Abstract
Young women in South Africa are at high risk for HIV infection. Cash transfers offer promise to reduce HIV risk. We present the design and baseline results from HPTN 068, a phase III, individually randomized trial to assess the effect of a conditional cash transfer on HIV acquisition among South African young women. A total of 2533 young women were randomized to receive a monthly cash transfer conditional on school attendance or to a control group. A number of individual-, partner-, household- and school-level factors were associated with HIV and HSV-2 infection. After adjusting for age, all levels were associated with an increased odds of HIV infection with partner-level factors conveying the strongest association (aOR 3.05 95 % CI 1.84–5.06). Interventions like cash transfers that address structural factors such as schooling and poverty have the potential to reduce HIV risk in young women in South Africa.
Keywords: HIV, Adolescents, South Africa, Young women, HIV prevention, Cash transfers, Education
Background
Young women continue to be at the epicentre of the human immunodeficiency virus (HIV) epidemic in South Africa. The latest available data show a national HIV prevalence of 5.6 % among adolescent girls aged 15–19 years, rising to 17.4 % for young women aged 20–24 years while among adolescent boys and young men it is one-fifth that figure [1]. Incidence of infection is also high, at over 5 % per year among young women in many settings in South Africa, where it is estimated that over 2000 young women aged 15–24 years are infected with HIV every week [2–4].
Due to these high infection rates among young women in sub-Saharan Africa (SSA), including South Africa, young women are considered a key population for greater focus of HIV prevention efforts [4]. Young women are at increased risk of HIV infection due to a combination of factors, but in particular structural factors, including lack of education, poverty, and negative gender norms which contribute to high rates of gender based violence. To date, there have been limited rigorously evaluated interventions aimed at addressing these structural factors to reduce HIV risk among young women in SSA [5, 6].
Higher levels of education have been shown to reduce HIV risk in young women [7–9]. In our prior research among young South African women, we found that those who had not completed high school were almost four times more likely to be infected with HIV compared to those who graduated [7]. Despite the benefits of education, many young people, in particular young women, do not complete school due to economic barriers [10].
Multiple factors such as cost of schooling and uniforms, the need to take care of small children, sick relatives and household chores, are important barriers to education [10, 11]. Cash transfers conditional on school attendance have been found to increase school enrollment and attendance and reduce structural risk factors for young women in many settings. In Mexico, Honduras, Malawi and Cambodia they have been shown to increase attendance [10]. In Malawi, a randomized controlled trial found that young women (aged 13–22) who received cash transfers had a 64 % lower prevalence of HIV compared to those not receiving cash transfers [11]. In South Africa, evidence from an observational study found that adolescent girls living in homes receiving the Child Support Grant (CSG), a national social protection cash transfer to poor households, were less likely to have engaged in transactional sex or age disparate sex [12]. In Kenya, adolescents living in homes receiving a government grant for orphans and vulnerable children were less likely to report coital debut than those who did not receive the grant [13]. There is also evidence from Kenya and Zimbabwe showing that different forms of social protection, such as provision of school uniforms or paying for school fees, can reduce the risk of pregnancy and sexual risk behaviors among vulnerable adolescent girls [14, 15].
We describe here the study design and baseline results of an individually randomized controlled trial that examines the impact of a cash transfer intervention conditioned on school attendance on HIV infection among high school adolescent girls in a rural area in northeast South Africa [HIV Prevention Trials Network study number 068 (HPTN 068)], Swa Koteka—“it is possible”. This is the first randomized controlled trial evaluating the impact of a conditional cash transfer on HIV incidence among young women.
Methods
Study Area
This study took place in the South African Medical Research Council and Wits University's Agincourt Health and Socio-Demographic Surveillance System (HDSS) site in the rural Bushbuckridge sub-district in Mpumalanga province, South Africa [16]. The study site is located 500 km northeast of Johannesburg. The area is characterized by high rates of poverty, unemployment and circular labor migration. HIV prevalence in Mpumalanga is 21.8 % among adults ages 15–49 [1] and prevalence in the study area in 2012 was 5.5 % among 15–19 year older women rising to 27 % by age 20–24 years and reaching 46 % by the time they reach the age of 35–39 years [17].
Study Population
Inclusion criteria for this study included females aged 13–20 years, enrolled in grades 8–11 within participating public schools, not married or pregnant by self-report, able to complete a computer survey on her own, having the documentation necessary to open a post office or bank account, having a parent/guardian who owns the documentation to open a post office or bank account living in the same home, intending to live within the study area until trial completion, and currently residing in one of 28 villages part of the Agincourt HDSS. Young women who tested HIV positive at baseline were eligible for study participation primarily to reduce stigma related to exclusion based on HIV status.
Study Design
This study is a phase III individually randomized trial to assess the impact of a conditional cash transfer on the acquisition of HIV among South African young women. Young women and their households were randomized in a 1:1 ratio to the intervention arm (monthly cash payments), conditional on the young woman completing 80 % school attendance, or to the control arm (no cash payments). IRB approval for this study was obtained from the University of North Carolina at Chapel Hill and the University of the Witwatersrand Human Research Ethics Committee.
Recruitment
Participants were recruited by drawing a sample of young women from the Agincourt HDSS and visiting them at their home to assess eligibility. Additionally, fliers with study information were distributed to participating schools as a mechanism to increase enrollment. Only one young woman from each household could be enrolled. If there were more than one eligible person in the household, those in grades 9 or 10 were given priority for selection as they would have more time in school and thus contribute more time to the study compared to someone in grade 11. If there were more than one young woman in grades 9 or 10 in the same household, then they were randomly selected using the “next birthday” method. The same method was used to select those in grades 8 or 11 if there were multiple young women in the household not in grade 9 or 10. Recruitment started at the house of the young woman and the study was explained to the parent/guardian and the young woman. Both parental/guardian consent and young woman consent was completed at the home for those who agreed to participate. Written assent was sought from young women under the age of 18 years.
Enrollment and Data Collection
After consent and assent forms were signed, a household socio-demographic interview was completed with the parents/guardians using Computer Assisted Personal Interview (CAPI). Upon completion of the household interview, young women were given an appointment to complete the study procedures at a ‘weekend camp’, which took place at the central study office or community venue on a Saturday, Sunday or occasional weekdays during school vacations. Young women visited stations set up in individual rooms for each study procedure. They completed an interview, administered partially by trained fieldworkers and partially by the young women themselves, using Audio Computer Assisted Self Interview (ACASI). They then underwent group pre-test counseling for HIV and herpes simplex virus type 2 (HSV-2), venous blood draw for rapid HIV testing, HSV-2 and additional HIV confirmatory testing which included CD4 for young women with suspected HIV infection (see “Methods” section), and individual post-test counseling. At the baseline visit young women were also randomized to the intervention or control arm. All young women received a small gift as appreciation at their visit worth approximately 3 USD.
Randomization
Individual randomization took place after all other study procedures at the baseline visit. Numbered, sealed envelopes containing a randomization assignment card were produced. Each village had a dedicated set of envelopes. Each envelope was allocated to one of two randomization arms (intervention or control). The envelopes were ordered numerically using block randomization. Each young woman picked an envelope from the set of envelopes specific to her village to help ensure that the process was perceived as fair and transparent. The participant was considered enrolled in the study once the envelope was assigned.
Follow Up
Young women were seen annually until the study completion date or their planned high school completion, whichever came first. Each annual study visit included an ACASI interview with the young woman, pre- and post-test counseling, a blood draw and HIV and HSV-2 testing for those who were not positive at the previous visit. A CAPI interview was also completed annually with the parent/guardian.
School Enrollment and Cash Payments
Attendance data were collected on all young women in the intervention arm each month using the official school attendance registers. Attendance data were collected on young women in the control arm 3 months of each year as a representative comparison to the intervention arm. We did not tell teachers or administrators who was in the study and attendance rosters were collected for all students. Study staff then identified study participants from the roster back at the office. If the young woman in the intervention arm attended 80 % of school days in a given month she received 100 Rand (approximately 12 USD) and her parent/guardian received 200 Rand (approximately 24 USD), deposited directly into their respective bank accounts. If the young woman was allocated to the control arm she received no cash payments.
Outcomes
HIV incidence was the primary endpoint for the trial. HIV testing was performed at enrollment, and at 12, 24, and 36 month visits. At the study site, screening for HIV infection was performed using Determine™ HIV-1/2 (Alere Medical Co.,Ltd, Matsudo-shi, Chiba, Japan) and FDA cleared Uni-gold™ Recombigen® HIV (Trinity Biotech plc, Bray, Co. Wicklow, Ireland) rapid tests in parallel. If both HIV rapid tests were non-reactive, no further testing was done at that study visit. If one or both of the HIV rapid tests was reactive, a CD4 cell count was performed, utilizing the CD4 BECTON–DICKINSON (BD) FACSCALIBUR TRUCOUNT Method (Becton, Dickinson and Company, BD Biosciences, San Jose, California USA) and confirmatory HIV testing was performed using FDA cleared GS HIV-1 WESTERN BLOT assay (Bio-Rad Laboratories, Inc. Redmond Washington, USA). If the Western blot was positive or indeterminate, a second Western blot was performed using a new blood sample collected at a second scheduled visit within 2 weeks of the first test result. If a participant was confirmed to be HIV-infected (if both Western blot tests were positive), no further HIV testing was done at follow-up visits, but blood was collected for a CD4 cell count test. If HIV status was not clear, further testing was performed with guidance from the HPTN Laboratory Center. Additional HIV testing was performed retrospectively at the HPTN Laboratory Center to confirm baseline HIV status and incident infections.
