Abstract
Serrated polyposis (SPP) is characterized by the development of multiple serrated polyps and an increased predisposition to colorectal cancer (CRC). In the present study, we aimed to characterize, at a clinical and molecular level, a cohort of SPP patients with or without a family history of SPP and/or polyps/CRC (SPP-FHP/CRC). Sixty-two lesions from 12 patients with SPP-FHP/CRC and 6 patients with sporadic SPP were included. The patients with SPP-FHP/CRC presented with an older mean age at diagnosis (p=0.027) and a more heterogeneous histological pattern of lesions (p=0.032) than the patients with sporadic SPP. We identified two molecular forms of SPP-FHP/CRC, according to the preferential location of the lesions: proximal/whole-colon or distal colon. Mismatch repair (MMR) gene methylation [mutS homolog 6 (MSH6)/mutS homolog 3 (MSH3)] or loss of heterozygosity (LOH) of D2S123 (flanking MSH6) were detected exclusively in the former (p=3.0×10−7), in most early lesions. Proximal/whole-colon SPP-FHP/CRC presented a higher frequency of O-6-methylguanine-DNA methyltransferase (MGMT) methylation/LOH, microsatel-lite instability (MSI) and Wnt mutations (19/29 vs. 7/17; 16/23 vs. 1/14, p=2.2×10−4; 15/26 vs. 2/15, p=0.006; 14/26 vs. 4/20, p=0.02) but a lower frequency of B-raf proto-oncogene, serine/threonine kinase (BRAF) mutations (7/30 vs. 12/20, p=0.0089) than the distal form. CRC was more frequent in cases of Kirsten rat sarcoma viral oncogene homolog (KRAS)-associated proximal/whole-colon SPP-FHP/CRC than in the remaining cases (4/4 vs. 1/8, p=0.01). Thus, SPP-FHP/CRC appears to be a specific entity, presenting two forms, proximal/whole-colon and distal, which differ in the underlying tumor initiation pathways. Early MGMT and MMR gene deficiency in the former may underlie an inherited susceptibility to genotoxic stress.
Keywords: colorectal cancer, genotoxic susceptibility, O-6-meth-ylguanine-DNA methyltransferase, mism atch repair gene methylation, serrated polyposis, proximal vs. distal colon
Introduction
Serrated polyposis (SPP), which was previously known as hyperplastic polyposis, is characterized by the presence of multiple colorectal epithelial polyps with a serrated architecture, termed serrated (SE) polyps, as well as an increased predisposition to colorectal cancer (CRC) (1–3). SE polyps differ from adenomatous (AD) polyps and are comprised of various lesions, namely: hyperplastic polyps (HPs), non-dysplastic lesions with normal proliferation and architecture but elongated crypts with a saw-toothed appearance; sessile serrated adenomas (SSAs), lesions that present abnormal proliferation and architecture and may or may not include dysplasia; and traditional serrated adenomas (TSAs) that are dysplastic polyps with prominent serration (1,4–6). The presence of multiple SE polyps has also been associated with other hereditary conditions, namely serrated pathway syndrome or Jass syndrome (7–9).
It has been proposed that these SE lesions arise through the serrated pathway rather than through the adenoma-carcinoma sequence pathway (7,10–13). It has also been suggested that the HP is the precursor lesion in this pathway, with SSA as an intermediate step which then progresses to an adenocarcinoma with or without microsatellite instability (MSI or MSS, respectively). At the molecular level, SE lesions associated with those hereditary serrated syndromes share some genetic alterations, namely the presence of B-raf proto-oncogene, serine/threonine kinase (BRAF) mutations and the methylator phenotype, termed CpG island methylator phenotype (CIMP) (14–16), although these are also common to the sporadic SE lesions.
However, the analysis of SPP lesions has revealed specific features which are distinct from the SE lesions occurring in a sporadic context; accordingly, in SPP, HPs, TSAs and CRC are preferentially located in the proximal colon, i.e. proximal to the splenic flexure (17–19). Moreover, patients with SPP have previously been found to present extensive DNA methylation in the normal mucosa of the proximal colon (20), suggesting the involvement of widespread gene promoter methylation (CIMP) (7,14,21). This phenotype appears to be related to MutL homolog 1 (MLH1) methylation, which has been associated with MSI status, rather than O-6-methylguanine-DNA methyltransferase (MGMT) methylation. However, MSI appears to be less frequent in SPP lesions than in sporadic lesions (14,22). Similarly, SPP lesions also exhibited a lower frequency of Kirsten rat sarcoma viral oncogene homolog (KRAS) mutations when compared with sporadic SE lesions (21,22). However, it was also found that most adenomas and CRCs from patients with SPP exhibited a classic morphology and that few of these had BRAF or KRAS mutations, although SE lesions presented a high frequency of mutations in these genes (22). Previous research has suggested that tumorigenesis associated with SPP may not necessarily follow the serrated pathway and may follow an alternate pathway, involving TSAs and tubulovillous adenomas (TVAs) as intermediate lesions that progress to MSS adenocarcinomas with KRAS mutations or even a traditional pathway with adenomatous polyposis coli (APC) mutations as the initiating events (10).
A review of published case studies of SPP reported that approximately 10–50% of patients with SPP have been described as having a family history of CRC (23). In agreement with these findings, several studies have described an increased risk of CRC in the first-degree relatives of probands diagnosed with SPP compared with the general population (2,17,18,24–28). These studies have contributed to the notion that there are SPP cases where heredity may play a role in the development of CRC and/or polyps. Indeed, another review on this subject reinforces the concept that familial SPP exists and also the importance of defining the genetic basis of familial SPP and of studying these families in a systematic manner (29).
Thus, in the present study, we aimed to characterize, at the clinical and molecular level, SE and AD lesions from a cohort of patients with SPP who had been stratified into two groups: patients with or without a family history of SPP and/or polyps/CRC in first-degree relatives, in order to elucidate the information available regarding this new SPP entity with an apparent hereditary component.
Patients and methods
Patients and specimens
Eighteen patients diagnosed with SPP according to the WHO diagnostic criteria (1) were included in this study: 12 patients with SPP associated with a family history of SPP and/or polyps/CRC (multiple or diagnosed at a young age) in first-degree relatives (designated herein as SPP-FHP/CRC) (11 index and one affected relative diagnosed simultaneously with the index patient), and 6 index patients without a family history of SPP/polyps/CRC (designated herein as sporadic SPP) from the familial colorectal cancer registry of the Portuguese Institute of Oncology of Lisbon Francisco Gentil (Lisbon, Portugal). No evidence of SPP and/or polyps/CRC was found in the first-degree relatives of the patients with sporadic SPP, either by regular colonoscopy examination or by the absence of symptoms. The patients were classified as presenting a family history of polyps in first-degree relatives (5/11), if at least one relative had been diagnosed with polyps at or under 52 years of age or with >10 polyps. We cannot exclude the possibility that some of these families, namely PH4 or PH6, may have Jass syndrome instead of SPP, due to the presence of a mixture of AD and SE lesions (7,9). All patients had developed >10 lesions prior to the date of recruitment.
Sixty-two lesions were included here: 1 hyperplastic colonic mucosa (HCM), 25 HPs, 8 TSAs, 11 SSAs, 1 adenomatous/serrated (AD/S) carcinoma (Ca), 1 serrated carcinoma (SCa), 8 tubular adenomas (TAs), 2 TVAs and 5 Ca. Two normal colonic mucosa (NCM) samples were also included in this study. Fresh colorectal lesions were obtained from colectomy or colonoscopy specimens from patients who underwent surgery or colonoscopy in the Portuguese Institute of Oncology of Lisbon Francisco Gentil. Sections from corresponding areas of the specimens submitted for diagnosis were divided into two parts: one was snap frozen in liquid nitrogen immediately after resection, while the other was formalin-fixed and paraffin-embedded.
Histological characterization, according to the WHO guidelines (1), was performed by experienced pathologists (R.F. and P.C.). The study was conducted in accordance with local ethical standards and in agreement with the Helsinki Declaration of 1975, as revised in 1983. Informed consent for diagnosis and additional investigational studies, which may result in improving the knowledge about the pathogenesis of the disease, was obtained from patients included in this study. Moreover, biological material used for DNA isolation was obtained from archival sections from colorectal adenomas and carcinomas specimens, submitted for diagnosis (histological classification) and derived from patients who underwent surgery or colonoscopy in the Portuguese Institute of Oncology of Lisbon Francisco Gentil; only somatic analysis was performed and samples are truly anonymized.
Methods
DNA isolation
DNA was isolated from fresh-frozen and/or paraffin-embedded tumor tissue and matched normal tissue. DNA was isolated from the paraffin-embedded tissues by proteinase K digestion, which was followed by phenol/chloroform extraction and ethanol precipitation, as previously described (30). DNA from the fresh frozen tissue was isolated by proteinase K digestion, followed by precipitation with a saturated NaCl solution and ethanol as previously described (31).
Somatic mutation analysis of the APC gene
APC mutation analysis was performed using the protein truncation test (PTT) for exon 15, as previously reported (30). Briefly, APC exon 15 was divided into four overlapping fragments that were amplified by polymerase chain reaction (PCR) and, subsequently, in vitro transcription and translation were performed using a TnT T7-coupled reticulocyte lysate system (Promega, Madison, WI, USA). In negative cases, the mutational cluster region was subsequently analyzed by automated sequencing in order to search for missense mutations. For the samples obtained from paraffin-embedded tissues, APC mutations were analyzed by single-strand conformational polymorphism (SSCP) or by automated sequencing (32).
Somatic mutation analysis of catenin beta 1 (CTNNB1)
Genomic DNA from each tumor sample was amplified by PCR for SSCP analysis of exon 3 of the CTNNB1 gene. The amplified products were analyzed in a mutation detection enhancement (MDE) gel and visualized by silver staining (33).
Somatic mutation analysis of the AXIN2 gene
AXIN2 mutation analysis was performed by amplification of a repetitive sequence containing the (G)7, (C)6 and (C)5 tracts (where a considerable mutation frequency was described) (34), followed by electrophoresis in 7% polyacrilamide gel containing formamide and urea and visualization by silver staining (33).
