Abstract
Study Objectives:
Obstructive sleep apnea (OSA) is common after stroke and predicts poor outcomes. Continuous positive airway pressure (CPAP) treats OSA but is generally poorly tolerated by stroke patients. We assessed whether nasal expiratory positive airway pressure (EPAP), an alternative to CPAP, may be an effective option after acute stroke.
Methods:
We conducted a randomized, controlled, two-period crossover study in which each acute ischemic stroke patient received 1 night of EPAP and 1 night without EPAP while OSA was monitored with a validated device, the Watch-PAT 200. Linear repeated- measures analyses were conducted. Sample size calculations indicated that 18 subjects would be required to detect a 10-point or larger average reduction in the apnea-hypopnea index (AHI, the primary outcome), with use of EPAP, with power ≥ 80% and α = 0.05.
Results:
Among the 19 subjects who completed the protocol, nasal EPAP treatment was associated with a nonsignificant absolute difference in AHI of −5.73 events/h in the primary analysis (p = 0.183, 95% confidence interval −14.4, 2.97) and a nonsignificant absolute difference in AHI of −5.43 events/h in the subgroup of patients who used nasal EPAP for ≥ 3 h (p = 0.314, 95% confidence interval −16.6, 5.76).
Conclusions:
This study suggests that EPAP is not an effective alternative to CPAP in acute stroke patients with OSA. Further work is needed to identify other more effective alternatives.
Clinical Trial Registration:
ClinicalTrials.gov, ID: NCT01703663
Citation:
Wheeler NC, Wing JJ, O'Brien LM, Hughes R, Jacobs T, Claflin E, Chervin RD, Brown DL. Expiratory positive airway pressure for sleep apnea after stroke: a randomized, crossover trial. J Clin Sleep Med 2016;12(9):1233–1238.
Keywords: obstructive sleep apnea, positive pressure respiration, stroke
INTRODUCTION
Obstructive sleep apnea is (OSA) is a serious medical condition that affects the majority of patients with ischemic stroke.1 Sleep apnea is an independent risk factor for stroke, with increase in risk associated with higher apnea-hypopnea index (AHI).2 Moreover, sleep apnea is an important predictor of poor functional outcome after stroke.3,4 Sleep-disordered breathing has been associated with a higher risk of death or dependency 6 months after stroke.3 Many factors likely underlie this association, including detrimental effects of hypoxia on brain recovery5 and the effects of poor sleep quality and daytime somnolence on patient participation with rehabilitation.
Although the negative effects of OSA on stroke recovery have been demonstrated, the benefits of OSA treatment have not been definitively tested. The most effective therapy for OSA outside the context of stroke is continuous positive airway pressure (CPAP), but adherence to this therapy historically has been particularly poor in stroke patients.1,6,7 For example, one 2006 study evaluating nasal CPAP after stroke found generally poor acceptance rates for nasal CPAP initiated during stroke unit hospitalization,8 with reasons including family/caregiver discomfort with the practical requirements for CPAP use, cognitive dysfunction or sundowning, and inability of patients with motor deficits to adjust this equipment. Positional therapy has been studied as a possible substitute for positive pressure treatment of sleep apnea after stroke,9 but with only moderate improvements in sleep apnea severity. Other alternatives to CPAP have not been studied in this population.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Obstructive sleep apnea (OSA) is widely prevalent after ischemic stroke and is associated with higher mortality and worsened outcomes, but stroke patients as a group may not tolerate conventional continuous positive airway pressure (CPAP). This study was designed to test the effects of nasal expiratory positive airway pressure (EPAP) within this important population.
Study Impact: This study supports the feasibility of diagnostic and clinical interventions for OSA during acute hospitalizations after stroke, but suggests that EPAP is not likely to treat OSA effectively in acute stroke patients intolerant to CPAP. Alternatives to CPAP and EPAP should be identified.
A simpler and possibly more tolerable alternative to CPAP is expiratory positive airway pressure (EPAP), which has been shown to reduce apneas in the general population.10,11 EPAP is provided by disposable valves, applied nightly to the nares; the valves provide resistance on expiration but little or no resistance on inspiration. Given the high prevalence of OSA, poor CPAP adherence after stroke, absence of a highly effective alternative approach to treatment of OSA in the poststroke setting, and promising preliminary findings with EPAP therapy in nonstroke patients, we tested whether EPAP use may be tolerable and effective to reduce OSA severity specifically in acute stroke patients.
