Abstract
Over the past decade there have been increasing reports of atypical femoral fractures (AFFs) associated with bisphosphonate use. Reported cases of bilateral involvement usually refer to sequential injuries, or a complete fracture with an incomplete injury to the contralateral limb. In this case report we describe simultaneous, bilateral, complete atypical femoral fractures following a simple fall. A history of prodromal pain, previous radiological evidence of cortical thickening and long term alendronate therapy for osteoporosis secondary to corticosteroid treatment paint a classical picture of the presentation of an atypical fracture pattern of which orthopaedic surgeons should be aware.
Keywords: Atypical femoral fracture, Bisphosphonate fracture, Subtrochanteric fracture
1. Introduction
Bisphosphonates have been widely used for the treatment of osteoporosis in men, postmenopausal women and those on glucocorticoid therapy to reduce bone loss and reduce fracture risk. Over the past decade there have been increasing reports of atypical femoral fractures (AFFs) associated with bisphosphonate use.1, 2, 3, 4 Many of these case reports highlight contralateral femoral changes seen on presentation or follow up and recommendations range from prophylactic surgical treatment with a locked cephalo-medullary nail, to medication holiday, protected weight bearing and observation. To the best of our knowledge there has only been a single published report of bilateral, simultaneous, AFFs in 2012.5 Anecdotally there appears to be an increased rate of presentation of this sub group of injury and this case highlights the classical features of this disease.
2. Case presentation
A 71-year-old white British female presented to Accident and Emergency following a fall from standing height onto her buttocks whilst out walking. She had acute pain in both proximal femora and initial investigations revealed bilateral complete subtrochanteric femoral fractures (see Fig. 1). Both injury patterns showed a transverse lateral cortical fracture with minimal comminution, with a short spiral fracture on the right and a short oblique fracture on the left with medial spike (Fig. 3, white arrow). There was evidence of periosteal reaction and endosteal beaking at the site of lateral fracture (Fig. 3, black arrow), along with generalised cortical thickening of the femora bilaterally.
Fig. 1.
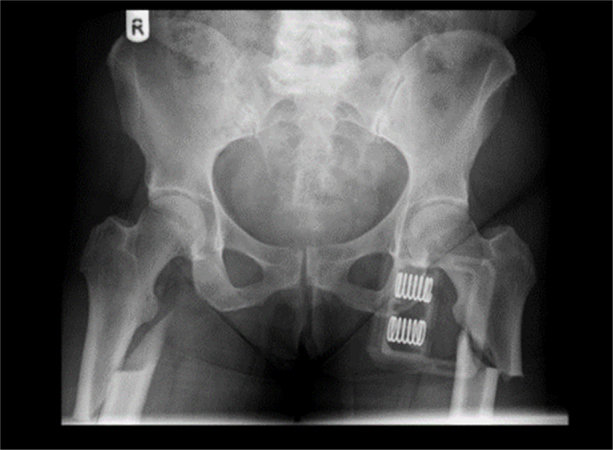
AP Pelvis XR on admission on skin traction.
Fig. 3.
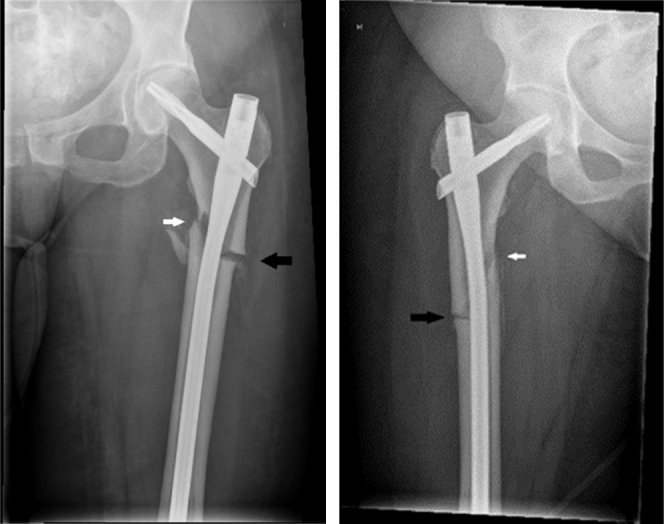
AP Femur X-rays following osteosynthesis, demonstrating features of atypical fracture.
Medical history included pulmonary sarcoid, for which she had been on prednisolone treatment for 18 years, and she had been taking bone protection in the form of weekly Alendronate 70 mg and daily Calcium replacement for 8 years since a DEXA scan confirmed osteoporosis. There was no history of weight loss, myeloma screen and breast examination were normal, and CT Chest/Abdomen/Pelvis showed no evidence of malignancy. Her calcium, 25(OH)D and phosphate levels were all in normal range.
She described bilateral thigh pain for 2–3 months prior to the fall and had seen her GP who had advised activity modification and simple analgesia. A previous Pelvic X-ray had been requested in 2014 due to bilateral hip pain and retrospectively there was evidence of subtle cortical thickening bilaterally at the site of the subsequent fractures (see Fig. 2, Fig. 3).
Fig. 2.

AP Pelvis XR in 2014.
The patient underwent osteosynthesis with consecutive cephalo-medullary femoral nails under a single anaesthetic. She was monitored closely in theatre and transfused 2 units of blood intra-operatively to account for fluid losses. Lactate levels and cardiovascular parameters remained stable and she tolerated the procedure well.
Post-operatively she underwent early mobilisation and review with ortho-geriatrician. Alendronate was stopped and she was commenced on vitamin D and calcium replacement therapy.
