Abstract
AIM
To investigate choroidal thickness in pregnant women and compare the measurements with those of normal nonpregnant women.
METHODS
Using enhanced depth imaging optical coherence tomography (EDI-OCT), choroidal thickness was measured at the fovea and at 1 mm and 3 mm superior, inferior, temporal, and nasal to the fovea in both healthy pregnant women and nonpregnant women. Pearson correlation analysis was performed to evaluate the relationships between subfoveal choroidal thickness (SFCT) and the demographic and ocular parameters. Pooled odds ratio (OR) and 95% confidence interval (CI) were calculated using fixed-effects model when Meta-analyses were conducted.
RESULTS
Comparison of choroidal thickness between the groups showed that it was significantly greater in healthy pregnant women's eyes than in normal nonpregnant women's eyes at all locations except at 3 mm superior and 3 mm temporal from the fovea (P<0.05). The mean SFCT was 344.13±50.94 µm in healthy pregnant women's eyes and 315.03±60.57 µm in normal nonpregnant women's eyes, with a statistically significant difference (P=0.008). Pearson correlation analysis showed that age and axial length were significantly related to SFCT in healthy pregnant women, normal nonpregnant women, and all subjects. The results of our cross-sectional study were consistent with the results of the further Meta-analysis, with a pooled weighted mean difference (WMD) of 33.66 µm (95% CI: 26.16 to 41.15) for SFCT.
CONCLUSION
Our results, along with the comprehensive Meta-analysis, suggest that choroidal thickness in healthy pregnant women is greater than that in normal nonpregnant women.
Keywords: choroidal thickness, pregnant, optical coherence tomography
INTRODUCTION
Pregnant women undergo many metabolic and anatomical physiological changes to accommodate the physiological stress on their bodies[1]. Several studies have reported that most important organs of the body are affected by these changes, including the eyes [2]. Numerous studies have demonstrated that pregnancy gives rise to several physiological ophthalmic changes, such as modifications to intraocular pressure (IOP)[3], a progressive decrease in corneal sensitivity, an increase in central corneal thickness (CCT) and curvature[4]–[5], and ocular blood flow changes[6]. As we all know, the choroid were mainly composed of the vascular tissue supplying the most of blood flow of ocular. Recent research has focused on choroidal modification as a key example of the physiological changes involved in the pathophysiology of pregnancy[7]–[8].
Choroidal thickness may be an important parameter for investigating pathogenesis in the choroid. In recent years, the development of enhanced depth imaging (EDI) has enabled choroidal examination with optical coherence tomography (OCT), which measures choroidal thickness more accurately, safely, and simply than other methods[9]–[12]. To date, a number of researchers have examined choroidal thickness in pregnant women to understand choroidal blood circulation during pregnancy[8],[13]–[16]. However, whether or not choroidal thickness changes in pregnant women remains controversial. For example, Takahashi et al[16] found that choroidal thickness was not significantly different between healthy pregnant women and normal nonpregnant women, whereas Kara et al's[15] study had inconsistent results. Whether or not choroidal thickness changes in pregnant women with preeclampsia also remains controversial. Thus, the possible association between choroidal thickness and pregnancy remains unclear, which justifies the need for more studies on this issue.
In this study, we first conducted a cross-sectional study and then performed a Meta-analysis to evaluate macular choroidal thickness in pregnant women and normal nonpregnant women.
SUBJECTS AND METHODS
Subjects and Enrollment Criteria
We conducted this observational, cross-sectional study of healthy pregnant women at Zhujiang Hospital. It was approved by the Ethical Review Committee of Zhujiang Hospital and adhered to the provisions of the Declaration of Helsinki for research involving human subjects. Written informed consent was obtained from the participants before the study began. All the subjects were from Chinese Han population, and they were prospectively and consecutively recruited for this study between September 2014 and March 2015.
For the healthy pregnant women group, the inclusion criteria were as follows: 1) women at weeks 28-38 of gestation; 2) women whose eyes had a spherical equivalent (SE) between -3 diopter (D) to 3 D; 3) women whose eyes had clear ocular media; 4) a clear image was obtained to enable precise measurement of the choroidal thickness. The exclusion criteria were as follows: 1) pregnant women who had a history of intraocular surgery, refractive surgery, or intravitreal injection; 2) pregnant women with any systemic and ocular disease except for mild ametropia; 3) pregnant women who had developed gestational diseases, such as diabetes, preeclampsia, or eclampsia. In the normal nonpregnant women group, we included subjects without any systemic and ocular disease except for mild ametropia and those whose eyes had a SE between -3 D to 3 D.
Examination
Each subject underwent a comprehensive ophthalmologic examination, including best corrected visual acuity, IOP measurement (applanation tonometry), slit-lamp biomicroscopy, color fundus photography (Canon, Retinal Camera CR-DGi, Japan), axial length (AL) and anterior chamber depth measurement (IOL-Master, Carl Zeiss Meditec, La Jolla, CA, USA), ophthalmoscopy fundus examination, B-scanning, refractive error measurement (KR-8900 version 1.07, Topcon Corporation, Tokyo, Japan), and CCT measurement. Each subject's age and blood pressure at the time of imaging were collected.