HSV-2 incidence was a secondary endpoint for the trial. HSV-2 testing was performed at enrollment, and at 12, 24, and 36 month visits. HSV-2 testing was performed using the Herpes Simplex Virus Type 2 IgG ELISA assay, (Kalon Biological, LTD Guildford, UK), with an index cut-off of 1.5. If the HSV-2 test was positive, no further HSV-2 testing was done at the study site at follow-up visits. HSV-2 results were confirmed retrospectively at the HPTN Laboratory Center.
Other secondary behavioral endpoints were collected using Questionnaire Development Software (QDS). Questionnaires were completed by the young woman herself using ACASI for sensitive questions (e.g. sexual behavior, mental health) and by a trained fieldworker using CAPI for questions that were not deemed sensitive (e.g. education history). Key secondary outcomes, collected via ACASI, included number of self-reported vaginal sex acts by the young woman in the past 3 months, number of sex partners in the last 12 months reported by the young woman, age difference between the young woman and any of the last 3 partners, coital debut of the young woman, incident pregnancy, and school attendance as determined from school attendance rosters.
Additional outcomes of interest were collected using CAPI and ACASI including HIV knowledge, sexual history, partner concurrency, intimate partner violence (IPV), educational history and attitudes, fertility and contraception history, employment and finances, consumption patterns, mental health, alcohol and drug abuse, and parent/guardian caregiving. Depression was measured using the Children's Depression Index (CDI), we used the short form as has been used previously among adolescents in South Africa and performed well [18]. The scale includes 10 items scored 0, 1, 2 and the range was 0–20. A cut off of ≥7 was indicative of depression. IPV was measured using the WHO violence against women instrument [19]. HIV knowledge was used with six questions adapted from a scale used in South Africa previously and included questions such as “You can get HIV if you share utensils with someone who is infected” and “You cannot get HIV from kissing a person who is HIV-positive” [20].
The household questionnaire, completed entirely using CAPI, included detailed information on socio-economic status including household consumption and expenditures as well as household assets.
Sample Size
The sample size required for the study was 2430 HIV negative young women, estimating that the HIV prevalence among the study population would be 4 % and HIV incidence would be 3 %. We estimated there would be approximately 1822 young women in grades 8, 9 and 10 who would be eligible (HIV-uninfected, ages 13–20) for the cash transfer intervention and an additional 608 women (HIV-uninfected, ages 13–20) in grade 11. Under the following four assumptions it was estimated that with 3 % HIV incidence we would have 84 % power to detect a 40 % effect (RR = 0.6). We assumed that: (1) young women in grades 8–10 would be followed for 3 years; (2) young women in grade 11 be followed for 2 years; (3) the study loss to follow up rate would be 5 % per year and; (4) half of the young women would be randomized to the control arm and half to the CCT arm.
Analysis
In this baseline analysis, we describe the distribution of primary outcomes, secondary outcomes, and important covariates that capture individual-, household-, partner-, and schooling factors within the full sample and by study arm. Using logistic regression models, we estimated odds ratios for the association between important covariates for each of these four key factors and prevalent HIV and HSV-2 infection. We controlled for potential confounding effects of age, with categorical variables for each 1-year age increment.
We also created dichotomous variables as indicators for risk for each of the four factors: individual, household, partner and schooling. Young women were categorized as having individual-level risk if they reported at least one of the following: any alcohol consumption, sex while drunk/on drugs, no condom use at last sex with at least one of last three partners, or multiple lifetime sex partners. Young women were categorized as having household-level risk if they reported at least one of the following: orphanhood, primary caregiver was non-parent, or lowest asset index quartile. Young women were categorized as having partner-level risk if they reported at least one of the following: any of last three partners were five or more years older, transactional sex with any of last three partners, or any of last three partners had other partners. Young women were categorized as having schooling related risk factors if they reported either of the following: repeated grade or missing more than 20 % of school days in a typical month. To compare the relative magnitude of HIV and HSV-2 prevalence at each level, we used logistic regression models to estimate odds ratios. To compare the relative importance of combinations of risk at different levels (e.g., household- and schooling-related risk together), we compared HIV and HSV-2 prevalence in each of the sixteen possible combinations, estimated from log-linear regression models. In order to adjust for potential type 1 error that can result from multiple comparisons, we have indicated in Tables 3 and 5 those associations that would remain significant after the Bonferroni adjustment for multiple comparisons. Between Tables 3 and 5 there are a total of 100 adjusted comparisons so any p value significant at the 0.0005 level would be significant and are indicated as such in the tables.
Table 3.
Relationship between baseline covariates and prevalent HIV and HSV-2 infection at among 2533 young women enrolled in HPTN 068 at baseline in Agincourt, South Africa March 2011–December 2012
| HIV |
HSV-2 |
|||||||
|---|---|---|---|---|---|---|---|---|
| OR (95 % CI) | p | aOR (95 % CI)a | p | OR (95 % CI) | p | aOR (95 % CI)a | p | |
| Individual | ||||||||
| Age | 1.31 (1.16–1.49) | <0.0001 | – | 1.74 (1.55–1.95) | <0.0001 | – | ||
| Ever pregnant | ||||||||
| Yes | 2.95 (1.69–5.13) | 0.0001 | 1.81 (0.97–3.40) | 0.06 | 4.83 (3.12–7.48) | <0.0001 | 2.07 (1.28–3.35) | 0.003 |
| No | 1 | 1 | 1 | 1 | ||||
| Ever vaginal sex | ||||||||
| Yes | 2.94 (1.89–1.59) | <0.0001 | 2.30 (1.37–3.85) | 0.002* | 7.57 (4.97–11.54) | <0.0001 | 4.11 (2.60–6.49) | <0.0001* |
| No | 1 | 1 | 1 | 1 | ||||
| Ever anal sex | ||||||||
| Yes | 1.95 (0.88–1.33) | 0.1 | 1.53 (0.68–3.46) | 0.3 | 3.43 (1.92–6.11) | <0.0001 | 2.19 (1.20–3.99) | 0.01 |
| No | 1 | 1 | 1 | 1 | ||||
| Early age of debut (<15 years) | ||||||||
| Yes | 2.05 (1.04–4.06) | 0.04 | 1.95 (0.98–3.89) | 0.06 | 2.15 (1.20–3.86) | 0.01 | 2.03 (1.10–3.72) | 0.02 |
| No | 1 | 1 | 1 | 1 | ||||
| Lifetime sex partners | ||||||||
| 0 | 1 | 1 | 1 | 1 | ||||
| 1 | 2.24 (1.24–4.07) | 0.008 | 1.93 (1.02–3.67) | 0.04 | 4.38 (2.53–7.58) | <0.0001 | 2.65 (1.48–1.71) | 0.001 |
| 2+ | 4.29 (2.58–7.14) | <0.0001 | 3.38 (1.86–6.12) | <0.0001* | 12.32 (7.75–19.57) | <0.0001 | 6.49 (3.90–10.82) | <0.0001* |
| Unprotected vaginal sex actsb | ||||||||
| None | 1 | 1 | 1 | 1 | ||||
| Any | 0.87 (0.41–1.82) | 0.7 | 0.69 (0.32–1.48) | 0.3 | 1.41 (0.85–2.35) | 0.2 | 1.16 (0.68–1.96) | 0.6 |
| Condom use at last sexb | ||||||||
| Yes | 1 | 1 | 1 | 1 | ||||
| No | 1.88 (0.97–3.64) | 0.06 | 1.77 (0.90–3.47) | 0.1 | 1.81 (1.11–2.94) | 0.02 | 1.67 (1.01–2.76) | 0.05 |
| Alcohol consumption | ||||||||
