Abstract
AIM
To review the results of our experience with the Medartis Aptus plating system for four corner arthrodesis of the wrist, which uses a combination of compression screws and variable angle locking screws.
METHODS
We reviewed the results of 17 procedures in 16 patients that underwent scaphoid excision and four corner fusion using the Medartis Aptus system between May 2010 and June 2014. The primary outcome measure was radiographic and clinical union.
RESULTS
The mean clinical follow up time was 20.6 mo. The mean union time was 6 mo. Two non-unions required revision procedures. The mean disabilities of the arm, shoulder and hand score taken after union was 36. The mean final grip strength was 27 kg. The mean final range of movement was 30° flexion and 31° of extension. All patients had a restored scapholunate angle on postoperative radiographs. There were no incidences of dorsal impingement.
CONCLUSION
Overall our experience with the Aptus plating system shows comparable results to other methods of fixation for four corner fusion, in the short to medium term.
Keywords: Wrist surgery, Arthrodesis, Locking plate, Scaphoidectomy, Partial fusion
Core tip: This paper demonstrates that a multi angle locking plate is a suitable device for four corner fusion. It demonstrates that results are comparable to those of other means of fusion in the short to medium term.
INTRODUCTION
Scaphoidectomy with four corner fusion is a well recognised surgical option for scapholunate advanced collapse (SLAC) and scaphoid non-union advanced collapse (SNAC) when the radio-lunate joint is preserved[1]. Multiple fixation options have been employed including K wires, headless screws, staples and plates[2-4]. Many techniques have been associated with significant complications. Circular “hub-cap” plates in particular have been associated with complications such as non-union and dorsal plate impingement[3,5]. In response to this, newer implants are increasingly being trialled including memory staples and plates with newer designs such as the carpal fusion plate[6,7]. Medartis™ (Basel, Switzerland) have designed the APTUS™ four corner fusion plate with some design variations compared to previous plates aimed at improving union rates and decrease dorsal impingement. Results of this plate have not previously been reported in the literature.
MATERIALS AND METHODS
A retrospective review of cases undergoing treatment with the Medartis APTUS™ Four Corner Fusion plate was performed in our unit. Cases performed at The University Hospital Birmingham and the Royal Orthopaedic Hospital were identified from a review of operating logs between May 2010 and June 2016, and the patients reviewed. Indications for surgery, associated procedures, pre-operative radiographic deformity and lunate type in particular were noted. Time to union, complications and need for further surgery were also assessed. At follow up patients also had their wrist range of movement assessed with flexion and extension measured according to the method described by Kendal et al[8] with a goniometer placed dorsally over the wrist and flexion measured on the ulnar border of the wrist. Grip strength was measured using a dynamometer (Jamar dynamometer; Sammons Preston Roylan, Bollingbrook Illinois) with the best grip strength of three trials of each surgically treated wrist compared with that of the opposite wrist (except in the one case of bilateral four corner fusion). A disabilities of the arm, shoulder and hand (DASH) score survey was also performed. All assessments were performed by four consultant hand surgeons within the 2 hospitals.
The study met the requirements of our hospital Institutional Review Board for clinical research. None of the authors have any conflict of interest to declare.
Surgical technique
All surgeries were performed by one of four hand surgeons at the Birmingham Hand Centre (which entails a group of hand surgeons working at both hospitals). All surgeons used the same dorsal approach under tourniquet control following intravenous antibiotics. A regional block was used in all cases except when iliac crest bone graft was taken. In all cases a dorsal 3-4 approach through the extensor retinaculum was used. A dorsal wrist ligament preserving approach was used, extending up along the radial styloid[9]. The radio-lunate articular surfaces were assessed either by arthroscopy or direct vision to ensure the joint was well preserved. The scaphoid was excised and where possible used for bone graft. A radial styloidectomy was performed in 1 case. The interfacing chondral surfaces of the four bones were denuded with a nibbler, curved periosteal elevator and osteotome leaving the very volar aspects untouched to maintain the normal gap between adjacent bones. Where subchondral bone was sclerotic, further holes were created with a K wire to allow maximal bone bleeding.
K wires were inserted into the carpal bones to realign the capitate and lunate and if necessary stabilise the hamate and triquetrum (only required about half the time). This was performed in 2 main ways: (1) an antegrade 1.6 mm K wire from radius to lunate (once the radiolunate angle had been corrected by flexion or extension of the wrist) and then advanced onto the capitate once a neutral capito-lunate angle was achieved and the radio-ulna translation corrected (often the capitate tries to slip off the lunate radially); and (2) a retrograde wire is passed between the second and third metacarpal bases with around 20 degrees of elevation off the hand, through the capitate and onto the lunate, which allows correction of any carpal malalignment present. Both K wire insertion methods are technically difficult due to the angles required and in addition the wire needs to be seated palmar in both bones to allow for the subsequent reamer to cut freely.
