Abstract
Study Objectives:
A number of authors have shown that children with OSA are more likely to have certain physical characteristics than healthy controls. With this in mind, our objectives were to collect normative baseline data and determine if there was a significant difference in anthropometric and dental measurements between children with OSA and age-matched nonsnoring controls.
Methods:
Children 2 to 12 y of age, in whom OSA was diagnosed by overnight polysomnography, were recruited to our experimental group. Age-matched nonsnoring controls were screened for signs of sleep-disordered breathing. Anthropometric measurements, including waist, neck, and hip circumferences, and waist-hip and neck-waist ratios, were obtained on all study participants preoperatively. Dental casts were acquired to determine intertooth distances and palatal height.
Results:
Sixty-one children (42 with OSA [69%] and 19 controls [31%]) with a mean age of 4.7 y participated in the study. Waist and hip circumferences were significantly larger in children with OSA (p = 0.001 and 0.001, respectively). However, there was no difference in neck circumference and waist-hip ratios between the two groups. Neck-waist ratio in children with OSA was significantly smaller than in controls (p = 0.001). Intertooth distance for the first (p < 0.0001) and second deciduous (p = 0.0002) and first permanent molars (p = 0.022) were significantly narrowed in children with OSA; however, no difference was seen in palatal height between groups. Body mass index was similar between groups (p = 0.76).
Conclusions:
Anthropometric and dental measurements were significantly different in children with OSA compared to nonsnorers. Future studies with a large sample size may allow us to determine if these measurements can be used by clinicians to identify children at risk for OSA.
Commentary:
A commentary on this article appears in this issue on page 1213.
Citation:
Smith DF, Dalesio NM, Benke JR, Petrone JA, Vigilar V, Cohen AP, Ishman SL. Anthropometric and dental measurements in children with obstructive sleep apnea. J Clin Sleep Med 2016;12(9):1279–1284.
Keywords: anthropometric measurements, dental casts, dental measurements, pediatric OSA, sleep-disordered breathing
INTRODUCTION
Sleep-disordered breathing (SDB) encompasses a spectrum of disorders, from primary snoring to obstructive sleep apnea (OSA).1 OSA is the most severe form of SDB and is characterized by partial or complete nocturnal obstruction of pharyngeal airflow. If untreated, resultant alterations in gas exchange and sleep structure may lead to the development of a wide array of clinical sequelae, including poor school performance,2,3 neurocognitive deficits,4 metabolic abnormalities,5,6 and cardiovascular morbidity.7–10
OSA occurs in approximately 2% to 4% of children11,12 and has a peak incidence in preschool-aged children.13 In children without syndromic or nonsyndromic craniofacial abnormalities, this condition is most commonly attributed to adenotonsillar hypertrophy. However, as in adults, increased fat deposition in the neck of children is also thought to be a contributing factor.14 More specifically, research indicates that the increase in childhood obesity has been significantly associated with both the prevalence and severity of pediatric OSA.15,16
BRIEF SUMMARY
Current Knowledge/Study Rationale: Given the difficulty with acquiring polysomnography based on access and cost, a number of studies have focused on alternative identifiers of OSA in children. Identifiers of interest have focused on physical characteristics that can be evaluated in clinical settings or are less costly to obtain, such as anthropometric and dental measurements.
Study Impact: We present preliminary data for anthropometric and dental measurements in children with OSA compared to nonsnoring control patients. Further, we demonstrate that children with OSA have significantly larger waist and hip circumferences, lower neck-waist ratios, and narrower first and second deciduous and first permanent molar intertooth distances compared to nonsnoring controls.
Although polysomnography (PSG) is considered the gold standard for the diagnosis of OSA in children,17 sleep studies are labor intense, costly, often have long waiting lists, and can be difficult to obtain due to limited access to specialists in pediatric sleep medicine.18,19 Numerous authors have evaluated the utility of anthropometric measurements in identifying adults at risk for OSA,20–23 with one study demonstrating that neck circumference was more predictive of OSA than body mass index (BMI).22 Although fewer anthropometric studies have been conducted in children, several authors suggest that larger neck circumference,24 larger waist circumference,25 higher waist-hip ratios,26 and higher neck-waist ratios27 are more likely to be present in children with SDB or OSA.