| High (at least once/month) | 1.16 (0.28–1.85) | 0.1 | 1.12 (0.27–1.73) | 0.2 | 2.85 (1.19–6.81) | 0.03 | 2.64 (1.07–6.55) | 0.04 |
| Low (up to once/month) | 1.81 (0.89–3.68) | 0.8 | 1.60 (0.78–3.31) | 0.9 | 1.99 (1.09–3.64) | 0.02 | 1.55 (0.83–2.88) | 0.2 |
| None | 1 | 1 | 1 | 1 | ||||
| Sex while drunk/on drugsb | ||||||||
| Yes | 1.27 (0.44–3.70) | 0.7 | 1.35 (0.46–3.99) | 0.6 | 1.43 (0.65–3.15) | 0.4 | 1.58 (0.70–3.56) | 0.3 |
| No | 1 | 1 | 1 | 1 | ||||
| Depressionc | ||||||||
| CDI ≥ 7 | 1.62 (0.97–2.70) | 0.06 | 1.39 (0.83–2.35) | 0.2 | 2.40 (1.58–3.65) | <0.0001 | 1.86 (1.20–2.88) | 0.005 |
| CDI < 7 | 1 | 1 | 1 | 1 | ||||
| HIV knowledged | 0.85 (0.73–0.99) | 0.04 | 0.83 (0.71–0.98) | 0.02 | 1.16 (1.02–1.33) | 0.03 | 1.13 (0.99–1.30) | 0.08 |
| Using birth controlb | ||||||||
| Yes | 1.48 (0.78–2.83) | 0.2 | 1.16 (0.59–2.27) | 0.7 | 1.38 (0.85–2.23) | 0.2 | 1.05 (0.63–1.73) | 0.9 |
| No | 1 | 1 | 1 | 1 | ||||
| Importance of not getting pregnant now | ||||||||
| Not important | 0.85 (0.51–1.43) | 0.6 | 0.92 (0.55–1.55) | 0.8 | 0.64 (0.40–1.05) | 0.08 | 0.77 (0.47–1.26) | 0.3 |
| Somewhat important | 1.29 (0.60–2.77) | 0.5 | 1.14 (0.53–2.48) | 0.7 | 2.35 (1.38–3.99) | 0.002 | 1.95 (1.12–3.40) | 0.02 |
| Very important | 1 | 1 | 1 | 1 | ||||
| Chance of HIV, lifetime | ||||||||
| No chance | 1 | 1 | 1 | 1 | ||||
| Some/high chance | 1.90 (1.20–3.02) | 0.006 | 1.73 (1.08–2.77) | 0.02 | 1.77 (1.19–2.62) | 0.005 | 1.44 (0.96–2.17) | 0.08 |
| Home/parent | ||||||||
| Household sizee | 0.88 (0.80–0.98) | 0.02 | 0.87 (0.79–0.97) | 0.009 | 0.94 (0.87–1.02) | 0.2 | 0.93 (0.86–1.01) | 0.07 |
| Orphan | ||||||||
| Both parents alive | 1 | 1 | 1 | 1 | ||||
| Single orphan | 1.80 (1.07–3.05) | 0.03 | 1.68 (0.99–2.85) | 0.06 | 1.17 (0.76–1.80) | 0.09 | 1.17 (0.76–1.81) | 0.2 |
| Double orphan | 5.87 (3.09–11.15) | <0.0001 | 5.48 (2.85–10.54) | <0.0001* | 1.33 (0.60–2.90) | 0.3 | 1.35 (0.62–2.94) | 0.5 |
| Parents at home | ||||||||
| Both parents | 1 | 1 | 1 | 1 | ||||
| Mother only | 1.16 (0.64–2.11) | 0.6 | 1.14 (0.63–2.08) | 0.7 | 1.89 (1.15–3.11) | 0.01 | 1.91 (1.14–3.20) | 0.01 |
| Father only | 1.58 (0.46–5.41) | 0.5 | 1.46 (0.42–5.09) | 0.5 | 2.70 (1.07–6.79) | 0.04 | 2.51 (0.97–6.54) | 0.06 |
| Neither parents | 2.91 (1.65–5.14) | 0.0002 | 2.78 (1.57–1.95) | 0.0005* | 2.39 (1.39–1.11) | 0.002 | 2.29 (1.31–1.00) | 0.004 |
| Maternal education | ||||||||
| Not secondary school graduate | 1.02 (0.61–1.73) | 0.9 | 0.85 (0.50–1.46) | 0.6 | 1.57 (0.97–2.56) | 0.07 | 1.14 (0.69–1.89) | 0.6 |
| Secondary school graduate | 1 | 1 | 1 | 1 | ||||
| Primary caregiver | ||||||||
| Parent | 1 | 1 | 1 | 1 | ||||
| Non-parent | 2.24 (1.43–3.51) | 0.0004 | 2.20 (1.40–3.46) | 0.0007 | 1.64 (1.10–2.44) | 0.02 | 1.64 (1.09–2.47) | 0.02 |
| Caregiver sick (bed-ridden)f | ||||||||
| Yes | 1.68 (0.67–1.26) | 0.3 | 1.89 (0.74–1.82) | 0.2 | 0.93 (0.34–2.59) | 0.9 | 1.08 (0.38–3.05) | 0.9 |
| No | 1 | 1 | 1 | |||||
| Food insecurityg | ||||||||
| Yes | 1.29 (0.82–2.03) | 0.3 | 1.16 (0.73–1.84) | 0.5 | 1.52 (1.03–2.23) | 0.03 | 1.25 (0.84–1.86) | 0.3 |
| No | 1 | 1 | 1 | 1 | ||||
| Assetsh | ||||||||
| Quartile 1 | 2.03 (1.01–4.06) | 0.05 | 1.87 (0.93–3.76) | 0.08 | 2.43 (1.37–4.31) | 0.002 | 2.09 (1.16–3.75) | 0.01 |
| Quartile 2 | 1.79 (0.89–3.61) | 0.1 | 1.70 (0.84–3.45) | 0.1 | 1.37 (0.74–2.56) | 0.3 | 1.24 (0.66–2.33) | 0.5 |
| Quartile 3 | 1.54 (0.74–3.21) | 0.2 | 1.46 (0.70–3.04) | 0.3 | 1.50 (0.81–2.80) | 0.2 | 1.35 (0.71–2.54) | 0.4 |
| Quartile 4 | 1 | 1 | 1 | 1 | ||||
| Partner | ||||||||
| Age difference with partnerb,i | ||||||||
| ≥5 years older | 2.09 (1.07–4.07) | 0.03 | 2.46 (1.24–4.90) | 0.01 | 2.05 (1.22–3.44) | 0.007 | 2.50 (1.45–4.30) | 0.0009 |
| <5 years older | 1 | 1 | 1 | 1 | ||||
| Partner has other partnersb,i | ||||||||
| Yes | 1.54 (0.71–3.35) | 0.3 | 1.39 (0.63–3.07) | 0.4 | 1.54 (0.84–2.80) | 0.2 | 1.37 (0.74–2.54) | 0.3 |
| No | 1 | 1 | 1 | 1 | ||||
| Don't know | 0.67 (0.25–1.85) | 0.4 | 0.64 (0.23–1.78) | 0.4 | 0.98 (0.48–1.99) | 1.0 | 0.90 (0.43–1.86) | 0.8 |
| Partner gave money or giftsb,i | ||||||||
| Yes | 2.50 (0.76–8.25) | 0.1 | 2.20 (0.66–7.35) | 0.2 | 1.51 (0.73–3.11) | 0.3 | 1.29 (0.61–2.72) | 0.5 |
| No | 1 | 1 | 1 | 1 | ||||
| Transactional sexb,i | ||||||||
| Yes | 2.52 (1.25–5.09) | 0.01 | 2.60 (1.27–5.36) | 0.009 | 1.17 (0.62–2.22) | 0.6 | 1.14 (0.59–2.20) | 0.7 |
| No | 1 | 1 | 1 | 1 | ||||
| Concurrent relationshipb,j | ||||||||
| Yes | 1.16 (0.54–2.48) | 0.7 | 1.01 (0.47–2.21) | 1.0 | 1.87 (1.11–3.18) | 0.02 | 1.66 (0.96–2.87) | 0.07 |
| No | 1 | 1 | 1 | 1 | ||||
| Ever physical abuse | ||||||||
| Yes | 1.61 (0.96–2.69) | 0.07 | 1.26 (0.74–2.15) | 0.4 | 1.93 (1.26–2.97) | 0.003 | 1.24 (0.79–1.94) | 0.3 |
| No | 1 | 1 | 1 | 1 | ||||
| Ever sexual abuse | ||||||||
| Yes | 1.49 (0.78–2.86) | 0.2 | 1.36 (0.70–2.63) | 0.4 | 1.12 (0.61–2.07) | 0.7 | 0.90 (0.48–1.70) | 0.7 |
| No | 1 | 1 | 1 | 1 | ||||
| School | ||||||||
| Grade enrollment | ||||||||
| Grade 8 | 1 | 1 | 1 | 1 | ||||
| Grade 9 | 0.50 (0.25–0.99) | 0.05 | 0.35 (0.17–0.75) | 0.006 | 1.11 (0.50–2.51) | 0.8 | 0.59 (0.24–1.40) | 0.2 |
| Grade 10 | 0.79 (0.44–1.44) | 0.4 | 0.34 (0.16–0.72) | 0.005 | 3.77 (1.93–7.38) | 0.0001 | 0.94 (0.42–2.07) | 0.9 |
| Grade 11 | 1.20 (0.67–2.16) | 0.5 | 9.34 (0.15–0.78) | 0.01 | 5.53 (2.83–10.81) | <0.0001 | 0.90 (0.39–2.07) | 0.8 |
| Age for grade | ||||||||
| Older than expected age | 2.44 (1.56–3.80) | <0.0001 | 1.54 (0.80–2.96) | 0.2 | 3.58 (2.43–5.27) | <0.0001 | 0.98 (0.57–1.68) | 0.9 |
| Expected age or younger | 1 | 1 | 1 | |||||
| Repeated grade | ||||||||
| Yes | 2.80 (1.78–4.39) | <0.0001 | 2.17 (1.25–3.79) | 0.006 | 3.28 (2.22–4.86) | <0.0001 | 1.26 (0.80–2.00) | 0.3 |
| No | 1 | 1 | 1 | 1 | ||||
| School days missed per month | ||||||||
| 0–4 days | 1 | 1 | 1 | 1 | ||||
| 5+ days | 2.69 (1.42–5.08) | 0.002 | 2.07 (1.07–4.01) | 0.03 | 2.78 (1.62–4.79) | 0.0002 | 1.72 (0.97–3.06) | 0.06 |
| Chance of school until matric | ||||||||
| No chance | 1.90 (0.58–6.29) | 0.3 | 1.83 (0.55–6.13) | 0.3 | 1.89 (0.74–4.86) | 0.2 | 1.93 (0.72–5.22) | 0.2 |
| Some chance | 1.51 (0.94–2.41) | 0.09 | 1.42 (0.88–2.29) | 0.1 | 0.68 (0.42–1.09) | 0.1 | 0.59 (0.36–0.95) | 0.03 |
| A high chance | 1 | 1 | 1 | 1 | ||||
An asterisk (*) following a p value indicates that this result would be significant at the 0.05 level after Bonferroni adjustment for multiple comparisons (adjusted models only—100 comparisons are reported in Tables 3 and 5)
Age-adjusted ORs, coding age categorically with a dummy variable for every year
Among sexually active, as defined by self-reported vaginal or anal sex history (n = 693)
Children's depression inventory measured with a 10 item scale with each item assigned a numerical value from 0 to 2 with the higher value assigned to more clinically severe behavior. Those with a score of 3 or above are categorized as depressed
HIV knowledge measured with an index of correct answers for six general HIV knowledge questions—incorrect answers and ‘don't know’ responses were coded as ‘0’. Odds ratios estimate the effect of each one-unit increase in HIV knowledge score
Odds ratios estimate the effect of each one-person increase in household size
In the last 30 days
Worried about having enough food in the last 12 months
Household asset index constructed by adding up number of working assets reported in the household across a range of assets: radio, stereo, television, satellite dish, etc
Among any of last three partners
Concurrency defined as at least two of the last three most recent relationships reported as ongoing
Table 5.
