson B, et al. Aryl hydrocarbon receptor deletion in cerebellar granule neuron precursors impairs neurogenesis. Dev Neurobiol. 2016;76:533–50. doi: 10.1002/dneu.22330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fritsche E, Schafer C, Calles C, et al. Lightening up the UV response by identification of the arylhydrocarbon receptor as a cytoplasmatic target for ultraviolet B radiation. Proc Natl Acad Sci U S A. 2007;104:8851–6. doi: 10.1073/pnas.0701764104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rannug U, Rannug A, Sjoberg U, Li H, Westerholm R, Bergman J. Structure elucidation of two tryptophan-derived, high affinity, Ah receptor ligands. Chem Biol. 1995;2:841–5. doi: 10.1016/1074-5521(95)90090-x. [DOI] [PubMed] [Google Scholar]
- 20.Rannug A, Rannug U, Rosenkranz H, et al. Certain photooxidized derivatives of tryptophan bind with very high affinity to the Ah receptor and are likely to be endogenous signal substances. J Biol Chem. 1987;262:15422–7. [PubMed] [Google Scholar]
- 21.Bergander L, Wincent E, Rannug A, Foroozesh M, Alworth W, Rannug U. Metabolic fate of the Ah receptor ligand 6-formylindolo[3,2-b]carbazole. Chem Biol Interact. 2004;149:151–64. doi: 10.1016/j.cbi.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Mukai M, Tischkau S. Effects of tryptophan photoproducts in the circadian timing system: searching for a physiological role for aryl hydrocarbon receptor. Toxicol Sci. 2007;95:172–81. doi: 10.1093/toxsci/kfl126. [DOI] [PubMed] [Google Scholar]
- 23.Ikuta T, Eguchi H, Tachibana T, Yonenda Y, Kawajiri K. Nuclear localization and export signals of the human aryl hydrocarbon receptor. J Biol Chem. 1998;273:2895–904. doi: 10.1074/jbc.273.5.2895. [DOI] [PubMed] [Google Scholar]
- 24.Fukunaga B, Probst M, Reisz-Porszasz S, Hankinson O. Identification of functional domains of the aryl hydrocarbon receptor. J Biol Chem. 1995;270:29270–8. doi: 10.1074/jbc.270.49.29270. [DOI] [PubMed] [Google Scholar]
- 25.Ikuta T, Kobayashi Y, Kawajiri K. Phosphorylation of nuclear localization signal inhibits the ligand-dependent nuclear import of aryl hydrocarbon receptor. Biochem Biophys Res Commun. 2004;317:545–50. doi: 10.1016/j.bbrc.2004.03.076. [DOI] [PubMed] [Google Scholar]
- 26.Bacsi S, Reisz-Porszasz S, Hankinson O. Orientation of the heterodimeric aryl hydrocarbon (dioxin) receptor complex on its asymmetric DNA recognition sequence. Mol Pharmacol. 1995;47:432–8. [PubMed] [Google Scholar]
- 27.Shanle E, Xu W. Endocrine disrupting chemicals targeting estrogen receptor signaling: identification and mechanisms of action. Chem Res Toxicol. 2011;24:6–19. doi: 10.1021/tx100231n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swedenborg E, Pongratz I. AhR and ARNT modulate ER signaling. Toxicology. 2010;268:132–8. doi: 10.1016/j.tox.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Feng S, Cao Z, Wang X. Role of aryl hydrocarbon receptor in cancer. Biochim Biophy Acta. 2013;1836:197–210. doi: 10.1016/j.bbcan.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Cuninkova L, Brown S. Peripheral circadian oscillators: interesting mechanisms and powerful tools. Ann N Y Acad Sci. 2008;1129:358–70. doi: 10.1196/annals.1417.005. [DOI] [PubMed] [Google Scholar]
- 31.Ralph M, Foster R, Davis F, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science. 1990;247:975–8. doi: 10.1126/science.2305266. [DOI] [PubMed] [Google Scholar]
- 32.Hardin P, Hall J, Rosbash M. Feedback of the Drosophila period gene product on circadian cycling of its messenger RNA levels. Nature. 1990;343:536–40. doi: 10.1038/343536a0. [DOI] [PubMed] [Google Scholar]