A number of authors have also investigated the use of dentofacial measurements to identify children at risk for OSA. To compensate for decreased airflow during sleep, children with SDB often change body, head, tongue, and/or mandible position,28 leading to changes in upper airway volume.29–31 These changes reportedly affect dentofacial morphology,32 especially the developing dentition.33–35 Compared to children without SDB, children with SDB have also been found to have narrower and shorter maxillary arches36 and reduced intercanine widths.35
In view of these collective findings, we hypothesized that both anthropometric data and dental measurements obtained from children with OSA would differ from those in nonsnoring children. Although anthropometric data and dental measurements have been separately evaluated in children with OSA, the two have not been examined together in a single population of children with OSA and compared to nonsnoring control patients. Based on information gleaned from the aforementioned studies, we anticipated that children with OSA would have larger neck, waist, and hip circumferences and narrower maxillary intertooth distances compared to nonsnoring age-matched controls. To test this hypothesis, we obtained anthropometric and dental measurements in children with OSA. To establish normative data, we also obtained these measurements in otherwise healthy nonsnoring controls.
METHODS
Study Participants
Study participants included two groups of children ranging in age from 2 to 12 y: (1) the experimental group, composed of children in whom OSA was previously diagnosed by overnight in-laboratory PSG and who were undergoing sleep surgery and (2) the control group, composed of nonsnoring, age-matched children who underwent screening for signs of SDB and were undergoing nonsleep-related surgery. Children were excluded from the control group if families reported positive findings on sleep screening. Screening for SDB was performed by the research coordinator and consisted of asking a series of questions about nighttime symptoms: (1) Does your child have any nighttime snoring? (2) Does your child have any noisy breathing while sleeping? (3) Have you ever witnessed pauses in your child's breathing at night? (4) Does your child ever have coughing, choking, gagging, or gasping while breathing at night? Children with craniofacial abnormalities, such as Pierre-Robin or Treacher Collins syndromes, dental malocclusions, genetic syndromes, and cleft palate or previous cleft repair were excluded from both study groups. An expedited institutional review board approval was obtained from the Johns Hopkins Hospital prior to the start of this study.
All children enrolled in this study were recruited from the preoperative area prior to scheduled elective procedures. OSA was previously diagnosed in children in the experimental group by sleep study and who were undergoing sleep-related procedures, such as adenotonsillectomy. Healthy controls were also recruited through screening in the preoperative area. These children were undergoing elective, urologic, or otolaryngologic nonsleep procedures. During the preoperative evaluation, sleep screening was performed, as described previously, to rule out signs of SDB. Demographic data and physical examination characteristics were collected prior to all surgical procedures. Because all children were already undergoing elective surgical procedures, dental casts were obtained after patients were anesthetized and intubated.
PSG Data
Pediatric sleep physicians reviewed and analyzed PSG data to establish the presence of OSA for children in the experimental group. OSA severity was determined according to the guidelines specified by the American Academy of Sleep Medicine: mild OSA was defined by an obstructive apnea-hypopnea index (oAHI) of 1 to < 5 events per hour; moderate OSA was defined as ≥ 5 to < 10 events per hour, and severe OSA as ≥ 10 events per hour.
Anthropometric Measurements
Height and weight were measured preoperatively using standardized equipment. A non-elastic tape measure was used to obtain the waist circumference at the level of the umbilicus. Neck circumference was measured at the midline, halfway between the cervical spine and anterior neck. Hip circumference was measured on the same plane as the greater trochanters. Waist-hip ratios were calculated by dividing hip measurements by waist measurements. Neck-waist ratios were calculated by dividing neck measurements by waist measurements.
Dental Casts
Dental casts were obtained after patients were anesthetized and intubated. Metal dental trays (Figure 1) and dental alginate were used to take impressions. Dental casts were subsequently made by filling the dental impressions with dental plaster and allowing the mold to dry for 45 min. The casts were collected and stored until dental measurements were performed.
Figure 1. The metal tray used for collecting dental impressions from both patients with obstructive sleep apnea and nonsnoring control patients in order to measure interdental distances and palatal height.