Enhanced Depth Imaging-Optical Coherence Tomography Examination
The choroidal images of spectral domain OCT with EDI mode were obtained using the Heidelberg Spectralis (Heidelberg Engineering, Heidelberg, Germany), as described previously[12]. In brief, the vertical and horizontal sections going directly through the center of the fovea were used for final analysis. Choroidal thickness was determined as the vertical distance from the hyperreflective line of the hyperreflective retinal pigment epithelium (RPE) to the line of the inner surface of the sclera. Choroidal thicknesses were measured at the subfovea, 1 mm and 3 mm, nasally, temporally, superiorly, and inferiorly. Measurements were performed in a masked fashion by two independent experienced OCT readers. The values of the measurements were compared for each observer and then averaged for analysis. One eye (right eye) per patient was selected for measurement. Because of the diurnal fluctuation of choroidal thickness[17], all EDI-OCT examinations were performed between 9:00 a.m. and 11:00 a.m.
Statistical Analysis
All statistical analyses were performed using SPSS version 17 (SPSS Inc., Chicago, IL, USA). All data are expressed as mean±standard deviation. Comparisons between healthy pregnant women and normal nonpregnant women were performed using independent t-tests for normally distributed variables. Pearson correlation analysis was performed to evaluate the relationships between subfoveal choroidal thickness (SFCT) and the demographic and ocular parameters. For all the tests, P<0.05 was considered significant.
Meta-analysis
A literature search of PubMed, ISI Web of Science, and EMBASE was performed to identify relevant studies. The following keywords were used in the search: gravida, pregnant, gestation, choroidal thickness, choroid. The websites of professional associations and Google Scholar were searched for additional information. Once relevant articles were identified, their reference lists were searched for additional articles. When our search identified several studies published by the same population, the most recent study was included. The final literature search was updated on May 2015, with no restrictions on publication year, language, or methodology.
In the Meta-analysis, the following inclusion criteria were used: 1) study type: cross-sectional or case-control design; 2) choroidal thickness measured by EDI-OCT; 3) comparison of macular choroidal thickness between pregnant and normal nonpregnant women. Editorials, letters to the editor, review articles, case reports, meeting abstracts, and animal experimental studies were excluded. Two reviewers independently extracted data from the included studies using a standardized data extraction form: first author, year of publication, number of pregnant women and controls, gestation week, trimester, and status of pregnant woman. Any discrepancies were addressed by conducting a discussion to reach a consensus.
Weighted mean differences (WMDs) were used to compare choroidal thickness between pregnant and normal nonpregnant women. All outcomes were reported with a 95% confidence interval (CI). Statistical heterogeneity between studies was assessed using a Chi-squared test, and the quantity of heterogeneity was evaluated using the I2 statistic. The WMD were calculated by fixed-effect model or random-effect model depending on the significance of heterogeneity. The statistical heterogeneity was considered insignificant when I2<50%[18]–[19]. To explore the source of heterogeneity, subgroup analyses were performed according to trimester, instrument used, and status of pregnant woman. To evaluate the influence of an individual dataset on the pooled results, a sensitivity analysis was performed to delete one single study at a time, and the combined estimates were recalculated based on the remaining studies. Potential publication bias was evaluated using Begg's test and Egger's test[20]–[21]. P<0.05 was considered statistically significant. All statistical analyses were performed using Stata (version 12; Stata Corp., College Station, Texas, USA).
RESULTS
Demographic and Baseline Characteristics of the Subjects
A total of 71 eyes of 71 normal nonpregnant women and 46 eyes of 46 healthy pregnant women on which OCT scans were conducted and for which clear images were acquired were included in the study. The mean age was 27.87±3.65y for normal nonpregnant women and 28.43±3.15y for healthy pregnant women. The mean SEs of the normal nonpregnant women's eyes and the healthy pregnant women's eyes were -1.04±1.17 D and -0.95±1.12 D, respectively. The mean ALs were 23.92±0.62 mm and 24.11±0.68 mm, respectively. The mean number of gestation weeks was 30.20±1.63wk for healthy pregnant women. The mean age, IOP, SEs, AL, anterior chamber depth, CCT, diastolic blood pressure, systolic blood pressure, diastolic ocular perfusion pressure, systolic ocular perfusion pressure, and mean ocular perfusion pressure of the two groups did not differ significantly. The demographic and baseline characteristics of the patients are summarized in Table 1.
Table 1. Clinical characteristics in study subjects.
| Characteristic | Control | Normal pregnant | P |
| No. of patients (eyes) | 71 (71) | 46 (46) | - |
| Age (a) | 27.87±3.65 | 28.43±3.15 | 0.394a |
| Gestation week (wk) | - | 30.20±1.63 | - |
| IOP at imaging (mm Hg) | 15.11±3.59 | 14.39±2.73 | 0.224a |
| Spherical equivalent (D) | -1.04±1.17 | -0.95±1.12 | 0.676a |
| Axial length (mm) | 23.92±0.62 | 24.11±0.68 | 0.125a |
| Anterior chamber depth (mm) | 3.07±0.49 | 3.13±0.49 | 0.610 |
| CCT (µm) | 542.18±33.30 | 539.52±32.28 | 0.670a |
| DBP (mm Hg) | 73.45±6.95 | 72.70±6.32 | 0.553 a |
| SBP (mm Hg) | 117.72±11.23 | 116.00±9.07 | 0.613 a |
| Diastolic OPP (mm Hg)1 | 58.34±7.77 | 58.30±7.09 | 0.978a |
| Systolic OPP (mm Hg)2 | 102.61±11.35 | 101.61±8.88 | 0.613 a |
| Mean OPP (mm Hg) 3 | 73.10±7.30 | 72.74±6.06 | 0.781 a |
SD: Standard deviation; IOP: Intraocular pressure; D: Diopter; CCT: Central corneal thickness; DBP: Diastolic blood pressure; SBP: Systolic blood pressure; OPP: Ocular perfusion pressure. aIndependent sample t-test; 1,2Calculated as the differential pressure between diastolic or systolic blood pressure and IOP; 3Calculated as the differential pressure between mean BP and IOP [mean BP=DBP+1/3×(SBP-DBP)].
