ABSTRACT
Background: Poorly Differentiated Thyroid Carcinoma (PDTC), especially advanced PDTC, is an aggressive disease and displays a much poorer prognosis compared with well differentiated thyroid carcinoma. Surgery is the recommended treatment in the early stage of PDTC, however, no effective treatment modalities are currently available for advanced PDTCMethods: Two advanced PDTC patients with no radioiodine uptake adopted a cytotoxic chemotherapy with liposomal doxorubicin (35 mg/m2, day 1) plus cisplatin (75 mg/m2, day1–3) every 3 weeks. Computer tomography (CT) was performed after 6 cycles (case 1) or 5 cycles (case 2) of chemotherapyResults: Our patients achieved remarkable response with one a Complete Remission (CR) and the other a very good Partial Remission (PR)Conclusion: Our findings indicate that liposomal doxorubicin-based chemotherapy regimens might produce response in PDTC patients, and improve their overall survival and quality of life. Hence we believe this result is very important for oncologists in treating PDTC.
KEYWORDS: Poorly differentiated thyroid carcinoma, chemotherapy, liposomal doxorubicin, cis-platinum, complete remission, partial remission
Abbreviations
- PDTC
Poorly differentiated thyroid carcinoma
- CR
Complete remission
- PR
Partial remission
- HE
Hematoxylin-eosin
- TIF1
Transcription factor 1
- HBME-1
Human bone marrow endothelial cell-1
- CEA
Carcinoembryonic antigen
- PET-CT
Positron emission tomography computed tomography
- AD
Liposomal doxorubicin and cis-platinum
- RECIST
Response evaluation criteria in solid tumors
- WDTC
Well-differentiated thyroid carcinoma
- GEMOX
Gemcitabine and oxaliplatin
- MDR
Multidrug resistance
- ABC transporter
ATP-binding cassette transporter
- P-gp
P-glycoprotein
- MRPs
MDR-associated proteins
- BCRPM
Breast cancer resistance protein
- ABCG2
ATP-binding cassette transporter G2
Background
The term of Poorly Differentiated Thyroid Carcinoma (PDTC) was coined by Sakamoto and Carcangiu in 1980, however, the pathologic diagnostic criteria was not unified until the Turin Meeting in Italy in 2006.1-2 PDTC is a rare disease, accounting for 4%-7% of all cases of thyroid cancer. In contrast to the well-differentiated thyroid cancer types, PDTC is more aggressive and often displays more extensive local invasion and lymphatic metastasis, and distant metastasis in lung and bone.3
No effective treatment modalities are currently available. Surgery is the recommended treatment in the early stage. Total thyroidectomy plus cervix lymph node dissection is warranted if the cancer remains confined locally. Around 15% of the PDTC patients probably have BRAF mutation, which leads to reduction in iodine uptake by thyroid cancer cells, and the effect of I131 is therefore limited. In addition, postoperative irradiation, radiotherapy, chemotherapy or multimodality treatment doesn’t improve survival in PDTC.
Here, we report the history of two PDTC patients with no radioiodine uptake who displayed a remarkable response to cytotoxic chemotherapy with liposomal doxorubicin plus cisplatin. We then discuss the potential role of liposomal doxorubicin plus cisplatin for PDTC patients.
Case report
Case1
In May 2013, a 42-year-old male presented with a lump in the right thyroid gland. He then had a “total thyroidectomy + modified neck dissection” surgery for the right thyroid gland and the postoperative pathology showed it to be PDTC (Fig. 1) (immunohistochemically, thyroglobulin, thyroid transcription factor 1 (TTF-1), cytokeratin 19 and human bone marrow endothelial cell markers 1 (HBME-1) are positive; calcitonin, chromogranin A, synaptophysin, Galectin-3, carcinoembryonic antigen (CEA) and CD56 are negative) with 9 positive lymph nodes in region VI. He did not receive I131 therapy or local radiotherapy after surgery. In January, 2014 (9 months from diagnosis), positron emission tomography-CT (PET-CT) indicated recurrences with swollen lymph nodes at the deep cervical space, the right side of trachea and arcus aortae, and metastasis in both lungs. The patient had no treatment until he had 30I125 seeds implanted in the cervix lump (0.8 mCi) due to cervix lymphadenovarix along with chest distress and tachypnea in April 2014. After I125 therapy, the cervix lump shrunk obviously. However, 2 months later, a type-B ultrasound and CT scan showed there to be many enlarged lymph nodes in both lungs and a shadow in thoracic vertebrae indicating metastasis. He then underwent a palliative operation to the lymph gland in the right neck (July 2014), I131 treatment with a dose of 100Ci (August 2014) and biotherapy (December, 2014), however, these treatments produced limited response. A type-B ultrasound and CT scan both showed enlarged lymph nodes in the right neck, clavicle mediastinum, hilum of right lung, and a cancer embolus (1.2 cmX1.0 cm) in the right internal jugular venous (Fig. 2). From December 30th to May 5th 2015, he received a liposomal doxorubicin and cis-platinum (AD) regimen (liposomal doxorubicin 35 mg/m2 day1, cis-platinum 75 mg/m2 day1–3) chemotherapy every 3 weeks. After 6 cycles of chemotherapy, the first CT evaluation revealed a remarkable reduction in the extension of the disease that reached a very good PR (90% according to the response evaluation criteria in solid tumors (RECIST)) (Fig. 2).