METHODS
We prospectively recruited alert subjects age 18 y or older who were admitted to the inpatient neurology service at the University of Michigan with an ischemic stroke, including transient ischemic attack with infarct,12 within the previous 14 days (ClinicalTrials.gov identifier: NCT01703663). The study protocol was approved by the University of Michigan Institutional Review Board. After consent from the patient or surrogate, study subjects were monitored on 2 consecutive nights with the Watch-PAT 200 (Itamar Medical, Israel), an FDA-approved portable diagnostic device consisting of a finger-mounted peripheral arterial tonometry (PAT) probe, a wrist-mounted device, and oxygen saturation monitor, without snoring monitor. The Watch-PAT 200 has been well validated against standard in-laboratory polysomnography.13–15 The device records PAT, heart rate, oxygen saturation, and actigraphy, which are then analyzed by device software. The PAT detects episodes of upper airway obstruction indirectly through identification of altered sympathetic tone, whereas actigraphy data are used to distinguish sleep versus wakefulness and estimate sleep time. A respiratory event is identified by any of three criteria in an attempt to approximate diagnostic criteria for clinical research16: (1) a PAT amplitude reduction with corresponding increase in pulse rate or in wrist activity, (2) a PAT amplitude reduction with a ≥ 3% oxygen desaturation, or (3) a ≥ 4% oxygen desaturation. An AHI is calculated as the number of respiratory events per hour of sleep.
The Watch-PAT was particularly well suited for this research because it does not require a nasal pressure or airflow sensor, which may be ineffective during use of EPAP.17 Patients were determined to have OSA if they had an AHI ≥ 5 on either the treatment night or the control night. Only data obtained during sleep time, based on Watch-PAT actigraphy data, were included in AHI calculations.
The study intervention consisted of nasal EPAP administered with the Provent device (Ventus Medical, Inc., Manchester, NH, now owned by Theravent, Inc.). Provent consists of two single-use valves (one in each nostril) held in place with an adhesive ring. This intervention was administered following a randomized, controlled, two-period crossover design (AB/BA) in which each patient underwent 1 night of EPAP and 1 night without EPAP, randomized to the order of treatment on a 1:1 basis. Two consecutive nights were used to limit the period effect, as OSA can improve over weeks to months after an acute stroke.
Other than age and presence of acute ischemic stroke, there were no other specific criteria for inclusion into the study population and initiation of the EPAP protocol. Exclusion criteria included contraindications identified by the Provent manufacturer, specifically known severe cardiopulmonary comorbidities such as heart disease, acute respiratory infection, pneumothorax, bullous lung disease, or other chronic respiratory disorders. Patients with medical comorbidities that preclude use of nasal EPAP, including transnasal tubes or current use of mechanical ventilation, CPAP, or supplemental oxygen, were also excluded. Other exclusion criteria included factors that affect accuracy of the WatchPAT, including use of alpha blockers or short acting nitrates, a permanent pacemaker, or sustained nonsinus arrhythmia.
A priori sample size calculations determined that at least 18 subjects were needed to detect a 10-point difference in the AHI with a power ≥ 80%, α = 0.05, and a two-sided test, based on the assumption that the within-patient standard deviation of AHI (based on night-to-night variability) is 10.18 The required sample size in crossover trials is typically substantially reduced compared with parallel group trials because between-subject variability is eliminated as subjects serve as their “own control.”19 The primary pre-specified study outcome variable was AHI. Prespecified secondary outcomes included mean and minimum oxygen saturation and an oxygen desaturation index calculated as the number of oxygen desaturations of ≥ 4% per hour of sleep time. Other exploratory outcomes included sleep efficiency (the amount of sleep time divided by the total recording time). The treatment effect of EPAP on AHI, oxygen saturation, and time spent asleep were estimated using a linear repeated-measures model, which accounts for the correlation of repeated measures within the same subject. A treatment-by-period interaction was planned to assess for crossover effect. The treatment-by-period interaction was non-significant and therefore was dropped from all models. Primary analyses were performed using an intention-to-treat analysis, which included, as part of the prespecified analysis plan, all patients who had an AHI ≥ 5 during at least 1 of the 2 nights (either the control night or the intervention night, or on both nights). Sensitivity analyses were conducted for two subgroups: (1) excluding those with AHI ≥ 5 on the intervention night but AHI < 5 on the control night, and (2) excluding those with fewer than 3 h of self-reported use of EPAP. Descriptive statistics were used to assess self-reported measures reported on a questionnaire administered by interview the day after EPAP use.