- 33.Jin X, Shearman L, Weaver D, Zylka M, de Vries G, Reppert S. A molecular mechanism regulating rhythmic output from the superchiasmatic circadian clock. Cell. 1999;96:57–68. doi: 10.1016/s0092-8674(00)80959-9. [DOI] [PubMed] [Google Scholar]
- 34.Lee C, Etchegaray J, Cagampang F, Loudon A, Reppert S. Posttranslational mechanisms regulate the mammalian circadian clock. Cell. 2001;107:855–67. doi: 10.1016/s0092-8674(01)00610-9. [DOI] [PubMed] [Google Scholar]
- 35.McIntosh B, Hogenesch J, Bradfield C. Mammalian Per-Arnt-Sim proteins in environmental adaptation. Annu Rev Physiol. 2010;72:625–45. doi: 10.1146/annurev-physiol-021909-135922. [DOI] [PubMed] [Google Scholar]
- 36.Denison M, Soshilov A, He G, DeGroot D, Zhao B. Exactly the same but different: promiscuity and diversity in the molecular mechanisms of action of the aryl hydrocarbon (dioxin) receptor. Toxicol Sci. 2011;124:1–22. doi: 10.1093/toxsci/kfr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu W, Ikeda M, Abe H, et al. Characterization of three splice variants and genomic organization of the mouse Bmal1 gene. Biochem Biophys Res Commun. 1999;260:760–7. doi: 10.1006/bbrc.1999.0970. [DOI] [PubMed] [Google Scholar]
- 38.Tischkau S, Jaeger C, Krager S. Circadian clock disruption in the mouse ovary in response to 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Lett. 2011;201:116–22. doi: 10.1016/j.toxlet.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu C, Wang C, Krager S, Bottum K, Tischkau S. Aryl hydrocarbon receptor activation attenuates Per1 gene induction and influences circadian clock resetting. Toxicol Sci. 2013;132:368–78. doi: 10.1093/toxsci/kfs345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu C, Krager S, Liao D, Tischkau S. Disruption of CLOCK-BMAL1 transcriptional activity is responsible for aryl hydrocarbon receptor-mediated regulation of Period1 gene. Toxicol Sci. 2010;115:98–108. doi: 10.1093/toxsci/kfq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mukai M, Lin T, Peterson R, Cooke P, Tischkau S. Behavioral rhythmicity of mice lacking AhR and attenuation of light-induced phase shift by 2,3,7,8-tetrachlorodibenzo-p-dioxin. J Biol Rhythms. 2008;23:200–10. doi: 10.1177/0748730408316022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petersen S, Curran M, Marconi S, Carpenter C, Lubbers L, McAbee M. Distribution of mRNAs encoding the arylhydrocarbon receptor, arylhydrocarbon receptor nuclear translocator, and arylhydrocarbon receptor nuclear translocator-2 in the rat brain and brainstem. J Comp Neurol. 2000;427:428–39. doi: 10.1002/1096-9861(20001120)427:3<428::aid-cne9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 43.Weber L, Ernst S, Stahl B, Rozman K. Tissue distribution and toxicokinetics of 2,3,7,8-tetrachlorodibenzo-p-dioxin in rats after intravenous injection. Fundam Appl Toxicol. 1993;21:523–34. doi: 10.1006/faat.1993.1129. [DOI] [PubMed] [Google Scholar]
- 44.Huang P, Rannug A, Ahlbom E, Hakansson H, Ceccatelli S. Effect of 2,3,7,8-tetrachlorodibenzo-p-dioxin on the expression of cytochrome P4501A1, the aryl hydrocarbon receptor, and the aryl hydrocarbon receptor nuclear translocator in rat brain and pituitary. Toxicol Appl Pharmacol. 2000;169:159–67. doi: 10.1006/taap.2000.9064. [DOI] [PubMed] [Google Scholar]