Dental Measurements
All dental measurements were performed by a single oral maxillofacial surgeon who was blinded as to the group assignment of study participants. Using the dental casts and Boley gauge calipers (Integra, Plainsboro, NJ), intertooth distances were recorded to 0.5 mm for each patient. Intermaxillary arch distances were obtained by measuring the transverse widths between the first and second deciduous molars and the first permanent molars. Widths were determined by measuring the shortest distance from each molar's palatal surface at the height of the gingiva. In the event that a molar was absent from one side of the dentition, intermaxillary distance was measured from the side of a visible molar to the estimated location of the contralateral side, using the midline as a point of symmetry. All measurements were represented in millimeters. To determine palatal height, the depth of the palate was measured posterior to the last molar. A straight-edge ruler was laid across the palate contacting the gingival edge on opposing sides. The vertical distance at right angles from this ruler to the palatal apex in the midline was recorded. The palatal height was determined as the farthest distance from the horizontal line to the palatal apex. All dental measurements were repeated in duplicate and the average taken.
Statistical Analyses
Categorical variables for normally distributed data were evaluated using an analysis of variance test. A Kruskal-Wallis test was used to analyze nonparametric data. Differences between group means and normal data were evaluated with a t test.
A power analysis was performed during the initial stages of the project. Although the number of patients recruited to the study was less than expected from the power study, the difference in measured parameters were large enough to reveal significant differences between groups.
RESULTS
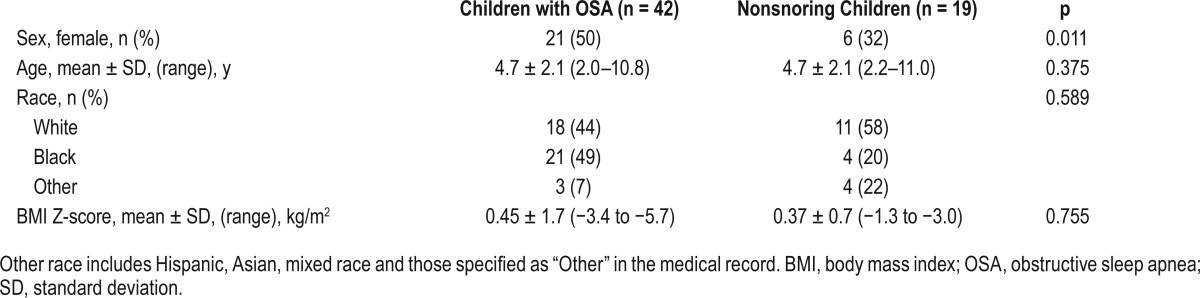
Sixty-one children (27 female, 44%) participated in our study; 42 (69%) had OSA and 19 (31%) were nonsnoring controls (Table 1). The mean age of participants in both the experimental and control groups was 4.7 y (standard deviation 2.1; p = 0.38). Eighteen children with OSA (44%) and 11 nonsnoring controls (58%) were white (non-Hispanic Caucasian) (p = 0.589). The BMI z-score was not significantly different between children with OSA and control patients (0.45 ± 1.7 vs. 0.37 ± 0.7; p = 0.755).
Table 1.
Demographic data for children with obstructive sleep apnea and age-matched nonsnoring controls.
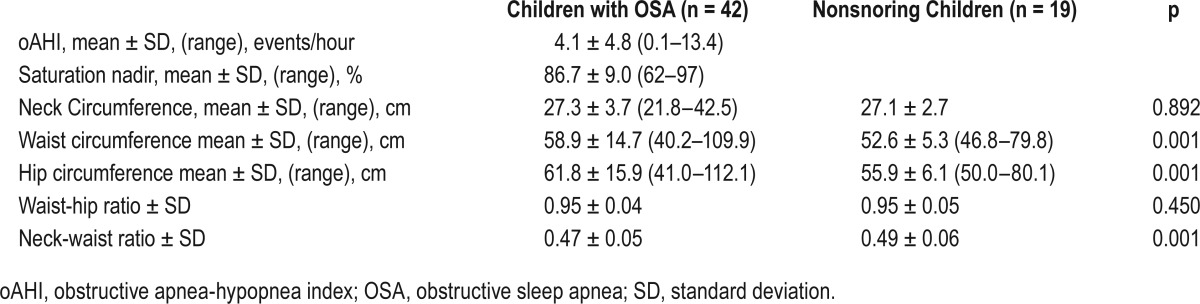
PSG and anthropometric data are presented in Table 2. The mean oAHI for children with OSA was 4.1 ± 4.8 events per hour (Table 2). Waist circumferences were significantly larger in children with OSA than in controls (58.9 ± 14.7 vs. 52.6 ± 5.3; p = 0.001, as were hip circumferences (61.8 ± 15.9 vs. 55.9 ± 6.1; p = 0.001). The neck-waist ratio in children with OSA was, however, significantly lower than in the controls (0.47 ± 0.05 vs. 0.49 ± 0.06, respectively; p = 0.001). There was no difference in either neck circumference (p = 0.892) or waist-hip ratios (p = 0.450) between children with OSA and nonsnoring controls.
