Abstract
Objective
Many women report positive life changes, or posttraumatic growth (PTG), as a result of their experience with breast cancer. However, despite compelling evidence that younger age at diagnosis is associated consistently with greater distress, age has not been integrated into models of PTG. Drawing from the theoretical and empirical literature, we tested whether key correlates (i.e., cancer-related impact and engagement, positive mood) of PTG varied by age at breast cancer diagnosis.
Methods
Participants were 175 women with early stage breast cancer followed from completion of primary treatment through one year post-treatment. Analyses involved data collected at the one-year assessment.
Results
As hypothesized, correlates of PTG varied significantly as a function of age. Perceived negative impact of the cancer experience was associated with growth for older women (p = .046), whereas approach-oriented coping (p = .004), an expansive time perspective (p = .007), and positive mood were associated with growth for younger women (p = .007).
Conclusions
Posttraumatic growth may involve distinct processes for women diagnosed at different ages. Consideration of lifespan developmental processes is necessary when studying positive adjustment to cancer.
Keywords: posttraumatic growth, breast cancer, aging, oncology, survivorship
Background
Adjustment to a breast cancer diagnosis is complex, with substantial variability in psychological response [1]. Cancer can interrupt women’s emotional, social, and career development, setting the stage for challenges to adjustment during distinct phases in the life course. Indeed, research indicates that the experience of cancer is different for younger and older women, with younger women evidencing greater distress throughout the cancer trajectory [2,3]. The association between age and positive outcomes, such as reports of posttraumatic growth (PTG), has received less attention [4]. PTG refers to the perception that one’s life has changed in valuable ways as a result of an adverse event, including deepened appreciation for life, enhanced relations with others, and/ or a reorganization of life’s priorities [5,6]. Perceptions of growth tend to be higher among younger survivors [7], and may be associated with other indicators of physical and mental well-being [8,9]. However, despite theoretical and clinical significance, the correlates and outcomes of perceived growth for women of different ages are rarely examined.
Theoretically, PTG is initiated only when a stressor is sufficiently disruptive to challenge fundamental assumptions about oneself and the world [5,6,8]. Growth is thought to occur when these assumptions are integrated into a new coherent worldview, primarily through cognitive processing, self-disclosure, and affective engagement [5,6]. Based on these theoretical models, Stanton and colleagues proposed two facilitative conditions for perceived growth in cancer survivors: significant impact from cancer and intentional engagement with the meaning and experience of cancer [8]. Indeed, empirical studies support the idea that greater negative impact from cancer, measured as illness intrusiveness [10], worry about recurrence and health [11], perceiving cancer as highly stressful or a threat to life [12, 13], and in some cases, more intensive cancer treatment [14], is associated with higher PTG in breast cancer survivors. Similarly, measures of cognitive processing [10,15]) as well as broader representations of intentional engagement, such as approach-oriented coping [8], are associated with PTG. More specifically, coping through emotional approach [16], seeking social support [17] problem-solving [18], and active-adaptive coping [10] are associated with PTG among cancer survivors.
Age can potentially influence both the impact of cancer and engagement with one’s cancer experience in breast cancer survivors. Younger breast cancer survivors experience greater impact from cancer, reporting greater emotional distress and poorer psychological adjustment than older survivors [2,3]. These findings may arise from the non-normative nature of a chronic disease at a younger age, which causes disruption in multiple life roles and may lead to feelings of isolation [19] and distress over premature menopause and infertility [3]. Researchers have suggested that higher life impact may contribute to PTG among younger individuals [15, 20], but no studies have tested whether the relationship between impact and PTG varies by age at diagnosis.
Relevant to engagement, distinct coping and emotion regulation strategies are used across the lifespan [21,22], likely in service of unique goals. Older individuals place greater emphasis on antecedent emotion regulation, aimed at preventing the onset of emotional distress and preserving well-being [22], and report greater motivation to down-regulate negative emotions and maintain positive emotions than younger individuals [23]. Age-related changes in coping may emerge in response to the increasing salience of mortality that accompanies growing older [22]. Socioemotional selectivity theory (SST) proposes that the realization that one has less time left to live facilitates an adaptive shift towards the prioritization of more immediately attainable goals, particularly emotional well-being [22]. By contrast, younger individuals have a more expansive time perspective and thus prioritize future-oriented goals, such as acquiring knowledge and information [22]. Age-related differences in time perspective might influence the emergence of PTG; however, this has not been assessed.