Relationship between risk factors at the individual-, household-, partner-, and school-level and prevalent HIV and HSV-2 infection, among young women enrolled in HPTN 068 at baseline in Agincourt, South Africa March 2011–December 2012
| HIV |
HSV-2 |
|||||||
|---|---|---|---|---|---|---|---|---|
| OR (95 % CI) | p | aOR (95 % CI)a | p | OR (95 % CI) | p | aOR (95 % CI)a | p | |
| Individual risk factorsb | ||||||||
| Yes | 2.87 (1.83–1.49) | <0.0001 | 2.30 (1.40–3.77) | 0.001 | 5.46 (3.66–8.15) | <0.0001 | 3.12 (2.03–4.78) | <0.0001* |
| No | 1 | 1 | 1 | 1 | ||||
| Household risk factorsc | ||||||||
| Yes | 2.30 (1.37–3.84) | 0.002 | 2.21 (1.32–3.71) | 0.003 | 1.99 (1.30–3.04) | 0.002 | 1.92 (1.24–2.97) | 0.003 |
| No | 1 | 1 | 1 | 1 | ||||
| Partner risk factorsd | ||||||||
| Yes | 3.76 (2.39–5.91) | <0.0001 | 3.05 (1.84–5.06) | <0.0001* | 6.84 (4.62–10.13) | <0.0001 | 3.84 (2.52–5.85) | <0.0001* |
| No | 1 | 1 | 1 | 1 | ||||
| School risk factorse | ||||||||
| Yes | 2.86 (1.81–1.53) | <0.0001* | 2.28 (1.32–3.95) | 0.003 | 3.38 (2.26–5.04) | <0.0001* | 1.35 (0.85–2.15) | 0.2 |
| No | 1 | 1 | 1 | 1 | ||||
An asterisk (*) following a p-value indicates that this result would be significant at the 0.05 level after Bonferroni adjustment for multiple comparisons (adjusted models only—100 comparisons are reported in Tables 3 and 5)
Age-adjusted ORs, coding age categorically with a dummy variable for every year
Reports at least one of the following risk factors: 1. No condom use at last sex with at least one of last three partners, 2. Multiple lifetime sex partners, 3. Any alcohol consumption, 4. Ever sex while drunk, 5. Ever sex while on drugs
Reports at least one of the following risk factors: 1. Single or double orphanhood, 2. Primary caregiver is non-parent, 3. Lowest asset quartile
Reports at least one of the following risk factors: 1. Older partner (by 5 or more years), 2. Transactional sex with at least one of last three partners, 3. Partner has other partners
Reports at least one of the following risk factors: 1. Repeated grade, 2. Miss >20 % school days in typical school week
Results
Screening took place between March of 2011 and December of 2012. Of the 10,134 young women screened using the AHDSS as the sampling frame, 2537 were enrolled. Of the 7597 not enrolled, the most frequent reason for ineligibility included not being enrolled in school or not in grades 8–11 (45 %) (Table 1). Refusal was not common, 5 % of parent/guardians and 2 % of young women refused participation.
Table 1.
Reasons for ineligibility among 7597 young women screened but not enrolled in HPTN 068, Agincourt, South Africa March 2011–December 2012
| N | % | |
|---|---|---|
| YW not in school, not in correct grade or participating schools | 3387 | 45 |
| Did not have a reason reported for ineligibility | 1486 | 20 |
| YW did not live in the home where the census had them registered | 748 | 10 |
| Someone else in the home already enrolled | 482 | 6 |
| P/G refused | 386 | 5 |
| YW refused | 127 | 2 |
| No parent/guardian in home | 224 | 3 |
| YW was not 13–20 years of age | 201 | 3 |
| YW/PG doesn't have documentation to open up account | 153 | 2 |
| YW were married | 74 | 1 |
| Unable to locate home or young woman | 105 | 1 |
| YW are pregnant | 53 | 1 |
| YW recorded in census as duplicate | 41 | 1 |
| YW already enrolled in study | 38 | 1 |
| YW were pre-screening eligible but not screening eligible | 26 | <1 |
| YW were deceased | 15 | <1 |
| Identified YW is male | 13 | <1 |
| YW can't read | 10 | <1 |
| YW/P/G disabled/mentally ill | 6 | <1 |
| YW planned to move outside the DSS | 4 | <1 |
| Eligible but not enrolled | 18 | <1 |
| Total | 7597 | 100 |
Individual Characteristics
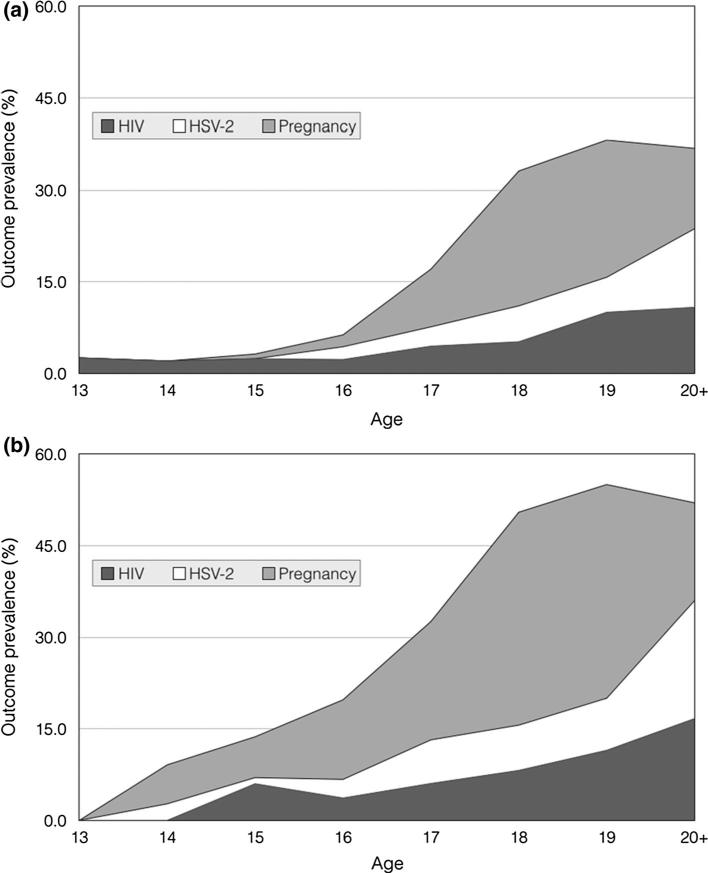
The median age in the cohort at baseline was 15 years (IQR 14–17). HIV prevalence at baseline was 3.2 % (n = 81) (95 % CI 2.6–4.0 %) and HSV-2 was 4.4 % (n = 112) (95 % CI 3.7–5.3 %) and 8.9 % (n = 223) (95 % CI 7.9–10.1 %) of young women reported having previously been pregnant. Among those who reported ever having had sex (27.4 %), HIV, HSV-2 and prior pregnancy prevalence were 6.2 % (95 % CI 4.7–8.3 %), 11.7 % (95 % CI 9.6–14.4 %), and 30.6 % (95 % CI 27.3–34.3 %), respectively. Figure 1 presents the prevalence of HIV, HSV-2 and prior pregnancy among the whole cohort and restricted to those sexually active, by age.