During K wire introduction it is important to reduce the capitate into the lunate, which can be especially difficult in type 2 lunates in which there is a tendency for the capitate to slip off the lunate radially.
A custom APTUS™ reamer is then placed in the cross of the 4 bones to allow the plate to be countersunk. It is important to ream the bones to equal depths especially on the lunate to allow the plate to be flush of deep to the dorsal lip to avoid dorsal impingement on wrist extension.
In some cases additional dorsal radial or iliac crest graft was taken to pack between the bones and this can be further compressed by reaming on a reverse setting with the bone graft in situ.
Once the plate is seated, inner non-locking compression screws are inserted to secure the four bones. Outer multidirectional (30 degree arc of variability) locking screws were then inserted. However if an angle outside the 30 degree arc is required to gain carpal purchase, a non locking screw can be used in these outer holes. The triquetrum was included in all fusions. An image intensifier was used throughout to check implant and carpal positions.
There was a variation in post-operative immobilisation from wool and crepe to 6 wk in a below elbow plaster (Table 1). If a cast was used for less than 6 wk patients began active mobilisation with a removable thermoplastic splint for comfort. From six weeks post-operative date onwards signs of union were assessed at regular intervals clinically by a lack of tenderness at the fusion site and/or with radiographic evidence of bridging trabeculae between the bones (although this was appreciably difficult due to the multiple overlapping cortices seen on plain radiographs (Figure 1A). Dorsal impingement was identified according to the description of Shindle et al[3] by the patient complaining of a sharp dorsal pain with maximal passive or active wrist extension.
Table 1.
Patient and surgery characteristics, time to union and follow up
| Number | Age | Sex | Hand | Classification | Lunate type | VISI/ DISI | Associated surgery | No. of screws | Union (mo) | Complications | Follow up (mo) |
| 1a | 64 | M | L | SLAC | 1 | PIN | 11 | 4 | 30 | ||
| 1b | 65 | M | R | SLAC | 1 | PIN | 11 | 6 | 24 | ||
| 2 | 52 | F | R | SLAC | 2 | V | PIN | 12 | 3 | 10 | |
| 3 | 40 | M | L | SLAC | 1 | D | Distal radius graft (previous PIN) | 12 | 9 | 11 | |
| 4 | 38 | M | L | SNAC | 1 | D | PIN + styloidectomy | 11 | 16 | Screws Penetrating CMC joint | 35 |
| 5 | 72 | F | L | SNAC | 1 | D | PIN + Iliac BG | 8 | 3 | 8 | |
| 6 | 55 | M | L | SNAC | 2 | D | PIN + distal radius graft | 11 | 2 | 18 | |
| 7 | 61 | M | R | SNAC | 2 | D | PIN + distal radius graft | 11 | 3 | 10 | |
| 8 | 33 | M | L | Lunate fracture | 1 | V | PIN | 12 | 171 | Non-union, revised | 23 |
| 9 | 35 | M | L | SNAC | 2 | PIN | 11 | 7 | Hypertrophic bone | 16 | |
| 10 | 50 | M | R | SNAC | 2 | PIN | 10 | 6 | Scar sensitivity | 25 | |
| 11 | 55 | M | L | SNAC | 1 | PIN | 10 | 4 | 26 | ||
| 12 | 46 | M | L | SNAC | 2 | D | PIN | 12 | 7 | 25 | |
| 13 | 48 | F | L | SNAC | 1 | D | PIN | 12 | 5 | 25 | |
| 14 | 40 | M | R | SNAC | 2 | PIN | 12 | 8 | Skin necrosis over plate + flap coverage | 24 | |
| 15 | 18 | M | R | Scaphoid | 2 | PIN, plate removal distal radius graft | 10 | 9 | 16 | ||
| 16 | 50 | M | R | SLAC | 1 | PIN | 12 | 271 | Non-union, revised | 27 |
Indicatates total time to final union including both index procedure and revision surgery. PIN: Posterior interosseous neurectomy; M: Male; F: Female; L: Left; R: Right; SLAC: Scapholunate advanced collapse; SNAC: Scaphoid nonunion advanced collapse; V: VISI; D: DISI; BG: Bone graft; CMC: Carpometacarpal.
