Abstract
Objective
Patients with severe sepsis have high mortality that is improved by timely, often expensive, treatments. Patients without insurance are more likely to delay seeking care; they may also receive less intense care.
Design
We performed a retrospective analysis of administrative database—Healthcare Costs and Utilization Project’s Nationwide Inpatient Sample—to test whether mortality is more likely among uninsured patients hospitalized for severe sepsis.
Patients
None.
Interventions
We used International Classification of Diseases—9th Revision, Clinical Modification, codes indicating sepsis and organ system failure to identify hospitalizations for severe sepsis among patients aged 18–64 between 2000 and 2008. We excluded patients with end-stage renal disease or solid organ transplants because very few are uninsured. We performed multivariate logistic regression modeling to examine the association of insurance status and in-hospital mortality, adjusted for patient and hospital characteristics. We performed subgroup analysis to examine whether the impact of insurance status varied by geographical region; by patient age, sex, or race; or by hospital characteristics such as teaching status, size, or ownership. We used similar methods to examine the impact of insurance status on the use of certain procedures, length of stay, and discharge destination.
Measurements and Main Results
There were 1,600,269 discharges with severe sepsis from 2000 through 2008 in the age group 18–64 years. Uninsured people, who accounted for 7.5% of admissions with severe sepsis, had higher adjusted odds of mortality (odds ratio, 1.43; 95% CI, 1.37–1.47) than privately insured people. The higher mortality in uninsured was present in all subgroups and was similar in each year from 2000 to 2008. After adjustment, uninsured individuals had a slightly shorter length of stay than insured people and were less likely to receive five of the six interventions we examined. They were also less likely to be discharged to skilled nursing facilities or with home healthcare after discharge.
Conclusions
Uninsured are more likely to die following admission for severe sepsis than patients with insurance, even after adjusting for potential confounders. This was not due to a hospital effect or demographic or clinical factors available in our administrative database. Further research should examine the mechanisms that lead to this association.
Keywords: administrative data, insurance status, mortality, outcomes, severe sepsis, uninsured
Many Americans lack health insurance. In 2008, the U.S. Census Bureau estimated that 44.7 million people (14.9% of the U.S. population) were without health insurance for at least part of the year (1). Although the Affordable Care Act will decrease the number of uninsured Americans, the Congressional Budget Office estimates that 20 million residents, including 14 million U.S. citizens, will remain without insurance when it is fully implemented in 2016. Previous work has demonstrated that a lack of health insurance impedes access to healthcare services and adversely affects outcomes in acute medical conditions (2–7).
Severe sepsis is a frequent and potentially lethal disease that requires early and aggressive management. The annual number of hospitalizations for severe sepsis rose steadily through the first years of the 21st century, reaching 343 per 100,000 population in 2007 (8). Furthermore, despite improvements in case fatality rates, over 27% of patients admitted with sepsis die during their hospital stay. Other investigators have found that uninsured individuals have worse outcomes of trauma, cancer, and acute coronary syndrome than their insured counterparts (2–4, 9). It is unclear whether this is because uninsured individuals are disproportionately treated in hospitals that have worse outcomes, because they have worse outcomes compared with insured patients treated in the same hospital, or both. A recent study found that uninsured adults admitted to the ICUs in Pennsylvania during 2005 and 2006 received fewer procedures and had higher 30-day mortality than clinically similar insured patients. This study did not address patients with severe sepsis in particular (10).
Given the increasing frequency of severe sepsis and the expanding number of evidence-based treatment options, many of which are expensive, it is important to determine how and to what degree insurance status affects the treatment and outcomes of patients admitted with this life-threatening condition. We therefore carried out the present investigation to describe the relationship of insurance status to treatment, inhospital mortality, and discharge destination of patients with severe sepsis. We used a large nationally representative administrative database to enhance the robustness of our results and determine whether insurance effects varied by hospital or patient characteristics.
METHODS
Data Source
We used the Nationwide Inpatient Sample (NIS), the largest all-payer inpatient care database, publicly available in the United States. This administrative dataset was created by the Agency for Healthcare Research and Quality as part of the Healthcare Cost and Utilization Project and contains data on 5–8 million hospital stays from about 1,000 hospitals sampled to approximate a 20% stratified sample of U.S. community hospitals but excludes federal hospitals. Each hospitalization is treated as an individual entry in the database and includes International Classification of Diseases—9th Clinical Modification (ICD-9-CM), codes for the principal diagnosis and up to 14 secondary diagnoses and 15 procedures associated with that stay. NIS includes information on all hospitalizations at participating hospitals, regardless of payer, including private insurance and the uninsured. NIS includes appropriate weights to allow the production of national estimates (11). We used data from the years 2000 to 2008 for this study. Because we used a publicly available dataset with no patient identifiers, this study was examined and found exempt from formal review by the Institutional Review Board of the Medical College of Wisconsin.