This study was designed to elucidate the role of age in PTG among breast cancer survivors and specifically to evaluate whether age moderates the association between negative impact, approach-oriented coping, time perspective, and PTG. Due to the limited research in this area, no directional hypotheses were advanced. We examined these questions in a cohort of women who had completed treatment for early-stage breast cancer, focusing on measures collected one year after treatment completion. Identifying factors associated with positive adjustment for women of different ages is important at this point in the survivorship trajectory. Women transitioning from patient to survivor face new challenges, including fear of recurrence, lingering side effects from cancer treatment, and a reduction in support from friends, family, and medical staff [24]. In addition, this study examined how age may influence positive mood in relation to PTG. Theoretical models do not suggest that PTG is associated with reduced distress [5], but empirical work suggests that positive mood may play an important role in PTG in cancer survivors [8,14]. Therefore, we assessed whether the relationship between PTG and positive mood was moderated by age.
Method
Participants and Procedure
Participants for this study were 175 breast cancer patients drawn from a larger longitudinal study of cognitive functioning in adult patients after breast cancer treatment at the University of California, Los Angeles (UCLA) [24]. Eligibility criteria for the parent study included English-speaking women, age 21–65 years, newly diagnosed with Stage 0–IIIA breast cancer, who had completed primary treatment within the past 3 months but not begun endocrine therapy. Exclusion criteria were prior cancer diagnosis, past chemotherapy, neurologic or psychotic-spectrum disorder, current major affective disorder, daily tobacco and alcohol use, or active immune-related disorder.
Recruitment took place in Los Angeles (5/2007–2/2011), using the LA County SEER registry to identify eligible patients of collaborating physicians. See Ganz (2013) [25] for details on participant screening, recruitment, and enrollment. Briefly, over 3,000 patients were mailed brochures describing the study; 440 responded, 240 were eligible after phone screening, 191 consented and participated, and 190 provided evaluable questionnaire data (79.6% participation rate). Nonparticipating eligible patients were less likely to be non-Hispanic white than participants, but did not differ on other major demographic or treatment-related variables [25].
After approval by the UCLA IRB and with informed consent, data were collected in person at UCLA at study entry (T1) and six (T2) and 12 (T3) months later. At each point, participants underwent neuropsychological testing, provided blood samples, and completed questionnaires. PTG and positive mood were assessed at each time point, but measures of impact, engagement, and time perspective were administered at T3 only. Thus, analyses for this study focused on data collected at T3, which occurred approximately one year after completion of primary treatment; 175 women provided questionnaire data at this assessment point (92.1% completion rate). Participants who did not return at T3 (n = 15) reported lower income than participants who completed both T1 and T3 assessments (p = .02), but did not differ on other demographic or treatment-related variables (all p’s > .27).
Measures
Demographic and treatment-related variables
Demographic information was obtained from self-report. Treatment-related information was obtained from medical record abstraction.
Posttraumatic Growth Inventory (PTGI)
The PTGI is a 21-item scale measuring the extent to which individuals believe they have changed in positive ways following significant adversity [26]. Participants indicate whether they experienced positive changes since their diagnosis as a result of their experience with breast cancer on a 0–5 scale (0 = I did not experience this change; 5 = I experienced this change to a very great degree). Reliability was high at both time points in the current study (α > .95).
Impact of Cancer v.2 Negative Impact Summary Scale (IOC NIS)
The IOC NIS was our primary measure of impact. This valid and reliable scale assesses negative effects of cancer on several domains of quality of life [27], and has shown significant associations with symptoms of post-traumatic stress in cancer survivors [28]. The IOC NIS scale has four subscales: Appearance Concerns (3 items), Body Change Concerns (3 items), Life Interference (7 items), and Worry (7 items). Participants endorsed statements about their experience with cancer on a 1–5 scale (1 = strongly disagree, 5 = strongly agree), in reference to their life “as it is now” with higher scores indicating greater negative impact. The total score represents the mean of all 20 items. Internal consistency in the current study was high (α = .94).
Perceived stressfulness of breast cancer
Participants completed a one-item rating of “how stressful your experience with breast cancer has been” since diagnosis (1 = not at all stressful, 5 = extremely stressful). In previous research with breast cancer survivors, perceived cancer stress has predicted PTG [12], and was used here as a secondary measure of impact.
COPE and Emotional Approach Coping (EAC) Scales
Approach-oriented coping was assessed using a composite of subscales from the Brief COPE [29], and the EAC [30], a method that been used in previous studies of PTG [e.g. 17]. Subscales from the Brief COPE included active coping, planning, acceptance, instrumental and emotional social support seeking (2 items each), and the EAC included emotional expression and emotional processing (4 items each). Positive reappraisal coping was excluded given overlap with PTG [5]. Items were completed in reference to “what you have been doing to cope with your experience of cancer, including your current physical or emotional concerns related to your cancer experience” and were rated on 4-point scale (1 = I don’t do this at all; 4 = I do this a lot). The means of each subscale were used to compute an overall composite mean, giving each subscale equal weight in the composite. Internal consistency was acceptable in the current study (α = .82). Subscales were positively and significantly correlated (r = 0.16 to .65, p < 0.05).