Figure 1.

A posterior-anterior (A) and lateral (B) view of a typical Scapholunate advanced collapse wrist prior to undergoing four corner fusion.
RESULTS
Seventeen procedures were performed on sixteen patients, 13 men and 3 women. The demographic data of the patients is included in Table 1. The mean age of the patients was 48 years (range 18-72 years). Ten operations were on a left wrist, seven on a right wrist. The indications were SLAC grade 2 in three wrists, grade 3 in two wrists and SNAC in ten wrists. One case was a salvage procedure for a failed fixation of a scaphoid fracture, another was a salvage procedure for a lunate fracture. Typical pre-operative appearances are shown in Figure 1.
The mean follow up time was 20.6 mo (range 8-35). Excluding the two non-unions that required revision procedures, the mean time to union on radiographic and clinical assessment was 6 mo (range 3-16). All fusions ultimately united including the two that required revision surgery. One case united after 16 mo but multiple screws were found to have broken during the follow up period. This patient went on to undergo metalwork removal as one screw penetrated the fifth carpometacarpal joint.
The final range of movement was invariably reduced compared to the contralateral side. The mean final flexion was 30 degrees (20-45) and the mean final extension was 31 degrees (10-60). There were no instances of dorsal impingement from the plate. Post-operative radiographs for a number of patients were taken in full wrist extension, and these demonstrated the ability of the plate to remain deep to the dorsal lip of the radius in extension (Figure 1A).
All patients had a restored scapholunate angle on postoperative radiographs (Mean = 60°). The mean capitolunate angle was 3° (range: 15°-3°)
Typical post-operative X-ray and computed tomography appearances are shown in Figures 2 and 3.
Figure 2.
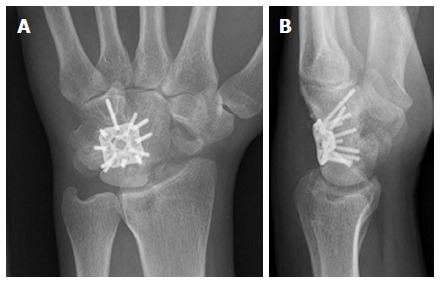
A posterio-anterior (A) and lateral (B) view of the plate in its final position.
Figure 3.
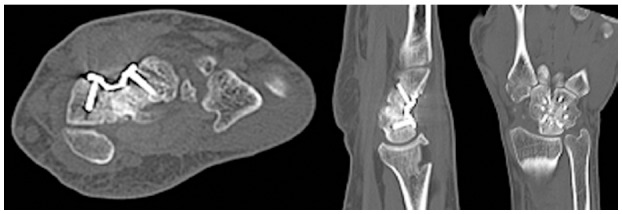
Coronal, Sagittal and axial, postoperative views following plate application and fusion.
The mean final grip strength was 27 kg (range: 4-48) which represented 72% (22%-129%) of the unaffected side. The mean DASH score at the latest follow up was 32 (13-61).
Table 2 shows that all but two patients managed to return to their previous occupation.
Table 2.
Outcomes at discharge or at latest follow up
| Number | JAMAR (kg) (unaffected) | % grip strength difference | Flexion (unaffected) | Extension (unaffected) | DASH | Return to work | Satisfied? |
| 1a | 22 | NA | 30 | 20 | 43 | Retired | Yes |
| 1b | 24 | NA | 25 | 40 | 43 | Retired | Yes |
| 2 | 11 (26) | 42% | 25 (50) | 15 (40) | 48 | Office | Yes |
| 3 | 30 (36) | 83% | 45 | 45 | 15 | Office | Yes |
| 4 | 32 (37) | 87% | 35 (92) | 18 (80) | 48 | Heavy manual | Yes |
| 5 | 4 (18) | 22% | 30 | 10 | 35 | Retired | Yes |
| 6 | 48 (32) | 150% | 30 | 45 | 20 | Office | Yes |
| 7 | 25 (38) | 66% | 45 | 45 | 13 | Retired | Yes |
| 8 | 22 (55) | 40% | 30 | 20 | 61 | No | No |
| 9 | 36 (48) | 75% | 20 | 10 | 43 | No | Yes |
| 10 | 30 (40) | 75% | 30 | 60 | 20 | Office | Yes |
| 11 | 18 (52) | 35% | 20 | 20 | 35 | Office | Yes |
| 12 | 26 (35) | 74% | 40 | 40 | 15 | Yes | Yes |
| 13 | 25 (30) | 83% | 20 | 50 | 13 | Manual | Yes |
| 14 | 45 (35) | 129% | 30 | 40 | 42 | No | No |
| 15 | 20 (38) | 53% | 20 | 35 | 15 | Office | Yes |
| 16 | 40 (55) | 73% | 30 | 15 | 27 | Office | Yes |
Data for the unaffected wrist where available are given in brackets. DASH: Disabilities of the arm, shoulder and hand.