Study Population
We used ICD-9-CM codes to identify patients 18 to 64 years old who were discharged with severe sepsis between 2000 and 2008. Based on a previously used and validated approach, we defined severe sepsis as either an ICD-9-CM code 995.92 (systemic inflammatory response syndrome due to infectious process with organ failure) or an ICD-9-CM code for septicemia, bacteremia, or fungemia and at least one organ failure code (12, 13). We provide specific codes in Appendices 1 and 2 (Supplemental Digital Content 1, http://links.lww.com/CCM/A756). We excluded patients aged 65 and over from the study because Medicare was the primary payer in about 90% of them. Similarly, patients with end-stage renal disease and organ transplants were excluded because they have a worse prognosis with severe sepsis (14, 15) and are almost entirely covered by Medicare; very few (< 1%) are uninsured. We also excluded admissions that lacked data regarding gender, age, or primary payer.
Definition of Variables
We used NIS variables to identify primary payer and patient age, gender, and race and median household income for the patient’s zip code of residence. NIS provides expected primary payer in six categories: 1) Medicare, 2) Medicaid, 3) private including Health Maintenance Organization, 4) self pay, 5) no charge, and 6) others. We combined the latter two groups as “others” and refer to self pay as “uninsured.” We divided age into five groups—18–24, 25–34, 35–44, 45–54, and 55–64—but also considered finer categories and treatment of age as a continuous variable. These did not change our results so we present only these categories. NIS provides six race categories: 1) white, 2) black, 3) Hispanic, 4) Asian or Pacific Islander, 5) Native American, and 6) others. Information about race is omitted from 20% to 25% of records in any particular year. We categorized patients without race information as “unknown” race. NIS provides information on the median household income for the patient’s zip code. We treated this as a four-level categorical variable across all years.
We identified comorbid conditions based on discharge diagnosis and procedure codes using the method of Charlson-Deyo (16). We entered each of the 17 conditions identified by this method as independent variables in our regression model since the Charlson-Deyo index that summarizes the impact of these comorbidities on mortality was not derived in sepsis patients. In analyses not presented in this article, we confirmed that the index did not predict mortality as well as the individual factors, but we use it as a summary of comorbidity. We also identified risk factors not identified by the Charlson-Deyo method if prior literature indicated that they were associated with sepsis mortality (Appendix 3, Supplemental Digital Content 1, http://links.lww.com/CCM/A756). We categorized admission source as emergency department, transfer from another hospital, transfer from another healthcare facility (e.g., nursing home), or others.
We used the three hospital ownership categories provided by NIS: 1) government—nonfederal, 2) private—nonprofit, and 3) private—investor-owned. We also used NIS classifications for a hospital’s geographic region (Northeast, Midwest, South, and West), teaching status, and size.
Outcomes
Our primary outcome of interest was in-hospital mortality, which is recorded as such in the NIS database. Secondary outcomes included receipt of treatments thought to reflect intensity of treatment of severe sepsis, length of stay (LOS), and discharge disposition. We used ICD-9-CM codes to identify patients who underwent mechanical ventilation, received blood transfusions, had placement of central venous catheters, had placement of pulmonary artery flotation catheters, had tracheostomy, had total parenteral nutrition, or had new dialysis (Appendix 3, Supplemental Digital Content 1, http://links.lww.com/CCM/A756). We grouped discharge disposition as routine, transfers to other acute care hospitals, and transfers to other healthcare facilities (e.g., skilled nursing facilities, intermediate care, inpatient rehabilitation, psychiatric hospitals, or inpatient hospice), home healthcare, and others (including against medical advice, unknown, and missing).
Statistical Analysis
We performed all statistical analyses using STATA IC 11.0 (StataCorp, College Station, TX). We used the strata and weights with appropriate survey commands to generate national estimates. For our descriptive analyses, we used analysis of variance to determine overall significance of differences among the insurance categories. We then made pairwise comparisons using Student t test for continuous variables and Pearson’s chi-square test for categorical variables. Statistical significance was defined as a p value of less than 0.05.
We constructed several multivariable models to assess the association of insurance status with in-hospital mortality. We used single predictor logistic regression to identify significant associations between putative risk factors and mortality. Variables found significant at p value less than 0.10 were candidates for inclusion in our primary model. We checked variables used in the final model for multicollinearity using tolerance and variance inflation factor; these were always very close to unity, suggesting minimal collinearity.
We then used a propensity score approach to further adjust for differences in which patients are uninsured. We used a logistic regression model to calculate the likelihood that a person would be uninsured. This model included factors that might affect the likelihood of being uninsured, regardless of their individual statistical significance. Thus, we included study year, hospital location (urban vs rural), patient age, gender, race, and median household income of the patient’s zip code of residence. We multiplied the propensity score by 100 and used the integral value of this as a measure of propensity to be uninsured. This variable was then added to the previously developed model. Our results were similar if we used propensity score quintiles.
To determine whether the observed differences in mortality risk reflected a hospital effect—that is, patients without insurance being more likely to be treated in hospitals with higher risk-adjusted mortality—we added a random effect for each individual hospital (NIS variable name—HOSPID)to the previous final model. Strata were included as a fixed effect, and survey weights were not used for this analysis as the appropriate methods of incorporation of survey weights into random effects models is controversial, and the weights in NIS have small variability, so inference with NIS data is not sensitive to their omission.