- 45.Jones M, Weisenburger W, Sipes I, Russell D. Circadian alterations in prolactin, corticosterone, and thyroid hormone levels and down-regulation of prolactin receptor activity by 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Appl Pharmacol. 1987;87:337–50. doi: 10.1016/0041-008x(87)90295-x. [DOI] [PubMed] [Google Scholar]
- 46.Seefeld M, Corbett S, Keesey R, Peterson R. Characterization of the wasting syndrome in rats treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Appl Pharmacol. 1984;73:311–22. doi: 10.1016/0041-008x(84)90337-5. [DOI] [PubMed] [Google Scholar]
- 47.Yellon S, Singh D, Garrett T, Fagoaga O, Nehlsen-Cannarella S. Reproductive, neuroendocrine, and immune consequences of acute exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin in the Siberian hamster. Biol Reprod. 2000;63:538–43. doi: 10.1095/biolreprod63.2.538. [DOI] [PubMed] [Google Scholar]
- 48.Pohjanvirta R, Tuomisto J. 2,3,7,8-tetrachlorodibenzo-p-dioxin enhances responsiveness to post-ingestive satiety signals. Toxicology. 1990;63:285–99. doi: 10.1016/0300-483x(90)90191-i. [DOI] [PubMed] [Google Scholar]
- 49.Pohjanvirta R, Tuomisto J, Linden J, Laitinen J. TCDD reduces serum melatonin levels in Long-Evans rats. Pharmacol Toxicol. 1989;65:239–40. doi: 10.1111/j.1600-0773.1989.tb01164.x. [DOI] [PubMed] [Google Scholar]
- 50.Linden J, Pohjanvirta R, Rahko T, Tuomisto J. TCDD decreases rapidly and persistently serum melatonin concentration without morphologically affecting the pineal gland in TCDD-resistant Han/Wistar rats. Pharmacol Toxicol. 1991;69:427–32. doi: 10.1111/j.1600-0773.1991.tb01325.x. [DOI] [PubMed] [Google Scholar]
- 51.Miller J, Settachan D, Frame L, Dickerson R. 2,3,7,8-Tetrachlorodibenzo-p-dioxin phase advances the deer mouse (Peromyscus manuculatur) circadian rhythm by altering expression of clock proteins. Organohalogen Compd. 1999;42:23–8. [Google Scholar]
- 52.Postuma R, Montplaisir J, Pelletier A, et al. Environmental risk factors for REM sleep behavior disorder: a multicenter case-control study. Neurology. 2012;79:428–34. doi: 10.1212/WNL.0b013e31825dd383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qu X, Metz R, Porter W, Neuendorff N, Earnest B, Earnest D. The clock genes period 1 and period 2 mediate diurnal rhythms in dioxin-induced Cyp1 A1 expression in the mouse mammary gland and liver. Toxicol Lett. 2010;196:28–32. doi: 10.1016/j.toxlet.2010.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qu X, Metz R, Porter W, Cassone V, Earnest D. Disruption of clock gene expression alters responses of the aryl hydrocarbon receptor signaling pathway in the mouse mammary gland. Mol Pharmacol. 2007;72:1349–58. doi: 10.1124/mol.107.039305. [DOI] [PubMed] [Google Scholar]
- 55.Qu X, Metz R, Porter W, Cassone V, Earnest D. Disruption of period gene expression alters the inductive effects of dioxin on the AhR signaling pathway in the mouse liver. Toxicol Appl Pharmacol. 2009;234:370–7. doi: 10.1016/j.taap.2008.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garrison P, Denison M. Analysis of the murine AhR gene promoter. J Biochem Mol Toxicol. 2000;14:1–10. doi: 10.1002/(sici)1099-0461(2000)14:1<1::aid-jbt1>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 57.Huang P, Ceccatelli S, Rannug A. A study on diurnal mRNA expression of CYP1A1, AHR, ARNT, and PER2 in rat pituitary and liver. Environ Toxicol Pharmacol. 2002;11:119–26. doi: 10.1016/s1382-6689(01)00111-9. [DOI] [PubMed] [Google Scholar]
- 58.Richardson V, Santostefano M, Birnbaum L. Daily cycle of bHLH-PAS proteins, Ah receptor and Arnt, in multiple tissues of female Sprague-Dawley rats. Biochem Biophys Res Commun. 1998;252:225–31. doi: 10.1006/bbrc.1998.9634. [DOI] [PubMed] [Google Scholar]