RESULTS
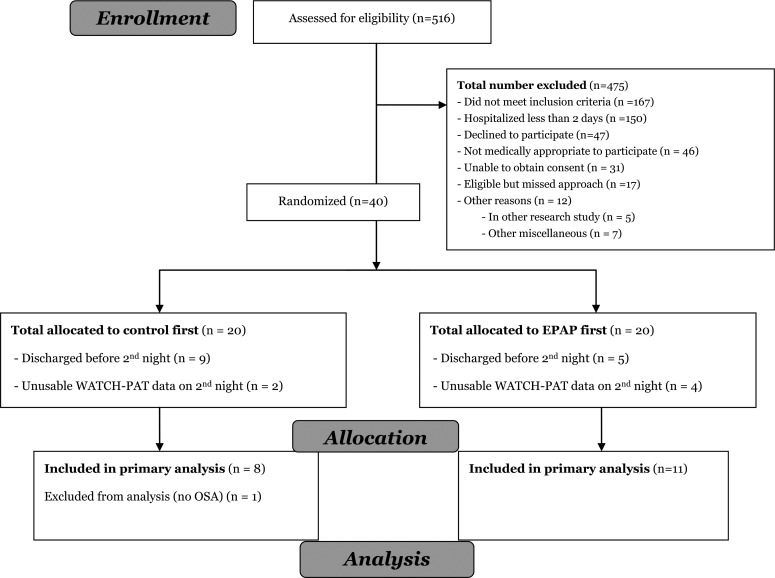
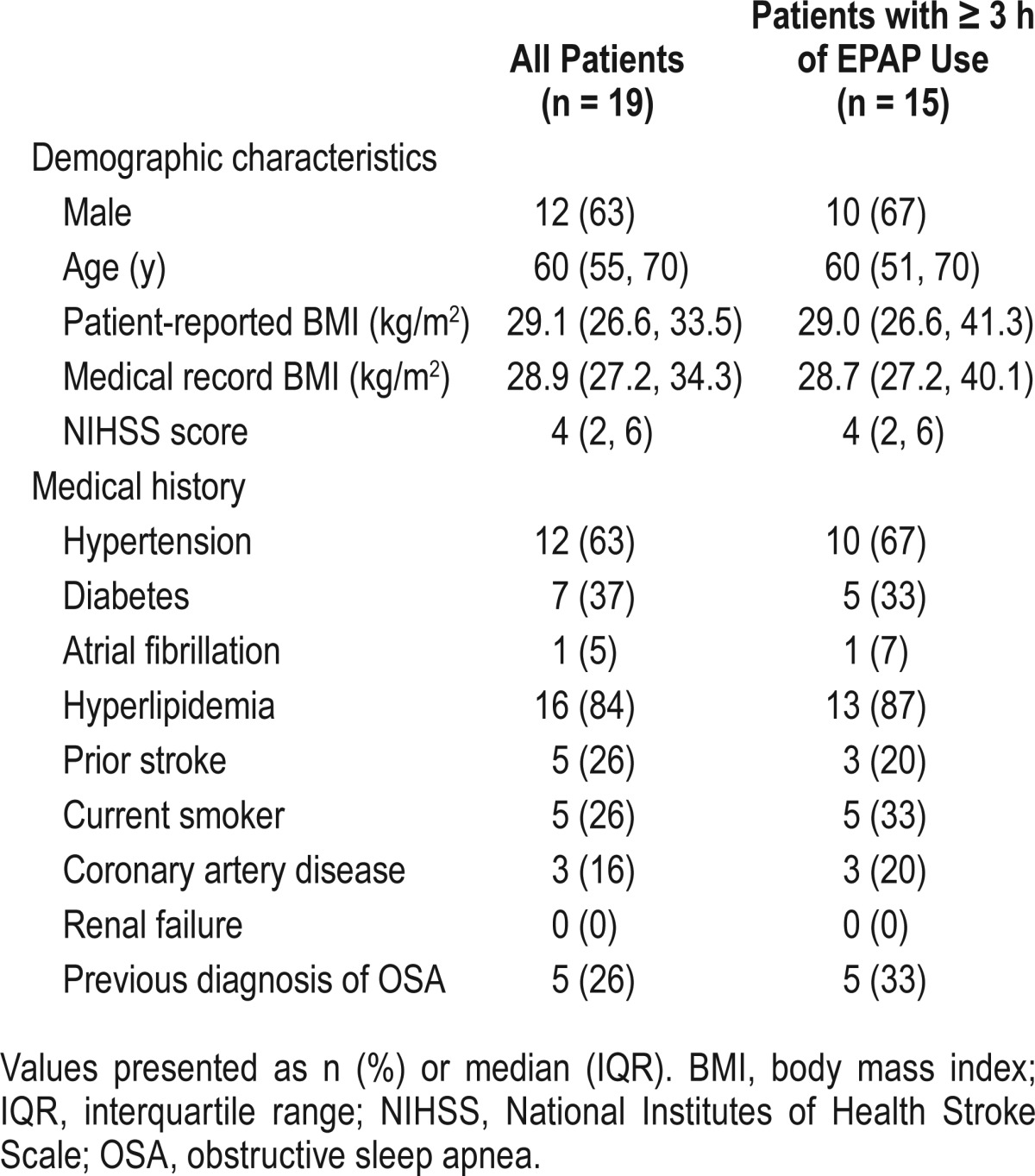
Forty subjects consented to participate in the study. Twenty did not complete the study protocol because of technical difficulties with the Watch-PAT or hospital discharge before completion of study protocol (Figure 1). No subject was excluded due to removal of or intolerance to the EPAP device. Of the 20 subjects who completed the study protocol, one subject had AHI < 5 on both nights and was therefore excluded from analysis. The 19 remaining enrolled subjects were mostly male, in advanced middle age or older, and overweight or obese. Most had hyper-tension and/or hyperlipidemia, and almost one in four had a previous diagnosis of OSA. Full baseline demographic and clinical characteristics are summarized in Table 1.
Figure 1. CONSORT flow diagram.
EPAP, expiratory positive airway pressure; OSA, obstructive sleep apnea.
Table 1.
Patient characteristics.