Figure 1.
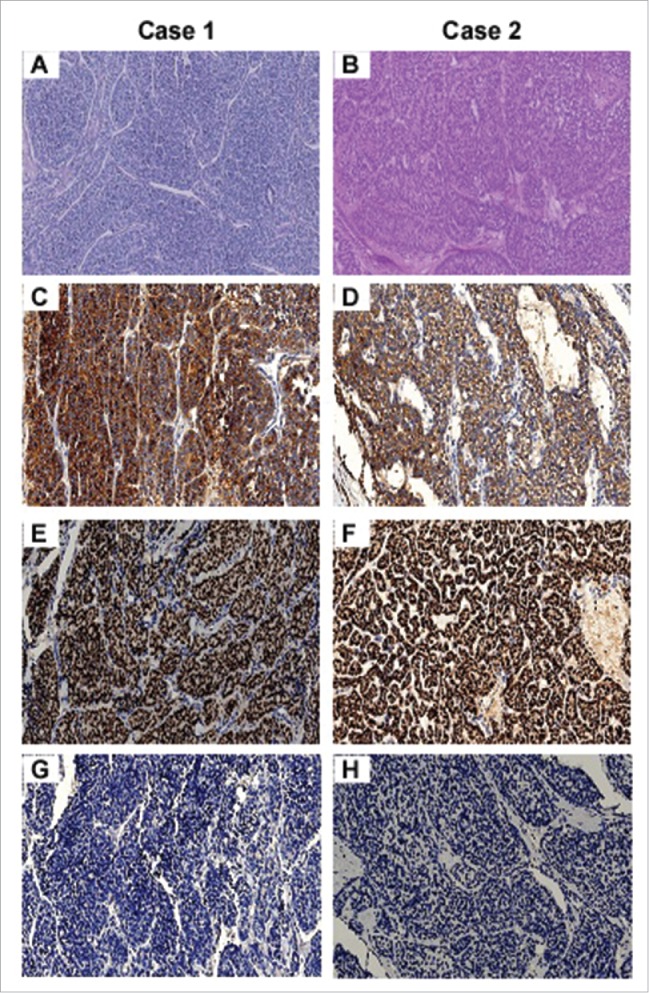
Histopathological features of two cases of PDTC. Tumor showed typical PDTC growth patterns of insular and trabecular growth in both case 1 (A) and case 2 (B) (hematoxylin-eosin (HE) stain). Immunohistochemical staining for thyroglobulin and thyroid transcription factor 1 (TTF1) is robust in both case1 (C and E) and case 2 (D and F), while staining of calcitonin is absent in both case 1 (G) and 2 (H). All images are 200× magnification.
Figure 2.