Fig. 1.
Prevalence of HIV, HSV-2 and prior pregnancy, by age at baseline among young women enrolled in HPTN 068, Agincourt, South Africa, March 2011–December 2012. a Among full sample (n = 2533) and b among sexually active (n = 693)
Baseline socio-demographic and HIV risk behaviors are reported in Table 2. More than a quarter of young women (26.6 %) reported ever having had vaginal sex; 6.6 % before the age of 15, and 12.9 % reported more than one lifetime sexual partner. Among those with vaginal or anal sex experience (n = 693), less than half (47.5 %) reported using a condom the last time they had sex and 28.2 % reported at least one unprotected sex acts in the past 3 months. Among these sexually experienced young women, over half (56.3 %) reported using birth control. Among all young women, just under a third (29.9 %) said it was ‘not important’ if they got pregnant now.
Table 2.
Baseline covariates, by study arm, among 2533 young women enrolled in HPTN 068, Agincourt, South Africa March 2011–December 2012
| Total (n = 2533) N (%) or median (IQR) | Arm = 1(n = 1261) N (%) or median (IQR) | Arm = 0(n= 1272) N (%) or median (IQR) | |
|---|---|---|---|
| Individual | |||
| Age | 15 (14–17) | 15 (14–17) | 15 (14–17) |
| HIV | |||
| Positive | 81 (3.2) | 36 (2.9) | 45 (3.6) |
| Negative | 2448 (96.8) | 1225 (97.2) | 1223 (96.5) |
| Missing | 4 | 0 | 4 |
| HSV-2 | |||
| Positive | 112 (4.4) | 55 (4.4) | 57 (4.5) |
| Negative | 2413 (95.6) | 1202 (95.6) | 1211 (95.5) |
| Missing | 8 | 4 | 4 |
| Ever pregnant | |||
| Yes | 223 (8.9) | 110 (8.8) | 113 (9.0) |
| No | 2279 (91.1) | 1138 (91.2) | 1141 (91.0) |
| Missing | 31 | 13 | 18 |
| Ever vaginal sex | |||
| Yes | 672 (26.6) | 334 (26.6) | 338 (26.7) |
| No | 1851 (73.4) | 924 (73.5) | 927 (73.3) |
| Missing | 10 | 3 | 7 |
| Ever anal sex | |||
| Yes | 120 (4.8) | 61 (4.9) | 59 (4.7) |
| No | 2408 (95.3) | 1197 (95.2) | 1211 (95.4) |
| Missing | 5 | 3 | 2 |
| Early age of debut (<15 years) | |||
| Yes | 166 (6.6) | 85 (6.8) | 81 (6.4) |
| No | 2347 (93.4) | 1170 (93.2) | 1177 (93.6) |
| Missing | 20 | 6 | 14 |
| Lifetime sex partners | |||
| 0 | 1830 (73.0) | 916 (73.3) | 914 (72.8) |
| 1 | 353 (14.1) | 163 (13.0) | 190 (15.1) |
| 2+ | 323 (12.9) | 171 (13.7) | 152 (12.1) |
| Missing | 27 | 11 | 16 |
| Unprotected vaginal sex actsa | |||
| 0 | 481 (71.8) | 228 (69.3) | 253 (74.2) |
| 1 | 80 (11.9) | 42 (12.8) | 38 (11.1) |
| 2 | 47 (7.0) | 27 (8.2) | 20 (5.9) |
| 3+ | 62 (9.3) | 32 (9.7) | 30 (8.8) |
| Missing | 23 | 12 | 11 |
| Condom use at last sexa | |||
| Yes | 321 (47.5) | 158 (47.7) | 163 (47.3) |
| No | 355 (52.5) | 173 (52.3) | 182 (52.8) |
| Missing | 17 | 10 | 7 |
| How often drink alcohol | |||
| Never | 2301 (91.1) | 1131 (90.0) | 1170 (92.2) |
| Up to once a month | 168 (6.7) | 93 (7.4) | 75 (5.9) |
| More than once a month | 57 (2.3) | 33 (2.6) | 24 (1.9) |
| Missing | 7 | 4 | 3 |
| Sex while drunk/on drugsa | |||
| Yes | 52 (7.6) | 24 (7.1) | 28 (8.0) |
| No | 634 (92.4) | 313 (92.9) | 321 (92.0) |
| Missing | 7 | 4 | 3 |
| Children's depression inventory2 | |||
| CDI < 7 | 1954 (81.3) | 961 (80.2) | 993 (82.3) |
| CDI ≥ 7 | 451 (18.8) | 237 (19.8) | 214 (17.7) |
| Missing | 128 | 63 | 65 |
| HIV knowledge scorec | |||
| All correct (6) | 80 (3.2) | 39 (3.1) | 41 (3.2) |
| More than 50 % correct (4–5) | 912 (36.2) | 455 (36.3) | 457 (36.1) |
| Less than or equal to 50 % correct (0–3) | 1527 (60.6) | 759 (60.6) | 768 (60.7) |
| Missing | 14 | 8 | 6 |
| Using birth controla | |||
| Yes | 387 (56.3) | 184 (54.1) | 203 (58.3) |
| No | 301 (43.8) | 156 (45.9) | 145 (41.7) |
| Missing | 5 | 1 | 4 |
| Importance of not getting pregnant now | |||
| Not important | 753 (29.9) | 379 (30.3) | 374 (29.6) |
| Somewhat important | 192 (7.6) | 98 (7.8) | 94 (7.4) |
| Very important | 1571 (62.4) | 775 (61.9) | 796 (63.0) |
| Missing | 17 | 9 | 8 |
| Chance of getting HIV, lifetime | |||
| No chance | 1842 (73.9) | 915 (74.0) | 927 (73.7) |
| Some chance | 449 (18.0) | 216 (17.5) | 233 (18.5) |
| A very high chance | 203 (8.1) | 105 (8.5) | 98 (7.8) |
| Missing | 39 | 25 | 14 |
| Home/parent | |||
| Household size | 6 (4–7) | 6 (4–8) | 6 (4–7) |
| Missing | 1 | 1 | 0 |
| Orphan | |||
| Both parents alive | 1723 (71.4) | 850 (70.9) | 873 (71.8) |
| Single orphan | 575 (23.8) | 287 (23.9) | 288 (23.7) |
| Double orphan | 117 (4.8) | 62 (5.2) | 55 (4.5) |
| Missing | 118 | 62 | 56 |
| Parents at home | |||
| Both parents | 914 (36.4) | 448 (35.8) | 466 (37.0) |
| Mother only | 986 (39.2) | 479 (38.2) | 507 (40.2) |
| Father only | 88 (3.5) | 49 (3.9) | 39 (3.1) |
| Neither parents | 526 (20.9) | 277 (22.1) | 249 (19.8) |
| Missing | 19 | 8 | 11 |
| Maternal education | |||
| Not HS graduate | 1681 (72.4) | 849 (73.1) | 832 (71.7) |
| HS graduate | 640 (27.6) | 312 (26.9) | 328 (28.3) |
| Missing | 212 | 100 | 112 |
| Primary caregiver | |||
| Mother | 1664 (65.8) | 813 (64.5) | 851 (67.0) |
| Father | 206 (8.1) | 107 (8.5) | 99 (7.8) |
| Grandparent | 359 (14.2) | 191 (15.2) | 168 (13.2) |
| Sibling | 169 (6.7) | 74 (5.9) | 95 (7.5) |
| Aunt/uncle | 104 (4.1) | 58 (4.6) | 46 (3.6) |
| Other | 26 (1.0) | 16 (1.3) | 10 (0.8) |
| Missing | 5 | 2 | 3 |
| Primary caregiver sickd | |||
| Yes, bed-ridden | 97 (3.8) | 46 (3.7) | 51 (4.0) |
| Yes, not bed-ridden | 287 (11.3) | 140 (11.1) | 147 (11.6) |
| No | 2146 (84.8) | 1073 (85.2) | 1073 (84.4) |
| Missing | 3 | 2 | 1 |
| Food insecuritye | |||
| Yes | 862 (34.3) | 412 (32.9) | 450 (35.7) |
| No | 1649 (65.7) | 839 (67.1) | 810 (64.3) |
| Missing | 22 | 10 | 12 |
| Assetsf | |||
| Quartile 1 | 645 (25.5) | 325 (25.8) | 320 (25.2) |
| Quartile 2 | 672 (26.6) | 329 (26.1) | 343 (27.1) |
| Quartile 3 | 616 (24.4) | 313 (24.9) | 303 (23.9) |
| Quartile 4 | 594 (23.5) | 292 (23.2) | 302 (23.8) |
| Missing | 6 | 2 | 4 |
| Partner | |||
| Age difference with partnera,g | |||
| ≥5 years older | 133 (19.7) | 64 (19.1) | 69 (20.2) |
| <5 years older | 544 (80.4) | 272 (81.0) | 272 (79.8) |
| Missing | 16 | 5 | 11 |
| Partner has other partnersa,g | |||
| Yes | 333 (48.4) | 164 (48.7) | 169 (48.2) |
| No | 166 (24.1) | 71 (21.1) | 95 (27.1) |
| Don't know | 189 (27.5) | 102 (30.3) | 87 (24.8) |
| Missing | 5 | 4 | 1 |
| Partner gave money or giftsa,g | |||
| Yes | 584 (84.8) | 286 (84.1) | 298 (85.4) |
| No | 105 (15.2) | 54 (15.9) | 51 (14.6) |
| Missing | 4 | 1 | 3 |
| Transactional sexa,g | |||
| Yes | 97 (14.2) | 45 (13.4) | 52 (15.1) |
| No | 585 (85.8) | 292 (86.7) | 293 (84.9) |
| Missing | 11 | 4 | 7 |
| Concurrent relationshipsa,h | |||
| Yes | 131 (19.2) | 67 (20.0) | 64 (18.4) |
| No | 551 (80.8) | 268 (80.0) | 283 (81.6) |
| Missing | 11 | 6 | 5 |
| Ever physical abuse | |||
| Yes | 431 (17.4) | 227 (18.4) | 204 (16.4) |
| No | 2043 (82.6) | 1005 (81.6) | 1038 (83.6) |
| Missing | 59 | 29 | 30 |
| Ever sexual abuse | |||
| Yes | 244 (9.8) | 106 (8.5) | 138 (11.0) |
| No | 2252 (90.2) | 1139 (91.5) | 1113 (89.0) |
| Missing | 37 | 16 | 21 |
| School | |||
| Grade enrollment | |||
| Grade 8 | 640 (25.3) | 322 (25.5) | 318 (25.0) |
| Grade 9 | 682 (26.9) | 327 (25.9) | 355 (27.9) |