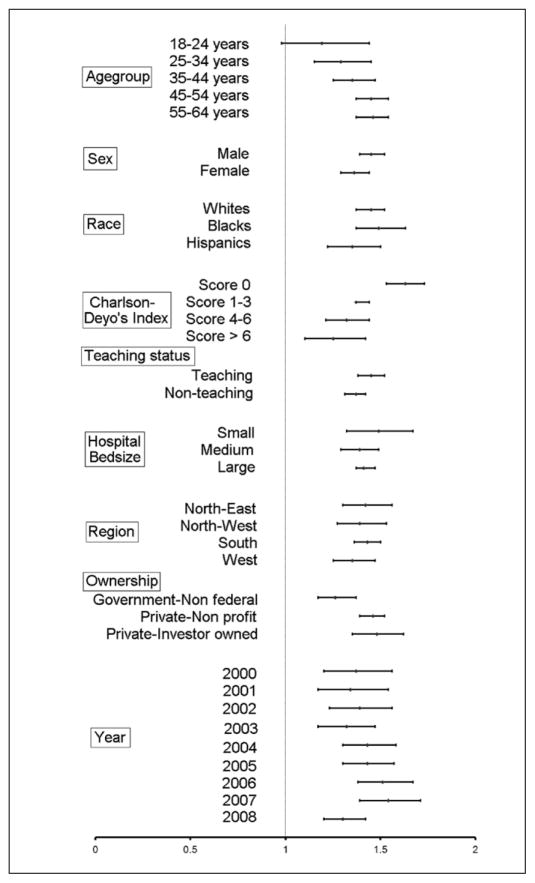
To ascertain whether these mortality differences are seen in subgroups defined by patient and hospital characteristics, we performed separate multivariable logistic regression in various subgroups. We generated a forest plot in Microsoft Excel of association of mortality with lacking insurance versus having private insurance. We used asymptotic Z tests to determine if the effect of lacking insurance on mortality was similar in each subgroup.
We used similar approaches for our secondary endpoints. We used logistic regression to determine the independent association of insurance status with receipt of each of the procedures we considered to represent more intensive treatment of severe sepsis. Similarly, we used linear regression to compare LOS between hospital survivors with and without insurance. As LOS is not normally distributed, we used natural log of LOS as the dependent variable. We used multinomial logistic regression to examine the association between insurance status and discharge disposition to 1) other nonhospital healthcare facilities (most commonly skilled nursing facilities) or 2) home with home healthcare versus other destinations.
RESULTS
From 2000 through 2008, after excluding patients with end-stage renal disease or prior solid organ transplants, there were 1,600,269 hospital discharges in the United States of patients 18 to 64 years old with severe sepsis. Of these, 7.5% were uninsured and 37.9% had private insurance; Medicaid was the primary payer for 24.5% and Medicare in 24.7% (Table 1). Uninsured patients were younger, more likely to be admitted in the South, and more likely to be male and nonwhite than insured patients. Their home zip codes also had lower mean annual income than those of insured individuals.
TABLE 1.
Demographic Characteristics of Patients Aged 18–64 Admitted With Severe Sepsis Over 2000 to 2008 Classified According to Insurance Status
| Variable | Uninsured | Private | Medicare | Medicaid | Othersa |
|---|---|---|---|---|---|
| Severe sepsis | 119,206 | 606,378 | 395,072 | 393,504 | 86,109 |
|
| |||||
| Age in years, mean ± sem | 46.4±0.09 | 51.2±0.05 | 53.1±0.05 | 47.4±0.08 | 48.7±0.15 |
|
| |||||
| Age category (%) | |||||
| 18–24b | 5.1 | 3.2 | 0.6 | 5.6 | 4.8 |
| 25–34b | 13.5 | 6.0 | 4.0 | 10.5 | 9.6 |
| 35–44b | 19.7 | 13.2 | 12.4 | 18.7 | 16.4 |
| 45–54b | 34.4 | 30.6 | 30.4 | 32.5 | 31.9 |
| 55–64b | 27.3 | 46.9 | 52.6 | 32.7 | 37.4 |
|
| |||||
| Sex (%) | |||||
| Maleb | 60.5 | 53 | 55.6 | 50.5 | 63.7 |
| Femaleb | 39.5 | 47 | 44.4 | 49.5 | 36.3 |
|
| |||||
| Race (%) | |||||
| Whiteb | 43.2 | 56.9 | 52.1 | 36.8 | 46.9 |
| African Americanb | 16.6 | 10.9 | 17.2 | 23 | 15.7 |
| Hispanicb | 15 | 5.8 | 6.7 | 14.3 | 12.8 |
| Asianb | 1.5 | 2.1 | 1.0 | 2.3 | 1.4 |
| Native Americansb | 0.6 | 0.4 | 0.5 | 1.0 | 1.5 |
| Othersb | 3.6 | 2.2 | 1.8 | 2.6 | 2.4 |
| Unknownb | 19.5 | 21.8 | 20.8 | 20 | 19.2 |
|
| |||||
| Region (%) | |||||
| North Eastb | 13.6 | 19 | 17.9 | 19.4 | 8.3 |