Future Time Perspective Scale (FTP)
The 10-item FTP scale [31] measures perceived limitations on time left to live. Participants indicate agreement with each of 10 items on a scale from 1 (very untrue) to 7 (very true). Items include “Most of my life lies ahead of me,” “Many opportunities await me in the future” and “I have the sense time is running out” (reverse coded). A total score is created by summing the items, with lower scores reflecting a less expansive time perspective (i.e. limited time to live), and higher scores reflecting a more expansive and future-oriented time perspective. Internal consistency in the current study was α = .87.
Positive and Negative Affect Scale (PANAS)
The PANAS is a reliable and valid 20-item scale used to assess positive and negative mood [32]. Participants indicated the extent to which they felt each of 10 positive and 10 negative feelings during the prior four weeks (1 = very slightly or not at all, 5 = extremely). Internal consistency in the current study was high for the positive (α > .93) and negative (α > .88) subscales.
Data Analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences v18. Age was treated as a continuous variable in all analyses. Demographic and treatment-related variables were examined for inclusion as covariates by assessing their Pearson-product moment or point-biserial correlations with PTG and with age.
Hierarchical regression analyses were conducted to evaluate whether age moderated the association between each of these variables and PTG concurrently at T3. All variables were mean-centered. The main effect for age, the main effect for the variable of interest, and covariates were entered in Step 1, and the interaction between age and the variable was entered in Step 2. Significant interactions were followed with simple slopes analyses using the PROCESS macro in SPSS and plotted using one standard deviation above and below the mean age [33]. Statistical significance was set at p < .05.
Results
Participant Characteristics
On average, participants were 53 years old at T3 (SD = 8.02, range = 33.5–66.7). The majority were white, married, and college educated. Approximately half the participants had received chemotherapy. Demographic and treatment-related variables are presented in Table 1. Descriptive information for psychosocial questionnaires is reported in Table 2.
Table 1.
Demographic and Medical Characteristics of the Sample (N = 175)
| Characteristics | No. | % |
|---|---|---|
| Race (n = 174) | ||
| White, non-Hispanic | 144 | 82.8 |
| Other race/ethnicity | 30 | 17.2 |
| Marital Status | ||
| Married/Partnered | 137 | 78.3 |
| Not Married/Partnered | 38 | 21.7 |
| Education | ||
| Postcollege | 91 | 52 |
| College | 52 | 29.7 |
| Some college/Associates | 29 | 16.6 |
| Vocational, HS or less | 3 | 1.7 |
| Employment | ||
| Full or part-time | 119 | 68 |
| Not employed | 56 | 32 |
| Annual household income (n = 173) | ||
| ≤ $60,000 | 29 | 16.7 |
| $60,001-$100,000 | 43 | 24.9 |
| > $100,000 | 101 | 58.4 |
| Stage of Diagnosis | ||
| 0 | 25 | 14.3 |
| 1 | 80 | 45.7 |
| 2 | 53 | 30.3 |
| 3 | 17 | 9.7 |
| Surgery | ||
| Mastectomy | 59 | 33.7 |
| Lumpectomy | 116 | 66.3 |
| Adjuvant therapy | ||
| Radiation therapy | 130 | 74.3 |
| Chemotherapy | 89 | 50.9 |
| Endocrine therapy (at T3; n = 174) | 123 | 70.7 |
| Months since diagnosis at T3 (n = 174) | M = 18.61 (SD = 2.88) | |
Note. Race, education, surgery, chemotherapy, and radiation data were collected at study entry; all other data collected 12 months later (T3). HS = high school.
Table 2.