| Grade 10 | 699 (27.6) | 354 (28.1) | 345 (27.1) |
| Grade 11 | 512 (20.2) | 258 (20.5) | 254 (20.0) |
| Missing | 0 | 0 | 0 |
| Age for grade | |||
| Expected age or younger | 1792 (70.8) | 884 (70.1) | 908 (71.4) |
| Older than expected age | 741 (29.3) | 377 (29.9) | 364 (28.6) |
| Missing | 0 | 0 | 0 |
| Repeated grade | |||
| Yes | 887 (35.0) | 445 (35.3) | 442 (34.8) |
| No | 1645 (65.0) | 815 (64.7) | 830 (65.3) |
| Missing | 1 | 1 | 0 |
| School days missed per month | |||
| 0–1 days | 2345 (93.4) | 1160 (93.3) | 1185 (93.5) |
| 5+ days | 166 (6.6) | 84 (6.8) | 82 (6.5) |
| Missing | 22 | 17 | 5 |
| Chance of school until matric | |||
| No chance | 58 (2.3) | 33 (2.6) | 25 (2.0) |
| Some chance | 676 (26.7) | 336 (26.7) | 340 (26.8) |
| A high chance | 1797 (71.0) | 892 (70.7) | 905 (71.3) |
| Missing | 2 | 0 | 2 |
Among sexually active, as defined by self-reported vaginal or anal sex history (n = 693)
b Children's depression inventory measured with a 10 item scale with each item assigned a numerical value from 0 to 2 with the higher value assigned to more clinically severe behavior. Those with a score of 7 or above are categorized as depressed
Index of correct answers for six general HIV knowledge questions—incorrect answers and don't know responses were coded as ‘0’
In the last 30 days
Worried about having enough food in the last 12 months
Household asset index constructed by adding up number of working assets reported in the household across a range of assets: radio, stereo, television, satellite dish, etc
Among any of last three partners
Concurrency defined as at least two of the last three most recent relationships reported as ongoing
Nearly one-fifth (18.8 %) of young women reported symptoms of depression in the Children's Depression Inventory. A small percentage of young women reported drinking alcohol more than once a month (2.3 %) and among those with sexual experience, 7.6 % reported ever having had sex while drunk or while using drugs. HIV knowledge was low, 60.6 % answered half or fewer of the questions correctly. Self-perceived HIV risk was very low—nearly three-quarters (73.9 %) of young women reported they had ‘no chance’ of getting HIV in their lifetime.
Several individual characteristics were associated with prevalent HIV and HSV-2 infections at enrollment, although only a few were statistically significant and after the Bonferonni adjustment for multiple comparisons even fewer (Table 3). Early age of debut was associated with a higher odds of both HIV and HSV-2 infection (aOR 1.95 95 % CI 0.98–3.89; aOR 2.03 95 % CI 1.10–3.72, respectively) (Table 3). Those with more sex partners also had a significantly higher odds of HIV and HSV-2 infection, as did those who reported ever having vaginal sex. Those with low knowledge of HIV and self-perceived some/high chance of acquiring HIV in their lifetime had a significantly higher odds of being HIV infected. Ever having been pregnant, having had anal sex, no condom use at last sex, depressive symptoms and high alcohol consumption were significantly associated with HSV-2 but not HIV.
Household Characteristics
The majority (71.4 %) of young women reported that both parents were alive (Table 2). Nearly a quarter (23.8 %) reported one parent had died, 4.8 % reported both parents had died, and 3.8 % reported having a sick parent/guardian who was bed-ridden in the last 30 days. The majority of young women reported that their mother was their primary caregiver (65.8 %) followed by a grandparent (14.2 %). Over one-third (34.3 %) of girls reported worrying about having enough food to eat the past 12 months.
Household-level characteristics were associated with HIV and HSV-2 infection at baseline (Table 3). Young women who reported that their primary caregiver was not a parent were more than twice as likely to be HIV infected and over 60 % more likely to be HSV-2 infected (aOR 2.20 95 % CI 1.40–3.46; aOR 1.64 95 % CI 1.09–2.47, respectively). Double orphans had significantly higher odds of HIV infection, compared to non-orphans and those young women who reported not living with either parent had a higher odds of HIV and HSV-2 infection. Similarly, those living in a household in the lowest asset index quartile were significantly more likely to HSV-2 infected, compared to the highest asset quartile.
Partner Characteristics
Among those with sexual experience, it was common for young women to report that their sex partners gave them money or gifts (84.8 %); however, only 14.2 % reported that they felt they had to have sex with their partner because of these transactions (Table 2). Older partners (any of the last three sex partners being 5 or more years older) were reported by 19.7 % of young women. Nearly half (48.4 %) reported thinking that one or more of their last three partners had other partners at the same time as maintaining a relationship with them. Lifetime experience of IPV was reported by 17.4 % of young women and 9.8 % of young women reported sexual abuse.
Young women who reported that any of their last three sex partners were five or more years older had a significantly higher odds of being HIV and HSV-2 infected (aOR 2.46 95 % CI 1.24–4.90; aOR 2.50 95 % CI 1.45–4.30, respectively) and those who reported that any of their last three sex partnerships involved transactional sex had a significantly higher odds of HIV infection (aOR 2.60 95 % CI 1.27–5.36).
Schooling Factors
Young women were evenly distributed in grades 8, 9, 10 and 11 at baseline (Table 2). Close to one-third (29.3 %) of the young women were older than the expected age for their school grade and 35.0 % had repeated a grade. A small percentage (6.6 %) reported missing 4 or more days of school in a typical month and 71.0 % reported that there was a high chance they would stay in school until they completed high school (Grade 12).
Young women who reported having repeated a grade or having missed 4 or more days of school in the last month were significantly more likely to be HIV infected (aOR 2.17 95 % CI 1.25–3.79; aOR 2.07 95 % CI 1.07–4.01, respectively) (Table 3). These same factors were also associated with an increased risk of HSV-2 infection, although the confidence intervals around the age-adjusted estimates included the null.
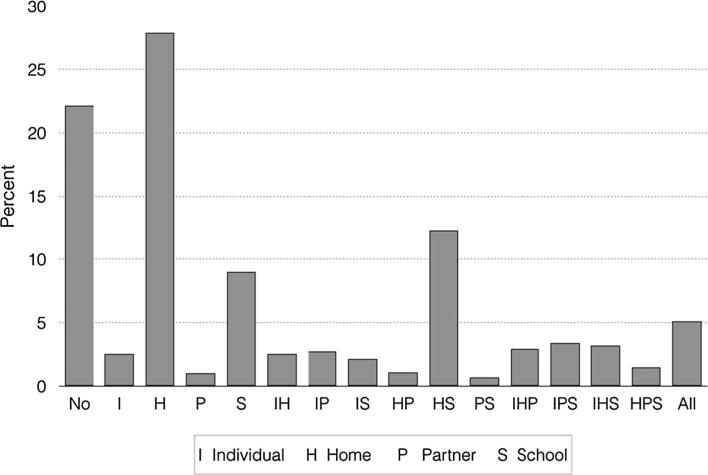
Combined Risk
Given that young women are placed at risk for HIV infection from multiple risk factors, which often operate at multiple levels (e.g., individual, partner, household and school), we examined the association between a young woman experiencing any important individual-, household-, partner- and school-level risk factor and HIV/HSV-2 infection prevalence. We also estimated HIV and HSV-2 prevalence within each possible combination of risk levels (e.g. among young women who report both individual-level risk factors and household-level risk factors). Close to a quarter (24.8 %) of young women reported an individual-level risk factor, over half reported a household-level risk factor (56.8 %), 17.7 % reported a partner-level risk factor and 37.6 % reported a school related risk factor (Table 4; Fig. 2).