Somatic mutation analysis of BRAF, KRAS and neuroblastoma RAS viral (v-ras) oncogene homolog (NRAS) genes
BRAF (exon 15: forward primer 5′-TCATAATGCTTG CTCTGATAGGA-3′; reverse primer 5′-GGCCAAAAATTTAATCAGTGGA-3′, KRAS (exon 2: forward primer 5′-GTGTGACATGTTCTAATATAGTCA-3′; reverse primer 5′-GAATGGTCCTGCACCAGTAA) (35) and NRAS (exons 2 and 3-primers were kindly provided by Dr Branca Cavaco), were amplified by PCR. The DNA samples were amplified in a standard PCR buffer (Invitrogen, Waltham, MA, USA). Mutations in these genes were analyzed by automated sequencing.
Sequencing analysis
After amplification, PCR products were purified with Illustra GFX™ PCR DNA and Gel Band purification kit (GE Healthcare, Little Chalfont, UK) according to the manufacturer's instructions. Sequencing reactions were performed using the BigDye Terminator Cycle Sequencing kit and the respective products were analyzed on the ABI PRISM™ 310 Genetic Analyzer (both from Applied Biosystems, Foster City, CA, USA) using Sequencing Analysis software. The pathogenic relevance of missense variants was evaluated by comparing aminoacid sequences using PolyPhen software (http://genetics.bwh.harvard.edu/pph/) and SIFT software (http://sift.jcvi.org/).
MSI/loss of heterozygosity (LOH) analysis
MSI status was analyzed using the Bethesda panel of reference markers (36). Each colonic lesion and paired normal DNA were amplified by PCR for each of the microsatellite markers and analyzed in the ABI Prism™ 310 Genetic Analyzer using GeneScan software (Applied Biosystems). The lesions were classified as MSI-high (H) when showing MSI in two or more of the five markers, MSI-low (L) when MSI was detected in one of the markers, and MSS when none of the markers revealed instability (37). In cases exhibiting MSI-L, BAT-40 and MYCL markers were also analyzed and the lesions were classified as MSI-H when MSI was detected in >40% of the 7 markers analyzed; otherwise they were classified as MSI-L, as previousy described (37).
A total of 4 dinucleotide markers flanking MGMT (D10S1703, D10S1676, D10S169 and D10S1651) were analyzed for each colonic lesion and paired normal DNA in order to evaluate the presence of LOH. Each lesion was subsequently scored as demonstrating LOH if the ratio between the areas of the normal and the tumor alleles was >1.5 or <0.67.
Regarding the D5S346 marker, LOH was evaluated (and confirmed using the D5S1965 marker) as indicative of loss of the APC gene. LOH of D2S123 and D17S250 was also evaluated as described above.
Methylation analysis
The analysis of MGMT and mismatch repair (MMR) gene promoter methylation was performed by methylation-specific multiplex ligation-dependent probe amplification (MS-MLPA) (38) using the SALSA MS-MLPA KIT ME011 MMR, (MRC-Holland, Amsterdam, The Netherlands). MS-MLPA reactions were performed as described by the manufacturer. The samples were analyzed using GeneScan software on the ABI Prism™ 310 Genetic Analyzer (Applied Biosystems). The results were normalized using MRC Coffalyser MLPA-DAT software v.9.4 (MRC-Holland). A ratio of 0.15 or higher, corresponding to 15% of methylated DNA, was indicative of promoter methylation as described elsewhere (32,39).
Statistical analysis
Fisher's exact test (using a two-sided or 2×3 table) and the χ2 test (http://www.quantitativeskills.com/sisa/index.htm) were used to compare categorical variables, and the Student's t-test (http://www.physics.csbsju.edu/stats/t-test.html) was used to compared continuous variables. A p-value <0.05 was considered to indicate a statistically significant difference.
Results
Clinical characterization
Table I summarizes the clinical features of the 18 patients included in this study, stratified into two groups: SPP-FHP/CRC and sporadic SPP. The average age at diagnosis (i.e. the age at which they presented symptoms) among our cohort of SPP patients (n=18) was 55±11 years (range 25–80); however, it was significantly higher in the SPP-FHP/CRC group than in the sporadic SPP group [60±10 years (range 41–80) vs. 46±15 years (range 25–68), p=0.027 (Student's t-test)] (Table II).
Table I.
Clinical features of the patients evaluated in this study, histological characterization of the respective lesions and family history of SPP and/or polyps/CRC in first-degree relatives.
| Family | Patient ID | Age at diagnosis in years | Gender | Total number of lesions | Type of lesionsa | Preferential location of lesionsb | CRC | WHO diagnostic criteriac | No. of affected individuals in the family | Family historyd (age at diagnosis in years) |
|---|---|---|---|---|---|---|---|---|---|---|
| SPP-FHP/CRC | ||||||||||
| PH1 | A756 | 62 | M | >100 | HP+TALGD+TSALGD+SSA | Whole colone | No | 3 | 3 | Son, >45 SE polyps (42); Son, 2 SE polyps (37) |
| PH3 | A755 | 41 | F | >100 | HP+TSALGD+TVALGD+SSA+TALGD | Whole colone | No | 3 | 3 | Mother, CRC (67); maternal aunt, CRC (58) |
| PH4 | CA638 | 66 | M | 19 | TSA (LGD+HGD)+VA | Whole colon | Yesf | 1 | 5 | Twin brother, 20 AD and SE polyps (70); son, 2 AD polyps (37); nephew, 18 AD polyps (54) |
| CA636 | 69 | M | 50 | HP+TALGD+TSALGD+TVALGDg | Proximal | Yesf | 3 | |||
| PH5 | A193 | 69 | F | 40 | HP+TALGD+TVAHGD | Proximal | Yes | 3 plus 1 | 3 | Sister, 2 AD polyps (67); son, 1 SE polyp (52) |
| PH6 | A478 | 64 | M | 50–100 | HP+TSALGD+TALGD+SSA | Distale | No | 3 plus 1 | 5 | Father, CRC (57); sister, 7 polyps (61); daughter, 1 SE polyp (39); son, 2 AD polyps (35) |
| PH7 | A759 | 50 | M | 50–100 | HP+TA | Whole colon | Yes | 3 | 3 | Mother, 2 AD polyps (75); brother, 8 SE and AD polyps (47) |
| PH8 | A760 | 59 | F | 45 | HP+SSA+TSALGD | Proximal | No | 1 plus 3 | 4 | Maternal grandfather, CRC; mother, CRC (73); sister, 3 AD polyps (61) |
| PH12 | A758 | 57 | M | 40 | HP | Distal | Yes | 3 | 2 | Brother, 1 AD polyp (44) |
| PH14 | A686 | 80 | M | 49 | HP+TSALGD+TALGD | Distal | No | 3 | 4 | Daughter, 2 SE polyps (54); daughter, 11 SE and 1 AD polyps (42); son, 1 AD polyp (44) |
| PH19 | A993 | 58 | F | 17 | HP+TALGD | Distal | No | 1 | 3 | Mother, CRC; sister, 6 polyps (68) |
| PH33 | A983 | 49 | M | 45 | HP+TSALGD+TALGD+SSA | Distal | No | 1 plus 3 | 4 | Paternal uncle, polyps (69); father, 1 AD polyp (77); brother, 1 AD polyp (50) |
| Sporadic SPP | ||||||||||
| PH9 | A500 | 48 | F | 40 | HP+SSA+TSALGD | Whole colon | No | 1 plus 3 | 1 | -h |
| PH10 | A989 | 25 | F | <100 | HP | NA | Yes | 3 plus 1 | 1 | -h |
| PH11 | A757 | 53 | M | 50 | HP+TSA | Distal | Yesf | 3 | 1 | -h |
| PH16 | A990 | 68 | M | 15 | HP+SSA | Whole colon | No | 1 | 1 | -h |
| PH18 | A992 | 46 | F | 10 | TSALGD+HP | Distal | No | 1 | 1 | -h |
| PH22 | A951 | 33 | F | 31 | HP+TALGD | Distal | No | 1 plus 3 | 1 | -h |
The type of lesion(s) that was prevalent (≥70%) in each patient is indicated in bold.
We considered a proximal or distal preferential location of the lesions when at least 70% of the lesions (majority serrated) were located in the proximal or distal colon, respectively.
WHO clinical criteria for the identification of serrated polyposis (SPP), as revised in 2010: i) At least five serrated polyps proximal to the sigmoid colon, two of which are greater than 10 mm in diameter. ii) Any number of serrated polyps occurring proximal to the sigmoid colon in an individual who has a first-degree relative with SPP iii) More than 20 serrated polyps of any size distributed throughout the colon.
AH families showed a dominant inheritance pattern with the exception of PH12, that revealed a recessive pattern.
The polyps are larger in the proximal colon.
Adenomatous/serrated carcinoma (AD/S);
with areas of traditional serrated adenoma (TSA).
No evidence of SPP and/or polyps/CRC was found in first-degree relatives of the sporadic SPP patients, either by regular colonoscopy examination or by absence of symptoms. CRC, colorectal cancer; M, male; F, female; HP, hyperplastic polyp; TALGD, tubular adenoma with low grade dysplasia; TSALGD, traditional serrated adenoma with low grade dysplasia; TVAHGD, tubulovillous adenoma with high grade dysplasia; SSA, sessile serrated adenoma; SE, serrated; TVALGD, tubulovillous adenoma with low grade dysplasia; LGD, low grade dysplasia; HGD, high grade dysplasia; VA, villous adenoma; AD, adenomatous; TA, tubular adenoma; NA, not available; FHP, family history of SPP.
Table II.
Comparison between clinical features in patients with sporadic SPP and those with SPP-FHP/CRC.
| Clinical feature | SPP-FHP/CRC | Sporadic SPP | p-value |
|---|---|---|---|
| Age at diagnosis (years) | 60±10 | 46±15 | 0.027 (Student's t-test) |
| Preferential location of lesions | |||
| Whole colon | 4/12 (33%) | 2/5 (40%) | NS |
| Proximal | 3/12 (25%) | 0/5 | NS |
| Distal | 5/12 (42%) | 3/5 (60%) | NS |
| ≥40 lesions | 10/12 (83%) | 3/6 (50%) | NS |
| AD lesions | 10/12 (83%) | 1/6 (17%) | 0.013a |
| ≥3 types of lesions | 9/12 (75%) | 1/6 (17%) | 0.032a |
Statistically significant values are shown in bold. NS, non-significant (p>0.05).