Correlations, Means and Standard Deviations of Study Variables
| Mean | SD | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 53 | 8.02 | 33–66 | ||||||||||||
| 2. PTG | 47.12 | 26.18 | 0–102 | −.26** | |||||||||||
| 3. IOC NIS | 2.67 | 0.81 | 1–4.8 | −.19* | .26** | ||||||||||
| 4. Approach Coping | 2.98 | 0.50 | 1–3.96 | −.06 | .23** | .02 | |||||||||
| 5. PSC | 3.31 | 1.11 | 1–5 | −.12 | .36** | .54** | −.05 | ||||||||
| 6. FTP | 45.35 | 11.12 | 17–69 | −.19* | .07 | −.50** | .21** | −.28** | |||||||
| 7. PA | 31.61 | 8.63 | 12–50 | .08 | .08 | −.47** | .12 | −.12 | .40** | ||||||
| 8. NA | 16.58 | 6.26 | 10–41 | .00 | .09 | .51** | .12 | .25** | −.37** | −.45** | |||||
| 9. Months since dx | 18.61 | 2.88 | 13.3–30.7 | −.18* | .17* | .19* | .01 | .23** | −.01 | .00 | −.01 | ||||
| 10. Surgery Typea | −.18* | .19* | .12 | −.02 | .09 | −.11 | .06 | .11 | .05 | ||||||
| 11. Chemotherapyb | −.16* | .26** | .15* | .06 | .19* | .04 | −.01 | .02 | .66** | .12 | |||||
| 12. Racec | .33** | −.24** | −.07 | −.13 | −.09 | −.10 | .05 | −.08 | −.12 | −.03 | −.09 |
Note. Surgery type, chemotherapy, and race data were collected at study entry; all other data collected 12 months later (T3). Correlations are Pearson-product moment or point-biserial where appropriate. PTG = Posttraumatic Growth Inventory; IOC NIS = Impact of Cancer v.2 Negative Impact Summary Scale; PSC = Perceived stressfulness of cancer; FTP = Future Time Perspective Scale; PA = positive affect; NA = negative affect; dx=diagnosis.
Surgery type coded as (0 = lumpectomy, 1 = mastectomy).
Chemotherapy coded as (0 = no, 1 = yes).
Race coded as (0 = Other Race/Ethnicity, 1 = White).
p < .05,
p <. 01
Associations between age, PTG, and study variables
First, we examined Pearson-product moment and point biserial correlations between demographic and treatment-related variables and the two key variables: age and PTG (see Table 2). Younger women were significantly less likely to be white, more likely to have been treated with mastectomy and chemotherapy, and were farther from diagnosis (all p’s < .05) than older women. PTG was also associated with non-white ethnicity, receipt of chemotherapy and mastectomy, and longer time since diagnosis (all p’s < .03). Therefore, we included race, surgery type, time since diagnosis, and chemotherapy treatment as covariates in regression analyses.
Turning to measures of impact and engagement, we found that PTG was positively correlated with higher negative impact of cancer (IOC NIS), higher perceived stressfulness of breast cancer, and greater use of approach-oriented coping (Table 2). Positive mood and time perspective were not significantly correlated with PTG. Younger women reported higher PTG and greater negative impact of cancer on the IOC NIS. Age was not correlated significantly with perceived stressfulness of breast cancer, approach-oriented coping, or positive mood. Age was negatively correlated with time perspective, indicating that younger women had a higher, more expansive time perspective, and older women had a lower, or less expansive time perspective.
Moderating Effects of Age on Correlates of PTG
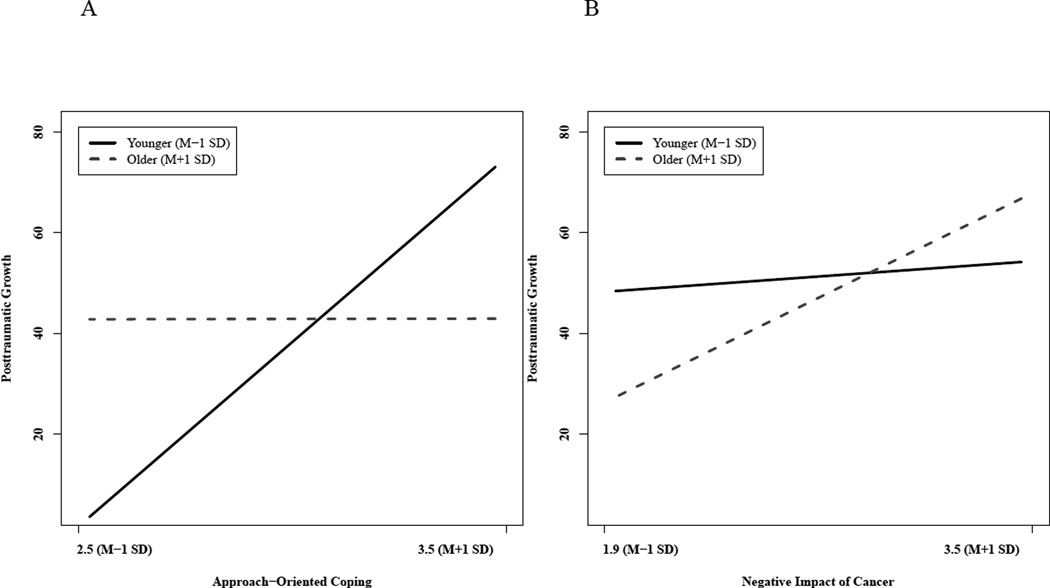
Hierarchical regression analyses were conducted to test the hypothesis that age moderated the association between cancer impact and PTG. As predicted, age interacted significantly with negative impact of cancer (IOC NIS), (interaction term b = 0.56, p < .05; see Table 3). Simple slopes analysis was used to decompose the interaction by computing regression lines at one standard deviation above and below the mean age (ages 45 and 61). As shown in Figure 1A, there was a significant association between negative impact and PTG among older women (simple slopes b = 10.70, p < .01), but not younger women (p = .59). Similar results emerged from regression analyses testing the relationship between receipt of chemotherapy and PTG (overall model R2 = .18, F(6, 166) = 5.98, p < .001). In this model, the interaction between age and chemotherapy was significant (ΔR2= .02, b = 1.07, p < .05), such that PTG was significantly related to receipt of chemotherapy among older women (simple slopes b = 21.17, p < .01), but not among younger women (p = .51). The overall model for perceived stressfulness of breast cancer as a correlate of PTG was also significant, R2 = .26, F(7, 162) = 8.02, p < .001, and the interaction between perceived stressfulness and age approached significance (ΔR2 = .01, simple slopes b = 0.38, p = .075).