x±s
Macular Choroidal Thickness Measurements
The mean SFCT was 315.03±60.57 µm in normal nonpregnant women and 344.13±50.94 µm in healthy pregnant women, with a statistically significant difference (P=0.008). For both groups, SFCT and thickness in the superior, nasal, inferior, and temporal quadrants 1 mm and 3 mm from the fovea are shown in Table 2. Macular choroidal thickness was significantly greater in healthy pregnant women than in normal nonpregnant women at all locations except for 3 mm superior and 3 mm temporal from the fovea.
Table 2. Average choroidal thickness and 95% CI at different locations in macula.
| Location (mm from fovea) | Normal pregnant |
Control |
Mean difference (µm)1 | 95%CI (µm) |
P | |||
| Mean (µm) | SD (µm) | Mean (µm) | SD (µm) | Lower bound | Upper bound | |||
| SFCT | 344.13 | 50.94 | 315.03 | 60.57 | 29.10 | 7.73 | 50.47 | 0.008 |
| Superior 1 mm | 302.32 | 54.18 | 269.67 | 79.04 | 32.65 | 6.26 | 59.03 | 0.009 |
| Superior 3 mm | 283.95 | 48.79 | 264.56 | 67.39 | 19.39 | -3.40 | 42.18 | 0.095 |
| Inferior 1 mm | 269.52 | 58.81 | 243.73 | 77.30 | 25.79 | 0.78 | 50.80 | 0.043 |
| Inferior 3 mm | 237.80 | 44.18 | 215.07 | 66.34 | 22.73 | 2.49 | 42.97 | 0.028 |
| Nasal 1 mm | 269.67 | 61.82 | 240.74 | 79.26 | 28.92 | 2.97 | 54.88 | 0.029 |
| Nasal 3 mm | 190.56 | 56.59 | 165.63 | 69.83 | 24.93 | 1.62 | 48.23 | 0.045 |
| Temporal 1 mm | 280.97 | 51.55 | 256.55 | 66.94 | 24.42 | 2.64 | 42.61 | 0.028 |
| Temporal 3 mm | 243.32 | 47.18 | 227.60 | 51.12 | 15.72 | -2.59 | 34.03 | 0.097 |
CI: Confidence interval; SD: Standard deviation; SFCT: Subfoveal choroidal thickness. 1Normal group as reference.
Factors Associated with Subfoveal Choroidal Thickness
Table 3 shows the results of the Pearson correlation analysis of SFCT. Pearson correlation analysis showed that age and AL were significantly related to SFCT in healthy pregnant women, normal nonpregnant women, and all subjects. None of the other variables were significantly associated with SFCT in healthy pregnant women, normal nonpregnant women, or all subjects.
Table 3. Association between subfoveal choroidal thickness with other factors.
| Factors | Healthy pregnant |
Normal nonpregnant women |
All |
|||
| r | P | r | P | r | P | |
| Age (a) | -0.416 | 0.015 | -0.320 | 0.036 | -0.197 | 0.033 |
| IOP at imaging (mm Hg) | 0.034 | 0.821 | 0.053 | 0.659 | 0.020 | 0.831 |
| Spherical equivalent (D) | -0.245 | 0.100 | 0.076 | 0.529 | -0.023 | 0.807 |
| Axial length (mm) | -0.337 | 0.022 | -0.274 | 0.046 | -0.258 | 0.005 |
| ACD (mm) | 0.012 | 0.938 | 0.172 | 0.152 | 0.123 | 0.185 |
| CCT (µm) | 0.255 | 0.087 | 0.103 | 0.391 | 0.141 | 0.130 |
| DBP (mm Hg) | -0.023 | 0.643 | -0.072 | 0.551 | -0.295 | 0.135 |
| SBP (mm Hg) | -0.014 | 0.925 | 0.177 | 0.141 | 0.095 | 0.309 |
| Diastolic OPP (mm Hg) | -0.039 | 0.754 | -0.089 | 0.461 | -0.083 | 0.403 |
| Systolic OPP (mm Hg) | -0.025 | 0.868 | 0.158 | 0.188 | 0.089 | 0.342 |
| Mean OPP (mm Hg) | -0.217 | 0.132 | 0.019 | 0.877 | -0.089 | 0.340 |
| Gestation week | 0.040 | 0.794 | - | - | - | - |
IOP: Intraocular pressure; D: Diopter; CCT: Central corneal thickness; DBP: Diastolic blood pressure; SBP: Systolic blood pressure; OPP: Ocular Perfusion Pressure.