Fisher's exact test (two-sided). AD, adenomatous; SPP, serrated polyposis; SPP-FHP/CRC, SPP associated with a family history of SPP and/or polyps/colorectal cancer (CRC) (multiple or diagnosed at a young age) in first-degree relatives.
The number of lesions was higher in the SPP-FHP/CRC group than in the sporadic SPP group (threshold, ≥40 lesions): [10/12 (83%) vs. 3/6 (50%) patients, respectively]. With respect to histological features, AD lesions were more frequent in the SPP-FHP/CRC group than in the patients with sporadic SPP [10/12 (83%) vs. 1/6 (17%), p=0.013]. Moreover, the patients with SPP-FHP/CRC presented a more heterogeneous spectrum of lesions in comparison with the patients with sporadic SPP. In agreement with these findings, the presence of three or more types of lesions was more frequent in the former group [9/12 (75%) vs. 1/6 (17%), p=0.032].
Regarding the location of the lesions in each patient, we observed that whereas some of the patients with SPP presented lesions dispersed uniformly throughout the whole colon, other patients with SPP presented a predominance of lesions in one of the two major segments, proximal or distal. Therefore, a prevalence of proximal or distal location of the lesions was considered when at least 70% of the lesions (majority SE) were located in the proximal or distal colon, respectively. In accordance, a preferential proximal location was observed in 3/12 (25%) of the SPP-FHP/CRC patients and in none of the patients with sporadic SPP (0/5). A preferential distal location was observed in 3/5 (60%) of the sporadic SPP patients and in 5/12 (42%) of the patients with SPP-FHP/CRC.
Molecular characterization
The molecular alterations found in each SPP-FHP/CRC lesion, namely mutations in RAS/RAF and Wnt signaling genes, MSI, MGMT and MMR methylation, LOH of MGMT locus and LOH at D2S123 and D17S250 markers, are presented in Table III. The spectra of these molecular alterations led us to observe that the somatic mutation/promoter hypermethylation spectra differs between those patients whose lesions were preferentially located in the proximal colon, or distributed throughout the whole colon, and those whose lesions were preferentially located in the distal colon, as shown in Table IV. This led us to stratify the patients with SPP-FHP/CRC into two groups, proximal/whole-colon and distal SPP-FHP/CRC.
Table III.
Results of the molecular analysis of SE and AD lesions from patients with SPP.
| A, Results of the molecular analysis of SE and AD lesions from patients SPP-FHP/CRC | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Family | Patient ID | Lesion ID | Type of lesion | Location of lesions | MSI | D2S123, D17S250 LOH | LOH of MGMT locus | Mutations
|
Promoter methylation | |||||
| APC | CTNNB1 | AXIN2 | BRAF | KRAS | MGMT | MMR genes | ||||||||
| Preferential location of lesions - proximal/whole-colon | ||||||||||||||
| PH1 | A756 | A756AS | TSALGD | NA | MSS′ | NC, NC | Yes | c.4099C>T (p.Q1367X) | N | N | – | N | M | MSH6 |
| A756AT1 | TALGD | NA | MSS′ | NC, N | No | c.4123C>T (p.H1375Y) | N | N | N | N | M | MSH6 | ||
| A756AT2 | TALGD | NA | MSS′ | NC, N | IC | c.4123C>T (p.H1375Y) | N | N | N | N | NM | NM | ||
| A756PH1 | HP | NA | MSS′ | NC, NC | Yes | N | N | – | N | N | M | MSH6, MSH3 | ||
| A756PH2 | SSA | NA | MSS′ | NC, N | IC | c.4289delC (p.T1430TfsX43) | N | N | – | N | M | MSH6 | ||
| PH3 | A755 | A755AS1 | TSALGD | Distal | MSI-H | NI, D17S250 | IC | NC | N | N | c.1785T>G (p.F595C) | N | – | – |
| A755AS2 | TSA | Proximal | MSI-L | NI, D17S250 | IC | c.4235G>A (p.G1412E) | c.115G>A (p.A39T) | N | c.1799T>A (p.V600E) | N | M | MSH6 | ||
| A755AS3 | TSALGD | Proximal | MSI-H | NI, NI | Yes | NC | N | N | N | N | NM | MSH6 | ||
| A755PH1 | HP | Proximal | MSI-L | NI, D17S250 | Yes | N | N | N | N | N | M | MSH6 | ||
| A755PH2 | SSA | Proximal | MSI-L | D2S123, D17S250 | IC | N | N | N | N | N | NM | NM | ||
| PH4 | CA638 | CA638AS | TSALGD | Distal | MSS | N, N | No | N | c.122C>T (p.T41I) | N | N | c.35G>C (p.G12A) | M | MSH3 |
| CA638C | Ca (AD/S) | Rectum | MSS | N, N | No | LOH | N | N | N | c.35G>A (p.Gl2D) | M | NM | ||
| CA636 | CA636AT1 | TALGD | Proximal | MSI-L | NI, D17S250 | Yes | c.4262delG (p.S1421MfsX52) | N | – | N | N | M | NM | |
| CA636C | Ca | Proximal | MSS | D2S123, N | Yes | NC | N | N | N | N | M | MLH3 | ||
| CA636AT2 | TALGD | Proximal | MSI-L | D2S123, NI | Yes | N | N | N | N | N | NM | NM | ||
| CA636AT3 | TALGD | Proximal | MSS | D2S123, D17S250 | Yes | N | N | N | c.1811G>A (p.W604X) | N | M | NM | ||
| CA636ATV | TVALGD | Proximal | MSI-H | NI, NI | IC | c.4024T>G (p.L1342V) | N | N | N | c.38G>A (p.G13D) | M | NM | ||
| PH5 | A193 | A193AT | TALGD | Proximal | MSI-L | N, D17S250 | IC | c.4189G>A (p.E1397K) | N | N | N | N | M | MSH6 |
| A193ATV | TVAHGD | Rectum | MSS | D2S123, N | Yes | c.4123C>T (p.H1375Y) | N | N | N | c.35G>A (p.G12D) | M | NM | ||
| A193C | Ca | Proximal | MSS | D2S123, D17S250 | Yes | N | N | N | N | N | M | NM | ||
| A193PH1 | HP | Proximal | MSS | D2S123, N | Yes | LOH, c.4123C>T (p.H1375Y) | N | N | N | N | M | NM | ||
| A193PH2 | HP | Proximal | MSS | D2S123, D17S250 | Yes | NC | N | N | N | N | M | NM | ||
| PH7 | A759 | A759T | Ca | Proximal | MSI-H | NI, N | IC | N | c.133T>C (p.S45P) | c.l994delG (p.G665AfsX24) | N | c.34G>A) (p.G12S) | NM | NM |
| PH8 | A760 | A643PA | HP | Proximal | MSS | NI, N | No | N | N | N | c.1799T>A (p.V600E) | N | M | NM |
| A643PB | HP | Distal | MSS | NI, N | No | N | N | N | c.1799T>A (p.V600E) | N | M | NM | ||
| A760AS1 | TSALGD | Proximal | MSS′ | NC, NC | Yes | LOH | N | N | c.1799T>A (p.V600E) | N | – | – | ||
| A760PH1 | SSA | NA | MSI-L | NI, D17S250 | – | c.3926_3930 delAAAGA (p.E1309DfsX2) | N | N | N | N | NM | NM | ||
| A760PH2 | SSA | Proximal | MSI-H | NI, NC | Yes | NC | N | N | N | N | – | – | ||
| A760PH3 | SSA | Proximal | MSI-L | NI, N | Yes | LOH | c.130C>T (p.P44S) | N | c.1799T>A (p.V600E) | N | NM | NM | ||
| A760PH4 | SSA | NA | MSI-L | NI, NC | Yes | LOH | N | N | N | N | NM | NM | ||
| A760PH5 | SSA | NA | MSI-L | NI, N | No | LOH | N | N | N | N | NM | NM | ||
| A760PH6 | SSA | NA | MSS | NI, N | No | LOH | N | N | N | N | NM | NM | ||
| Preferential location of lesions - distal | ||||||||||||||
| PH6 | A478 | A478PA2 | HP | NA | MSS | N, N | No | N | N | N | c.1799T>A (p.V600E) | N | M | NM |
| A478PB | HP | NA | MSS | N, N | – | N | N | N | c.1799T>A (p.V600E) | N | – | – | ||
| A478PC | NCM | NA | MSS | N, N | – | N | N | N | N | c.35G>T (p.G12V) | NM | NM | ||
| A478PD | NCM | NA | MSS | N, N | – | N | – | – | N | – | – | – | ||
| A478PE | HCM | NA | MSS | N, N | – | N | N | N | N | c.35G>A (p.G12D) | NM | NM | ||
| A478PF | TALGD | NA | MSS | N, N | – | N | N | N | N | N | NM | NM | ||
| A478PG | HP | NA | MSS | N, N | No | N | N | N | c.1799T>A (p.V600E) | N | M | NM | ||
| A478PH | HP | NA | MSS | N, N | No | N | N | N | c.1799T>A (p.V600E) | N | NM | NM | ||
| A462PH1 | SSA | NA | MSS | N, N | No | N | N | N | c.1799T>A (p.V600E) | N | M | NM | ||
| A462PH2 | SSA | NA | MSS | N, N | IC | N | N | N | c.1799T>A (p.V600E) | N | M | NM | ||
| PH12 | A758 | A758C | Ca | Distal | MSI-L | NI, NC | No | LOH | N | N | c.1799T>A (p.V600E) | N | M | NM |
| A758PH | HP | Rectum | MSI-L | NI, D17S250 | IC | LOH | N | N | c.1799T>A (p.V600E) | N | M | NM | ||
| PH14 | A686 | A686P1A | HP | Distal | MSS | N, N | No | N | N | N | N | c.35G>A (p.G12D) | NM | NM |
| A686P2B | HP | Distal | MSS | N, N | No | N | N | N | N | c.35G>T (p.G12V) | M | NM | ||
| A686P3C | HP | Distal | MSS | N, N | No | N | N | N | N | c.35G>A (p.G12D) | NM | NM | ||
| A686P4D | HP | Distal | MSS | N, N | No | N | N | N | N | c.35G>A (p.G12D) | NM | NM | ||
| A686P5E | HP | Distal | MSS | N, N | – | N | N | N | N | c.35G>T (p.G12V) | – | – | ||
| PH19 | A993 | A993PH1 | HP | Rectum | MSS* | – | Yes | NC | c.115G>A (p.A39T) | N | c.1799T>A (p.V600E) | N | – | – |
| PH33 | A983 | A983PA | HP | Proximal | MSS* | – | No | N | N | N | c.1799T>A (p.V600E) | N | NM | NM |
| A983PB | HP | Proximal | MSS* | – | No | N | N | N | c.1799T>A (p.V600E) | N | NM | NM | ||