| North Westb | 14.9 | 23.2 | 21.5 | 19.2 | 12.8 |
| Southb | 54.5 | 37.2 | 43.7 | 38.5 | 54.1 |
| Westb | 17 | 20.6 | 16.9 | 22.9 | 24.7 |
|
| |||||
| Annual zip income | |||||
| 1–38,999b | 33.5 | 17.9 | 30.9 | 38.9 | 32.6 |
| 39,000–47,999b | 28.1 | 23.3 | 28.3 | 27 | 27.7 |
| 48,000–62,999b | 21.7 | 26.3 | 22.5 | 20.2 | 22.7 |
| ≥ 63,000b | 16.7 | 32.5 | 18.2 | 13.9 | 17 |
|
| |||||
| Hospital characteristics (%) | |||||
| Nonteachingb | 49.9 | 46.9 | 52.8 | 43.4 | 45.7 |
| Teachingb | 50.1 | 53.1 | 47.2 | 56.6 | 54.3 |
| Smallb | 9.4 | 9.5 | 10.9 | 8.8 | 8.2 |
| Mediumb | 26 | 23.2 | 23.9 | 24.7 | 24 |
| Largeb | 64.7 | 67.3 | 65.2 | 66.4 | 67.9 |
|
| |||||
| Hospital ownership (%) | |||||
| Government—nonfederalb | 23.3 | 10.7 | 13.2 | 18.2 | 27.4 |
| Private—nonprofitb | 62.9 | 77.1 | 72.1 | 68.8 | 55.4 |
| Private—investor ownedb | 13.8 | 12.1 | 14.7 | 13 | 17.2 |
Patients with “no charge” or “others.”
p < 0.05 using chi-square test.
Table 1 demonstrates demographic characteristics of patients classified by insurance status.
Clinical Characteristics
Uninsured patients were more likely to be admitted through the emergency department than were privately insured patients. On average, they had more organs fail during their hospital stay, a surrogate for sepsis severity. However, uninsured patients had fewer comorbid conditions as measured by Charlson-Deyo’s comorbidity index (Table 2). Patients without insurance were less likely to have diabetes, congestive heart failure, chronic lung disease, and cancer but more likely to have cirrhosis or HIV infection.
TABLE 2.
Clinical Characteristics and Outcomes of Patients Aged 18–64 Admitted With Severe Sepsis Over 2000 to 2008 Classified According to Insurance Status
| Uninsured | Private | Medicare | Medicaid | Othersa | |
|---|---|---|---|---|---|
| Charlson-Deyo’s comorbid index | |||||
| 0b | 37.9 | 32.2 | 29.6 | 28.9 | 36.3 |
| 1–3b | 44.2 | 47.3 | 53.1 | 47 | 45.3 |
| 4–6b | 13 | 11.5 | 11.8 | 15.7 | 12.2 |
| 7 or moreb | 4.9 | 9.0 | 5.5 | 8.4 | 6.2 |
|
| |||||
| Comorbidities (%) | |||||
| Coronary artery diseaseb | 9.1 | 11.8 | 14.1 | 9.8 | 10 |
| Congestive heart failureb | 11.9 | 14.7 | 21.9 | 16.6 | 12.9 |
| Atrial fibrillationb | 5.6 | 8.8 | 9.4 | 6.1 | 6.9 |
| Diabetes mellitusb | 17.3 | 18.8 | 25 | 21.1 | 17.8 |
| Body mass index ≥ 40b | 2.4 | 3.6 | 4.3 | 3.4 | 2.3 |
| Peripheral vascular diseaseb | 3.1 | 3.6 | 5.1 | 3.8 | 3.4 |
| Strokeb | 3.8 | 3.3 | 2.8 | 3.5 | 3.3 |
| Paralysisa | 1.7 | 2.6 | 6.8 | 5.1 | 3.3 |
| Chronic lung diseaseb | 21.9 | 23.1 | 35.8 | 29.2 | 24.1 |
| Cirrhosisb | 15.7 | 11.2 | 9.8 | 14.9 | 14 |
| Chronic kidney diseaseb | 4.2 | 5.3 | 8.4 | 6.2 | 5.1 |
| HIV infectionb | 5.4 | 2.2 | 4.3 | 8.1 | 4.3 |
| Rheumatologic and collagen vascular diseasesb | 1.4 | 2.9 | 3.4 | 2.2 | 1.9 |
| Immunodeficiencyb | 0.2 | 0.3 | 0.3 | 0.2 | 0.2 |
| Malnutritionb | 12.1 | 12.9 | 14.1 | 14.1 | 11.9 |
| Cancer without metastasisb | 5.1 | 11.3 | 5.1 | 7.2 | 7.1 |
| Cancer with metastasisb | 3.8 | 10.6 | 4.0 | 5.9 | 5.7 |