Eligible Articles for Meta-analysis
In order to obtain more information about the difference in choroidal thickness between pregnant women and normal nonpregnant women, we performed a Meta-analysis. A total of 38 papers were identified by our literature search, of which 23 were excluded as duplicate studies and 7 were excluded based on titles and abstracts. Thus, eight studies were included in the Meta-analysis [7]–[8],[13]–[16],[22]–[23]. Of these eight articles, Atas et al's[8] and Sayin et al's[23] studies involved two types of pregnant women (healthy pregnant women and pregnant women with preeclampsia), and Goktas et al's[7] study involved two trimesters (first and third). We grouped the different types of pregnant women and different trimesters into separate datasets. In another article[13], the authors separated the data into that for right eyes and that for left eyes and included pregnant women in two trimesters (first and third). We assumed that the right eyes with different trimesters and the left eyes with different trimesters were the subjects in four datasets. Overall, 14 datasets plus the present dataset were selected for Meta-analysis.
Characteristics of the Included Studies
The eight studies plus the present study, which represented a total of 489 pregnant women's eyes and 435 normal nonpregnant women's eyes, were included in the Meta-analysis. Among these studies, six originated from Turkey, one from the United States, one from Japan, and one from China. The main characteristics of the included studies are presented in Table 4.
Table 4. Characteristics of included studies.
| First author (year) | Location | CT | Instrument | Age (a)1 | Gestation(wk) | Trimester | Pregnant | No. eyes (normal pregnant /control) |
| Takahashi[16] (2013) | Japan | SFCT | Spectralis | 30.4/30.0 | 31.0±3.2 | Third trimester | Healthy pregnant | 25/27 |
| Sayin[23](2014) | Turkey | SFCT | Cirrus-HD OCT | 30.2/28.1 | 28.0±5.8 | Third trimester | Healthy pregnant | 46/40 |
| Sayin[23](2014) | Turkey | SFCT | Cirrus-HD OCT | 30.5/30.2 | 29.7±5.5 | Third trimester | Preeclampsia | 33/40 |
| Goktas[7](2014) | Turkey | SFCT | Spectralis | 26.9/29.4 | 33.1±2.8 | Third trimester | Healthy pregnant | 30/30 |
| Goktas[7](2014) | Turkey | SFCT | Spectralis | 28.5/29.4 | 7.4±2.6 | First trimester | Healthy pregnant | 30/30 |
| Garg[14](2014) | USA | SFCT | Spectralis | 32.7/37.9 | 32.5±4.9 | Third trimester | Preeclampsia | 15/19 |
| Kara[15](2014) | Turkey | SFCT | Cirrus-HD OCT | 21.6/22.0 | 27.3±6.6 | Third trimester | Healthy pregnant | 100/100 |
| Atas[8](2014) | Turkey | SFCT | Spectralis | 27.7/29.0 | 31.37±4.9 | Third trimester | Healthy pregnant | 25/26 |
| Atas[8](2014) | Turkey | SFCT | Spectralis | 30.8/29.0 | 38.35±3.1 | Third trimester | Preeclampsia | 27/26 |
| Ulusoy[22](2015) | Turkey | SFCT | Spectralis | 28.0/27.4 | 31.97±3.77 | Third trimester | Healthy pregnant | 58/72 |
| Dadaci[13] (2015)2 | Turkey | SFCT | Cirrus-HD OCT | 28.9/29.2 | 35.1±1.9 | Third trimester | Healthy pregnant | 27/25 |
| Dadaci[13](2015)3 | Turkey | SFCT | Cirrus-HD OCT | 28.9/29.2 | 35.1±1.9 | Third trimester | Healthy pregnant | 27/25 |
| Dadaci[13](2015)2 | Turkey | SFCT | Cirrus-HD OCT | 28.9/29.2 | 6.8±0.8 | First trimester | Healthy pregnant | 27/25 |
| Dadaci[13](2015)3 | Turkey | SFCT | Cirrus-HD OCT | 28.9/29.2 | 6.8±0.8 | First trimester | Healthy pregnant | 27/25 |
| Present (2015) | China | SFCT | Spectralis | 28.4/27.8 | 30.2±1.63 | Third trimester | Healthy pregnant | 46/71 |
CT: Choroidal thickness; SFCT: Subfoveal choroidal thickness; OCT: Optical coherence tomography. 1Normal pregnant /control; 2Data from the right eye; 3Data from the left eye.