- 59.Zhang J, Yeager R, Klaassen C. Circadian expression profiles of drug-processing genes and transcription factors in mouse liver. Drug Metab Dispos. 2009;37:106–15. doi: 10.1124/dmd.108.024174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ko H, Okino S, Ma Q, Whitlock JJ. Dioxin-induced CYP1 A1 transcription in vivo: the aromatic hydrocarbon receptor mediates transactivation, enhancer-promoter communication, and changes in chromatin structure. Mol Cell Biol. 1996;16:430–6. doi: 10.1128/mcb.16.1.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tanimura N, Kusunose N, Matsunaga N, Koyanagi S, Ohdo S. Aryl hydrocarbon receptor-mediated Cyp1a1 expression is modulated in a CLOCK-dependent circadian manner. Toxicology. 2011;290:203–7. doi: 10.1016/j.tox.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 62.Sato S, Shirakawa H, Tomita S, et al. Low-dose dioxins alter gene expression related to cholesterol biosynthesis, lipogenesis, and glucose metabolism through the aryl hydrocarbon receptor-mediated pathway in mouse liver. Toxicol Appl Pharmacol. 2008;229(1):10–9. doi: 10.1016/j.taap.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 63.Wang C, Xu C, Krager S, Bottum K, Liao D, Tischkau S. Aryl hydrocarbon receptor deficiency enhances insulin sensitivity and reduces PPAR- alpha pathway activity in mice. Environ Health Perspect. 2011;119:1739–44. doi: 10.1289/ehp.1103593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Danaei G, Finucane M, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2–7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 65.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27 485 people. Occup Environ Med. 2001;58:747–52. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Karlsson B, Knutsson A, Lindahl B, Alfredsson L. Metabolic disturbances in male workers with rotating three-shift work. Results of the WOLF study. Int Arch Occup Environ Health. 2003;76:424–30. doi: 10.1007/s00420-003-0440-y. [DOI] [PubMed] [Google Scholar]
- 67.Pietroiusti A, Neri A, Somma G, et al. Incidence of metabolic syndrome among night-shift healthcare workers. Occup Environ Med. 2009;67:54–7. doi: 10.1136/oem.2009.046797. [DOI] [PubMed] [Google Scholar]
- 68.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 69.Barclay J, Husse J, Bode B, et al. Circadian desynchrony promotes metabolic disruption in a mouse model of shiftwork. PLoS One. 2012;7:e37150. doi: 10.1371/journal.pone.0037150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Turek F, Joshu C, Kohsaka A, et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science. 2005;308:1043–5. doi: 10.1126/science.1108750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mimura J, Fujii-Kuriyama Y. Functional role of AhR in the expression of toxic effects by TCDD. Biochim Biophys Acta. 2003;1619:263–8. doi: 10.1016/s0304-4165(02)00485-3. [DOI] [PubMed] [Google Scholar]
- 72.Calvert G, Sweeney M, Deddens J, Wall D. Evaluation of diabetes mellitus, serum glucose, and thyroid function among United States workers exposed to 2,3,7,8-tetrachlorodibenzo-p-dioxin. Occup Environ Med. 1999;56:270–6. doi: 10.1136/oem.56.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cranmer M, Louie S, Kennedy R, Kern P, Fonseca V. Exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) is associated with hyperinsulinemia and insulin resistance. Toxicol Sci. 2000;56:431–6. doi: 10.1093/toxsci/56.2.431. [DOI] [PubMed] [Google Scholar]