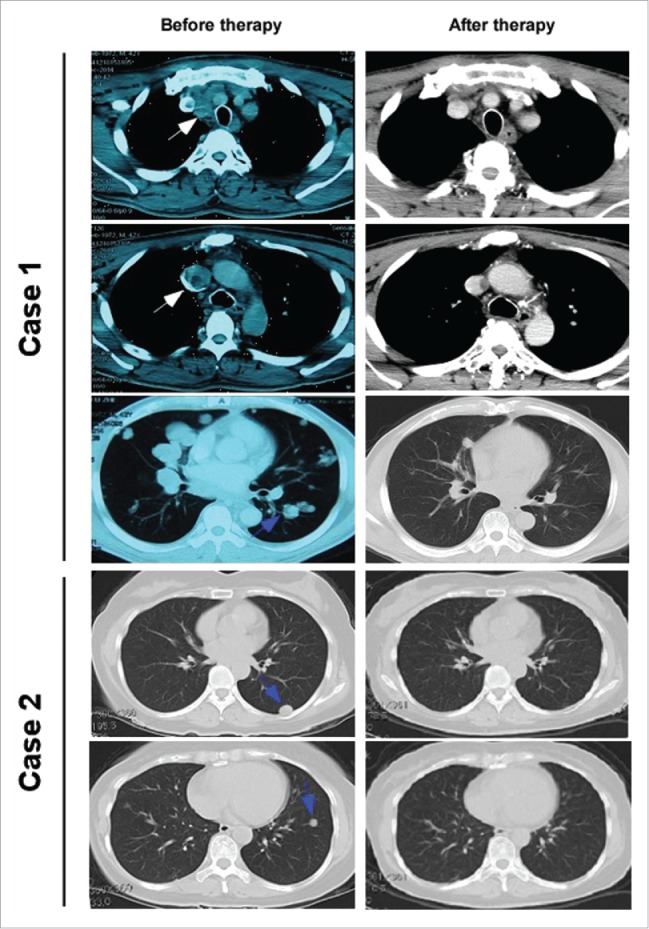
Chest CT scan images taken prior and subsequent to AD regimen therapy. Enhanced CT of chest with case 1 showed a remarkable reduction in the size of metastatic lymph node located beside trachea and esophagus, and an obvious decrease of cancer embolus (1.2 cm×1.0 cm) in right internal jugular venous (white arrows). Lung window of CT of both case 1and case 2 reveals that a very good response in metastatic lesions of both lungs (blue arrows).
Case 2
In February 2013, a 57-year-old female presented with nodules in the neck, and a type-B ultrasound determined a nodule was located in left thyroid. Then on February 28th 2013, she had a total thyroidectomy and postoperative pathology indicated it was a left PDTC with a size of 2.8 cmX2.5 cmX2 cm, which had an infiltrated tumor capsule and blood vessels (Fig 1). Immunohistochemical analysis showed that ki67, cytokeratin 19 and TTF1 were positive, P53, chromogranin A, synaptophysin, CD56, thyroglobulin, calcitonin, cytokeratin 7 and CD31 were negative (Fig. 2). After surgery she received tumor bed and intensity modulated radiation therapy in the neck with planning target volume 200cGyX30 times. And she came to the Department of Radiotherapy in Zhejiang Cancer hospital for treatment due to metastasis in both lungs for 1 week. Chest CT revaluation showed many space-occupying lesions in both lungs indicating metastasis in both lungs after the thyroid carcinoma surgery. From November 17th to February 11th 2014, she underwent 5 cycles of AD regimen (liposomal doxorubicin 35 mg/m2 day1, cis-platinum 75 mg/m2 day1–3). After 2 cycles, the CT evaluation was PR, and after 4 cycles, the CT evaluation was CR (Fig. 2). After 5 cycles of AD regimen, she suffered myelosuppression (grade 4) and foot syndrome (grade 3). She was showed improvement after treatment and she did not receive the 6th chemotherapy treatment. The patient is in good condition and has maintained CR for 7 months following the last treatment.
Discussion
PDTC is a rare disease and its biological behaviors are between well-differentiated (WDTC) and undifferentiated (anaplastic) carcinomas. The diagnosis criteria of PDTC includes a solid/trabecular/insular pattern of growth and at least one of the following features: nucleus distortion, mitotic activity ≥3×10 high power field, and tumor necrosis. It often reflects as an external lump on the thyroid gland and local invasion, and the course of the disease is invasive and will often metastasize into lung and bone. And 5-year and 10-year survival rates are 50% and 34%, respectively, which are much worse than those of WDTC (95% and 86%, respectively).3
Patients exhibiting well-differentiated thyroid carcinoma with high iodine uptake can often be cured after surgery followed by radioiodine therapy, while PDTC usually shows poor or no radioiodine uptake, so the effect of I131 is not satisfactory.4 Radiotherapy is only for local advanced patients and produces limited effect. Recently, advances in the understanding of the biology of PDTC, have enabled the identification of various important molecular changes, such as in BRAF, TP53 and RAS genes and other mutations, which provides the basis for developing targeted therapies. Tyrosine kinase inhibitors, such as vandetanib, sunitinib and motesanib, for PDTC are under clinical trial, but the effect is controversial and more individualized.5-7 It is still a conundrum for doctors to treat advanced PDTC patients with no available effective regimens.