Meta-analysis Results
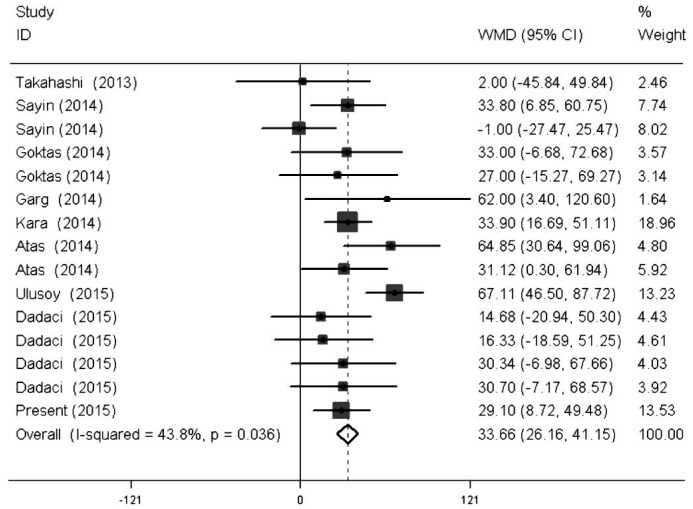
Fifteen datasets were identified that reported results on comparison of SFCT between pregnant women and normal nonpregnant women, with a WMD of 33.66 µm (95% CI: 26.16 to 41.15). Among the studies, statistically significant heterogeneity was detected (P=0.036; I2=43.8%).The results of the pooled WMD and the heterogeneity test of the Meta-analysis are presented in Table 5 and Figure 1. Considering that OCT precision was 10 µm, this difference could have been caused by instrument error. We then stratified the studies based on the instrument used. Subgroup analysis showed that a different examination instrument obtained similar results. In addition, several studies included women in both the first and third trimesters of pregnancy, which could have affected choroidal thickness. Therefore, we also stratified the studies according to trimester. The results showed that women in the first trimester of pregnancy and those in the third trimester had similar choroidal thickness. Notably, some studies included pregnant women with preeclampsia, and the different study on SFCT of pregnant with preeclampsia had the opposite conclusion. Thus, we stratified the studies again according to the presence or absence of preeclampsia. The subgroups showed that SFCT in healthy pregnant women was significantly greater than in normal nonpregnant women. However, SFCT in pregnant women with preeclampsia was not significantly different from SFCT in normal nonpregnant women, with a WMD of 17.82 µm (95% CI: -1.17 to 36.82). Detailed information about the subgroups is presented in Table 5.
Table 5. Pooled estimates of all studies comparing subfoveal choroidal thickness in normal pregnant eyes with normal control eyes.
| Subgroup | No. of studies | WMD (fixed) (95%CI) | Test for heterogeneity |
Test for overall effect |
||
| I2(%) | P | Z | P | |||
| All | 15 | 33.66 (26.16, 41.15) | 43.8 | 0.036 | 8.80 | <0.001 |
| Trimester | ||||||
| First trimester | 3 | 51.70 (36.09, 67.30) | 60.3 | 0.080 | 6.49 | <0.001 |
| Third trimester | 12 | 28.25 (19.70, 36.80) | 16.5 | 0.282 | 6.48 | <0.001 |
| Instrument | ||||||
| Spectralis | 8 | 43.21 (32.42, 53.99) | 47.0 | 0.067 | 7.85 | <0.001 |
| Cirrus-HD OCT | 7 | 24.74 (14.32, 35.16) | 0.00 | 0.438 | 4.65 | <0.001 |
| Pregnant | ||||||
| Healthy pregnant | 12 | 36.58 (28.42, 44.74) | 34.9 | 0.111 | 8.79 | <0.001 |
| Preeclampsia | 3 | 17.82 (-1.17, 36.82) | 58.7 | 0.089 | 1.84 | 0.066 |
WMD: Weighted mean differences; CI: Confidence interval; OCT: Optical coherence tomography.
Figure 1. Forest figure of all studies comparing subfoveal choroidal thickness in pregnant women and those in normal nonpregnant women.
Sensitivity Analysis and Publication Bias
To evaluate the robustness of the pooled results, single studies in the Meta-analysis were deleted in turn to reflect the influence of individual studies on the pooled estimates. The corresponding estimates before and after the deletion of any single study was generally similar, suggesting high stability in the Meta-analysis results. In addition, the sensitivity analysis revealed that two studies, by Sayin et al[23] and Ulusoy et al[22], were the main origin of heterogeneity. The I2 significantly declined from 43.8% to 26.7% (P=0.168) after removing the study by Sayin et al[23] and to 1.7% (P=0.431) after removing the study by Ulusoy et al[22] (Table 6). Begg's test (P=0.621) and Egger's test (P=0.495) were conducted to quantitatively assess the publication bias of the included studies. No significant publication bias was observed.
Table 6. Sensitivity analysis of the Meta-analysis.