Table 4.
Prevalence of risk factors at the individual-, household-, partner-, and school-level, by study arm, among 2533 young women enrolled in HPTN 068, Agincourt, South Africa March 2011–December 2012
| Total (n = 2533) N (%) | Arm = 1(n = 1261) N (%) | Arm = 0(n= 1272) N (%) | |
|---|---|---|---|
| Individual risk factors | |||
| Yes | 603 (24.8) | 308 (25.3) | 295 (24.2) |
| No | 1831 (75.2) | 909 (74.7) | 922 (75.8) |
| Missing | 99 | 44 | 55 |
| Household risk factors | |||
| Yes | 1417 (56.8) | 714 (57.6) | 703 (56.1) |
| No | 1076 (43.2) | 526 (42.4) | 550 (43.9) |
| Missing | 40 | 21 | 19 |
| Partner risk factors | |||
| Yes | 442 (17.7) | 215 (17.2) | 227 (18.1) |
| No | 2062 (82.4) | 1034 (82.8) | 1028 (81.9) |
| Missing | 29 | 12 | 17 |
| School risk factors | |||
| Yes | 949 (37.6) | 480 (38.3) | 469 (37.0) |
| No | 1572 (62.4) | 772 (61.7) | 800 (63.0) |
| Missing | 12 | 9 | 3 |
Reports at least one of the following risk factors: 1. No condom use at last sex with at least one of last three partners, 2. Multiple lifetime sex partners, 3. Any alcohol consumption, 4. Ever sex while drunk, 5. Ever sex while on drugs
Reports at least one of the following risk factors: 1. Single or double orphanhood, 2. Primary caregiver is non-parent, 3. Lowest asset quartile
Reports at least one of the following risk factors: 1. Older partner (by 5 or more years), 2. Transactional sex with at least one of last three partners, 3. Partner has other partners
Reports at least one of the following risk factors: 1. Repeated grade, 2. Miss >20 % school days in typical school week
Fig. 2.
Frequency of combinations of risk factors at the individual-, household-, partner-, and school-level among young women enrolled in HPTN 068 at baseline in Agincourt, South Africa March 2011–December 2012
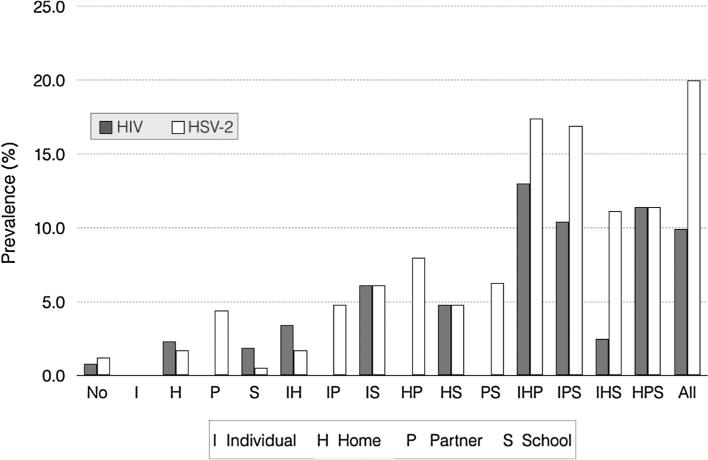
After adjusting for age, all categories were associated with a significantly increased odds of HIV infection with partner-level factors conveying the strongest association with HIV infection (aOR 3.05 95 % CI 1.84–5.06, Table 5). This was true for HSV-2 infection as well, except that the confidence interval around the estimate for schooling related factors included the null after adjusting for age. When looking at these risk levels in combination, prevalence of both HIV and HSV-2 generally increased with increasing number of risk levels experienced (Fig. 3). Interestingly, individual-level risk factors by themselves did not appear to place young women at higher risk for prevalent HIV or HSV-2 infection, but only did so when paired with risk at higher levels. The combination of household- and schooling related risk factors was associated with higher HIV prevalence than expected given the prevalence with either risk level alone [likelihood ratio (LLR) test Chi square statistic: 6.00, p-value 0.01]. The three-way combination of individual-, household- and schooling related risk and the three-way combination of household-, partner- and schooling related risk were associated with higher HSV-2 prevalence than anticipated given the prevalence observed at each level alone (LLR test Chi square statistic: 6.02, p-value 0.01; LLR test Chi square statistic: 3.91, p-value 0.05, respectively).
Fig. 3.
Prevalence of HIV and HSV-2 across each combination of risk factors at the individual-, household-, partner-, and school-level among young women enrolled in HPTN 068 at baseline in Agincourt, South Africa March 2011–December 2012
Discussion
Young women in South Africa face some of the highest risks of HIV infection in the world [4]. Cash transfers have increasingly been advocated for as a possible tool to reduce HIV infection among young women [4, 21, 22]. This is the first randomized controlled trial to examine the impact on HIV incidence of a cash transfer conditional on school attendance among young women and thus the results have important implications for prevention programs and policy. We designed this cash transfer study with the aim of increasing school attendance, which we hypothesized would decrease the risk of HIV infection in young women. There is a robust literature from numerous settings demonstrating that conditional cash transfers have been effective in increasing school attendance by helping individuals overcome economic barriers to schooling [10]. We based the cash transfer amount used in the study on the government of South Africa's CSG, which is part of the government's social protection plan and in 2015 provided R330 per month to poor households for every child under the age of 18 (up to a maximum of 6 per caregiver) [23]. We chose to focus on schooling as the key mechanism to reduce HIV risk based on prior research we conducted among young women in South Africa showing that those who did not complete school were at increased risk of HIV infection [7]. It is also possible that cash transfers may reduce HIV risk through mechanisms other than schooling. Cash transfer evaluations that have shown an impact on HIV risk among young women suggest that cash transfers may alter the types of partners that young women select. In Zomba, Malawi, young women receiving cash reported that they were less likely to have older partners (partners who were 25 years or older) as well as less likely to have frequent sex (sex once a week) [11].
We designed the cash transfer payment scheme to maximize the potential for HIV prevention. The Zomba trial provided money directly to young women in school (the amount varied from USD 1–5 per month) as well as to the parent/guardian (the amount varied from USD 4–10 per month); most other cash transfer studies with adolescents do not provide money directly to the minor. In our trial we also provided one-third of the money to the young woman and two-thirds to the parent guardian. Our rationale for this was that in trying to change the behavior of young women, it is the young woman who needs support and an incentive to attend school as much as the parent/guardian. In another study conducted among adolescent girls in South Africa, girls (aged 10–18 years) living in households receiving the CSG were less likely to report incident transactional sex and older partners, again supporting the idea that extra cash in these homes helps young women to make different partner choices [12].
Among this cohort of adolescent girls attending high school in rural South Africa, baseline prevalence of HIV and HSV-2 were relatively low. These low infection levels are consistent with the young average age (mean age 15) and limited sexual experience of the cohort, and with the fact that everyone was enrolled in school at baseline. We anticipate that as these young women age and experience sexual debut, HIV prevalence will increase rapidly. In South Africa, HIV incidence and prevalence increase dramatically after the age of 18 [1, 24]. We know that HIV prevalence among women in this setting escalates from 5 % among 15–19 year olds to 27 % by age 20–24 and peaks at 46 % by age 35–39 years [17]. Thus it is worrying that >70 % of the young woman thought they had no risk of acquiring HIV in their lifetime and also that only ~60 % had correct basic knowledge about HIV.
Despite the low prevalence at baseline, a large proportion of the population reported structural risk factors at the household- and school-level, as well as more traditional individual- and partner-level risk factors, which were associated with an increased odds of HIV and HSV-2 infection. One-third of girls reported experiencing food insecurity in the last year and having repeated a grade, and close to a third were orphans or were older than expected for their grade in school. Among the sexually active girls, about half reported using a condom at last sex and just over half reported using contraception. A significant proportion also reported partnering patterns suggestive of increased HIV risk; 20 % reported having a partner 5 or more years older and 14 % reported engaging in transactional sex. When grouping these factors into different domains or levels of influence, over half of young women reported experiencing a household-level factor which increased their risk of HIV or HSV-2. Over a third (38 %) reported a schooling related risk factor and 37.5 % reported risk factors at more than one level. While individual factors, such as partner number, and partner-level factors, like older partners and transactional sex, were associated with HIV infection, we also observed that structural level factors such as orphanhood and poor school attendance were prevalent in the population and were associated with increased risk of HIV and HSV-2 as well. We also observed that young women who experienced multiple risk factors at multiple levels had very high HIV or HSV-2 prevalence. For example, while no young women with just partner-level risk factors tested HIV+, if young women had a partner-, individual- and household-level risk factor the prevalence of HIV was 13 %. These results confirm the need for prevention interventions that address multiple risk factors at different levels; specifically those beyond the level of the individual, and including structural factors.