3. Discussion
In response to worry from patients and physicians, a working group of the European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis and the International Osteoporosis Foundation reviewed the evidence relating to bisphosphonate use and an association with AFFs in 2010.6 They advised a sense of proportion when considering the relative risks and benefits, pointing out that the risk-benefit ratio remains heavily weighted towards continued use of bisphosphonates. However, they urged physicians to discuss these risks with their patients and remain vigilant for early signs of atypical fractures.
In 2014 the American Society for Bone and Mineral Research (ASBMR) published an update to their own earlier guidelines.7 They confirmed that the epidemiological evidence for a relationship between bisphosphonates and AFFs had become more compelling, suggesting long term use (more than 3 years) could be associated with an incidence of 100 cases per 100,000 person-years. The exact pathogenesis of these fractures remains uncertain, but the unique fracture pattern shows characteristics of stress reactions and brittle failure. Current evidence suggests bisphosphonates may negatively impact collagen maturation within bone, as well as reducing bone turnover leading to reduced toughness and accumulation of stress damage from cyclical loading.8, 9 This can in turn lead to development of stress fractures and the suppression of normal bone remodelling directly impairs the primary mechanism by which these fractures heal.
The ASBMR produced a list of major and minor features of AFFs and advised that for the purposes of case definition, at least 4 of the major features should be present (see Table 1). Our case exhibited all 5 of the major features, and many of the minor features and thus we can predict that this injury may be slow to heal and require careful follow up. She will also benefit from specific input from the orthogeriatricians regarding her medical management. There is a general consensus of opinion that, unlike when managing routine fragility fractures, anti-resorptive medications should be stopped in the event of diagnosing an atypical fracture and vitamin D and calcium levels should be checked and appropriately replaced. In the event of complete fractures, the need for surgical management is clear, but in incomplete fractures there has been some debate about optimal treatment. With functional pain there has been a tendency towards prophylactic surgical fixation with cephalomedullary nails, but over recent years there has been some anecdotal evidence supporting the use of teriparatide alongside cessation of anti-resorptive medication and protected weight-bearing to hasten healing. This remains controversial and further randomised controlled trials are needed.
Table 1.
Diagnostic features of atypical femoral fractures.
| Major features | Minor features |
|---|---|
| Fracture associated with minimal or no trauma, e.g. fall from standing height or less | Generalised increase in cortical thickness of the femoral diaphyses |
| Fracture line originates at the lateral cortex and is transverse in orientation, although it may become oblique as it progresses medially across the femur | Unilateral or bilateral prodromal symptoms such as dull or aching pain in the groin or thigh |
| Complete fractures extend through both cortices and may be associated with a medial spike; incomplete fractures involve only the lateral cortex | Bilateral incomplete or complete femoral diaphysis fractures |
| Fracture is non-comminuted or minimally comminuted | Delayed fracture healing |
| Localised periosteal or endosteal thickening of the lateral cortex is present at the fracture site (“beaking” or “flaring”) |
A key recommendation remains awareness and vigilance amongst patients and healthcare providers. Although cases remain rare, the large numbers of patients treated with bisphosphonates in the UK make AFFs increasingly common and classically the condition is bilateral with prodromal pain. Patients on long term bisphosphonate treatment who complain of hip or thigh pain require prompt imaging of the entire length of both femurs with a high index of suspicion for these atypical fractures. Early diagnosis and management is likely to reduce morbidity and potentially can avoid the need for surgical procedures in this fragile patient group.
Authors’ contributions
Mark Higgins was responsible for case selection, literature review and writing of the case report. Sam Morgan-John and Sachin Badhe were responsible for obtaining history from patient, consenting patient, providing senior supervision and proof reading the case report.
Conflicts of interest
The authors have none to declare.
References
- 1.Capeci C.M., Tejwani N.C. Bilateral low-energy simultaneous or sequential femoral fractures in patients on long-term alendronate therapy. J Bone Jt Surg Am. 2009;91:2556–2561. doi: 10.2106/JBJS.H.01774. [DOI] [PubMed] [Google Scholar]
- 2.Cermak K., Shumelinsky F., Alexiou J., Gebhart M.J. Case reports: subtrochanteric femoral stress fractures after prolonged alendronate therapy. Clin Orthop Relat Res. 2009;468:1991–1996. doi: 10.1007/s11999-009-1192-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson R.N., Phillips J.R., McCauley S.H., Elliott J.R., Moran C.G. Atypical femoral fractures and bisphosphonate treatment. J Bone Jt Surg Br. 2012;94-B(3):385–390. doi: 10.1302/0301-620X.94B3.27999. [DOI] [PubMed] [Google Scholar]
- 4.Isaacs J.D., Shidiak L., Harris I.A., Szomor Z.L. Femoral insufficiency fractures associated with prolonged bisphosphonate therapy. Clin Orthop Relat Res. 2010;468:3384–3392. doi: 10.1007/s11999-010-1535-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zafeiris C.P., Stathopoulos I.P., Kourkoumelis G., Gkikas E., Lyritis G.P. Simultaneous bilateral atypical femoral fractures after alendronate therapy. J Musculoskelet Neuronal Interact. 2012;12(4):262–264. [PubMed] [Google Scholar]
- 6.Rizzoli R., Åkesson K., Bouxsein M. Subtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group Report. Osteoporosis Int. 2011;22(2):373–390. doi: 10.1007/s00198-010-1453-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shane E., Burr D., Abrahamsen B. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29:1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 8.Allen M.R., Reinwald S., Burr D.B. Alendronate reduces bone toughness of ribs without significantly increasing microdamage accumulation in dogs following 3 years of daily treatment. Calcif Tissue Int. 2008;82:354–360. doi: 10.1007/s00223-008-9131-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burr D.B., Liu Z., Allen M.R. Duration-dependent effects of clinically relevant oral alendronate doses on cortical bone toughness in beagle dogs. Bone. 2015;71(February):58–62. doi: 10.1016/j.bone.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