In the past, chemotherapy was thought to have limited effect in thyroid cancer patients who have iodine tolerance. Adriamycin is the most common drug in thyroid gland chemotherapy, and its effectiveness in single agent or combination chemotherapy is 0–20%.8-9 Recently, paclitaxel was found to produce some response in patients who were in later advanced thyroid follicular carcinoma into differentiated thyroid carcinoma. Span reported 6 cases of metastatic iodine tolerance of patients with differentiated thyroid carcinoma adopted gemcitabine and oxaliplatin (GEMOX) regimen chemotherapy, with 2 cases PR, 1 case CR and the other 3 case stable disease.10 However, there has been very limited research into the chemotherapy of PDTC.
Doxorubicin was one of the first drugs encapsulated within liposomes and liposomal doxorubicin (Doxyl/ Caelyx) is actually approved for the treatment of metastatic and drug-resistant breast and ovary cancers.11 However, liposomal doxorubicin is rarely used for PDTC, and there is only one case report in which single agent liposomal doxorubicin was utilized in an anaplastic thyroid carcinoma patient with an encouraging response (70% according to RECIST).12 Therefore, it is also believed to be an effective drug for PDTC. In our case, a cell cycle-independent drug, cisplatin, was combined with the liposomal doxorubicin (cycle-dependent), which was thought to be more active. As a result, there were remarkable response in the two cases of PDTC with such regimen. It might indicate the following mechanism: chemotherapy alone has been largely unsuccessful for PDTC, possibly related to intrinsic or acquired multidrug resistance (MDR).8,13,14 It is believed that ATP-binding cassette transporters (ABC transporters), such as P-glycoprotein (P-gp), MDR-associated proteins (MRPs), play an important role in chemotherapy failure in PDTC. However, liposomal doxorubicin has greater drug delivery within the tumor core due to the enhanced permeability and retention effect.15 Liposomal drugs seem also less susceptible than free drugs to the efflux activity by ABC transporters, such as P-gp, MRPs and breast cancer resistance protein/ ATP-binding cassette transporter G2 (BCRP/ABCG2). Liposomal drugs ensure a more prolonged release of the drug within tumor cells, since they are less potent inducers of P-gp than free drugs,8 or directly interfere with P-gp activity.16 Therefore, it is possible that the liposomal doxorubicin might be an effective drug which can overcome the efflux transporters in PDTC. Further studies using this drug, including mechanistic investigation, need to be conducted in the future.
Summary
Our findings indicate that liposomal doxorubicin based chemotherapy regimens might be effective for advanced PDTC, which may improve the patients' prognosis and quality of life. In addition, these results also suggest that the role of chemotherapy should be reconsidered in PDTC treatment, especially advanced PDTC.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgment
Our sincere gratitude to the patient and his family for their permission to use the pictures and slides for this paper.