Table 3.
Hierarchical Regression Analyses with Impact and Engagement Predicting Posttraumatic Growth as a Function of Age
| Predictor | ΔR2 | B | SE (B) |
|---|---|---|---|
| Impact | |||
| Step 1 | .19*** | ||
| Racea | −10.98* | 5.24 | |
| Surgery Typeb | 7.16 | 4.05 | |
| Chemotherapyc | 10.80* | 5.02 | |
| Months since diagnosis | −0.22 | 0.88 | |
| Age | −0.38 | 0.25 | |
| Negative Impact (IOC NIS) | 6.22** | 2.38 | |
| Constant | 53.11** | 15.99 | |
| Step 2 | .02* | ||
| Age* Negative Impact (IOC NIS) | 0.56* | 0.28 | |
| Total R2 | .21* | ||
| Final model F(df) | 6.07*** (7, 161) | ||
| Engagement | |||
| Step 1 | .19*** | ||
| Race | -10.81* | 5.18 | |
| Surgery Type | 7.14 | 3.97 | |
| Chemotherapy | 12.12* | 4.93 | |
| Months since diagnosis | −0.10 | 0.85 | |
| Age | −0.48 | 0.25 | |
| Approach-Oriented Coping | 12.80** | 3.80 | |
| Constant | 49.06** | 15.57 | |
| Step 2 | .04* | ||
| Age* Approach-Oriented Coping | −1.52** | 0.52 | |
| Total R2 | .23* | ||
| Final model F(df) | 7.01*** (7, 161) | ||
Note. Estimates displayed are for the final regression model, variables are mean centered.
N =169. IOC NIS = Impact of Cancer v.2 Negative Impact Summary Scale.
Race coded as (0 = Other Race/Ethnicity, 1 = White).
Surgery type coded as (0 = lumpectomy, 1 = mastectomy).
Chemotherapy coded as (0 = no, 1 = yes).
p < .05,
p < .01,
p < .001.
Figure 1.
The moderating effect of age on the relationship between the negative impact of cancer (IOC NIS) and PTG (Panel A) and approach-oriented coping and PTG (Panel B). Higher negative impact was significantly related to higher PTG only among older women, whereas use of approach-oriented coping was related to higher PTG only among younger women. Estimated slopes represent women who are 45 years old (1 SD below the mean age) and 61 years old (1 SD above the mean age).
Age also significantly moderated the association between approach-oriented coping and PTG (interaction term b = −1.52, p < .01; see Table 3). As shown in Figure 1B, PTG was significantly related to approach-oriented coping among younger women (simple slopes b = 25.00, p < .001), but not older women (p = .90). Exploratory hierarchical regression analyses decomposed the approach-oriented composite to determine whether particular subscales were driving this effect. The same pattern of results was seen when using emotional processing (interaction term b = −.80, p < .05), seeking emotional social support (interaction term b = −.67, p < .05), and seeking instrumental social support (interaction term b = −.51, p < .05), in place of the approach-oriented composite. Simple slopes revealed that PTG was significantly associated with emotional processing (simple slopes b = 15.60, p < .01) seeking emotional support (simple slopes b = 14.45, p < .001), and seeking instrumental social support (simple slopes b = 7.38, p < .05) among younger women only. Active coping, planning, acceptance and emotional expression yielded non-significant interaction terms for the full model.