| Study excluded | Fixed effects model |
Test of homogeneity |
|||
| WMD | 95%CI | Q | I2(%) | P | |
| None | 33.66 | 26.16, 41.15 | 24.89 | 43.8 | 0.036 |
| Takahashi[16] (2013) | 34.46 | 26.87, 42.04 | 23.17 | 43.9 | 0.040 |
| Sayin[23] (2014) | 33.65 | 25.84, 41.45 | 24.89 | 47.8 | 0.024 |
| Sayin[23] (2014) | 36.68 | 28.86, 44.50 | 17.73 | 26.7 | 0.168 |
| Goktas[7] (2014) | 33.68 | 26.05, 41.32 | 24.89 | 47.8 | 0.024 |
| Goktas[7] (2014) | 33.87 | 22.26, 41.49 | 24.79 | 47.6 | 0.025 |
| Garg[14] (2014) | 33.19 | 25.63, 40.74 | 23.98 | 45.8 | 0.031 |
| Kara[15] (2014) | 33.60 | 25.27, 41.93 | 24.89 | 47.8 | 0.024 |
| Atas[8] (2014) | 32.09 | 24.40, 39.77 | 21.54 | 39.6 | 0.063 |
| Atas[8] (2014) | 33.82 | 26.09, 41.55 | 24.86 | 47.7 | 0.024 |
| Ulusoy[22] (2015) | 28.56 | 20.51, 36.60 | 13.22 | 1.7 | 0.431 |
| Dadaci[13] (2015) | 34.54 | 26.87, 42.21 | 23.75 | 45.3 | 0.034 |
| Dadaci[13] (2015) | 34.50 | 26.82, 42.17 | 23.90 | 45.6 | 0.032 |
| Dadaci[13] (2015) | 33.80 | 26.15, 41.45 | 24.86 | 47.7 | 0.024 |
| Dadaci[13] (2015) | 33.78 | 26.13, 41.43 | 24.87 | 47.7 | 0.024 |
| Present (2015) | 34.37 | 26.31, 42.43 | 24.67 | 47.3 | 0.026 |
DISCUSSION
Pregnancy is a special period in which great physiological and pathological changes occur, including immunological, hormonal, metabolic, and cardiovascular changes[1]. Vascular changes are particularly notable. Researchers have reported that during pregnancy, vascular resistance begins to decrease during early gestation due to hormonal changes[24]–[25]; decreased vascular resistance may increase blood flow in organs. As is well known, the choroid is a highly vascular structure and has one of the highest ratios of blood flow to tissue volume in the body[26]. We speculate that decreased vascular resistance and the subsequent increase in blood flow in choroidal vessels play a role in the increase of choroidal thickness in pregnant women. Based on this speculation, we conducted a cross-sectional study and performed a Meta-analysis to evaluate macular choroidal thickness in pregnant women and normal nonpregnant women.
The results of the present study showed that the mean SFCT in healthy pregnant women was 344.13±50.94 µm, whereas the mean SFCT in normal nonpregnant women was 315.03±60.57 µm. Choroidal thickness in healthy pregnant women was significantly greater than in normal nonpregnant women. These results are consistent with most previous studies[8],[15],[23]. They are also supported by the results of our Meta-analysis, which showed that SFCT in healthy pregnant women was significantly greater than in normal nonpregnant women, with a pooled WMD of 36.58 µm (95%CI: 28.42 to 44.74). More importantly, the present study used strict recruitment and exclusion criteria. Our data are highly comparable in terms of the patients recruited, with the demographic and baseline characteristics of the groups closely matched. Based on the data, we conclude that macular choroidal thickness in healthy pregnant women is greater than in normal nonpregnant women, which is consistent with what we speculated. However, one study[16], whose subjects comprised 25 healthy pregnant women and 27 nonpregnant women, showed that choroidal thickness was not significantly different between healthy pregnant women and nonpregnant women. This difference may be attributable to the small number of subjects in Takahashi et al's[16] study. It is important to note that in the present study, we measured choroidal thickness in the macular region of nine locations and found that at most locations, choroidal thickness in healthy pregnant women was greater than in normal nonpregnant women, which indicates that the choroid is thickened diffusely in healthy pregnant women.
In this study, the Pearson correlation analysis showed that the mean choroidal thickness within the macula has a negative correlation with axial length and age in both healthy pregnant women and normal nonpregnant women. These correlations are consistent with the findings of previous studies with respect to healthy subjects[27]–[29]. The result of our study implied that despite the increase of choroidal thickness in healthy pregnant women, the overall trend of physiological change is toward equilibrium.
We also performed a Meta-analysis to evaluate the difference in SFCT between pregnant women and normal nonpregnant women. The pooled results showed that a significant difference in SFCT was detected between pregnant and normal nonpregnant women, with a WMD of 33.66 µm (95%CI: 26.16 to 41.15). Our significant findings were reflected in the Meta-analysis. In the Meta-analysis, some studies included pregnant women with preeclampsia, which is characterized by systemic vascular changes leading to new-onset hypertension[30]. We therefore stratified the pregnant women group into a healthy pregnant women subgroup and a preeclampsia subgroup. Interestingly, the pooled results showed that choroidal thickness in healthy pregnant women was greater than in normal nonpregnant women but that it is not greater in pregnant women with preeclampsia than in normal nonpregnant women. Regarding this finding, it has been shown that in the case of preeclampsia, blood pressure is always elevated and systemic vascular resistance is increased, which might impact blood flow into the choroid and affect choroidal thickness. Furthermore, as a previous study showed, plasma volume expansion and blood volume increase starts in the first trimester and reaches maximum levels in the third trimester[31]. The studies included in the Meta-analysis contained different trimesters, which might have affected choroidal thickness. However, the stratification analysis showed that different trimesters exhibited similar results, which are less prone to chance results and indicate the robustness of our findings. In addition, in order to gain reliable results, sensitivity analyses were performed by excluding each individual study in turn. This procedure did not greatly change the pooled results, which supported the reliability and the stability of this Meta-analysis.