Two patients remain unsatisfied at the last follow up for reasons mentioned below. One is awaiting a wrist arthroscopy and the other had skin necrosis around the dorsal wound requiring flap coverage. No additional data are available.
Complications
One patient had broken screws that were impinging on the 5th CMCJ and required removal.
One patient had a very sensitive scar that failed to settle down during the follow up period.
Two patients exhibited radial drift, with the trapezium abutting the radius on post operative radiographs. Neither had any associated clinical symptoms. A further patient had an area of skin necrosis over the dorsal wrist incision site and required debridement and a radial forearm flap to cover the soft tissue defect. He has made a good functional recovery but is significantly affected by the cosmetic appearance of his wrist.
Two patients failed to unite by 15 mo and were therefore revised with the same implant. Both went onto unite successfully. One of these patients has returned to work and is satisfied, and the other has ongoing ulnar sided wrist pain which is awaiting a wrist arthroscopy.
DISCUSSION
In the setting of SNAC and SLAC wrists, scaphoidectomy and four corner fusions with a plate is very attractive. Compared to fixation techniques such as K wires, four corner fixation plates have the potential advantages of increased stability, higher fusion rates, shorter periods of immobilisation and improved range of motion[8].
The design of the Medartis APTUS™ plate arose from documented concerns with previous circular dorsal plates[3,5]. Complications included radiographic non-union rates as high as 62.5% dorsal impingements as frequent as 25% and an overall complication rate of up to 56%[3,8]. The Medartis™ plate design is low profile (1.4 mm thick) and has variable screw fixation options. The carpus is reamed to allow the plate to sit sunken within the carpal bones, to minimise plate impingement on the dorsal lip of the radius. There was no evidence of dorsal impingement in our study.
The Medartis™ plate (which comes in 2 sizes, 17 and 15 mm diameter) allows compression with central non-locking screws as well as locking screw fixation. Each locking screw can be inserted within a 30 degree arc (locked with a unique Trilock™ system allowing adjustment of the screw angle up to 3 times), this allows for greater adjustment by the surgeon to get optimal bony purchase with the screws. Locking screws are theoretically stronger than traditional screws as was borne out in Kraisarin’s cadaveric study[10]. Locking screws alone may hinder compression at the fusion site and fix the carpus bone in a distracted position[8]. They may also create too rigid a construct to allow interfragmentary motion, a factor which we think occurred in our case when several screws broke. The high fusion rate of implants that allow compression including K wires memory staples and the carpal fusion system plate highlights the need for compression in a four corner fusion[6,7,11].
Hence, by allowing compression prior to locking fixation, the Medartis™ plate appears to promote fusion over previous dorsal plate designs.
All patients in our study reported mild to no pain following surgery, in contrast to Kendall et al[8] but in keeping with other studies[12]. In all cases a PIN neurectomy was performed at the time of surgery, except in one case when the PIN neurectomy had previously been performed. Pain tended to be located over the ulnar side of the wrist in flexion and ulnar deviation.
The patients in our study fixed with the Medartis APTUS™ plate appeared to have a relatively long time to fusion. It is known however that time to union is difficult to diagnose on plain radiographs as the circular plate blocks the area of fusion and hence some authors only diagnose a non-union where a secondary procedure is required[3,8]. Whilst we used clinical assessment to diagnose carpal fusion, this has not been validated. As time to union may not be an objective measurement, it may be that the need for a secondary procedure for fusion as reported by Kendall et al[8] is more useful.
Our mean follow up is just under two years. A long term follow up study of four corner fusions suggests that most complications occur with a two year initial period after which there is long term satisfaction with the procedure[13].
The main limitation with this study, in that, it involved a relatively small retrospective cohort. Furthermore, the addition of pre-operative range of motion, grip strength and DASH scores would have been a useful adjunct to this data. We believe that our data support performing a PIN neurectomy at the time of surgery as well as using an inset circular plate that allows both compression and locking screw fixation of the carpus. With an improvement of wrist plates specifically designed for four corner fusion, there will hopefully be an improvement in the results of four corner fusion to match the high success and low complication rates of total wrist fusion.
