ABSTRACT
Increasing numbers of perinatally HIV (PHIV+)-infected youth are surviving into adulthood with better access to treatment. However, few studies examine positive outcomes in the face of adversity (resilience) for PHIV+ youth. Social Action Theory (SAT) provided the theoretical framework for this study of PHIV + youth in South Africa (SA), allowing examination of contextual, social, and self-regulatory factors that influence behavioral health. Data were from youth and caregiver baseline interviews, simply pooled from a pilot (N=66) and larger (n=111) randomized control trial (RCT) of the VUKA Family program. For this analysis, outcomes included emotional and behavioral functioning (total difficulties), and prosocial behaviors. Potential SAT correlates included socio-demographics; caregiver health and mental health; parent-child relationship factors; stigma, and child coping, support; and self-esteem. Regression analyses adjusted for age, gender, and study revealed significant associations at the contextual, social, and self-regulation level. Lower total child difficulties scores were associated with lower caregiver depression (β = 3.906,p < .001), less caregiver-reported communication about difficult issues (β = 1.882, p = .009) and higher youth self-esteem (β = -0.119, p = .020). Greater prosocial behaviors were associated with greater caregiver-reported communication (β = 0.722, p = .020) and child use of wishful thinking for coping (β = 5.532, p = .009). Less youth depression was associated with higher caregiver education (β =−0.399, p = .010), greater caregiver supervision (β = −1.261, p = .012), more social support seeking (β = −0.453, p = .002), higher youth self-esteem (β = −0.067, p < .001), lower internalized stigma (β = 0.608, p = .040), and child use of resignation for coping (β = 1.152, p = .041). Our data support evidence-based family interventions that also promote youth self-regulation skills to enhance the health and mental health of PHIV+ youth.
KEYWORDS: Resilience, HIV+ adolescents, social action theory, mental health
With the increase in the availability of antiretroviral treatment (ART) in South Africa (SA), a large cohort of perinatally HIV (PHIV+)-infected youth, once not expected to outlive childhood, are now aging into adolescence and young adulthood (Sohn & Hazra, 2013; UNAIDS, 2014). However, a set of complex issues related to identification, care, and treatment of children with perinatal HIV infection persists. For example, despite the decrease in the number of children with severe illness at ART initiation, 62% of children were still initiating therapy with advanced disease in 2013 (World Health Organization Stage III/IV disease) (Davies et al., 2013).
In addition to the normative stressors associated with adolescent physiological, psychological, and social development, PHIV+ youth are likely to confront a number of additional challenges, both HIV and non-HIV related, including illness and death of parents and siblings, caregiving responsibilities for younger siblings or other family members, stigma and discrimination related to HIV or orphanhood, and an uncertain future (Lowenthal et al., 2014; Petersen et al., 2010). Studies from SA and other parts of the world have consistently shown that the majority of PHIV+ youth come from families that are larger and poorer, have lower rates of employment, and are living in impoverished communities (Bachmann & Booysen, 2003; Cluver, Boyes, Orkin, & Sherr, 2013). Moreover, high rates of emotional and behavioral health problems among PHIV+ youth have been noted in a number of studies in both high- and low-resource contexts (Bomba et al., 2010; Mellins & Malee, 2013; Mellins et al., 2012; Puthanakit & Siberry, 2013). Various studies from the USA and sub-Saharan Africa have found that PHIV+ youth, similar to same age peers, are engaging in substance use and sexual behaviors, and use condoms inconsistently (Bauermeister, Elkington, Robbins, Kang, & Mellins, 2012; Birungi, Mugisha, Obare, & Nyombi, 2009; Mellins et al., 2011; Tassiopoulos et al., 2013). Furthermore, PHIV+ adolescents and young adults have lower levels of medication adherence and higher levels of drug resistance relative to younger children and adults (Van Dyke et al., 2016), increasing risk of adverse medical outcomes and transmission of HIV to others.