- 74.Henriksen G, Ketchum N, Michalek J, Swaby J. Serum dioxin and diabetes mellitus in veterans of Operation Ranch Hand. Epidemiology. 1997;8:252–8. doi: 10.1097/00001648-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 75.Bertazzi P, Consonni D, Bachetti S, et al. Health effects of dioxin exposure: a 20-year mortality study. Am J Epidemiol. 2001;153:1031–44. doi: 10.1093/aje/153.11.1031. [DOI] [PubMed] [Google Scholar]
- 76.Warner M, Mocarelli P, Brambilla P, et al. Diabetes, metabolic syndrome, and obesity in relation to serum dioxin concentrations: the Seveso women’s health study. Environ Health Perspect. 2013;121:906–11. doi: 10.1289/ehp.1206113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Arsenescu V, Arsenescu R, King V, Swanson H, Cassis L. Polychlorinated biphenyl-77 induces adipocyte differentiation and proinflammatory adipokines and promotes obesity and atherosclerosis. Environ Health Perspect. 2008;116:761–8. doi: 10.1289/ehp.10554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim M, Pelloux V, Guyot E, et al. Inflammatory pathway genes belong to major targets of persistent organic pollutants in adipose cells. Environ Health Perspect. 2012;120:508–14. doi: 10.1289/ehp.1104282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Baker N, Karounos M, English V, et al. Coplanar polychlorinated biphenyls impair glucose homeostasis in lean C57BL/6 mice and mitigate beneficial effects of weight loss on glucose homeostasis in obese mice. Environ Health Perspect. 2013;121:105–10. doi: 10.1289/ehp.1205421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fujiyoshi P, Michalek J, Matsumura F. Molecular epidemiologic evidence for diabetogenic effects of dioxin exposure in U.S. Air force veterans of the Vietnam war. Environ Health Perspect. 2006;114:1677–83. doi: 10.1289/ehp.9262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ruan H, Hacohen N, Golub T, Van Parijs L, Lodish H. Tumor necrosis factor-alpha suppresses adipocyte-specific genes and activates expression of preadipocyte genes in 3T3-L1 adipocytes: nuclear factor-kappaB activation by TNF-alpha is obligatory. Diabetes. 2002;51:1319–36. doi: 10.2337/diabetes.51.5.1319. [DOI] [PubMed] [Google Scholar]
- 82.Dere E, Lo R, Celius T, Matthews J, Zacharewski T. Integration of genome-wide computation DRE search, AhR ChIP-chip and gene expression analyses of TCDD-elicited responses in the mouse liver. BMC Genomics. 2011;12:365. doi: 10.1186/1471-2164-12-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Remillard R, Bunce N. Linking dioxins to diabetes: epidemiology and biologic plausibility. Environ Health Perspect. 2002;110:853–8. doi: 10.1289/ehp.02110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Boverhof D, Burgoon L, Tashiro C, et al. Comparative toxicogenomic analysis of the hepatotoxic effects of TCDD in Sprague Dawley rats and C57BL/6 mice. Toxicol Sci. 2006;94:398–416. doi: 10.1093/toxsci/kfl100. [DOI] [PubMed] [Google Scholar]
- 85.Denison MS, Heath-Pagliuso S. The Ah receptor: a regulator of the biochemical and toxicological actions of structurally diverse chemicals. Bull Environ Contam Toxicol. 1998;61:557–68. doi: 10.1007/pl00002973. [DOI] [PubMed] [Google Scholar]
- 86.Gasiewicz T, Kende A, Rucci G, Whitney B, Willey J. Analysis of structural requirements for Ah receptor antagonist activity: ellipticines, flavones, and related compounds. Biochem Pharmacol. 1996;52:1787–803. doi: 10.1016/s0006-2952(96)00600-4. [DOI] [PubMed] [Google Scholar]