| A983PC | HP | Distal | MSS* | – | No | N | N | N | c.1799T>A (p.V600E) | N | NM | NM | ||
| A983PD | TALGB | Distal | MSS* | No | c.4189G>T (p.E1397X) | N | N | N | N | NM | NM | |||
| B, Results of the molecular analysis of SE and AD lesions from patients with SPP without a family history of SPP and/or polyps/CRC in first-degree relatives | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Family | Patient ID | Lesion ID | Type of lesion | Location of lesions | MSI | D2S123, D17S250 LOH | Mutations
|
Promoter methylation | |||||
| APC | CTNNB1 | AXIN2 | BRAF | KRAS | MGMT | MMR genes | |||||||
| Preferential location of lesions - Proximal/whole-colon | |||||||||||||
| PH9 | A500 | A500PA1 | HP | Proximal | MSS | D2S123, NI | N | N | N | c.l799T>A(p.V600E) | N | NM | MLH1 |
| A500PB2 | HP | Proximal | MSS | N, NI | N | N | N | c.l799T>A(p.V600E) | N | NM | NM | ||
| PH16 | A990 | A990ASS | SSA | NA | MSS* | – | NC | N | N | N | N | M | NM |
| A990PH1 | HP | Rectum | MSS* | – | NC | N | N | N | N | NM | MSH3 | ||
| Preferential location of lesions - Distal | |||||||||||||
| PH10 | A989 | A989C | Ca | Distal | MSS* | – | NC | N | N | N | N | NM | NM |
| PH11 | A757 | A757AS1 | SCa | NA | MSS | N, N | c.4233delT (p.S1411RfsX4) | N | N | N | N | M | NM |
| PH18 | A992 | A992AS1 | TSALGB | Distal | MSS* | – | NC | N | N | c.l799T>A(p.V600E) | N | – | – |
| A992AS2 | TSALGB | Distal | MSS* | – | NC | N | N | N | N | – | – | ||
| PH22 | A951 | A951P1 | HP | Rectum | MSS* | – | N | N | N | c.l799T>A(p.V600E) | N | NM | NM |
| A951P2 | HP | Distal | MSS* | – | N | N | N | c.l799T>A(p.V600E) | N | NM | NM | ||
SE, serrated; AD, adenomatous; MSI, microsatellite instability; LOH, loss of heterozygosity; MMR, mismatch repair; NA, not available; MSS′, microsatellite stable (missing one marker, D2S123); NC, not completed; N, no mutation; -, not performed; M, methylated; IC, inconclusive; NM, non-methylated; MSI-H, microsatellite instability high; NI, not informative; MSI-L, microsatellite instability low; NCM, normal colonic mucosa; HCM, hyperplastic colonic mucosa; SCa, serrated carcinoma; MSH, mutS Homolog; SPP, serrated polyposis; CRC, colorectal cancer. MSS*, microsatellite stable (only performed for BAT-26, due to the lack of normal tissue for this sample). APC missense mutations were not taken into account, although p.H1375Y and p.E1397K mutations have been predicted by in silico analysis to be probably pathogenic (data not shown).
Table IV.
Molecular characterization of lesions from patients with SPP-FHP/CRC, stratified by preferential location of the lesions in each patient.
| Molecular characterization | Preferential location of lesions
|
p-value | |
|---|---|---|---|
| Proximal/whole-colon | Distal colon | ||
| Total Wnt gene mutations | 14/26 (54%) | 4/20 (20%) | 0.02b |
| Total RAS/RAF gene mutations | 12/30 (40%) | 18/20 (90%) | 3.7×10−4b |
| BRAF gene mutations | 7/30 (23%) | 12/20 (60%) | 0.0089 (χ2 test) |
| KRAS gene mutations | 5/32 (16%) | 6/20 (30%) | NS |
| MSIa | 15/26 (58%) | 2/15 (13%) | 0.0059b |
| MMR gene methylation and/or LOH of D2S123 | 17/18 (94%) | 0/11 | 3.0×10−7b |
| MGMT gene methylation | 19/29 (65%) | 7/17 (41%) | NS |
| LOH of MGMT locus | 16/23 (70%) | 1/14 (7%) | 2.2×10−4b |
Except for one lesion, microsatellite instability (MSI), either microsatellite instability-low (MSI-L) or microsatellite instability-high (MSI-H), was detected only in dinucleotide microsatellite markers.
Fisher's exact test (two-sided). SPP, serrated polyposis; CRC, colorectal cancer; SPP-FHP/CRC, SPP associated with a family history of SPP and/or polyps/CRC (multiple or diagnosed at a young age) in first-degree relatives; MMR, mismatch repair; LOH, loss of heterozygosity; MGMT, O-6-methylguanine-DNA methyltransferase. Statistically significant values are shown in bold. NS, non-significant (p>0.05).
Although the ratio between the different types of lesions in the two groups, proximal/whole-colon and distal, do not match, i.e. in the former a higher proportion of AD lesions have been analyzed [in a recent study, individuals with large and right-sided SE lesions also had significantly more AD lesions compared with those without such types of SE lesions (40)], we found differences with respect to the mutation spectrum, even considering only HPs or SSAs, which have been analyzed in both groups. Accordingly, HPs and SSAs from patients with proximal/whole-colon SPP-FHP/CRC presented RAS/RAF gene mutations less frequently [2/6 (33%) and 1/7 (14%) vs. 14/14 and 2/2, respectively, p=0.003 and p=0.08] whereas MMR gene methylation or LOH of D2S123 [flanking mutS homolog 6 (MSH6)] occurred more frequently (4/4 and 2/2 vs. 0/7 and 0/2, respectively, p=0.003 and p=0.33), when compared with the same type of lesions from distal SPP-FHP/CRC patients (Table V). Moreover, SE and AD lesions presented a similar spectrum of molecular alterations, especially among each patient. The exception were BRAF mutations that were significantly more frequent in SE lesions [17/36 (47%) vs. 2/14 (14%), p=0.05] (Table V). For each patient, either presenting proximal/whole-colon or distal SPP-FHP/CRC, the spectra of somatic molecular alterations detected in the lesions were similar regardless of the location of each specific lesion. For example, in a patient with a prevalence of proximal lesions, these presented a specific mutation pattern that was shared by the few distal lesions that were analyzed from the same patient and different from the proximal lesions from patients with a predominance of distal lesions and vice versa (Table IIIA).
Table V.
Molecular characterization of SPP-FHP/CRC lesions stratified by histological type of lesions and the preferential location of the lesions in each patient (proximal/whole-colon or distal).
| HCM | HP | TSA | SSA | SCa | SE lesions | TA | TVA | Ca | AD lesions | SE+AD lesions | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Wnt gene mutations | |||||||||||
| Proximal/whole-colon | – | 1/4 (25%)a | 4/4a | 6/7(86%)a | 1/1 | 12/16 (75%)b,c | 1/6 (17%) | 0/2 | 1/2 (50%) | 2/10 (20%)b | 14/26 (54%) |
| Distal colon | 0/1 | 2/14 (14%) | – | 0/2 | – | 2/17 (12%)c | 1/2 (50%) | – | 1/1 | 2/3 (67%) | 4/20 (20%) |
| Total RAS/RAF gene mutations | |||||||||||
| Proximal/whole-colon | – | 2/6 (33%) | 4/5 (80%) | 1/7 (14%) | 1/1 | 8/19 (42%)d | 1/6 (17%) | 2/2 | 1/3 (33%) | 4/11 (36%) | 12/30 (40%) |
| Distal colon | 1/1 | 14/14 | – | 2/2 | – | 17/17d | 0/2 | – | 1/1 | 1/3 (33%) | 18/20 (90%) |
| BRAF gene mutations | |||||||||||
| Proximal/whole-colon | – | 2/6 (33%) | 3/5 (60%) | 1/7 (14%) | 0/1 | 6/19 (32%)e | 1/6 (17%) | 0/2 | 0/3 | 1/11 (9%) | 7/30 (23%) |
| Distal colon | 0/1 | 9/14 (64%) | – | 2/2 | – | 11/17 (65%)e | 0/2 | – | 1/1 | 1/3 (33%) | 12/20 (60%) |
| KRAS gene mutations | |||||||||||
| Proximal/whole-colon | – | 0/6 | 1/6 (17%) | 0/8 | 1/1 | 2/21 (10%)f | 0/6 | 2/2 | 1/3 (33%) | 3/11 (27%) | 5/32 (16%) |
| Distal colon | 1/1 | 5/14(36%) | – | 0/2 | – | 6/17 (35%)f | 0/2 | – | 0/1 | 0/3 | 6/20 (30%) |
| MSI | |||||||||||
| Proximal/whole-colon | – | 1/5 (20%)g | 3/4 (75%)g | 6/7(86%)g | 0/1 | 10/17 (59%)h | 3/4 (75%) | 1/2 (50%) | 1/3 (33%) | 5/9 (56%) | 15/26 (58%) |
| Distal colon | 0/1 | 1/10(10%) | – | 0/2 | – | 1/13 (8%)h | 0/1 | – | 1/1 | 1/2 (50%) | 2/15 (13%) |
| MMR gene methylation and/or LOH of D2S123 | |||||||||||
| Proximal/whole-colon | – | 4/4 | 4/4 | 2/2 | 0/1 | 10/11 (91%)i | 4/4 | 1/1 | 2/2 | 7/7 | 17/18 (94%) |
| Distal colon | 0/1 | 0/7 | – | 0/2 | – | 0/10i | 0/1 | – | – | 0/1 | 0/11 |
| MGMT gene methylation | |||||||||||
| Proximal/whole-colon | – | 6/6j | 3/4 (75%) | 1/7 (14%) | 1/1 | 11/18(61%) | 4/6 (67%) | 2/2 | 2/3 (67%) | 8/11 (73%) | 19/29 (65%) |
| Distal colon | 0/1 | 4/11 (36%)j | – | 2/2 | – | 6/14 (43%) | 0/2 | – | 1/1 | 1/3 (33%) | 7/17(41%) |
| LOH of MGMT locus | |||||||||||
| Proximal/whole-colon | – | 4/6 (67%)k | 3/4 (75%) | 3/5 (60%) | 0/1 | 10/16 (63%)l | 3/4 (75%) | 1/1 | 2/2 | 6/7 (86%) | 16/23 (70%) |
| Distal colon | – | 1/11 (9%)k | – | 0/1 | – | 1/12 (8%)l | 0/1 | – | 0/1 | 0/2 | 1/14 (7%) |
Statistically significant values are shown in bold.