At baseline there were a number of other important findings. Despite the young age of the cohort, 17 % reported having experienced IPV in their lifetime. South Africa is known for having extremely high rates of IPV [25, 26]. That close to one-fifth of the population had experienced IPV, despite the fact that only a quarter reported ever having had sex, is notable and again emphasizes how widespread this problem is and the imperative to address it. Markers of depression were high in this group with almost 19 % of young women reporting symptoms indicative of depression. Prior research in South Africa with young people and also using the same measure of depression found that 17 % of AIDS orphaned adolescents and 9 % of non-orphans were depressed [18]. Mental health is overlooked in rural settings and there is limited allocation of mental health care resources. This clearly requires greater attention by policy-makers and service providers.
The study has some limitations. Firstly, while we are aiming to measure various levels of HIV risk for young women, all indicators were measured at the young woman or parent/guardian level, thus school related factors are not truly indicative of characteristics of the school itself but rather factors related to the young woman's education and schooling. Further, all measures related to the partner were reported by the young woman. Second, all behavioral data were self-reported and thus maybe over or under-reported; however, the use of ACASI should help with reducing social desirability bias [27]. Further, as this study was a cash transfer to keep young women in school the results are not generalizable to young women out of school. That said, they are relevant for programs aiming to keep young women in school, in particular in poor, rural areas of South Africa. This paper presents a broad description of a cohort of young women in rural South Africa at high risk for HIV, and identifies key socio-demographic and behavioral factors associated with prevalent HIV and HSV-2 infection. The intention of presenting these associations is to better understand the demographic profile of those at heightened risk for sexually transmitted infections. Cautious interpretation of each specific association is warranted due to the high number of associations tested, small number of prevalent outcomes, and cross-sectional nature of the data.
Conclusion
Young women in SSA face extremely high risk and rates of HIV infection. Cash transfers are potentially one mechanism to address structural factors that increase young women's risk in many settings. This is the first randomized trial with an HIV incidence endpoint to examine the impact of a cash transfer conditional on school attendance among young women. This study is unique in that we are collecting detailed information to better understand the causal pathways through which cash transfers may work to reduce HIV risk. Results of this study will have important implications for better understanding the role of conditional cash transfers to prevent HIV infection among young women in SSA.
Acknowledgments
Overall support for the HIV Prevention Trials Network (HPTN) was provided by the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Mental Health (NIMH) and the National Institute on Drug Abuse (NIDA) of the National Institutes of Health (NIH) under Award Numbers UM1AI068619 (HPTN Leadership and Operations Center), UM1AI068617 (HPTN Statistical and Data Management Center), and UM1AI068613 (HPTN Laboratory Center). The study was also funded under Award Number 5R01MH087118-02 and R24 HD050924 to the Carolina Population Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health.
References
- 1.Shisana O, Rehle T, LC S, Zuma K, Jooste S, N Z, et al. South African National HIV prevalence, incidence and behaviour survey 2012. Cape Town: 2014. [DOI] [PubMed] [Google Scholar]
- 2.Abdool Karim Q, Kharsany AB, Frohlich JA, Werner L, Mashego M, Mlotshwa M, et al. Stabilizing HIV prevalence masks high HIV incidence rates amongst rural and urban women in KwaZulu-Natal, South Africa. Int J Epidemiol. 2010 doi: 10.1093/ije/dyq176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372(6):509–18. doi: 10.1056/NEJMoa1402269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNAIDS . The gap report. UNAIDS; Geneva: 2014. [Google Scholar]
- 5.Cowan F, Pettifor A. HIV in adolescents in sub-Saharan Africa. Curr Opin HIV AIDS. 2009;4(4):288–93. doi: 10.1097/COH.0b013e32832c7d10. [DOI] [PubMed] [Google Scholar]
- 6.Pettifor A, Bekker LG, Hosek S, DiClemente R, Rosenberg M, Bull SS, et al. Preventing HIV among young people: research priorities for the future. J Acquir Immune Defic Syndr (1999) 2013;63(2):S155–60. doi: 10.1097/QAI.0b013e31829871fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pettifor AE, Levandowski BA, MacPhail C, Padian NS, Cohen MS, Rees HV. Keep them in school: the importance of education as a protective factor against HIV infection among young South African women. Int J Epidemiol. 2008;37(6):1266–73. doi: 10.1093/ije/dyn131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hargreaves JR, Bonell CP, Boler T, Boccia D, Birdthistle I, Fletcher A, et al. Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in sub-Saharan Africa. AIDS. 2008;22(3):403–14. doi: 10.1097/QAD.0b013e3282f2aac3. [DOI] [PubMed] [Google Scholar]
- 9.Jukes M, Simmons S, Bundy D. Education and vulnerability: the role of schools in protecting young women and girls from HIV in southern Africa. AIDS. 2008;22(4):S41–56. doi: 10.1097/01.aids.0000341776.71253.04. [DOI] [PubMed] [Google Scholar]
- 10.Fizbein A, Schady N. Conditional cash transfers reducing present and future poverty. 2009 [Google Scholar]
- 11.Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–9. doi: 10.1016/S0140-6736(11)61709-1. [DOI] [PubMed] [Google Scholar]
- 12.Cluver L, Boyes M, Orkin M, Pantelic M, Molwena T, Sherr L. Child-focused state cash transfers and adolescent risk of HIV infection in South Africa: a propensity-score-matched case-control study. Lancet Glob Health. 2013;1(6):e362–70. doi: 10.1016/S2214-109X(13)70115-3. [DOI] [PubMed] [Google Scholar]
- 13.Handa S, Halpern CT, Pettifor A, Thirumurthy H. The government of Kenya’s cash transfer program reduces the risk of sexual debut among young people age 15–25. PLoS One. 2014;9(1):e85473. doi: 10.1371/journal.pone.0085473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cho H, Hallfors DD, Mbai II, Itindi J, Milimo BW, Halpern CT, et al. Keeping adolescent orphans in school to prevent human immunodeficiency virus infection: evidence from a randomized controlled trial in Kenya. J Adolesc Health. 2011;48(5):523–6. doi: 10.1016/j.jadohealth.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hallfors DD, Cho H, Rusakaniko S, Mapfumo J, Iritani B, Zhang L, et al. The impact of school subsidies on HIV-related outcomes among adolescent female orphans. J Adolesc Health. 2015;56(1):79–84. doi: 10.1016/j.jadohealth.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kahn K, Collinson MA, Gómez-Olivé FX, Mokoena O, Twine R, Mee P, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012;41:988–1001. doi: 10.1093/ije/dys115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomez-Olive FX, Angotti N, Houle B, Klipstein-Grobusch K, Kabudula C, Menken J, et al. Prevalence of HIV among those 15 and older in rural South Africa. AIDS Care. 2013;25(9):1122–8. doi: 10.1080/09540121.2012.750710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cluver L, Gardner F, Operario D. Psychological distress amongst AIDS-orphaned children in urban South Africa. J Child Psychol Psychiatry. 2007;48(8):755–63. doi: 10.1111/j.1469-7610.2007.01757.x. [DOI] [PubMed] [Google Scholar]
- 19.García-Moreno C, et al. WHO multi-country study on women’s health and domestic violence against women: initial results on prevalence, health outcomes and women’s responses. Geneva: 2005. [Google Scholar]
- 20.Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–43. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- 21.UNICEF Social protection preogrammes contribute to HIV prevention. 2015 [Google Scholar]
- 22.Pettifor A, MacPhail C, Nguyen N, Rosenberg M. Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS Behav. 2012;16(7):1729–38. doi: 10.1007/s10461-012-0240-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Department of Social Development, SASSA, UNICEF . The South African Child Support Grant impact assessment: evidence from a survey of children, adolescents, and their households. Pretoria: 2012. [Google Scholar]
- 24.Pettifor A, Rees H, Steffenson A, Hlongwa-Madikizela L, Mac-Phail C, Vermaak K, et al. HIV and sexual behaviour among young South African a national survey of 15–24 year olds. Reproductive Health Research Unit; Johannesburg: 2004. [Google Scholar]
- 25.Jewkes R, Abrahams N. The epidemiology of rape and sexual coercion in South Africa: an overview. Soc Sci Med. 2002;55:1231–44. doi: 10.1016/s0277-9536(01)00242-8. [DOI] [PubMed] [Google Scholar]
- 26.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–8. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 27.Langhaug LF, Sherr L, Cowan FM. How to improve the validity of sexual behaviour reporting: systematic review of questionnaire delivery modes in developing countries. Trop Med Int Health. 2010;15(3):362–81. doi: 10.1111/j.1365-3156.2009.02464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]