We first conducted a cross-sectional study and then performed a Meta-analysis to evaluate macular choroidal thickness in pregnant women and normal nonpregnant women. Nevertheless, we recognize that the Meta-analysis has some limitations. First, significant heterogeneity existed in the studies. However, the sensitivity analysis found that two studies were the main source of this heterogeneity, and when we excluded them, the remaining studies still showed similar results. Second, the eligibility criteria for inclusion of cases were different among the studies. For instance, some studies included first-trimester data, whereas others included third-trimester data. However, subgroup analyses by trimester did not alter the pooled results. Third, the measurements of choroidal thickness were performed manually in the studies, and automated software is required for a more objective evaluation. However, previous research has demonstrated that choroidal thickness measurement using EDI-OCT is highly reproducible and repeatable[32]–[33]. Fourth, since the subjects in this study were all young adults, there was a lack of data from older subjects. However, the young pregnant adults had the basic characteristics of choroidal thickness typically found in pregnant women.
Despite these limitations, this study has some important advantages. First, it is the first synthesis to explore choroidal thickness in pregnant women and provides the most up-to-date information in this area. Second, the results of our cross-sectional study were consistent with those of the corresponding Meta-analysis. Third, our results are less prone to selection and publication bias, which ensures that the conclusions are more objective and reliable.
Taken together, our results and the comprehensive Meta-analysis suggest that choroidal thickness in pregnant women is greater than in normal nonpregnant women, even across different subgroups.
Acknowledgments
Foundation: Supported by the First People's Hospital of Chenzhou (No. N2014-009).
Conflicts of Interest: Liu R, None; Kuang GP, None; Luo DX, None; Lu XH, None.
REFERENCES
- 1.Tan EK, Tan EL. Alterations in physiology and anatomy during pregnancy. Best Pract Res Clin Obstet Gynaecol. 2013;27(6):791–802. doi: 10.1016/j.bpobgyn.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Chawla S, Chaudhary T, Aggarwal S, Maiti GD, Jaiswal K, Yadav J. Ophthalmic considerations in pregnancy. Med J Armed Forces India. 2013;69(3):278–284. doi: 10.1016/j.mjafi.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akar Y, Yucel I, Akar ME, Zorlu G, Ari ES. Effect of pregnancy on intraobserver and intertechnique agreement in intraocular pressure measurements. Ophthalmologica. 2005;219(1):36–42. doi: 10.1159/000081781. [DOI] [PubMed] [Google Scholar]
- 4.Weinreb RN, Lu A, Beeson C. Maternal corneal thickness during pregnancy. Am J Ophthalmol. 1988;105(3):258–260. doi: 10.1016/0002-9394(88)90006-2. [DOI] [PubMed] [Google Scholar]
- 5.Park SB, Lindahl KJ, Temnycky GO, Aquavella JV. The effect of pregnancy on corneal curvature. CLAO J. 1992;18(4):256–259. [PubMed] [Google Scholar]
- 6.Chen HC, Newsom RS, Patel V, Cassar J, Mather H, Kohner EM. Retinal blood flow changes during pregnancy in women with diabetes. Invest Ophthalmol Vis Sci. 1994;35(8):3199–3208. [PubMed] [Google Scholar]
- 7.Goktas S, Basaran A, Sakarya Y, Ozcimen M, Kucukaydin Z, Sakarya R, Basaran M, Erdogan E, Alpfidan I. Measurement of choroid thickness in pregnant women using enhanced depth imaging optical coherence tomography. Arq Bras Oftalmol. 2014;77(3):148–151. doi: 10.5935/0004-2749.20140038. [DOI] [PubMed] [Google Scholar]
- 8.Atas M, Acmaz G, Aksoy H, Demircan S, Atas F, Gulhan A, Zararsiz G. Evaluation of the macula, retinal nerve fiber layer and choroid in preeclampsia, healthy pregnant and healthy non-pregnant women using spectral-domain optical coherence tomography. Hypertens Pregnancy. 2014;33(3):299–310. doi: 10.3109/10641955.2013.877924. [DOI] [PubMed] [Google Scholar]
- 9.Hamzah F, Shinojima A, Mori R, Yuzawa M. Choroidal thickness measurement by enhanced depth imaging and swept-source optical coherence tomography in central serous chorioretinopathy. BMC Ophthalmol. 2014;14:145. doi: 10.1186/1471-2415-14-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang W, Wang W, Zhou M, Chen S, Gao X, Fan Q, Ding X, Zhang X. Peripapillary choroidal thickness in healthy Chinese subjects. BMC Ophthalmol. 2013;13:23. doi: 10.1186/1471-2415-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirooka K, Tenkumo K, Fujiwara A, Baba T, Sato S, Shiraga F. Evaluation of peripapillary choroidal thickness in patients with normal-tension glaucoma. BMC Ophthalmol. 2012;12:29. doi: 10.1186/1471-2415-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou M, Wang W, Ding X, Huang W, Chen S, Laties AM, Zhang X. Choroidal thickness in fellow eyes of patients with acute primary angle-closure measured by enhanced depth imaging spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54(3):1971–1978. doi: 10.1167/iovs.12-11090. [DOI] [PubMed] [Google Scholar]