p=0.02, Fisher's exact test (2×3).
p=0.0091, Fisher's exact test (two-sided).
p=0.0011, Fisher's exact test (two-sided).
p=1.3×10−4, Fisher's exact test (two-sided).
p=0.049, Fisher's exact test (two-sided).
p=0.062, Fisher's exact test (two-sided).
p=0.017, Fisher's exact test (2×3).
p=0.0049, Fisher's exact test (two-sided).
p=3.12×10−5, Fisher's exact test (two-sided).
p=0.017, Fisher's exact test (two-sided).
p=0.027, Fisher's exact test (two-sided).
p=0.0045, Fisher's exact test (two-sided). SPP, serrated polyposis; CRC, colorectal cancer; SPP-FHP/CRC, SPP associated with a family history of SPP and/or polyps/CRC (multiple or diagnosed at a young age) in first-degree relatives; MMR, mismatch repair; HCM, hyperplastic colonic mucosa; HP, hyperplastic polyp; TSA, traditional serrated adenoma; TVA, tubulovillous adenoma; SSA, sessile serrated adenoma; TA, tubular adenoma; AD, adenomatous; Ca, carcinoma; SCa, serrated carcinoma; SE, serrated; LOH, loss of heterozygosity.
The abovementioned findings led us to analyze the molecular data from the patients with SPP-FHP/CRC, who were stratified into two groups: proximal/whole-colon and distal SPP-FHP/CRC.
Proximal/whole-colon vs. distal SPP-FHP/CRC
Mutations in the Wnt genes, as well as MSI, were significantly more frequent in the patients with proximal/whole-colon SPP-FHP/CRC than in the patients with distal SPP-FHP/CRC [14/26 (54%) vs. 4/20 (20%), p=0.02; 15/26 (58%) vs. 2/15 (13%), p=0.0059] (Table IV). Interestingly, among the proximal/whole-colon SPP-FHP/CRC samples, Wnt gene mutations were significantly more frequent in the SE lesions than in the AD lesions [12/16 (75%) vs. 2/10 (20%), p=0.0091]. In the SE lesions, Wnt gene mutations, as well as MSI, were more frequent in TSAs (4/4 and 3/4) and in SSAs (6/7 and 6/7) and rarely detected in HPs (1/4 and 1/5) (p=0.02 and p=0.017, respectively) (Table V).
Similarly, LOH of the MGMT locus and MGMT methylation were also more frequent in lesions from the patients with proximal/whole-colon SPP-FHP/CRC, in comparison with lesions from the patients with distal SPP-FHP/CRC [16/23 (70%) vs. 1/14 (7%), p=2.2×10−4; 19/29 (65%) vs. 7/17 (41%), p=0.1, respectively] (Table IV). The same difference was observed even considering SE lesions only (Table V). In particular, MGMT methylation was detected in all HP lesions (6/6) from proximal/whole-colon SPP-FHP/CRC, in contrast to the lower frequency observed in HPs from distal SPP-FHP/CRC (4/11, 36%) (p=0.017).
Interestingly, among lesions which were deemed informative for methylation analysis and loss of LOH of D2S123, the presence of MMR gene methylation or of the D2S123 LOH (flanking MSH6) was only observed in proximal/whole-colon SPP-FHP/CRC lesions [17/18 (94%) vs. 0/11, p=3.0×10−7]. These alterations were found in the majority of early lesions and in all histological types (Tables IIIA and IV). It is of note that MLH1 methylation was not detected in any of the SPP-FHP/CRC lesions, being observed only in one lesion from the sporadic SPP group (Table IIIB). Moreover, it is also of note that except for one lesion, MSI, either MSI-L or MSI-H was detected only in dinucleotide microsatellite markers.
By contrast to the abovementioned molecular alterations, in the SPP-FHP/CRC samples, BRAF and KRAS mutations were more frequent in the lesions located in the distal colon than those located in the proximal/whole-colon [12/20 (60%) vs. 7/30 (23%), p=0.0089 (χ2 test) and 6/20 (30%) vs. 5/32 (16%), respectively], although the latter was not statistically significant (Table IV). Considering only the SE lesions, mutations in the RAS/RAF genes were detected in all the lesions from the distal SPP-FHP/CRC, namely in all HPs (14/14), HCM (1/1) and in one NCM (Table IIIA), but in only 8/19 (42%) lesions from the proximal/whole-colon SPP-FHP/CRC (p=1.3×10−4).
With respect to KRAS/BRAF mutations, two groups of patients were observed among those with either proximal/whole-colon or distal SPP-FHP/CRC: one group whose lesions presented KRAS mutations (PH4, PH5, PH7 and PH14) and another group, whose lesions presented BRAF mutations (PH3, PH8, PH19 and PH33) (Table IIIA). One patient presented either BRAF- or KRAS-positive lesions (family PH6). Notably, CRC was more frequent in the patients with proximal/whole-colon SPP-FHP/CRC associated with KRAS mutations than in the remaining patients [4/4 vs. 1/8 (12%), p=0.01] (Tables I and IIIA).
Discussion
SPP-FHP/CRC and sporadic SPP differ at the clinical level
The patients with SPP-FHP/CRC and sporadic SPP differed with respect to clinical and histological features. The older mean age at diagnosis (60 vs. 46 years old) of the former may underlie a slower process of tumorigenesis. This is in contrast to that which has been observed in relation to other hereditary CRC syndromes, namely in familial adenomatous polyposis and in Lynch syndrome, which are diagnosed at an earlier age (usually ≤50 years old) compared to the age at diagnosis in patients with sporadic CRC (>60 years old) (32,41). The presence of a more heterogeneous histological pattern of lesions in patients with SPP-FHP/CRC, associated with the concomitant presence of both SE and AD lesions, compared with the lesions in patients with sporadic SPP, suggests the involvement of other pathways in the tumorigenic process associated with SPP-FHP/CRC, in addition to the serrated pathway of tumorigenesis.
Molecular alterations involved in tumor initiation distinguish between two forms of SPP-FHP/CRC: proximal/whole-colon and distal
Two forms of SPP-FHP/CRC appear to exist according to the preferential location of the lesions in the colon and rectum, proximal/whole-colon and distal, which differ with respect to the somatic events involved in tumor initiation. LOH and methylation of MGMT, MMR gene methylation and/or LOH of D2S123 and Wnt gene mutations appear to be the major somatic events that lead to tumor initiation in proximal/whole-colon SPP-FHP/CRC. By contrast, in distal SPP-FHP/CRC, KRAS or BRAF mutations were found in the majority of early lesions and thus seem to play a major role in tumor initiation.
We have previously shown that distinct Wnt gene mutations are selected in sporadic and hereditary CRC according to tumor location, i.e. proximal or distal colon (33,42). We and others have also proposed that this finding is the result of the selection of a specific level of β-catenin signaling, optimal for tumor formation, which differs along the colorectum, thus contributing to differences in lesion distribution in specific types of CRC, such as Lynch syndrome (42,43). Proving this, variable gradients in the number of stem cells and physiological Wnt activity have been demonstrated throughout the length of the intestinal tract (44). Thus, in a similar fashion, tumorigenic pathways may also differ between proximal and distal SPP-FHP/CRC.
MGMT and MMR alterations, followed by Wnt gene mutations, are involved in the initiation of proximal/whole-colon SPP-FHP/CRC
The exclusive detection of MMR gene methylation (mainly of MSH6) and/or LOH of D2S123 (flanking MSH6) in proximal/whole-colon SPP-FHP/CRC, in the majority of early lesions and in all histological types, appears to suggest that the MMR system plays an important role in the initiation of proximal/whole-colon SPP-FHP/CRC, which is in agreement with the high frequency of MSI (either MSI-L or MSI-H) in these lesions (58%). Interestingly, MMR methylation and, consequently, MMR deficiency were not associated with MLH1 methylation as has been previously observed in sporadic SE lesions located in the proximal colon (7), but rather with MSH6 or mutS homolog 3 (MSH3) methylation. Accordingly, a high frequency of LOH of the MSH3 locus has been recently described in sporadic MSI-L CRC, suggesting that the impairment of other MMR genes such as MSH3 or MSH6, as observed in the present study, are involved in an MSI-L pathway, instead of MLH1, which is usually associated with the MSI-H serrated pathway (45). The detection of MSI almost exclusively in dinucleotide microsatellite markers is in agreement with this finding, since this type of MSI has been described to be a characteristic feature of MSI-L tumors (46). Interestingly, in the present study, MSI was detected more frequently at D2S123 followed by D17S250.