Primary, Secondary, and Exploratory Analyses
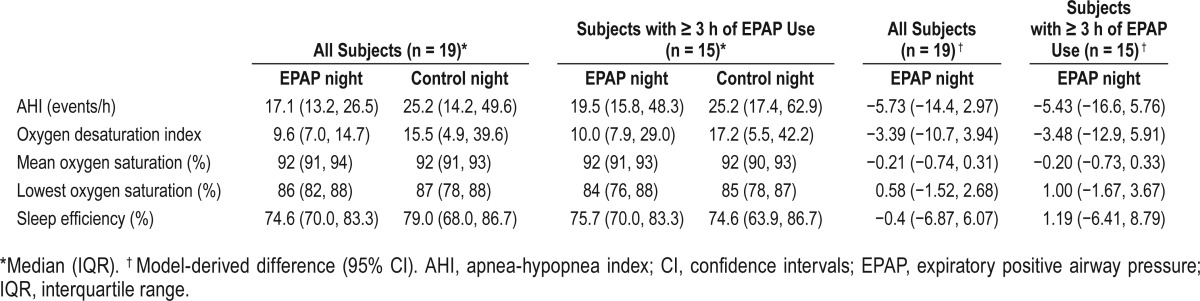
In the primary analysis, median AHI was 17.1 on the intervention night and 25.2 on the control night. Nasal EPAP treatment was associated with a nonsignificant AHI difference derived from the model of −5.73 (95% confidence interval −14.4, 2.97) in the primary analysis. Similarly, model results did not differ by treatment night for oxygen desaturation, mean oxygen saturation, lowest oxygen saturation, or sleep efficiency (Table 2).
Table 2.
Sleep characteristics: raw data and model results.
Sensitivity Analyses
Sensitivity analysis was performed to exclude one subject whose AHI was ≥ 5 on the treatment night but with AHI < 5 on the control night, with similar results compared to the primary analysis (data not shown). Sensitivity analysis including only subjects who self-reported at least 3 h of EPAP use also showed nonsignificant AHI reductions (Table 2).