- 13.Dadaci Z, Alptekin H, Oncel Acir N, Borazan M. Changes in choroidal thickness during pregnancy detected by enhanced depth imaging optical coherence tomography. Br J Ophthalmol. 2015;99(9):1255–1259. doi: 10.1136/bjophthalmol-2014-306343. [DOI] [PubMed] [Google Scholar]
- 14.Garg A, Wapner RJ, Ananth CV, Dale E, Tsang SH, Lee W, Allikmets R, Bearelly S. Choroidal and retinal thickening in severe preeclampsia. Invest Ophthalmol Vis Sci. 2014;55(9):5723–5729. doi: 10.1167/iovs.14-14143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kara N, Sayin N, Pirhan D, Vural AD, Araz-Ersan HB, Tekirdag AI, Yildirim GY, Gulac B, Yilmaz G. Evaluation of subfoveal choroidal thickness in pregnant women using enhanced depth imaging optical coherence tomography. Curr Eye Res. 2014;39(6):642–647. doi: 10.3109/02713683.2013.855236. [DOI] [PubMed] [Google Scholar]
- 16.Takahashi J, Kado M, Mizumoto K, Igarashi S, Kojo T. Choroidal thickness in pregnant women measured by enhanced depth imaging optical coherence tomography. Jpn J Ophthalmol. 2013;57(5):435–439. doi: 10.1007/s10384-013-0265-5. [DOI] [PubMed] [Google Scholar]
- 17.Tan CS, Ouyang Y, Ruiz H, Sadda SR. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53(1):261–266. doi: 10.1167/iovs.11-8782. [DOI] [PubMed] [Google Scholar]
- 18.Li D, Zhou M, Peng X, Sun H. Homocysteine, methylenetetrahydrofolate reductase C677T polymorphism, and risk of retinal vein occlusion: an updated meta-analysis. BMC Ophthalmol. 2014;14:147. doi: 10.1186/1471-2415-14-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou M, Wang W, Huang W, Zhang X. Trabeculectomy with versus without releasable sutures for glaucoma: a meta-analysis of randomized controlled trials. BMC Ophthalmol. 2014;14:41. doi: 10.1186/1471-2415-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. [PubMed] [Google Scholar]
- 22.Ulusoy DM, Duru N, Ataş M, Altinkaynak H, Duru Z, Açmaz G. Measurement of choroidal thickness and macular thickness during and after pregnancy. Int J Ophthalmol. 2015;8(2):321–325. doi: 10.3980/j.issn.2222-3959.2015.02.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sayin N, Kara N, Pirhan D, Vural A, Araz Ersan HB, Tekirdag AI, Polat I, Gulac B, Yilmaz G. Subfoveal choroidal thickness in preeclampsia: comparison with normal pregnant and nonpregnant women. Semin Ophthalmol. 2014;29(1):11–17. doi: 10.3109/08820538.2013.839813. [DOI] [PubMed] [Google Scholar]
- 24.Gaillard R, Bakker R, Willemsen SP, Hofman A, Steegers EA, Jaddoe VW. Blood pressure tracking during pregnancy and the risk of gestational hypertensive disorders: the Generation R Study. Eur Heart J. 2011;32(24):3088–3097. doi: 10.1093/eurheartj/ehr275. [DOI] [PubMed] [Google Scholar]
- 25.Duvekot JJ, Peeters LL. Maternal cardiovascular hemodynamic adaptation to pregnancy. Obstet Gynecol Surv. 1994;49(12 Suppl):S1–14. doi: 10.1097/00006254-199412011-00001. [DOI] [PubMed] [Google Scholar]
- 26.Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res. 2010;29(2):144–168. doi: 10.1016/j.preteyeres.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maul EA, Friedman DS, Chang DS, Boland MV, Ramulu PY, Jampel HD, Quigley HA. Choroidal thickness measured by spectral domain optical coherence tomography: factors affecting thickness in glaucoma patients. Ophthalmology. 2011;118(8):1571–1579. doi: 10.1016/j.ophtha.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hirata M, Tsujikawa A, Matsumoto A, Hangai M, Ooto S, Yamashiro K, Akiba M, Yoshimura N. Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52(8):4971–4978. doi: 10.1167/iovs.11-7729. [DOI] [PubMed] [Google Scholar]
- 29.Ouyang Y, Heussen FM, Mokwa N, Walsh AC, Durbin MK, Keane PA, Sanchez PJ, Ruiz-Garcia H, Sadda SR. Spatial distribution of posterior pole choroidal thickness by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52(9):7019–7026. doi: 10.1167/iovs.11-8046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–1131. doi: 10.1097/01.AOG.0000437382.03963.88. [DOI] [PubMed] [Google Scholar]
- 31.Thornburg KL, Jacobson SL, Giraud GD, Morton MJ. Hemodynamic changes in pregnancy. Semin Perinatol. 2000;24(1):11–14. doi: 10.1016/s0146-0005(00)80047-6. [DOI] [PubMed] [Google Scholar]
- 32.Shao L, Xu L, Chen CX, Yang LH, Du KF, Wang S, Zhou JQ, Wang YX, You QS, Jonas JB, Wei WB. Reproducibility of subfoveal choroidal thickness measurements with enhanced depth imaging by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54(1):230–233. doi: 10.1167/iovs.12-10351. [DOI] [PubMed] [Google Scholar]
- 33.Rahman W, Chen FK, Yeoh J, Patel P, Tufail A, Da Cruz L. Repeatability of manual subfoveal choroidal thickness measurements in healthy subjects using the technique of enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52(5):2267–2271. doi: 10.1167/iovs.10-6024. [DOI] [PubMed] [Google Scholar]