MGMT methylation and LOH of the MGMT locus were the most frequent alterations in proximal/whole-colon SPP-FHP/CRC, and MGMT methylation was detected in all HPs, commonly known as the precursor lesion (12). Therefore, we suggest that, similarly to MMR alterations, LOH and methylation of MGMT may also be early events in SPP-FHP/CRC proximal/whole-colon tumorigenesis. Notably, among the 17 lesions informative for both MMR and MGMT alterations in this form of SPP-FHP/CRC, in 16 (94%) both events were noted (Table IIIA). It is known that MGMT deficiency results in the inability to repair O6-methylguanine in the DNA, caused by genotoxic stress, which, once accumulated, leads to the translocation of the MutSα complex (MSH2 and MSH6) into the nucleus, thus increasing GT mismatch binding activity (47). This may lead to a selective pressure for molecular changes that impair MSH2 or MSH6 function such as promoter hypermethylation or LOH, thus explaining the association between the latter and MGMT methylation in the same early SPP-FHP/CRC lesions. Thus, we suggest a primary role for MGMT methylation, O6-methylguanine errors and MMR alterations in tumor initiation of proximal/whole-colon SPP-FHP/CRC. We further suggest that this molecular signature may indicate that a germline defect in the mechanisms regulating the response to genotoxic stress underlies the genetic susceptibility in this form of SPP-FHP/CRC.
In the present study, the higher frequency of Wnt gene mutations in proximal SPP-FHP/CRC, particularly in SE lesions, when compared with the AD lesions, suggests that this pathway also plays an important role in this form of SPP-FHP/CRC, especially in the transition to SE adenoma since this frequency was significantly higher in TSA and SSA than in HP and HCM (p=8.4×10−4). In agreement, CTNNB1 or AXIN2 mutations, that are selected almost exclusively in proximal colorectal tumors with MSI (33), were detected in 4/14 (28%) TSAs and SSAs from proximal/whole-colon SPP-FHP/CRC. Moreover, among APC nonsense and missense mutations, the majority (7/8; 88%) were of the transition type which is a characteristic feature of cells presenting MMR defects (48–50).
The occurrence of LOH of D2S123 and/or D17S250 dinucleotide marker in the present study [17/48 (35%) and 7/51 (14%), respectively], has been previously described in Paneth cell metaplasia, a condition that is commonly observed in the small intestine and the proximal colon of elderly individuals (51,52). Therefore, MGMT deficiency may make these cells more exposed to genotoxic stress, thus leading to molecular changes in Wnt genes and consequently to commitment to Paneth cell lineage [to which Wnt gene mutations largely contribute (53)] and to Paneth cell metaplasia. Therefore, colonic mucosa with Paneth cell metaplasia may be one of the pre-neoplastic lesions in the development of proximal/whole-colon SPP-FHP/CRC.
BRAF and KRAS mutations play different roles in proximal and distal SPP-FHP/CRC
Our finding that patients with proximal/whole-colon or distal SPP-FHP/CRC may carry, preferentially, either KRAS or BRAF mutations, supports previous observations suggesting that different forms of SPP exist, depending on whether lesions follow a KRAS or a BRAF pathway (22).
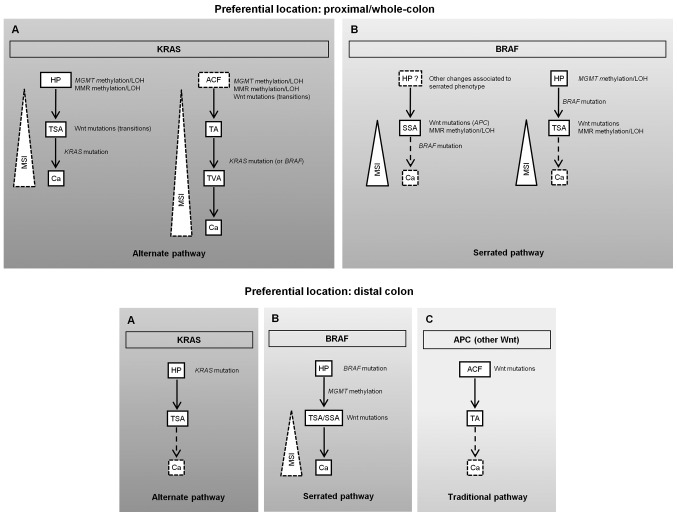
In addition, in the present study, we noted distinct roles for these mutations between proximal and distal SPP-FHP/CRC. BRAF or KRAS mutations were detected in the majority of distal SPP-FHP/CRC lesions, mostly SE early lesions, thus underlining their importance in early stages, whereas in proximal/whole-colon SPP-FHP/CRC these mutations (mainly of KRAS) appear to be more important in tumor progression (mostly detected in TSAs, TVAs and Cas). Accordingly, a KRAS or alternate pathway has been proposed to be involved in the transition from TSA or TVA to CRC in SPP (10). Indeed, in patients with proximal/whole-colon SPP-FHP/CRC, KRAS mutations were found only in TSAs, TVAs or Cas (PH4, PH5 and PH7) which is in accordance with their association with the development of a villous architecture and hence with malignant transformation (10,54–56). Therefore, as TSAs and TVAs shared early somatic events with HPs and TAs, respectively, from the same patients, and based on the model of SPP tumorigenesis previously presented by Leggett and Whitehall (10), we propose that proximal/whole-colon SPP-FHP/CRC tumorigenesis may follow an alternate or KRAS pathway, where TVA and TSA may develop from TA and HP, respectively, finally leading to CRC, that may or may not present with MSI (Fig. 1A, upper panel). Alternatively, a serrated or BRAF pathway (families PH3 and PH8) where SSA or TSA will probably lead to MSI-H cancer carrying BRAF mutations may also occur (Fig. 1B, upper panel). In this model, a deficient DNA repair pathway characterized by MGMT and MMR gene methylation and/or LOH followed by Wnt gene mutations, appears to be predominant in proximal SPP-FHP/CRC (Fig. 1, upper panel).
Figure 1.
Proposed pathways for colorectal tumorigenesis in proximal/whole-colon (upper panel) and distal serrated polyposis (SPP) associated with a family history of SPP and/or polyps/colorectal cancer (SPP-FHP/CRC) (bottom panel). Both of these forms may follow a KRAS (alternate) or a BRAF (serrated) pathway, (A and B), respectively, in the upper and lower panels. In addition, in distal SPP, an adenomatous polyposis coli (APC) (traditional) pathway may also occur [(C) in bottom panel]. Each lesion or molecular alteration in these proposed pathways is hypothesized based on the results obtained in the present study and we do not exclude that, in some cases, some of these molecular alterations may not occur, or even that other molecular alterations may also be found. The steps involving lesions that were not analyzed in this study and about which we have previously published information are represented by broken arrows. In some pathways a broken line was used to represent the increase in microsatellite instability (MSI) with tumor progression, to suggest a lower frequency in those cases. Ca, carcinoma; H P, hyperplastic polyp; MMR, mismatch repair; SSA, sessile serrated adenoma; TA, tubular adenoma; TSA, traditional serrated adenoma; TVA, tubulovillous adenoma.
In distal SPP-FHP/CRC, either KRAS (PH6 and PH14) or BRAF (PH6, PH12, PH19 and PH33) mutations play a major role in tumor initiation, either through an alternate or a serrated pathway (Fig. 1A and B, bottom panel, respectively). Wnt gene mutations and MMR defects were detected in the only carcinoma presented by these patients and thus are likely involved in tumor progression. As PH6 and PH33 also presented TAs and did not present TVAs, we hypothesize that, in distal SPP-FHP/CRC, some AD lesions may also develop through a traditional pathway initiated by APC mutations (Fig. 1C, bottom panel).
CRC is more frequent in patients with proximal/whole-colon SPP-FHP/CRC with TSAs, TVAs and KRAS mutations
The association of KRAS mutations in TSA or TVA with the development of CRC in proximal/whole-colon SPP-FHP/CRC suggests a higher contribution of the alternate pathway in the development of CRC in patients with SPP-FHP/CRC. Supporting our hypothesis, KRAS mutations have been previously described as more prevalent than BRAF mutations in a series of SE carcinomas occurring in the sporadic context, mainly in those presenting adjacent serrated adenomas (51%) (57). Moreover, in the same study, SE carcinomas were frequently MSS and presented a higher frequency of MGMT loss compared with traditional carcinomas, which is in agreement with our findings demonstrating that MGMT deficiency plays a prominent role in SPP-FHP/CRC, mainly in the proximal colon.
The findings that KRAS and BRAF mutations promote serrated and hyperplastic features, despite being incapable of initiating colonic adenoma development by themselves (58,59), may contribute to the apparent lower incidence of CRC in distal SPP-FHP/CRC, as according to the results of our present study, KRAS or BRAF mutations appear to be the initial molecular events in this form. However, additional studies involving more families are warranted.
In conclusion, SPP-FHP/CRC appears to be a distinct clinical and histological entity differing from sporadic SPP. However, we suggest that two forms of SPP-FHP/CRC appear to exist, proximal/whole-colon and distal, which differ mainly in the molecular alterations detected in early lesions. We further propose that a germline defect in the mechanisms regulating the response to genotoxic damage may underlie the genetic susceptibility in the former. In addition, our results suggest that CRC appears to develop more frequently in proximal/whole-colon SPP-FHP/CRC following an alternate KRAS pathway, thus underlining the importance of a complete clinical, histological and molecular characterization for CRC risk evaluation in further studies involving families with SPP. The results of these studies may be used to design appropriate guidelines for the clinical management of proximal and distal colonic presentations of SPP that assumes major relevance considering the increased risk of CRC and/or polyps in first-degree relatives.
Acknowledgments
The authors thank all the patients who participated in this study, Dr Inês Francisco for the DNA extraction and Dr Branca Cavaco for the primers for the NRAS gene. This study was sponsored and financed by a grant from Núcleo Regional do Sul, Liga Portuguesa Contra o Cancro, Terry Fox (NRS/LPCC-Terry Fox), and Fundação para a Ciência e Tecnologia (FCT), POCI/SAU-OBS/56921/2004.