| Lymphoma and leukemiab | 2.9 | 7.1 | 2.8 | 3.7 | 3.9 |
|
| |||||
| Number of organ failures (%) | |||||
| Oneb | 46.6 | 50.0 | 50.5 | 48.7 | 48.4 |
| Twob | 26.5 | 26.4 | 27.9 | 27.4 | 26.6 |
| Threeb | 15.8 | 14.4 | 14.2 | 15.1 | 15.0 |
| Fourb | 7.8 | 6.5 | 5.5 | 6.5 | 7.1 |
| Fiveb | 2.8 | 2.1 | 1.5 | 2.0 | 2.3 |
| Six or sevenb | 0.6 | 0.4 | 0.3 | 0.4 | 0.4 |
|
| |||||
| Three or more organ failures (%)b | 27 | 23.4 | 21.5 | 24 | 24.8 |
|
| |||||
| Type of organ failure (%) | |||||
| Respiratoryb | 58.9 | 54.8 | 56.3 | 58.6 | 58.1 |
| Cardiacb | 30.7 | 31.1 | 31.5 | 30.4 | 30.2 |
| Renalb | 45.6 | 46.1 | 45.6 | 44.4 | 46.2 |
| Hepaticb | 10.4 | 7.9 | 6.2 | 9.0 | 9.1 |
| Metabolicb | 20 | 17.3 | 17 | 17.7 | 19 |
| Neurologicalb | 6.4 | 5.7 | 7.2 | 6.4 | 5.7 |
| Hematologicalb | 21.7 | 21 | 14.6 | 18.6 | 19.9 |
|
| |||||
| Admission source (%) | |||||
| From emergency departmentb | 79.1 | 64 | 70.7 | 73.9 | 72.4 |
| Transfer from other hospitalsb | 6.2 | 9.0 | 7.4 | 6.4 | 7.3 |
| From nursing homesb | 1.5 | 2.1 | 4.2 | 3.9 | 1.9 |
| Law/othersb | 13.1 | 24.8 | 17.7 | 15.8 | 17.8 |
Patients with “no charge” or “others.”
p < 0.05 using chi-square test.
Outcomes
Mortality
In bivariable analysis, uninsured patients had higher mortality (30.0%) than privately insured patients (25.3%) or those with Medicaid (26.9%) (Table 3). The odds of death for uninsured patients remained higher than those of patients covered by private insurance or Medicaid after adjusting for age, gender, race, zip code income, admission source, organ system failures, comorbidity burden, hospital characteristics, and year of admission (Table 4, Model B).
TABLE 3.
Outcomes and Procedures Performed in Patients Aged 18–64 Admitted With Severe Sepsis Over 2000 to 2008 Classified According to Insurance Status
| Uninsured | Private | Medicare | Medicaid | Othersa | |
|---|---|---|---|---|---|
| Mortalityb | 30 | 25.3 | 24.9 | 26.9 | 25.5 |
|
| |||||
| Length of stay in survivors (d)c | 12 (6–22) | 12 (6–23) | 12 (7–21) | 13 (7–25) | 13 (7–24) |
|
| |||||
| Disposition in survivors (%) | |||||
| Homeb | 61.3 | 42.1 | 27.3 | 36.6 | 50.6 |
| Facilityb,d | 17 | 27.4 | 47 | 38.3 | 24.3 |
| Home careb | 10.3 | 21.1 | 17.4 | 16.4 | 13.8 |
| Othersb,e | 11.4 | 9.4 | 8.3 | 9.7 | 12.4 |
|
| |||||
| Procedures (%) | |||||
| Invasive mechanical ventilationb | 49.1 | 43.4 | 44.5 | 48.6 | 47.5 |
| Blood transfusionsb | 22.6 | 24.4 | 23 | 26.6 | 23.5 |
| Tracheostomyb | 7.7 | 9.2 | 7.9 | 10 | 9.5 |
| Central venous catheterb | 41.2 | 42.3 | 45.1 | 45.2 | 43.4 |
| Pulmonary artery flotation catheterb | 0.2 | 0.3 | 0.3 | 0.3 | 0.2 |
| Total parenteral nutrition | 5.1 | 8.1 | 5.7 | 5.8 | 5.5 |
| New dialysisb | 7.1 | 7.8 | 7.0 | 7.6 | 7.2 |
Patients with “no charge” or “others.”
p < 0.05 using chi-square test.
Median days(interquartile range).
Facility includes skilled nursing facility, long-term acute care, rehabilitation, etc.
Others include transfers to other hospitals, against medical advice and unknown.
TABLE 4.