Table 2.
Anthropometric and polysomnographic data for children with obstructive sleep apnea and age-matched nonsnoring controls.
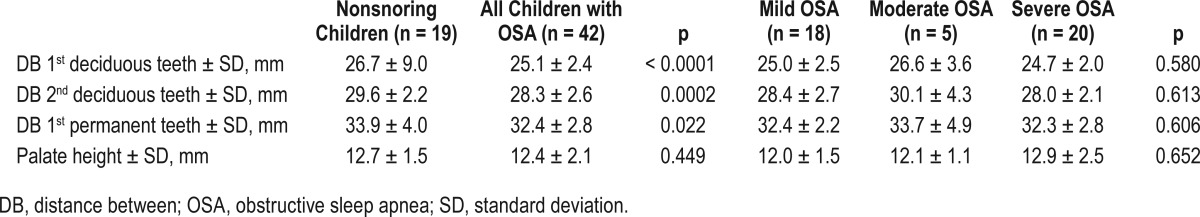
In children with OSA, the intertooth distances for the first and second deciduous molars and the first permanent molars were significantly narrower than in nonsnorers (p ≤ 0.001, p = 0.003, and p = 0.022, respectively) (Table 3). Palatal height in children with OSA was not significantly different from that in non-snorers (p = 0.449). However, there was no significant difference in intertooth distances for the first deciduous (p = 0.580), second deciduous (p = 0.613), and first permanent molars (p = 0.606) between those with mild, moderate, or severe OSA. A subgroup analysis of children by age revealed significant differences in intertooth distances between children with OSA and controls, regardless of whether children were younger or older than 6 y. Although the study was not powered for multiple comparisons, regression analyses were carried out to examine the effects of sex and neck-waist ratios on intertooth distances and palatal heights. Sex appeared to have a significant effect on the first and second deciduous intertooth distances, but had no effect on the molar intertooth distances or palatal height. There did not appear to be a significant effect from neck-waist ratios on any intertooth distances or the palatal height. However, in light of the fact that we were underpowered to assess this relationship, it is unclear if there is a significant role for sex on intertooth distances.
Table 3.
Intertooth distances in children with obstructive sleep apnea and age-matched nonsnoring controls.
DISCUSSION
This is the first study to report normative dental data through the use of casting techniques. As anticipated, we found that waist circumference and hip circumference were significantly larger in children with OSA than in nonsnoring controls. In addition, intertooth distances were significantly narrower in children with OSA than in controls. Contrary to our expectations, however, there was no difference in neck circumference or waist-hip ratio between the two groups, nor was there a difference in palatal height. Also, the neck-waist ratio in children with OSA was significantly smaller than in controls.
Because of the significant expense and limited accessibility of pediatric PSG, clinicians continue to search for alternatives to diagnose OSA in children. In an effort to identify anthropometric measurements that could be used to identify OSA, a number of studies have examined these measurements in children.24–27,37 Several authors have reported findings consistent with our data. In the Childhood Adenotonsillectomy (CHAT) study, Chervin et al.37 found that mild to moderate OSA in children managed with watchful waiting was more likely to resolve in patients with smaller waist circumferences. Although children in our study were not followed longitudinally, those with OSA were found to have a larger waist circumference.
Unlike the CHAT study, data reported by Katz et al.27 were not consistent with our anthropometric findings. These authors reported that neck-waist ratio was significantly higher in children with OSA than in children without OSA.27 This discrepancy could perhaps be explained by the fact that children who participated in our study were substantially younger (mean age of 4.7 y) than those who participated in the investigation by Katz et al.27 (mean age of 12.1 y, range 7.0–17.9 y). More specifically, given that physiologic differences in body fat distribution and anatomic proportions change with age, making a direct comparison of findings between these two studies is difficult. In addition, both groups of children had a mean neck-waist ratio that was higher than the threshold of 0.47, which Katz et al.27 suggested was associated with a higher incidence of OSA; this limits the interpretation of this finding.