- 87.Chiaro C, Patel R, Perdew G. 12(R)-Hydroxy-5(Z),8(Z),10(E),12(Z)-eicosatetraenoic acid [12(R)-HETE], an arachidonic acid derivative, is an activator of the aryl hydrocarbon receptor. Mol Pharmacol. 2008;74:1649–56. doi: 10.1124/mol.108.049379. [DOI] [PubMed] [Google Scholar]
- 88.Schaldach C, Riby J, Bjeldanes L. Lipoxin A4: a new class of ligand for the Ah receptor. Biochemistry. 1999;38:7594–600. doi: 10.1021/bi982861e. [DOI] [PubMed] [Google Scholar]
- 89.Seidel S, Winters G, Rogers W, et al. Activation of the Ah receptor signaling pathway by prostaglandins. J Biochem Mol Toxicol. 2001;15:187–96. doi: 10.1002/jbt.16. [DOI] [PubMed] [Google Scholar]
- 90.McMillan B Bradfield C. The aryl hydrocarbon receptor is activated by modified low-density lipoprotein. Proc Natl Acad Sci U S A. 2007;104:1412–7. doi: 10.1073/pnas.0607296104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Moyer B, Rojas I, Kerley-Hamilton J, et al. Inhibition of the aryl hydrocarbon receptor prevents Western diet-induced obesity. Model for AHR activation by kynurenine via oxidized-LDL, TLR2/4, TGFβ, and IDO1. Toxicol Appl Pharmacol. 2016;300:13–24. doi: 10.1016/j.taap.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jeuken A, Keser B, Khan E, Brouwer A, Koeman J, Denison M. Activation of the Ah receptor by extracts of dietary herbal supplements, vegetables, and fruits. J Agric Food Chem. 2003;51:5478–87. doi: 10.1021/jf030252u. [DOI] [PubMed] [Google Scholar]
- 93.Zhang S, Qin C, Safe S. Flavonoids as aryl hydrocarbon receptor agonists/antagonists: effects of structure and cell context. Environ Health Perspect. 2003;111:1877–82. doi: 10.1289/ehp.6322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tittlemier S. Dietary exposure to a group of naturally produced organohalogens (halogenated dimethyl bipyrroles) via consumption of fish and seafood. J Agric Food Chem. 2004;52:2010–5. doi: 10.1021/jf0347261. [DOI] [PubMed] [Google Scholar]
- 95.Biljes D, Hammerschmidt-Kamper C, Kadow S, et al. Impaired glucose and lipid metabolism in ageing aryl hydrocarbon receptor deficient mice. EXCLI J. 2015;14:1153–63. doi: 10.17179/excli2015-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Phillips T, Hen R, Crabbe J. Complications associated with genetic background effects in research using knockout mice. Psychopharmacology. 1999;147:5–7. doi: 10.1007/s002130051128. [DOI] [PubMed] [Google Scholar]
- 97.Thackaberry E, Bedrick E, Goens M, et al. Insulin regulation in AhR-null mice: embryonic cardiac enlargement, neonatal macrosomia, and altered insulin regulation and response in pregnant and aging AhR-null females. Toxicol Sci. 2003;76:407–17. doi: 10.1093/toxsci/kfg229. [DOI] [PubMed] [Google Scholar]
- 98.Kerley-Hamilton J, Trask H, Ridley C, et al. Obesity is mediated by differential aryl hydrocarbon receptor signaling in mice fed a Western diet. Environ Health Perspect. 2012;120:1252–9. doi: 10.1289/ehp.1205003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Xu C, Wang C, Zhang Z, et al. Aryl hydrocarbon receptor deficiency protects mice from diet-induced adiposity and metabolic disorders through increased energy expenditure. Int J Obes (Lond) 2015;39:1300–9. doi: 10.1038/ijo.2015.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Eckel-Mahan K, Patel V, Mohney R, Vignola K, Baldi P, Sassone-Corsi P. Coordination of the transcriptome and metabolome by the circadian clock. Proc Natl Acad Sci U S A. 2012;109:5541–6. doi: 10.1073/pnas.1118726109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Eckel-Mahan K, Patel V, Mateo S, et al. Reprogramming of the circadian clock by nutritional challenge. Cell. 2013;155:1464–78. doi: 10.1016/j.cell.2013.