Relationship Between Insurance Status and Mortality Using Different Modelsa
| Private | Medicare | Medicaid | Othersb | |
|---|---|---|---|---|
| Unadjusted odds ratio | 0.79 (0.76–0.81) | 0.78 (0.75–0.80) | 0.86 (0.83–0.89) | 0.80 (0.77–0.84) |
| Adjusted for age, gender, and race (model A) | 0.74 (0.72–0.77) | 0.70 (0.68–0.73) | 0.84 (0.82–0.87) | 0.77 (0.73–0.80) |
| Adjusted for model A + zip income + hospital characteristics + number of organ dysfunction + individual comorbidities (model B) | 0.66 (0.64–0.69) | 0.80 (0.77–0.84) | 0.80 (0.77–0.83) | 0.73 (0.69–0.78) |
| Adjusted for model C + propensity score (model C) | 0.66 (0.64–0.69) | 0.80 (0.77–0.83) | 0.80 (0.77–0.83) | 0.74 (0.70–0.78) |
| Adjusted for model D + procedures (model D) | 0.69 (0.66–0.72) | 0.84 (0.80–0.87) | 0.82 (0.71–0.79) | 0.75 (0.71–0.79) |
| Adjusted for model E with random effect of admission to any hospital (model E) | 0.69 (0.67–0.72) | 0.82 (0.79–0.85) | 0.81 (0.78–0.85) | 0.76 (0.72–0.80) |
All comparisons are with uninsured.
Patients with “no charge” or “others.”
The results are shown as odds ratio (95% CI).
The effect of insurance status on mortality was essentially unchanged when we included the predicted likelihood a person would be uninsured (Table 4, Model D). Similarly, the odds ratio (OR) did not change when we added variables for whether or not procedures were used (Table 4, Model E), suggesting that differential use of these procedures does not account for increase in mortality. Similarly, the addition of random effects terms to account for hospital effect did not reduce the odds of mortality for the uninsured relative to privately insured patients (Table 4, Model E). This suggests that the higher mortality risk among uninsured patients is not due to treatment in hospitals with higher mortality rates. We present the independent effect of each variable in our final model in Appendix 4 (Supplemental Digital Content 1, http://links.lww.com/CCM/A756).
The odds of mortality were higher in uninsured individuals in all subgroups we examined (Fig. 1). Although the mortality rate for severe sepsis declined significantly over the years, the differences in mortality between uninsured patients and those with private insurance remained virtually unchanged between 2000 and 2008 (Appendices 4 and 5, Supplemental Digital Content 1, http://links.lww.com/CCM/A756). Similarly, the risk of mortality in the uninsured cohort was significantly higher than for patients with private insurance in each subgroup we examined. However, magnitude of the difference in mortality risk was greater in both private investor owned (OR, 1.46; 95% CI, 1.39–1.52) and private not for profit (OR, 1.48; 95% CI, 1.35–1.62) hospitals than in government nonfederal hospitals (OR, 1.27; 95% CI, 1.17–1.38) (p for both interactions < 0.05).
Figure 1.
Comparison of uninsured versus private insurance in various subgroups. The graph shows odds ratio of mortality in severe sepsis adjusting for the other variables in Table 3.
Processes of Care
Both in bivariable analysis (Table 3) and after adjusting for potential confounders, uninsured patients were more likely to receive invasive mechanical ventilation in comparison to other insurance categories. Conversely, they were less likely to undergo the other procedures we examined—central venous catheter placement, pulmonary artery catheter placement, total parenteral nutrition, tracheostomy, blood transfusions, and new dialysis (Table 3, Appendix 6, Supplemental Digital Content 1, http://links.lww.com/CCM/A756). LOS was slightly shorter in uninsured patients (Table 3, Appendix 7, Supplemental Digital Content 1, http://links.lww.com/CCM/A756).
Discharge Destination
Uninsured patients were less likely than other patients to be discharged to a nonhospital healthcare facility (17% vs 27%, p < 0.001) or to be discharged home with home healthcare (10.3% vs 21%, p < 0.001) when compared with privately insured patients. After adjusting for potential confounders, odds for being discharged to a nonhospital healthcare facility were 2.06 times higher in privately insured (Appendix 7, Supplemental Digital Content 1, http://links.lww.com/CCM/A756). The adjusted odds of being discharged with home healthcare were 2.64 times higher for privately insured patients (Appendix 7, Supplemental Digital Content 1, http://links.lww.com/CCM/A756).
DISCUSSION
We have shown that the association of insurance status with mortality reported for other medical conditions is also seen with severe sepsis. In particular, we report a 45% increased risk of death during admission for severe sepsis for uninsured patients relative to privately insured patients, adjusting for demographic, clinical, and hospital factors. Our analysis suggests that the increased mortality is not because uninsured patients use different hospitals. Rather, our data suggest that the elevated mortality risk reflects different outcomes among uninsured and privately insured patients within hospitals. We found this association in all patient and hospital subgroups that we examined; furthermore, it has been present from 2000 through 2008, a period when overall severe sepsis mortality has dropped significantly.
Our results are consistent with prior studies of the relationship of insurance to outcomes of critical illnesses (17–19). Lyon et al (10), for example, found an association between lack on insurance and increased 30-day mortality among patients admitted to ICUs throughout Pennsylvania. We arrived at similar conclusions although our estimates of the impact of insurance status on mortality risk are larger. This may reflect differences in the population studied; we restricted our attention to the diagnosis of severe sepsis (the leading cause of admission to noncoronary ICUs in the United States), whereas Lyon et al (10) included all patients admitted to the ICU. Furthermore, we used a larger, nationally representative sample and were able to confirm that these effects persisted over 9 years in a range of hospital and patient subgroups.