Regardless of age, we found that intertooth distances between first and second deciduous and first premolars were significantly narrower in children with OSA than in nonsnorers. These findings support the hypothesis that the narrower maxillary width seen in children with OSA stems from a genetic predisposition for OSA and is not a result of progressive narrowing of the maxilla because of OSA.36 Our results contrast with those reported in two longitudinal studies that demonstrated widening of maxillary widths in children with OSA after tonsillectomy and adenoidectomy.38,39 However, larger studies will be required to add significant weight to either of these hypotheses. Similar to previous research,40 children in our study with OSA did not demonstrate a difference in palatal height compared to nonsnorers. Although the role of various dental measurements have been examined, the validity of palatal height as a predictor of pediatric OSA is currently unknown.
Limitations of our study include the small sample size of the control group. Because we matched children by age and many of the screened children were snorers, our control group was smaller than we anticipated. However, each nonsnoring patient was matched 1:2 with a study group patient by age. Additionally, we did not match on race or sex, as our evaluation of the literature did not suggest that there were differences in children based on these factors. Although there were no significant differences in race between the study and control groups, there were more females in the OSA group than in the control group; these demographic factors may be uncontrolled confounders. We suggest that future studies should include a larger sample size, especially for the nonsnoring controls. This would enhance the value of normative baseline data and the generalizability of our findings. In some instances when children did not have contralateral molars, intertooth distances were calculated based on estimated location of the opposing molar. This could yield an error in calculating the intertooth distances. Last, we did not obtain PSG evaluations for nonsnoring controls, but rather screened them clinically for snoring and signs of SDB. Therefore, we cannot be certain that none of our controls had SDB or OSA; however, even if there were children with SDB in the control group, this would have led to regression to the mean and made it less likely that we would see significant differences between our study and control groups.
CONCLUSIONS
We found that anthropometric and dental measurements were significantly different in children with OSA compared to non-snoring controls. Specifically, we found that children with OSA had larger waist circumference, larger hip circumference, smaller neck-waist ratio, and narrower intertooth distances. However, no significant difference was seen between palatal height in children with OSA and nonsnoring controls. Future studies with a larger sample size that controls for race and sex may allow us to determine if these measurements can be used by clinicians to identify children at risk for OSA and would be particularly valuable when overnight PSG is inaccessible or too costly.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- BMI
body mass index
- CHAT
Childhood Adenotonsillectomy
- DB
distance between
- n
number
- oAHI
obstructive apnea-hypopnea index
- OSA
obstructive sleep apnea
- PSG
polysomnography
- SD
standard deviation
- SDB
sleep-disordered breathing
- y
year
REFERENCES
- 1.Carroll JL. Obstructive sleep-disordered breathing in children: new controversies, new directions. Clin Chest Med. 2003;24:261–82. doi: 10.1016/s0272-5231(03)00024-8. [DOI] [PubMed] [Google Scholar]
- 2.Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998;102:616–20. doi: 10.1542/peds.102.3.616. [DOI] [PubMed] [Google Scholar]
- 3.Weissbluth M, Davis AT, Poncher J, Reiff J. Signs of airway obstruction during sleep and behavioral, developmental, and academic problems. J Dev Behav Pediatr. 1983;4:119–21. doi: 10.1097/00004703-198306000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Chervin RD, Archbold KH. Hyperactivity and polysomnographic findings in children evaluated for sleep-disordered breathing. Sleep. 2001;24:313–20. doi: 10.1093/sleep/24.3.313. [DOI] [PubMed] [Google Scholar]