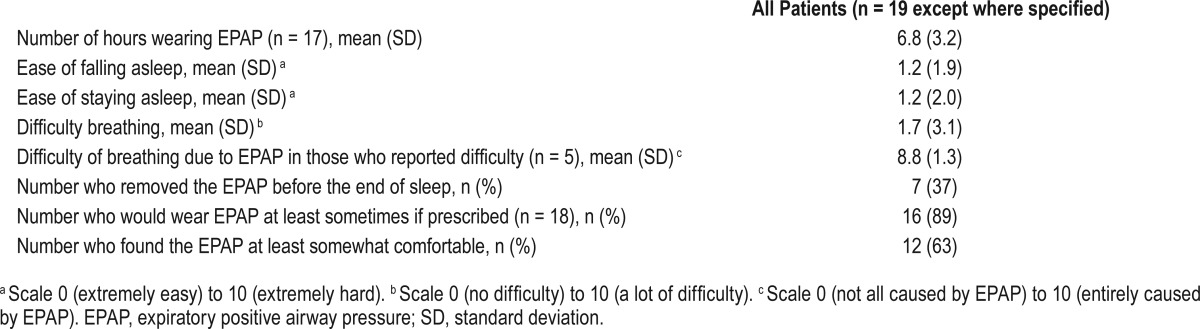
Self-Reported Measures
In general, the majority of subjects reported good tolerability of the EPAP device, with more than 75% reporting use for more than 3 h. A significant minority did report some discomfort or difficulty breathing associated with use of this device. Detailed results of subject self-reported subjective sleep quality and tolerability of the EPAP device are included in Table 3.
Table 3.
Patient perception of the sleep experience, and subjective tolerability of the provent expiratory positive airway pressure device.
DISCUSSION
This randomized, controlled, 2-night crossover trial of nasal EPAP therapy for OSA suggests that nasal EPAP is tolerable but not adequately effective in acute ischemic stroke patients. Although a small difference in AHI may have been missed, given 80% power to detect an AHI difference of ≥ 9.6 as confirmed by post hoc calculations, this study argues against a clinically satisfactory treatment effect of EPAP in acute stroke patients.
One possible explanation for this negative result could be that Provent is less effective in stroke patients than in non-stroke patients, though the clinical or physiological basis for this is not clear. Furthermore, although early studies of nasal EPAP in the general OSA population demonstrated a modest but meaningful reduction in AHI throughout a range of sleep apnea severity,10,20 newer evidence suggests that nasal EPAP may be less effective than previously believed.21 A recent study compared CPAP, nasal EPAP, and placebo in a small group of patients with known moderate to severe OSA and found similar recurrence of OSA in the nasal EPAP and placebo EPAP groups.21 Nasal EPAP, like conventional CPAP, has also been associated with development of complex apneas and an increased frequency of central apneas during treatment.22 Existing evidence suggests that in stroke patients obstructive apneas are much more common than central apneas at baseline,23 but it is possible that the measured AHI during EPAP treatment may have captured some purely central or complex apneas.
Other possible explanations for this negative result include (1) underestimation of treatment effect due to possible inadequate EPAP use, though sensitivity analysis that excluded those with poorer self-reported use showed similar results, and (2) overestimation of treatment effect in prior studies due to inaccurate measurement of AHI.17 The current study is unique among EPAP trials in that it assessed OSA without introducing possible measurement error from a nasal pressure cannula inserted through the EPAP device.17
With respect to tolerability, most patients reported nasal EPAP use for greater than 3 h during the intervention night. Furthermore, sleep efficiency was similar on the EPAP and no EPAP nights, even in those with EPAP use ≥ 3 h per night, which suggests that EPAP use did not substantially interfere with sleep. However, several subjects reported discomfort or subjective breathing difficulty during the night associated with the EPAP device use. Tolerability of nasal EPAP in the acute stroke population may not generalize to the larger population of patients with sleep apnea.
OSA prevalence was very high in this population of acutely hospitalized stroke patients, and the reason for this particularly high prevalence is not clear. Although information concerning specific infarction location and size was not collected, existing observational data do suggest a high frequency of sleep apnea in the stroke population overall,23 with a prevalence of approximately 84% in stroke patients with brainstem involvement and 59% in patients with other infarction locations.24 We do not think that this particularly high prevalence can be attributed to other factors relating to the subtype or size of infarct, as other observational studies have not found differences in the prevalence of sleep-disordered breathing based on ischemic stroke subtype,25 stroke severity, or infarction size.26
Limitations of the study include use of the Watch-PAT device, which, although well validated, is not the gold standard measure of OSA and sleep duration, and which required exclusion criteria that diminish the generalizability of results. We also lacked objective measures of EPAP use, though patient self-reported surveys did suggest that most patients were able to use EPAP for at least 3 h during the treatment night. Another limitation is that sleep time and device adherence were measured by actigraphy and patient self-report, respectively, rather than objective monitoring with full polysomnography or direct visualization. This may overestimate sleep duration and device adherence, which may influence our estimates of the effect of EPAP treatment. We note, however, that sensitivity analysis did not show a significant effect on AHI even when limited to patients with high self-reported use. Use of nasal EPAP for only 1 night may also underestimate its medium- or long-term efficacy, as patients were not given several nights of treatment to adjust to the device, as this was not feasible in the context of a crossover design during the acute stroke hospitalization. We did not collect data about long-term efficacy or tolerability of nasal EPAP in the acute stroke population.