Regarding whether age moderated the association between time perspective and PTG, the overall model was significant, R2 = .20, F(7, 160) = 5.73, p < .001, as was the interaction between age and time perspective (ΔR2 = .04, b = −0.06, p < .01). PTG was significantly related to a more expansive time perspective for younger women (simple slopes b = 0.69, p < .05) and was not related to time perspective for older women (p = .13).
Finally, hierarchical regression analyses were used to test whether age moderated the association between PTG and positive mood. Demographic and treatment-related covariates, age, and PTG were entered in Step 1. Step 1 also included negative mood to allow for an independent assessment of positive mood. The interaction between age and PTG was entered in Step 2. The overall model was significant, R2 = .27, F(8, 164) = 7.73, p < .001, as was the interaction between age and PTG (ΔR2 = .04, interaction term b =−0.01 p < .01). Analysis of simple slopes revealed that PTG was significantly associated with higher positive mood among younger women (simple slopes b = 0.12, p = .001), but not older women (p = .73).
Conclusions
In investigating whether age is an important contextual variable in understanding positive adjustment to breast cancer, we found distinct age-related differences unaccounted for by current theories of PTG. Theory and prior studies suggest that perceiving breast cancer as threatening and stressful is one important facilitator of PTG [5,8]. We noted such a pattern in bivariate analyses, but these relations were qualified by age. Specifically, greater negative impact of cancer and receipt of chemotherapy were associated with PTG only among older women, with the same trend observed for perceived stressfulness of breast cancer. Similarly, although we noted a significant association between approach-oriented coping and PTG for the total sample, this relationship was also qualified by age. Greater use of approach-oriented coping was associated with higher PTG only among younger women. Of note, these striking differences were evident within a restricted age range (33 years old to 66 years old).
The findings paint a complex picture of PTG in breast cancer survivors. Contrary to theory, we found no association between perceived growth and negative impact among younger women. This is notable given prior suggestion that greater impact may contribute to higher perceived growth among younger individuals [15,34]. It is unlikely that our indicators of negative impact were less relevant to younger women, as younger women reported higher scores on the NIS, were more likely to receive chemotherapy, and reported levels of perceived stressfulness of breast cancer equivalent to that of older women. Instead, our results suggest that PTG for younger survivors reflects a hopeful and forward-looking experience that is less closely tied to negative impact. Among the younger women in our sample, perceived growth was strongly associated with approach-oriented coping, positive mood, and an expansive, future oriented perspective, which together may reflect a sense of optimism and self-efficacy [35,36]. Given the convergence of these measures, we find it unlikely that PTG among younger women reflects a defensive coping strategy [9] or adherence to social expectations to adopt a positive attitude [15].
By contrast, perceived growth was unrelated to approach-oriented coping in older women, even though women of all ages endorsed approach-oriented coping. This suggests that approach-oriented coping, including emotional processing and seeking support, might be less relevant for older survivors, at least in terms of PTG. This interpretation is consistent with a developmental shift towards avoiding emotional distress observed in the general literature [21,23]. It is also possible that different types of engagement may be more relevant for older survivors. Experiencing and expressing generativity, or an outward-looking care for others and future generations, is an important feature in middle and late adulthood [34,37] and shows moderate associations with PTG among cancer survivors [4]. Furthermore, altruism, empathy, and prosocial behavior [37,38] increase with age. Coping by increasing altruistic behaviors (e.g., acting as a mentor to other cancer survivors) or making plans for future generations (e.g., spending time with grandchildren) might reflect the types of strategies important for growth among older women.
Developmental shifts may also contribute to distinct associations between positive mood and perceived growth. Research suggests that low-arousal positive affect increases with age and is more valued than high-arousal positive affect among older adults [23, 39]. The current study assessed positive mood using the PANAS, a measure that primarily taps high-arousal positive emotions [39]. Thus, it is possible that measures more aligned with adults’ emotional trajectories might better capture positive outcomes of PTG among older women.
Several limitations to this study should be noted. We describe women as “older” versus “younger”, but our results are limited to women between the ages of 33 and 66. Further, age serves as a proxy for other development processes. Examining PTG in the context of biopsychosocial transitions, such as menopause, or within developmental frameworks will be valuable [e.g., 4,34,40]. Analyses were cross-sectional and conducted in the survivorship period; our findings cannot capture the dynamic nature of adaptation to cancer over time or establish causality. Finally, despite a broad recruiting strategy, the generalizability of the results to more diverse groups of survivors is an important topic for research.