- 5.Gozal D, Capdevila OS, Kheirandish-Gozal L. Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am J Respir Crit Care Med. 2008;177:1142–9. doi: 10.1164/rccm.200711-1670OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de la Eva RC, Baur LA, Donaghue KC, Waters KA. Metabolic correlates with obstructive sleep apnea in obese subjects. J Pediatr. 2002;140:654–9. doi: 10.1067/mpd.2002.123765. [DOI] [PubMed] [Google Scholar]
- 7.Amin RS, Carroll JL, Jeffries JL, et al. Twenty-four-hour ambulatory blood pressure in children with sleep-disordered breathing. Am J Respir Crit Care Med. 2004;169:950–6. doi: 10.1164/rccm.200309-1305OC. [DOI] [PubMed] [Google Scholar]
- 8.Enright PL, Goodwin JL, Sherrill DL, Quan JR, Quan SF. Blood pressure elevation associated with sleep-related breathing disorder in a community sample of white and Hispanic children: the Tucson Children's Assessment of Sleep Apnea study. Arch Pediatr Adolesc Med. 2003;157:901–4. doi: 10.1001/archpedi.157.9.901. [DOI] [PubMed] [Google Scholar]
- 9.Marcus CL, Greene MG, Carroll JL. Blood pressure in children with obstructive sleep apnea. Am J Respir Crit Care Med. 1998;157:1098–103. doi: 10.1164/ajrccm.157.4.9704080. [DOI] [PubMed] [Google Scholar]
- 10.Quan SF, Gersh BJ. Cardiovascular consequences of sleep-disordered breathing: past, present and future: report of a workshop from the National Center on Sleep Disorders Research and the National Heart, Lung, and Blood Institute. Circulation. 2004;109:951–7. doi: 10.1161/01.CIR.0000118216.84358.22. [DOI] [PubMed] [Google Scholar]
- 11.Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance, and behaviour in 4-5 year olds. Arch Dis Child. 1993;68:360–6. doi: 10.1136/adc.68.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159:1527–32. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- 13.Farber JM. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;110:1255–7. doi: 10.1542/peds.110.6.1255-a. [DOI] [PubMed] [Google Scholar]
- 14.Tung A. The biology and genetics of obesity and obstructive sleep apnea. Anesthesiol Clin North Am. 2005;23:445–61. doi: 10.1016/j.atc.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Arens R, Muzumdar H. Childhood obesity and obstructive sleep apnea syndrome. J Appl Physiol. 2010;108:436–44. doi: 10.1152/japplphysiol.00689.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunton GF, Kaplan J, Wolch J, Jerrett M, Reynolds KD. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10:393–402. doi: 10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics, Section of Pediatric Pulmonology. “Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome.”. Pediatrics. 2002;109:704–12. doi: 10.1542/peds.109.4.704. [DOI] [PubMed] [Google Scholar]
- 18.Portier F, Portmann A, Czernichow P, et al. Evaluation of home versus laboratory polysomnography in the diagnosis of sleep apnea syndrome. Am J Respir Crit Care Med. 2000;162:814–8. doi: 10.1164/ajrccm.162.3.9908002. [DOI] [PubMed] [Google Scholar]
- 19.Katz SL, Witmans M, Barrowman N, et al. Pediatric sleep resources in Canada: the scope of the problem. Pediatr Child Health. 2014;19:367–72. doi: 10.1093/pch/19.7.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davies RJ, Stradling JR. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. Eur Respir J. 1990;3:509–14. [PubMed] [Google Scholar]
- 21.Hoffstein V, Mateika S. Differences in abdominal and neck circumferences in patients with and without obstructive sleep apnoea. Eur Respir J. 1992;5:377–81. [PubMed] [Google Scholar]
- 22.Davies RJ, Ali NJ, Stradling JR. Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax. 1992;47:101–5. doi: 10.1136/thx.47.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma SK, Kurian S, Malik V, et al. A stepped approach for prediction of obstructive sleep apnea in overtly asymptomatic obese subjects: a hospital based study. Sleep Med. 2004;5:351–7. doi: 10.1016/j.sleep.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Yu PL, Ford G. Does neck size predict the presence and severity of OSAS in children? Sleep. 2008;31:A62. (Abstract Suppl) [Google Scholar]