CONCLUSIONS
This study supports the feasibility of diagnostic and clinical interventions for OSA during acute hospitalizations after stroke, but suggests that EPAP is not likely to treat OSA effectively in acute stroke patients intolerant to CPAP. Alternatives to CPAP and EPAP should be identified in this important population.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was funded in part by the National Center for Advancing Translational Sciences of the NIH UL1TR000433. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Wheeler is partially supported by NIH grant U10NS086526. Dr. O'Brien receives nonfinancial support from Philips Respironics, Inc. Dr. Chervin is President-Elect of the American Academy of Sleep Medicine, Vice-President of the International Pediatric Sleep Association, and member of the Boards of Directors for the American Sleep Medicine Foundation, the American Board of Sleep Medicine, and the Association of Professional Sleep Societies. He is also an Advisory Board member of the notfor-profit corporation Sweet Dreamzzz, Inc. He is a paid consultant for Zansors and MC3. His research in sleep medicine is partially supported by the NIH, the University of Michigan Medical School, the University of Michigan Medical Innovation Center, and the National Multiple Sclerosis Society. He participated in developing patented technology and tools relative to diagnosis of sleep disorders (patents owned by the University of Michigan) and developed a questionnaire for childhood sleep problems with copyright owned by the University of Michigan and electronic use rights licensed to Zansors. He receives royalties for contributions to UpToDate (Sleep Specialty Editor) and Cambridge University Press. The University of Michigan has received educational gifts from Philips Respironics and Fisher Paykel at his request. Dr. Brown serves as an editorial board member of Neurology, is funded by NIH grants R01HL123379, R01 NS070941, R01 HL126700, U10NS086526, and R01 DC012760, and received research support from the Blue Cross Blue Shield of Michigan Foundation, Michigan Department of Community Health, and the University of Michigan for stroke-related research. The other authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CPAP
continuous positive airway pressure
- EPAP
expiratory positive airway pressure
- IQR
interquartile range
- NIHSS
National Institutes of Health Stroke Scale
- OSA
obstructive sleep apnea
REFERENCES
- 1.Broadley SA, Jorgensen L, Cheek A, et al. Early investigation and treatment of obstructive sleep apnoea after acute stroke. J Clin Neurosci. 2007;14:328–33. doi: 10.1016/j.jocn.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. NEJM. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 3.Turkington PM, Allgar V, Bamford J, Wanklyn P, Elliott MW. Effect of upper airway obstruction in acute stroke on functional outcome at 6 months. Thorax. 2004;59:367–71. doi: 10.1136/thx.2003.005348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munoz R, Duran-Cantolla J, Martinez-Vila E, et al. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke. 2006;37:2317–21. doi: 10.1161/01.STR.0000236560.15735.0f. [DOI] [PubMed] [Google Scholar]
- 5.Brown DL. Sleep disorders and stroke. Semin Neurol. 2006;26:117–22. doi: 10.1055/s-2006-933315. [DOI] [PubMed] [Google Scholar]
- 6.Brown DL, Chervin RD, Kalbfleisch JD, et al. Sleep apnea treatment after stroke (SATS) trial: is it feasible? J Stroke Cerebrovasc Dis. 2013;22:1216–24. doi: 10.1016/j.jstrokecerebrovasdis.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bassetti CL, Milanova M, Gugger M. Sleep-disordered breathing and acute ischemic stroke: diagnosis, risk factors, treatment, evolution, and long-term clinical outcome. Stroke. 2006;37:967–72. doi: 10.1161/01.STR.0000208215.49243.c3. [DOI] [PubMed] [Google Scholar]
- 8.Palombini L, Guilleminault C. Stroke and treatment with nasal CPAP. Eur J Neurol. 2006;13:198–200. doi: 10.1111/j.1468-1331.2006.01169.x. [DOI] [PubMed] [Google Scholar]