Reference
- 1.Sakamoto A, Kasai N, Sugano H. Poorly differentiated carcinoma of the thyroid. A clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer 1983; 52:1849-55; PMID:6313176; http://dx.doi.org/ [DOI] [PubMed] [Google Scholar]
- 2.Volante M, Collini P, Nikiforov YE, Sakamoto A, Kakudo K, Katoh R, Lloyd RV, LiVolsi VA, Papotti M, Sobrinho-Simoes M, et al.. Poorly differentiated thyroid carcinoma: the Turin proposal for the use of uniform diagnostic criteria and an algorithmic diagnostic approach. Am J Surg Pathol 2007; 31:1256-64; PMID:17667551; http://dx.doi.org/ 10.1097/PAS.0b013e3180309e6a [DOI] [PubMed] [Google Scholar]
- 3.Hannallah J, Rose J, Guerrero MA. Comprehensive literature review: recent advances in diagnosing and managing patients with poorly differentiated thyroid carcinoma. Int J Endocrinol 2013; 2013:317487; PMID:23476646; 10.1155/2013/317487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fat I, Kulaga M, Dodis R, Carling T, Theoharis C, Rennert NJ. Insular variant of poorly differentiated thyroid carcinoma. Endocr Pract 2011; 17:115-21; PMID:20634178; http://dx.doi.org/ 10.4158/EP09368.RA [DOI] [PubMed] [Google Scholar]
- 5.Soares P, Lima J, Preto A, Castro P, Vinagre J, Celestino R, Couto JP, Prazeres H, Eloy C, Máximo V, et al.. Genetic alterations in poorly differentiated and undifferentiated thyroid carcinomas. Curr Genomics 2011; 12:609-17; PMID:22654560; http://dx.doi.org/ 10.2174/138920211798120853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta-Abramson V, Troxel AB, Nellore A, Puttaswamy K, Redlinger M, Ransone K, Mandel SJ, Flaherty KT, Loevner LA, O'Dwyer PJ, et al.. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008; 26:4714-9; PMID:18541894; http://dx.doi.org/ 10.1200/JCO.2008.16.3279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carr LL, Mankoff DA, Goulart BH, Eaton K D, Capell PT, Kell EM, Bauman JE, Martins RG. Phase II study of daily sunitinib in FDG-PET-positive, iodine-refractory differentiated thyroid cancer and metastatic medullary carcinoma of the thyroid with functional imaging correlation. Clin Cancer Res 2010; 16:5260-8; PMID:20847059; http://dx.doi.org/ 10.1158/1078-0432.CCR-10-0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shimaoka K, Schoenfeld DA, DeWys WD, Creech RH, DeConti R. A randomized trial of doxorubicin versus doxorubicin plus cisplatin in patients with advanced thyroid carcinoma. Cancer 1985; 56:2155-60; PMID:3902203; http://dx.doi.org/ [DOI] [PubMed] [Google Scholar]
- 9.Williams SD, Birch R, Einhorn LH. Phase II evaluation of doxorubicin plus cisplatin in advanced thyroid cancer: a Southeastern Cancer Study Group Trial. Cancer Treat Rep 1986; 70:405-7; PMID:3955552 [PubMed] [Google Scholar]
- 10.Spano JP, Vano Y, Vignot S, De La Motte Rouge T, Hassani L, Mouawad R, Menegaux F, Khayat D, Leenhardt L. GEMOX regimen in the treatment of metastatic differentiated refractory thyroid carcinoma. Med Oncol 2012; 29:1421-8; PMID:21947747; http://dx.doi.org/ 10.1007/s12032-011-0070-2 [DOI] [PubMed] [Google Scholar]
- 11.Markman M. Pegylated liposomal doxorubicin in the treatment of cancers of the breast and ovary. Expert Opin Pharmacother 2006; 7:1469-74; PMID:16859430; http://dx.doi.org/ 10.1517/14656566.7.11.1469 [DOI] [PubMed] [Google Scholar]
- 12.Moscetti L, Padalino D, Capomolla E, Nelli F, Pollera CF. A partial response in anaplastic carcinoma of the thyroid with liposomal doxorubicin. J Exp Clin Cancer Res 2005; 24:151-4; PMID:15943045 [PubMed] [Google Scholar]
- 13.Gottlieb JA, Hill CS Jr. Chemotherapy of thyroid cancer with adriamycin. Experience with 30 patients. N Engl J Med 1974; 290:193-7; PMID:4808917; http://dx.doi.org/ 10.1056/NEJM197401242900404 [DOI] [PubMed] [Google Scholar]
- 14.Robbins J, Merino MJ, Boice JD Jr, Ron E, Ain KB, Alexander HR, Norton JA, Reynolds J. Thyroid cancer: a lethal endocrine neoplasm. Ann Intern Med 1991; 115:133-47; PMID:2058861; http://dx.doi.org/ 10.7326/0003-4819-115-2-133 [DOI] [PubMed] [Google Scholar]
- 15.Jabr-Milane LS, van Vlerken LE, Yadav S, Amiji MM. Multi-functional nanocarriers to overcome tumor drug resistance. Cancer Treat Rev 2008; 34:592-602; PMID:18538481; http://dx.doi.org/ 10.1016/j.ctrv.2008.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kopecka J, Salzano G, Campia I, Lusa S, Ghigo D, De Rosa G, Riganti C. Insights in the chemical components of liposomes responsible for P-glycoprotein inhibition. Nanomedicine 2014; 10:77-87; PMID:23850894; 10.1016/j.nano.2013.06.013 [DOI] [PubMed] [Google Scholar]