Despite these limitations, the present findings demonstrate age as a key contextual factor in the study of PTG. Impact and engagement are central in other theoretical models of positive change following adversity [9], and our results suggest explicitly incorporating age and socioemotional changes across the lifespan could advance our understanding of perceived growth. Lower PTG in older cancer survivors is not due solely to lower impact and lower engagement. Rather, the findings suggest that PTG involves distinct processes and may reflect a different experience for younger and older women.
Acknowledgments
Supported by funding from NIH/NCI R01 CA 109650, the Breast Cancer Research Foundation (PAG), and the NIH/NIMH Predoctoral Fellowship 5T32MH015750-35 (CCB)
Footnotes
Declaration of Conflicting Interests
The authors had no conflicts of interest with respect to their authorship or the publication of this article.
References
- 1.Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: Identifying distinct trajectories of change. Health Psychology. 2004;23(1):3–15. doi: 10.1037/0278-6133.23.1.3. doi: http://dx.doi.org/10.1037/0278-6133.23.1.3. [DOI] [PubMed] [Google Scholar]
- 2.Kroenke CH, Rosner B, Chen WY, Kawachi I, Colditz Ga, Holmes MD. Functional impact of breast cancer by age at diagnosis. Journal of Clinical Oncology. 2004;22(10):1849–1856. doi: 10.1200/JCO.2004.04.173. [DOI] [PubMed] [Google Scholar]
- 3.Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: A systematic review. Journal of the National Cancer Institute. 2012;104(5):386–405. doi: 10.1093/jnci/djr541. [DOI] [PubMed] [Google Scholar]
- 4.Bellizzi KM. Expressions of generativity and posttraumatic growth in adult cancer survivors. International Journal of Aging & Human Development. 2004;58(4):267–287. doi: 10.2190/DC07-CPVW-4UVE-5GK0. [DOI] [PubMed] [Google Scholar]
- 5.Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004;15(1):1–18. [Google Scholar]
- 6.Janoff-Bulman R, Frantz CP. The impact of trauma on meaning: From meaningless world to meaningful life. In: Powers M, Brewir CR, editors. The Transformation of Meaning in Psychological Therapies. Hoboken, NJ: John Wiley & Sons Inc; 1997. pp. 91–106. [Google Scholar]
- 7.Koutrouli N, Anagnostopoulos F, Potamianos G. Posttraumatic stress disorder and posttraumatic growth in breast cancer patients: A systematic review. Women & Health. 2012;52(5):503–516. doi: 10.1080/03630242.2012.679337. [DOI] [PubMed] [Google Scholar]
- 8.Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of posttraumatic growth: Research and practice. Mahwah, NJ: Erlbaum; 2006. pp. 138–175. [Google Scholar]
- 9.Sumalla EC, Ochoa C, Blanco I. Posttraumatic growth in cancer: Reality or illusion? Clinical Psychology Review. 2009;29(1):24–33. doi: 10.1016/j.cpr.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Danhauer SC, Case LD, Tedeschi R, Russell G, Vishnevsky T, Triplett K, Avis NE. Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology. 2013;22(12):2676–2683. doi: 10.1002/pon.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonough MH, Sabiston CM, Wrosch C. Predicting changes in posttraumatic growth and subjective well-being among breast cancer survivors: the role of social support and stress. Psycho-Oncology. 2014;23(1):114–120. doi: 10.1002/pon.3380. [DOI] [PubMed] [Google Scholar]
- 12.Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22(5):487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- 13.Cordova MJ, Cunningham LLC, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychology. 2001;20(3):176–185. doi: [PubMed] [Google Scholar]
- 14.Bower JE, Meyerowitz BE, Desmond KA, Bernaards CA, Rowland JH, Ganz P. Perceptions of positive meaning and vulnerability following breast cancer: Predictors and outcomes among long-term breast cancer survivors. Annals of Behavioral Medicine. 2005;29(3):236–245. doi: 10.1207/s15324796abm2903_10. [DOI] [PubMed] [Google Scholar]
- 15.Manne S, Ostroff J, Winkel G, Goldstein L, Fox K, Grana G. Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosomatic Medicine. 2004;66(3):442–454. doi: 10.1097/01.psy.0000127689.38525.7d. [DOI] [PubMed] [Google Scholar]
- 16.Thornton AA, Owen JE, Kernstine K, Koczywas M, Grannis F, Cristea M, Stanton AL. Predictors of finding benefit after lung cancer diagnosis. Psycho-Oncology. 2011;21(4):365–373. doi: 10.1002/pon.1904. [DOI] [PubMed] [Google Scholar]
- 17.Thornton AA, Perez MA. Posttraumatic growth in prostate cancer survivors and their partners. Psycho-Oncology. 2006;15(4):285–296. doi: 10.1002/pon.953. [DOI] [PubMed] [Google Scholar]