- 9.Svatikova A, Chervin RD, Wing JJ, Sanchez BN, Migda EM, Brown DL. Positional therapy in ischemic stroke patients with obstructive sleep apnea. Sleep Med. 2011;12:262–6. doi: 10.1016/j.sleep.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 10.Berry RB, Kryger MH, Massie CA. A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: a randomized controlled trial. Sleep. 2011;34:479–85. doi: 10.1093/sleep/34.4.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenthal L, Massie CA, Dolan DC, Loomas B, Kram J, Hart RW. A multicenter, prospective study of a novel nasal EPAP device in the treatment of obstructive sleep apnea: efficacy and 30-day adherence. J Clin Sleep Med. 2009;5:532–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–89. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi JH, Kim EJ, Kim YS, et al. Validation study of portable device for the diagnosis of obstructive sleep apnea according to the new AASM scoring criteria: Watch-PAT 100. Acta Otolaryngol. 2010;130:838–43. doi: 10.3109/00016480903431139. [DOI] [PubMed] [Google Scholar]
- 14.Ayas NT, Pittman S, MacDonald M, White DP. Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med. 2003;4:435–42. doi: 10.1016/s1389-9457(03)00111-4. [DOI] [PubMed] [Google Scholar]
- 15.Pittman SD, Ayas NT, MacDonald MM, Malhotra A, Fogel RB, White DP. Using a wrist-worn device based on peripheral arterial tonometry to diagnose obstructive sleep apnea: in-laboratory and ambulatory validation. Sleep. 2004;27:923–33. doi: 10.1093/sleep/27.5.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 17.Milne S, Amis TC, Wheatley JR, Kairaitis K. Sensitivity and specificity of hypopnoea detection using nasal pressure in the presence of a nasal expiratory resistive device (Provent(R)) Physiol Meas. 2014;35:2447–58. doi: 10.1088/0967-3334/35/12/2447. [DOI] [PubMed] [Google Scholar]
- 18.Hein H, Behnke G, Jorres RA, Magnussen H. The therapeutic effect of theophylline in mild obstructive sleep apnea/hypopnea syndrome: results of repeated measurements with portable recording devices at home. Eur J Med Res. 2000;5:391–9. [PubMed] [Google Scholar]
- 19.Jones B, Lewis JA. The case for cross-over trials in phase III. Stat Med. 1995;14:1025–38. doi: 10.1002/sim.4780140921. [DOI] [PubMed] [Google Scholar]
- 20.Patel AV, Hwang D, Masdeu MJ, Chen GM, Rapoport DM, Ayappa I. Predictors of response to a nasal expiratory resistor device and its potential mechanisms of action for treatment of obstructive sleep apnea. J Clin Sleep Med. 2011;7:13–22. [PMC free article] [PubMed] [Google Scholar]
- 21.Rossi VA, Winter B, Rahman NM, et al. The effects of provent on moderate to severe obstructive sleep apnoea during continuous positive airway pressure therapy withdrawal: a randomised controlled trial. Thorax. 2013;68:854–9. doi: 10.1136/thoraxjnl-2013-203508. [DOI] [PubMed] [Google Scholar]
- 22.Chopra A, Das P, Ramar K, Staats B, St Louis EK. Complex sleep apnea associated with use of nasal expiratory positive airway (NEPAP) device. J Clin Sleep Med. 2014;10:577–9. doi: 10.5664/jcsm.3716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med. 2010;6:131–7. [PMC free article] [PubMed] [Google Scholar]
- 24.Brown DL, McDermott M, Mowla A, et al. Brainstem infarction and sleep-disordered breathing in the BASIC sleep apnea study. Sleep Med. 2014;15:887–91. doi: 10.1016/j.sleep.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown DL, Mowla A, McDermott M, et al. Ischemic stroke subtype and presence of sleep-disordered breathing: the BASIC sleep apnea study. J Stroke Cerebrovasc Dis. 2015;24:388–93. doi: 10.1016/j.jstrokecerebrovasdis.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iranzo A, Santamaria J, Berenguer J, Sanchez M, Chamorro A. Prevalence and clinical importance of sleep apnea in the first night after cerebral infarction. Neurology. 2002;58:911–6. doi: 10.1212/wnl.58.6.911. [DOI] [PubMed] [Google Scholar]