COMMENTS
Background
Scaphoidectomy with four corner fusion is a well recognised surgical option for scapholunate advanced collapse (SLAC). A variety of fixation methods have been tried and the newest implants are plates of various designs.
Research frontiers
Many of the current plates have problems with non-union or impingement.
Innovations and breakthroughs
The Medartis Aptus plate has some design variations compared to previous plates aimed at improving union rates and decrease dorsal impingement. These may be achieved through its multiangle locking configuration as well as its cortical screw holes and low profile design.
Applications
This plate is a useful solution for four corner arthrodesis in patients with SLAC or scaphoid non-union advanced collapse.
Terminology
SLAC wrist: Scapholunate advanced collapse.
Peer-review
It is a well written manuscript overall that worth publishing.
Footnotes
Institutional review board statement: The study met the requirements of our hospital Institutional Review Board for clinical research. None of the authors have any conflict of interest to declare.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: None of the individual authors of this paper have any conflicts of interest.
Data sharing statement: No additional data are available for this study. All data are included in the paper itself.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: February 1, 2016
First decision: March 24, 2016
Article in press: June 3, 2016
P- Reviewer: Drampalos E, Vulcano E S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9:358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]
- 2.Vance MC, Hernandez JD, Didonna ML, Stern PJ. Complications and outcome of four-corner arthrodesis: circular plate fixation versus traditional techniques. J Hand Surg Am. 2005;30:1122–1127. doi: 10.1016/j.jhsa.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Shindle MK, Burton KJ, Weiland AJ, Domb BG, Wolfe SW. Complications of circular plate fixation for four-corner arthrodesis. J Hand Surg Eur Vol. 2007;32:50–53. doi: 10.1016/j.jhsb.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 4.Ball B, Bergman JW. Scaphoid excision and 4-corner fusion using retrograde headless compression screws. Tech Hand Up Extrem Surg. 2012;16:204–209. doi: 10.1097/BTH.0b013e3182688c6a. [DOI] [PubMed] [Google Scholar]
- 5.Stanley JK. Re: Mulford JS, Ceulemans LJ, Nam D, Axelrod TS. Proximal row carpectomy vs. four corner fusion for scapholunate (SLAC) or scaphoid nonunion advanced collapse (SNAC) wrists: a systematic review of outcomes. J Hand Surg Eur. 2009, 34: 256-63. J Hand Surg Eur Vol. 2009;34:819–820; author reply 820. doi: 10.1177/1753193408100954. [DOI] [PubMed] [Google Scholar]
- 6.Van Amerongen EA, Schuurman AH. Four-corner arthrodesis using the Quad memory staple. J Hand Surg Eur Vol. 2009;34:252–255. doi: 10.1177/1753193408094444. [DOI] [PubMed] [Google Scholar]
- 7.Allison DM. A new plate for partial wrist fusions: results in midcarpal arthrodesis. J Hand Surg Eur Vol. 2011;36:315–319. doi: 10.1177/1753193410395357. [DOI] [PubMed] [Google Scholar]
- 8.Kendall CB, Brown TR, Millon SJ, Rudisill LE, Sanders JL, Tanner SL. Results of four-corner arthrodesis using dorsal circular plate fixation. J Hand Surg Am. 2005;30:903–907. doi: 10.1016/j.jhsa.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Berger RA. A method of defining palpable landmarks for the ligament-splitting dorsal wrist capsulotomy. J Hand Surg Am. 2007;32:1291–1295. doi: 10.1016/j.jhsa.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 10.Kraisarin J, Dennison DG, Berglund LJ, An KN, Shin AY. Biomechanical comparison of three fixation techniques used for four-corner arthrodesis. J Hand Surg Eur Vol. 2011;36:560–567. doi: 10.1177/1753193411406799. [DOI] [PubMed] [Google Scholar]
- 11.Ashmead D, Watson HK, Damon C, Herber S, Paly W. Scapholunate advanced collapse wrist salvage. J Hand Surg Am. 1994;19:741–750. doi: 10.1016/0363-5023(94)90177-5. [DOI] [PubMed] [Google Scholar]
- 12.Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am. 1995;20:965–970. doi: 10.1016/S0363-5023(05)80144-3. [DOI] [PubMed] [Google Scholar]
- 13.Trail IA, Murali R, Stanley JK, Hayton MJ, Talwalkar S, Sreekumar R, Birch A. The long-term outcome of four-corner fusion. J Wrist Surg. 2015;4:128–133. doi: 10.1055/s-0035-1549277. [DOI] [PMC free article] [PubMed] [Google Scholar]