- 18.Widows MR, Jacobsen PB, Booth-Jones M, Fields KK. Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychology. 2005;24(3):266–273. doi: 10.1037/0278-6133.24.3.266. [DOI] [PubMed] [Google Scholar]
- 19.Thewes B, Butow P, Girgis A, Pendlebury S. The psychosocial needs of breast cancer survivors: A qualitative study of the shared and unique needs of younger versus older survivors. Psycho-Oncology. 2004;13(3):177–189. doi: 10.1002/pon.710. [DOI] [PubMed] [Google Scholar]
- 20.Blank TO. Cancer and Aging Handbook: Research and Practice. Hoboken, JH: Wiley-Blackwell; 2013. Theoretical Perspectives from Gerontology and Lifespan Development; pp. 347–364. [Google Scholar]
- 21.Baltes PB, Lindenberger U, Staudinger U. Lifespan theory in developmental psychology. In: Damon W, Lerner R, editors. Handbook of child psychology: Volume 1: Theoretical models of human development. 5th. Hoboken, NJ: John Wiley & Sons, Inc; 1998. pp. 569–664. [Google Scholar]
- 22.Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. American Psychologist. 1999;54(3):165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 23.Scheibe S, Carstensen L. Emotional aging: Recent findings and future trends. Journal of Gerontology: Psychological Sciences. 2010;65B(2):135–144. doi: 10.1093/geronb/gbp132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stanton AL. What happens now? Psychosocial care for cancer survivors after medical treatment completion. Journal of Clinical Oncology. 2012;30(11):1215–1220. doi: 10.1200/JCO.2011.39.7406. [DOI] [PubMed] [Google Scholar]
- 25.Ganz PA, Kwan L, Castellon SA, Oppenheim A, Bower JE, Silverman DHS, Belin TR. Cognitive complaints after breast cancer treatments: Examining the relationship with neuropsychological test performance. Journal of the National Cancer Institute. 2013;105(11):791–801. doi: 10.1093/jnci/djt073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9(3):455–470. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 27.Crespi CM, Ganz PA, Petersen L, Castillo A, Caan B. Refinement and psychometric evaluation of the impact of cancer scale. Journal of the National Cancer Institute. 2008;100(21):1530–1541. doi: 10.1093/jnci/djn340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hahn EE, Hays RD, Kahn KL, Litwin MS, Ganz PA. Post-traumatic stress symptoms in cancer survivors: relationship to the impact of cancer scale and other associated risk factors. Psycho-Oncology. 2014 doi: 10.1002/pon.3623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carver C. You want to measure coping but your protocol’s too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 30.Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: Scale construction and validation. Journal of Personality and Social Psychology. 2000;78(6):1150–1169. doi: 10.1037//0022-3514.78.6.1150. [DOI] [PubMed] [Google Scholar]
- 31.Carstensen LL, Lang FR. Future time perspective scale. Stanford University; 1996. [Google Scholar]
- 32.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 33.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press; 2013. [Google Scholar]
- 34.Blank TO, Bellizzi KM. A gerontologic perspective on cancer and aging. Cancer. 2008;112(11 Suppl):2569–2576. doi: 10.1002/cncr.23444. [DOI] [PubMed] [Google Scholar]
- 35.Allemand M, Hill PL, Ghaemmaghami P, Martin M. Forgivingness and subjective well-being in adulthood: The moderating role of future time perspective. Journal of Research in Personality. 2012;46(1):32–39. [Google Scholar]
- 36.Nes LS, Segerstrom SC. Dispositional optimism and coping: A meta-analytic review. Personality and Social Psychology Review. 2006;10(3):235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- 37.Freund AM, Blanchard-Fields F. Age-related differences in altruism across adulthood: Making personal financial gain versus contributing to the public good. Developmental Psychology. 2014;50(4):1125–1136. doi: 10.1037/a0034491. doi: http://dx.doi.org/10.1037/a0034491. [DOI] [PubMed] [Google Scholar]
- 38.Sze JA, Gyurak A, Goodkind MS, Levenson RW. Greater emotional empathy and prosocial behavior in late life. Emotion. 2012;12(5):1129. doi: 10.1037/a0025011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scheibe S, English T, Tsai JL, Carstensen LL. Striving to feel good: Ideal affect, actual affect, and their correspondence across adulthood. Psychology and Aging. 2013;28(1):160–171. doi: 10.1037/a0030561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rowland JH. Developmental stage and adaptation: Adult model. In: Holland JD, Rowland JH, editors. Handbook of psycho-oncology. New York, NY: Oxford University Press; 1990. pp. 25–43. [Google Scholar]