- 25.Bixler EO, Vgontzas AN, Lin HM, et al. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep. 2009;32:731–6. doi: 10.1093/sleep/32.6.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sanchez-Armengol A, Fuentes-Pradera MA, Capote-Gil F, et al. Sleep-related breathing disorders in adolescents aged 12 to 16 years: clinical and polygraphic findings. Chest. 2001;119:1393–400. doi: 10.1378/chest.119.5.1393. [DOI] [PubMed] [Google Scholar]
- 27.Katz SL, Vaccani JP, Barrowman N, Momoli F, Bradbury CL, Murto K. Does neck-to-waist ratio predict obstructive sleep apnea in children? J Clin Sleep Med. 2014;10:1303–8. doi: 10.5664/jcsm.4284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Behlfelt K. Enlarged tonsils and the effect of tonsillectomy. Characteristics of the dentition and facial skeleton. Posture of the head, hyoid bone and tongue. Mode of breathing. Swed Dent J Suppl. 1990;72:1–35. [PubMed] [Google Scholar]
- 29.Solow B, Skov S, Ovesen J, Norup PW, Wildschiødtz G. Airway dimensions and head posture in obstructive sleep apnoea. Eur J Orthod. 1996;18:571–9. doi: 10.1093/ejo/18.6.571. [DOI] [PubMed] [Google Scholar]
- 30.Ono T, Otsuka R, Kuroda T, Honda E, Sasaki T. Effects of head and body position on two- and three-dimensional configurations of the upper airway. J Dent Res. 2000;79:1879–84. doi: 10.1177/00220345000790111101. [DOI] [PubMed] [Google Scholar]
- 31.Hiyama S, Takashi O, Ishiwata Y, Kuroda T. Effects of mandibular position and body posture on nasal patency in normal awake subjects. Angle Orthod. 2002;72:547–53. doi: 10.1043/0003-3219(2002)072<0547:EOMPAB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Solow B, Sandham A. Cranio-cervical posture: a factor in the development and function of the dentofacial structures. Eur J Orthod. 2002;24:447–56. doi: 10.1093/ejo/24.5.447. [DOI] [PubMed] [Google Scholar]
- 33.Löfstrand-Tideström B, Thilander B, Ahlqvist-Rastad J, Jakobsson O, Hultcrantz E. Breathing obstruction in relation to craniofacial and dental arch morphology in 4-year-old children. Eur J Orthod. 1999;21:323–32. doi: 10.1093/ejo/21.4.323. [DOI] [PubMed] [Google Scholar]
- 34.Hultcrantz E, Larsson M, Hellquist R, Ahlqvist-Rastad J, Svanholm H, Jakobsson OP. The influence of tonsillar obstruction and tonsillectomy on facial growth and dental arch morphology. Int J Pediatr Otorhinolaryngol. 1991;22:125–34. doi: 10.1016/0165-5876(91)90032-7. [DOI] [PubMed] [Google Scholar]
- 35.Pirilä K, Tahvanainen P, Huggare J, Nieminen P, Löppönen H. Sleeping positions and dental arch dimensions in children with suspected obstructive sleep apnea syndrome. Eur J Oral Sci. 1995;103:285–91. doi: 10.1111/j.1600-0722.1995.tb00028.x. [DOI] [PubMed] [Google Scholar]
- 36.Hultcrantz E, Löfstrand Tideström B. The development of sleep disordered breathing from 4 to 12 years and dental arch morphology. Int J Pediatr Otorhinolaryngol. 2009;73:1234–41. doi: 10.1016/j.ijporl.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 37.Chervin RD, Ellenberg SS, Hou X, et al. Prognosis for spontaneous resolution of obstructive sleep apnea in children. Chest. 2015;148:1204–13. doi: 10.1378/chest.14-2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zettergren-Wijk L, Forsberg C-M, Linder-Aronson S. Changes in dentofacial morphology after adeno-tonsillectomy in young children with obstructive sleep apnoea—a 5 year follow-up study. Eur J Orthod. 2006;28:319–26. doi: 10.1093/ejo/cji119. [DOI] [PubMed] [Google Scholar]
- 39.Souki BQ, Pimenta GB, Franco LP, Becker HMG, Pinto JA. Changes in vertical dentofacial morphology after adeno-tonsillectomy during deciduous and mixed dentitions mouth breathing children—1 year follow-up study. Int J Pediatr Otorhinolaryngol. 2010;74:626–32. doi: 10.1016/j.ijporl.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Pirila-Parkinnen K, Pirttiniemi P, Nieminen P, Tolonen U, Pelttari U, Lopponen H. Dental arch morphology in children with sleep-disordered breathing. Eur J Orthod. 2009;31:160–7. doi: 10.1093/ejo/cjn061. [DOI] [PubMed] [Google Scholar]