Abbreviations
- AD
adenomatous
- APC
adenomatous polyposis coli
- AD/S
adenomatous/serrated
- BRAF
B-raf proto-oncogene, serine/threonine kinase
- Ca
carcinoma
- CIMP
CpG island methylator phenotype
- CRC
colorectal cancer
- CTNNB1
catenin beta 1
- KRAS
Kirsten rat sarcoma viral oncogene homolog
- HCM
hyperplastic colonic mucosa
- HP
hyperplastic polyp
- LOH
loss of heterozygosity
- MDE
mutation detection enhancement
- MGMT
O-6-methylguanine-DNA methyltransferase
- MLH1
mutL homolog 1
- MMR
mismatch repair
- MSI
microsatellite instability
- MSI-H
microsatellite instability-high
- MSI-L
microsatellite instability-low
- MSS
microsatellite stable
- MSH3
mutS homolog 3
- MSH6
mutS homolog 6
- NCM
normal colonic mucosa
- NRAS
neuroblastoma RAS viral (v-ras) oncogene homolog
- PCR
polymerase chain reaction
- PTT
protein truncation test
- SCa
serrated carcinoma
- SE
serrated
- SPP
serrated polyposis
- SPP-FHP/CRC
SPP associated with a family history of SPP and/or polyps/CRC (multiple or diagnosed at a young age) in first-degree relatives
- SSA
sessile serrated adenoma
- SSCP
single-strand conformational polymorphism
- TA
tubular adenoma
- TSA
traditional serrated adenoma
- TVA
tubulovillous adenoma
References
- 1.Snover DC, Ahnen DJ, Burt RW, Odze RD. Serrated polyps of the colon and rectum and serrated polyposis. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of Tumours of the Digestive System. IARC; Lyon: 2010. pp. 160–165. [Google Scholar]
- 2.Kalady MF, Jarrar A, Leach B, LaGuardia L, O'Malley M, Eng C, Church JM. Defining phenotypes and cancer risk in hyper-plastic polyposis syndrome. Dis Colon Rectum. 2011;54:164–170. doi: 10.1007/DCR.0b013e3181fd4c15. [DOI] [PubMed] [Google Scholar]
- 3.Rosty C, Parry S, Young JP. Serrated polyposis: an enigmatic model of colorectal cancer predisposition. Pathol Res Int. 2011;2011:157073. doi: 10.4061/2011/157073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snover DC, Jass JR, Fenoglio-Preiser C, Batts KP. Serrated polyps of the large intestine: a morphologic and molecular review of an evolving concept. Am J Clin Pathol. 2005;124:380–391. doi: 10.1309/V2EPTPLJRB3FGHJL. [DOI] [PubMed] [Google Scholar]
- 5.Aust DE, Baretton GB, Members of the Working Group GI-Pathology of the German Society of Pathology Serrated polyps of the colon and rectum (hyperplastic polyps, sessile serrated adenomas, traditional serrated adenomas, and mixed polyps)-proposal for diagnostic criteria. Virchows Arch. 2010;457:291–297. doi: 10.1007/s00428-010-0945-1. [DOI] [PubMed] [Google Scholar]
- 6.Rosty C, Hewett DG, Brown IS, Leggett BA, Whitehall VL. Serrated polyps of the large intestine: current understanding of diagnosis, pathogenesis, and clinical management. J Gastroenterol. 2013;48:287–302. doi: 10.1007/s00535-012-0720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young J, Jass JR. The case for a genetic predisposition to serrated neoplasia in the colorectum: hypothesis and review of the literature. Cancer Epidemiol Biomarkers Prev. 2006;15:1778–1784. doi: 10.1158/1055-9965.EPI-06-0164. [DOI] [PubMed] [Google Scholar]
- 8.Lindor NM. Hereditary colorectal cancer: MYH-associated polyposis and other newly identified disorders. Best Pract Res Clin Gastroenterol. 2009;23:75–87. doi: 10.1016/j.bpg.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Roberts A, Nancarrow D, Clendenning M, Buchanan DD, Jenkins MA, Duggan D, Taverna D, McKeone D, Walters R, Walsh MD, et al. Linkage to chromosome 2q32.2-q33.3 in familial serrated neoplasia (Jass syndrome) Fam Cancer. 2011;10:245–254. doi: 10.1007/s10689-010-9408-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–2100. doi: 10.1053/j.gastro.2009.12.066. [DOI] [PubMed] [Google Scholar]
- 11.Jass JR, Iino H, Ruszkiewicz A, Painter D, Solomon MJ, Koorey DJ, Cohn D, Furlong KL, Walsh MD, Palazzo J, et al. Neoplastic progression occurs through mutator pathways in hyperplastic polyposis of the colorectum. Gut. 2000;47:43–49. doi: 10.1136/gut.47.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jass JR, Young J, Leggett BA. Hyperplastic polyps and DNA microsatellite unstable cancers of the colorectum. Histopathology. 2000;37:295–301. doi: 10.1046/j.1365-2559.2000.01028.x. [DOI] [PubMed] [Google Scholar]
- 13.Snover DC. Update on the serrated pathway to colorectal carcinoma. Hum Pathol. 2011;42:1–10. doi: 10.1016/j.humpath.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Chan AO, Issa JP, Morris JS, Hamilton SR, Rashid A. Concordant CpG island methylation in hyperplastic polyposis. Am J Pathol. 2002;160:529–536. doi: 10.1016/S0002-9440(10)64872-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kambara T, Simms LA, Whitehall VL, Spring KJ, Wynter CV, Walsh MD, Barker MA, Arnold S, McGivern A, Matsubara N, et al. BRAF mutation is associated with DNA methylation in serrated polyps and cancers of the colorectum. Gut. 2004;53:1137–1144. doi: 10.1136/gut.2003.037671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weisenberger DJ, Siegmund KD, Campan M, Young J, Long TI, Faasse MA, Kang GH, Widschwendter M, Weener D, Buchanan D, et al. CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet. 2006;38:787–793. doi: 10.1038/ng1834. [DOI] [PubMed] [Google Scholar]
- 17.Chow E, Lipton L, Lynch E, D'Souza R, Aragona C, Hodgkin L, Brown G, Winship I, Barker M, Buchanan D, et al. Hyperplastic polyposis syndrome: phenotypic presentations and the role of MBD4 and MYH. Gastroenterology. 2006;131:30–39. doi: 10.1053/j.gastro.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 18.Yeoman A, Young J, Arnold J, Jass J, Parry S. Hyperplastic polyposis in the New Zealand population: a condition associated with increased colorectal cancer risk and European ancestry. N Z Med J. 2007;120:U2827. [PubMed] [Google Scholar]
- 19.Boparai KS, Mathus-Vliegen EM, Koornstra JJ, Nagengast FM, van Leerdam M, van Noesel CJ, Houben M, Cats A, van Hest LP, Fockens P, Dekker E. Increased colorectal cancer risk during follow-up in patients with hyperplastic polyposis syndrome: a multicentre cohort study. Gut. 2010;59:1094–1100. doi: 10.1136/gut.2009.185884. [DOI] [PubMed] [Google Scholar]
- 20.Minoo P, Baker K, Goswami R, Chong G, Foulkes WD, Ruszkiewicz AR, Barker M, Buchanan D, Young J, Jass JR. Extensive DNA methylation in normal colorectal mucosa in hyperplastic polyposis. Gut. 2006;55:1467–1474. doi: 10.1136/gut.2005.082859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wynter CV, Walsh MD, Higuchi T, Leggett BA, Young J, Jass JR. Methylation patterns define two types of hyperplastic polyp associated with colorectal cancer. Gut. 2004;53:573–580. doi: 10.1136/gut.2003.030841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carvajal-Carmona LG, Howarth KM, Lockett M, Polanco-Echeverry GM, Volikos E, Gorman M, Barclay E, Martin L, Jones AM, Saunders B, et al. Molecular classification and genetic pathways in hyperplastic polyposis syndrome. J Pathol. 2007;212:378–385. doi: 10.1002/path.2187. [DOI] [PubMed] [Google Scholar]
- 23.Guarinos C, Sánchez-Fortún C, Rodríguez-Soler M, Alenda C, Payá A, Jover R. Serrated polyposis syndrome: molecular, pathological and clinical aspects. World J Gastroenterol. 2012;18:2452–2461. doi: 10.3748/wjg.v18.i20.2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boparai KS, Reitsma JB, Lemmens V, van Os TA, Mathus-Vliegen EM, Koornstra JJ, Nagengast FM, van Hest LP, Keller JJ, Dekker E. Increased colorectal cancer risk in first-degree relatives of patients with hyperplastic polyposis syndrome. Gut. 2010;59:1222–1225. doi: 10.1136/gut.2009.200741. [DOI] [PubMed] [Google Scholar]
- 25.Win AK, Walters RJ, Buchanan DD, Jenkins MA, Sweet K, Frankel WL, de la Chapelle A, McKeone DM, Walsh MD, Clendenning M, et al. Cancer risks for relatives of patients with serrated polyposis. Am J Gastroenterol. 2012;107:770–778. doi: 10.1038/ajg.2012.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caetano AC, Ferreira H, Soares J, Ferreira A, Gonçalves R, Rolanda C. Phenotypic characterization and familial risk in hyperplastic polyposis syndrome. Scand J Gastroenterol. 2013;48:1166–1172. doi: 10.3109/00365521.2013.830329. [DOI] [PubMed] [Google Scholar]
- 27.Hazewinkel Y, Koornstra JJ, Boparai KS, van Os TA, Tytgat KM, van Eeden S, Fockens P, Dekker E. Yield of screening colonoscopy in first-degree relatives of patients with serrated polyposis syndrome. J Clin Gastroenterol. 2014 doi: 10.1097/MCG.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 28.Jasperson KW, Kanth P, Kirchhoff AC, Huismann D, Gammon A, Kohlmann W, Burt RW, Samadder NJ. Serrated polyposis: colonic phenotype, extracolonic features, and familial risk in a large cohort. Dis Colon Rectum. 2013;56:1211–1216. doi: 10.1097/DCR.0b013e3182a11cca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lanspa SJ, Ahnen DJ, Lynch HT. Serrated polyposis: the last (or only the latest?) frontier of familial polyposis? Am J Gastroenterol. 2012;107:779–781. doi: 10.1038/ajg.2012.62. [DOI] [PubMed] [Google Scholar]