Our analysis does not provide a ready explanation for the mortality difference. It is possible that uninsured patients were sicker than their insured counterparts in ways that we could not measure. In addition to foregoing or reducing use of preventive and primary care services (20–22), uninsured patients are more likely to delay or forgo necessary care for potentially serious conditions (23, 24) all of which may contribute to worse outcomes when they are admitted (24). Studies of acute coronary syndromes, for example, suggest that uninsured patients present later and have greater severity of illness that contributes to their increased risk of death (2–4, 25). This would be especially important in severe sepsis where early and aggressive treatment appears to prevent mortality and morbidity (26). As with any observational dataset, we cannot exclude residual confounding from such unmeasured severity factors. This risk is heightened because we lack physiologic data; for example, our administrative data do not allow us to distinguish degrees of acute kidney injury or identify vital sign abnormalities, both of which are associated with sepsis outcomes.
We also considered the impact of hospital. Haider et al (4) have shown that outcomes are worse for trauma patients admitted to hospitals with a poor payer mix. As uninsured patients are more likely to be hospitalized at such hospitals, this could contribute to their higher mortality. However, when we removed the hospital effect by entering hospital as a random effect in our model, differences in mortality were unchanged.
Differences in practices at the end of life could also contribute to higher in-hospital mortality.
We observed that uninsured patients were less likely to be discharged to nonacute healthcare facilities or discharged home with home healthcare than patients with private or Medicaid insurance. Although we do not know why this occurred, it is possible that difficulty transferring the sickest chronically ill uninsured patients to lower acuity settings would allow more deaths of these patients to occur in the hospital. Our data do not include information on deaths after discharge. Similarly, it is possible that physicians were more likely to withdraw life support from terminally ill patients who were uninsured, as seen in a prior study (27); this would allow deaths to be recognized as in-hospital, rather than occurring after discharge. Our finding that mortality differences were lowest in government-funded hospitals could reflect less sensitivity to cost pressures favoring withdrawal of life support.
As most procedures we studied were performed less frequently in the uninsured, it is possible that less intense care contributed to the higher mortality. Although controlling for these specific procedures did not explain the difference in mortality, other services that do affect mortality may also be used less routinely in those without insurance. Uninsured patients have also been less likely to undergo invasive procedures in previous studies in critical care settings (28). Although prior work does suggest that physician decision making is influenced by insurance status (29, 30), nonclinical factors such as distrust of the health system, poor understanding of disease processes and therapies, and poor support systems may combine with financial disincentives to discourage patients’ acceptance of such procedures (27). Furthermore, similar procedures may be performed for different reasons—mechanical ventilation for airway protection may have different severity implications than the same procedure done for respiratory failure. We cannot distinguish such indications with our administrative data.
Although we used a nationally representative, well-characterized database, our study has several important limitations. First, there is no agreed upon definition of sepsis or severe sepsis in studies of administrative data; if we had used a different definition, we might have had different results. Related to this, coding practices may differ depending on the patient’s insurance. The financial incentive for complete capture of procedure and comorbidity status is less if one will not be paid in either case. However, there is ongoing pressure for hospitals to document the amount of uncompensated care that they provide, which would mitigate a tendency to undercode discharges of uninsured patients. Our results regarding discharge destination should also be viewed with caution because we did not have data regarding where the patient was living prior to admission. If uninsured patients were more often homeless, for example, their lower rates of discharge with home care would be expected. Finally, since NIS cannot distinguish multiple hospitalizations of the same patient, our observations are not truly independent; thus, we underestimate the true width of the CIs around our risk estimates.
Despite these limitations, our study represents another clinical scenario where lack of insurance is associated with increased mortality risk. Future research is needed to clarify the mechanisms that lead to this reduced survival, which would allow clinical researchers to develop and test appropriate interventions.
Supplementary Material
Footnotes
Dr. Kumar contributed to study design, statistical analysis, and writing of the article. Dr. Taneja contributed to critical review and revision of the article. Dr. Majumdar contributed to critical review and revision of the article. Dr. Jacobs contributed to critical review and revision of the article. Dr. Whittle contributed to critical review, statistical analysis, and revision of the article. Dr. Nanchal contributed to study design, statistical analysis, and writing of the article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
The authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.United States Census Bureau. [Accessed April 10, 2012]; Available at: http://www.census.gov/hhes/www/hlthins/data/historical/HIB_tables.html.