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hatanaka F, Matsubara C, Myung J, et al. Genome-wide profiling of the core clock protein BMAL1 targets reveals a strict relationship with metabolism. Mol Cell Biol. 2010;30:5636–48. doi: 10.1128/MCB.00781-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rey G, Cesbron F, Rougemont J, Reinke H, Brunner M, Naef F. Genome-wide and phase-specific DNA-binding rhythms of BMAL1 control circadian output functions in mouse liver. PLoS Biol. 2011;9:e1000595. doi: 10.1371/journal.pbio.1000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Carlstedt-Duke J. Tissue distribution of the receptor for 2,3,7,8-tetrachlorod-ibenzo-p-dioxin in the rat. Cancer Res. 1979;39:3172–6. [PubMed] [Google Scholar]
- 105.Carver L, Hogenesch J, Bradfield C. Tissue specific expression of the rat Ah-receptor and ARNT mRNAs. Nucleic Acids Res. 1994;22:3038–44. doi: 10.1093/nar/22.15.3038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.FitzGerald C, Fernandez-Salguero P, Gonzalez F, Nebert D, Puga A. Differential regulation of mouse Ah receptor gene expression in cell lines of different tissue origins. Arch Biochem Biophys. 1996;333:170–8. doi: 10.1006/abbi.1996.0378. [DOI] [PubMed] [Google Scholar]
- 107.Balsalobre A, Damiola F, Schibler U. A serum shock induces circadian gene expression in mammalian tissue culture cells. Cell. 1998;93:929–37. doi: 10.1016/s0092-8674(00)81199-x. [DOI] [PubMed] [Google Scholar]
- 108.Karchner S, Jenny M, Tarrant A, et al. The active form of human aryl hydrocarbon receptor (AHR) repressor lacks exon 8, and its Pro 185 and Ala 185 variants repress both AHR and hypoxia-inducible factor. Mol Cell Biol. 2009;29:3465–77. doi: 10.1128/MCB.00206-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Beedanagari S, Bebenek I, Bui P, Hankinson O. Resveratrol inhibits dioxin-induced expression of human CYP1A1 and CYP1B1 by inhibiting recruitment of the aryl hydrocarbon receptor complex and RNA polymerase II to the regulatory regions of the corresponding genes. Toxicol Sci. 2009;110:61–7. doi: 10.1093/toxsci/kfp079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ciolino H, Daschner P, Wang T, Yeh G. Effect of curcumin on the aryl hydrocarbon receptor and cytochrome P450 1 A1 in MCF-7 human breast carcinoma cells. Biochem Pharmacol. 1998;56:197–206. doi: 10.1016/s0006-2952(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 111.Kim S, Henry E, Kim D, et al. Novel compound 2-methyl-2H-pyrazole-3-carboxylic acid (2-methyl-4–0-tolylazo-phenyl)-amide (CH-223191) prevents 2,3,7,8-TCDD-induced toxicity by antagonizing the aryl hydrocarbon receptor. Mol Pharmacol. 2006;69:1871–8. doi: 10.1124/mol.105.021832. [DOI] [PubMed] [Google Scholar]
- 112.Murray I, Flaveny C, DiNatale B, et al. Antagonism of aryl hydrocarbon receptor signaling by 6,2′4′-trimethoxyflavone. J Pharmacol Exp Ther. 2010;332:135–44. doi: 10.1124/jpet.109.158261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Smith K, Murray I, Tanos R, et al. Identification of a high-affinity ligand that exhitibs, complete aryl hydrocarbon receptor antagonism. J Pharmacol Exp Ther. 2011;338:318–27. doi: 10.1124/jpet.110.178392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhao B, Degroot D, Hayashi A, He G, Denison M. CH223191 is a ligand-selective. Antagonist of the Ah (Dioxin) receptor. Toxicol Sci. 2010;117:393–403. doi: 10.1093/toxsci/kfq217. [DOI] [PMC free article] [PubMed] [Google Scholar]