- 30.Albuquerque C, Breukel C, van der Luijt R, Fidalgo P, Lage P, Slors FJ, Leitão CN, Fodde R, Smits R. The 'just-right' signaling model: APC somatic mutations are selected based on a specific level of activation of the beta-catenin signaling cascade. Hum Mol Genet. 2002;11:1549–1560. doi: 10.1093/hmg/11.13.1549. [DOI] [PubMed] [Google Scholar]
- 31.Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16:1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Francisco I, Albuquerque C, Lage P, Belo H, Vitoriano I, Filipe B, Claro I, Ferreira S, Rodrigues P, Chaves P, et al. Familial colorectal cancer type X syndrome: two distinct molecular entities? Fam Cancer. 2011;10:623–631. doi: 10.1007/s10689-011-9473-7. [DOI] [PubMed] [Google Scholar]
- 33.Albuquerque C, Baltazar C, Filipe B, Penha F, Pereira T, Smits R, Cravo M, Lage P, Fidalgo P, Claro I, et al. Colorectal cancers show distinct mutation spectra in members of the canonical WNT signaling pathway according to their anatomical location and type of genetic instability. Genes Chromosomes Cancer. 2010;49:746–759. doi: 10.1002/gcc.20786. [DOI] [PubMed] [Google Scholar]
- 34.Liu W, Dong X, Mai M, Seelan RS, Taniguchi K, Krishnadath KK, Halling KC, Cunningham JM, Boardman LA, Qian C, et al. Mutations in AXIN2 cause colorectal cancer with defective mismatch repair by activating beta-catenin/TCF signalling. Nat Genet. 2000;26:146–147. doi: 10.1038/79859. [DOI] [PubMed] [Google Scholar]
- 35.Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417:949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 36.Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN, Srivastava S. A National Cancer Institute: Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58:5248–5257. [PubMed] [Google Scholar]
- 37.Umar A. Lynch syndrome (HNPCC) and microsatellite instability. Dis Markers. 2004;20:179–180. doi: 10.1155/2004/486032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nygren AO, Ameziane N, Duarte HM, Vijzelaar RN, Waisfisz Q, Hess CJ, Schouten JP, Errami A. Methylation-specific MLPA (MS-MLPA): simultaneous detection of CpG methylation and copy number changes of up to 40 sequences. Nucleic Acids Res. 2005;33:e128. doi: 10.1093/nar/gni127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gylling A, Ridanpää M, Vierimaa O, Aittomäki K, Avela K, Kääriäinen H, Laivuori H, Pöyhönen M, Sallinen SL, Wallgren-Pettersson C, et al. Large genomic rearrangements and germline epimutations in Lynch syndrome. Int J Cancer. 2009;124:2333–2340. doi: 10.1002/ijc.24230. [DOI] [PubMed] [Google Scholar]
- 40.Yamada A, Minamiguchi S, Sakai Y, Horimatsu T, Muto M, Chiba T, Boland CR, Goel A. Colorectal advanced neoplasms occur through dual carcinogenesis pathways in individuals with coexisting serrated polyps. PLoS One. 2014;9:e98059. doi: 10.1371/journal.pone.0098059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Filipe B, Baltazar C, Albuquerque C, Fragoso S, Lage P, Vitoriano I, Mão de Ferro S, Claro I, Rodrigues P, Fidalgo P, et al. APC or MUTYH mutations account for the majority of clinically well-characterized families with FAP and AFAP phenotype and patients with more than 30 adenomas. Clin Genet. 2009;76:242–255. doi: 10.1111/j.1399-0004.2009.01241.x. [DOI] [PubMed] [Google Scholar]
- 42.Albuquerque C, Bakker ER, van Veelen W, Smits R. Colorectal cancers choosing sides. Biochim Biophys Acta. 2011;1816:219–231. doi: 10.1016/j.bbcan.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 43.Christie M, Jorissen RN, Mouradov D, Sakthianandeswaren A, Li S, Day F, Tsui C, Lipton L, Desai J, Jones IT, et al. Different APC genotypes in proximal and distal sporadic colorectal cancers suggest distinct WNT/β-catenin signalling thresholds for tumourigenesis. Oncogene. 2013;32:4675–4682. doi: 10.1038/onc.2012.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leedham SJ, Rodenas-Cuadrado P, Howarth K, Lewis A, Mallappa S, Segditsas S, Davis H, Jeffery R, Rodriguez-Justo M, Keshav S, et al. A basal gradient of Wnt and stem-cell number influences regional tumour distribution in human and mouse intestinal tracts. Gut. 2013;62:83–93. doi: 10.1136/gutjnl-2011-301601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Plaschke J, Preussler M, Ziegler A, Schackert HK. Aberrant protein expression and frequent allelic loss of MSH3 in colorectal cancer with low-level microsatellite instability. Int J Colorectal Dis. 2012;27:911–919. doi: 10.1007/s00384-011-1408-0. [DOI] [PubMed] [Google Scholar]
- 46.Hatch SB, Lightfoot HM, Jr, Garwacki CP, Moore DT, Calvo BF, Woosley JT, Sciarrotta J, Funkhouser WK, Farber RA. Microsatellite instability testing in colorectal carcinoma: choice of markers affects sensitivity of detection of mismatch repair-deficient tumors. Clin Cancer Res. 2005;11:2180–2187. doi: 10.1158/1078-0432.CCR-04-0234. [DOI] [PubMed] [Google Scholar]
- 47.Christmann M, Kaina B. Nuclear translocation of mismatch repair proteins MSH2 and MSH6 as a response of cells to alkylating agents. J Biol Chem. 2000;275:36256–36262. doi: 10.1074/jbc.M005377200. [DOI] [PubMed] [Google Scholar]
- 48.Sohn KJ, Choi M, Song J, Chan S, Medline A, Gallinger S, Kim YI. Msh2 deficiency enhances somatic Apc and p53 mutations in Apc+/−Msh2−/− mice. Carcinogenesis. 2003;24:217–224. doi: 10.1093/carcin/24.2.217. [DOI] [PubMed] [Google Scholar]
- 49.Oliveira C, Westra JL, Arango D, Ollikainen M, Domingo E, Ferreira A, Velho S, Niessen R, Lagerstedt K, Alhopuro P, et al. Distinct patterns of KRAS mutations in colorectal carcinomas according to germline mismatch repair defects and hMLH1 methylation status. Hum Mol Genet. 2004;13:2303–2311. doi: 10.1093/hmg/ddh238. [DOI] [PubMed] [Google Scholar]
- 50.Mark SC, Sandercock LE, Luchman HA, Baross A, Edelmann W, Jirik FR. Elevated mutant frequencies and predominance of G:C to A:T transition mutations in Msh6(−/−) small intestinal epithelium. Oncogene. 2002;21:7126–7130. doi: 10.1038/sj.onc.1205861. [DOI] [PubMed] [Google Scholar]
- 51.Wada R, Yamaguchi T, Tadokoro K. Colonic Paneth cell metaplasia is pre-neoplastic condition of colonic cancer or not? J Carcinog. 2005;4:5. doi: 10.1186/1477-3163-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wada R. Proposal of a new hypothesis on the development of colorectal epithelial neoplasia:nonspecific inflammation - colorectal Paneth cell metaplasia - colorectal epithelial neoplasia. Digestion. 2009;79(Suppl 1):9–12. doi: 10.1159/000167860. [DOI] [PubMed] [Google Scholar]
- 53.Andreu P, Peignon G, Slomianny C, Taketo MM, Colnot S, Robine S, Lamarque D, Laurent-Puig P, Perret C, Romagnolo B. A genetic study of the role of the Wnt/beta-catenin signalling in Paneth cell differentiation. Dev Biol. 2008;324:288–296. doi: 10.1016/j.ydbio.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 54.Sada M, Mitomi H, Igarashi M, Katsumata T, Saigenji K, Okayasu I. Cell kinetics, p53 and bcl-2 expression, and c-Ki-ras mutations in flat-elevated tubulovillous adenomas and adenocarcinomas of the colorectum: comparison with polypoid lesions. Scand J Gastroenterol. 1999;34:798–807. doi: 10.1080/003655299750025732. [DOI] [PubMed] [Google Scholar]
- 55.Maltzman T, Knoll K, Martinez ME, Byers T, Stevens BR, Marshall JR, Reid ME, Einspahr J, Hart N, Bhattacharyya AK, et al. Ki-ras proto-oncogene mutations in sporadic colorectal adenomas: relationship to histologic and clinical characteristics. Gastroenterology. 2001;121:302–309. doi: 10.1053/gast.2001.26278. [DOI] [PubMed] [Google Scholar]
- 56.Jass JR, Baker K, Zlobec I, Higuchi T, Barker M, Buchanan D, Young J. Advanced colorectal polyps with the molecular and morphological features of serrated polyps and adenomas: concept of a 'fusion' pathway to colorectal cancer. Histopathology. 2006;49:121–131. doi: 10.1111/j.1365-2559.2006.02466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.García-Solano J, Conesa-Zamora P, Carbonell P, Trujillo-Santos J, Torres-Moreno DD, Pagán-Gómez I, Rodríguez-Braun E, Pérez-Guillermo M. Colorectal serrated adenocarcinoma shows a different profile of oncogene mutations, MSI status and DNA repair protein expression compared to conventional and sporadic MSI-H carcinomas. Int J Cancer. 2012;131:1790–1799. doi: 10.1002/ijc.27454. [DOI] [PubMed] [Google Scholar]
- 58.Feng Y, Bommer GT, Zhao J, Green M, Sands E, Zhai Y, Brown K, Burberry A, Cho KR, Fearon ER. Mutant KRAS promotes hyperplasia and alters differentiation in the colon epithelium but does not expand the presumptive stem cell pool. Gastroenterology. 2011;141:1003–1013. e1–10. doi: 10.1053/j.gastro.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carragher LA, Snell KR, Giblett SM, Aldridge VS, Patel B, Cook SJ, Winton DJ, Marais R, Pritchard CA. V600EBraf induces gastrointestinal crypt senescence and promotes tumour progression through enhanced CpG methylation of p16INK4a. EMBO Mol Med. 2010;2:458–471. doi: 10.1002/emmm.201000099. [DOI] [PMC free article] [PubMed] [Google Scholar]