- 2.Vidovich MI, Vasaiwala S, Cannon CP, et al. Get With Guidelines Steering Committee and Investigators. Association of insurance status with inpatient treatment for coronary artery disease: Findings from the Get With the Guidelines program. Am Heart J. 2010;159:1026–1036. doi: 10.1016/j.ahj.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 4.Haider AH, Chang DC, Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 5.Wilper AP, Woolhandler S, Lasser KE, et al. Health insurance and mortality in US adults. Am J Public Health. 2009;99:2289–2295. doi: 10.2105/AJPH.2008.157685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fowler RA, Noyahr LA, Thornton JD, et al. American Thoracic Society Disparities in Healthcare Group. An official American Thoracic Society systematic review: The association between health insurance status and access, care delivery, and outcomes for patients who are critically ill. Am J Respir Crit Care Med. 2010;181:1003–1011. doi: 10.1164/rccm.200902-0281ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Brien JM, Jr, Lu B, Ali NA, et al. Insurance type and sepsis-associated hospitalizations and sepsis-associated mortality among US adults: A retrospective cohort study. Crit Care. 2011;15:R130. doi: 10.1186/cc10243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar G, Kumar N, Taneja A, et al. Nationwide trends of severe sepsis in the twenty first century (2000–2007) Chest. 2011;140:1223–1231. doi: 10.1378/chest.11-0352. [DOI] [PubMed] [Google Scholar]
- 9.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am J Surg. 2010;199:554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Lyon SM, Benson NM, Cooke CR, et al. The effect of insurance status on mortality and procedural use in critically ill patients. Am J Respir Crit Care Med. 2011;184:809–815. doi: 10.1164/rccm.201101-0089OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project. [Accessed October 28, 2011];Introduction to the HCUP National Inpatient Sample (NIS) 2008 Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2008_INTRODUCTION.pdf.
- 12.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 13.Dombrovskiy VY, Martin AA, Sunderram J, et al. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: A trend analysis from 1993 to 2003. Crit Care Med. 2007;35:1244–1250. doi: 10.1097/01.CCM.0000261890.41311.E9. [DOI] [PubMed] [Google Scholar]
- 14.Kumar G, Sood P, Sakhuja A, et al. Outcomes of severe sepsis in solid organ transplants—A nationwide analysis. Crit Care Med. 2010;38(12 Suppl):U167. [Google Scholar]
- 15.Kumar G, Sakhuja A, Kumar N, et al. End-stage renal disease but not chronic kidney disease is a predictor for worse outcomes in patients with severe sepsis and septic shock. Chest. 2010;138:387A. [Google Scholar]
- 16.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 17.Danis M, Linde-Zwirble WT, Astor A, et al. How does lack of insurance affect use of intensive care? A population-based study. Crit Care Med. 2006;34:2043–2048. doi: 10.1097/01.CCM.0000227657.75270.C4. [DOI] [PubMed] [Google Scholar]
- 18.Durairaj L, Will JG, Torner JC, et al. Prognostic factors for mortality following interhospital transfers to the medical intensive care unit of a tertiary referral center. Crit Care Med. 2003;31:1981–1986. doi: 10.1097/01.CCM.0000069730.02769.16. [DOI] [PubMed] [Google Scholar]
- 19.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: Differences in care and mortality, by insurance status. Am J Public Health. 1994;84:1605–1608. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 21.Richardson LC, Tian L, Voti L, et al. The roles of teaching hospitals, insurance status, and race/ethnicity in receipt of adjuvant therapy for regional-stage breast cancer in Florida. Am J Public Health. 2006;96:160–166. doi: 10.2105/AJPH.2004.053579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hafner-Eaton C. Physician utilization disparities between the uninsured and insured. Comparisons of the chronically ill, acutely ill, and well nonelderly populations. JAMA. 1993;269:787–792. [PubMed] [Google Scholar]
- 23.Baker DW, Shapiro MF, Schur CL. Health insurance and access to care for symptomatic conditions. Arch Intern Med. 2000;160:1269–1274. doi: 10.1001/archinte.160.9.1269. [DOI] [PubMed] [Google Scholar]
- 24.Weissman JS, Stern R, Fielding SL, et al. Delayed access to health care: Risk factors, reasons, and consequences. Ann Intern Med. 1991;114:325–331. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- 25.Kelz RR, Gimotty PA, Polsky D, et al. Morbidity and mortality of colorectal carcinoma surgery differs by insurance status. Cancer. 2004;101:2187–2194. doi: 10.1002/cncr.20624. [DOI] [PubMed] [Google Scholar]
- 26.Rivers E, Nguyen B, Havstad S, et al. Early Goal-Directed Therapy Collaborative Group: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 27.Diringer MN, Edwards DF, Aiyagari V, et al. Factors associated with withdrawal of mechanical ventilation in a neurology/neurosurgery intensive care unit. Crit Care Med. 2001;29:1792–1797. doi: 10.1097/00003246-200109000-00023. [DOI] [PubMed] [Google Scholar]
- 28.Schnitzler MA, Lambert DL, Mundy LM, et al. Variations in healthcare measures by insurance status for patients receiving ventilator support. Clin Perform Qual Health Care. 1998;6:17–22. [PubMed] [Google Scholar]
- 29.Mort EA, Edwards JN, Emmons DW, et al. Physician response to patient insurance status in ambulatory care clinical decision-making. Implications for quality of care. Med Care. 1996;34:783–797. doi: 10.1097/00005650-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Kollef MH. Private attending physician status and the withdrawal of life-sustaining interventions in a medical intensive care unit population. Crit Care Med. 1996;24:968–975. doi: 10.1097/00003246-199606000-00016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.