However, it is also true that despite the increased risk and vulnerabilities facing PHIV+ youth, some studies show that many are presenting with behavioral health problems that are the same or less than uninfected peers. For example, several studies have found relatively low rates of substance use (Elkington, Bauermeister, Brackis-Cott, Dolezal, & Mellins, 2009; Mellins, 2013; Mellins & Malee, 2013; Williams et al., 2010) and late onset of sexual behaviors (Bauermeister et al., 2012; Mellins & Malee, 2013) among PHIV+ youth relative to uninfected youth. Although some studies suggest that PHIV+ youth experience high rates of psychiatric disorders and mental health problems, a number of studies have also found no significant differences in rates of psychiatric disorders between PHIV+ and demographically similar uninfected youth, including PHIV-exposed, but uninfected youth and HIV− youth who have HIV+ family members (Gadow et al., 2010; Gadow et al., 2012; Mellins et al., 2012; Sopena, Evangeli, Dodge, & Melvin, 2010). Furthermore, HIV-associated neurocognitive disorders range widely from 8 to 60% in untreated children, suggesting that not all children and adolescents experience the same level of vulnerability (Nassen et al., 2014). Even in studies that have found higher rates of mental health and other problems among PHIV+ youth, large proportions of youth have displayed no risk outcomes (Kapetanovic et al., 2011; Mellins, 2013; Mellins et al., 2011). All this suggests the presence of factors in the lives of some PHIV+ youth that promote resilience, broadly defined as the achievement of positive outcomes despite circumstances that are linked with negative outcomes (Zolkoski & Bullock, 2012).
While few studies specifically related to resilience among PHIV+ youth exist, particularly in low-resource contexts, a review of the evidence from other fields and preliminary work in HIV suggests that the child’s health status and cognitive function, parental health and mental health, as well as stressful life events and disruptive neighborhoods, may be associated with worse mental health outcomes, while parental involvement and communication with the child and parent and teacher social support are associated with positive outcomes (Catalano, Hawkins, Berglund, Pollard, & Arthur, 2002; Gadow et al., 2012; Kia-Keating, Dowdy, Morgan, & Noam, 2011; Luthar, Sawyer, & Brown, 2006; Mellins & Malee, 2013; Petersen et al., 2010). Resilience is, therefore, both a function of characteristics of the individual child and the relationships that support the child, as well as the quality of that child’s environment, which provides the resources necessary for positive development, despite adverse circumstances (Ungar et al., 2007).
The existing literature has consistently emphasized that resilience is most strongly bolstered when protective factors at the levels of individual, family, and community are strengthened (Benzies & Mychasiuk, 2009; Stein et al., 2014). While understanding the areas of risk is essential to targeting these vulnerabilities, these findings do not tell us “how” to intervene. Understanding factors that can facilitate the health and well-being of PHIV+ youth as they age, that is, studying the influences that can bolster resilience, is increasingly valued in designing programs and identifying points of intervention that might most effectively promote positive outcomes and avert negative effects (Mofenson & Cotton, 2013).
As a model of behavior change, Social Action Theory (SAT; Ewart, 1991) offers a useful lens for examining the contextual, social, and individual factors that may explain resilience. SAT emphasizes the context in which behavior occurs and the developmentally driven self-regulatory and social interaction processes that affect adaptive behavior. Contextual elements that have been found to be protective in general child and youth populations include safe neighborhoods, access to quality schools and health services, a stable and sufficient family income, and community financial support (Benzies & Mychasiuk, 2009). At the level of social interactions, parent–child and other family relationship factors have been associated with positive outcomes across populations. For example, parent–child supervision, positive emotional expression, family cohesion, and supportive parent–child communication have been associated with positive youth development (Fergus & Zimmerman, 2005; Zolkoski & Bullock, 2012) and may be critical for PHIV+ youth (Mellins & Malee, 2013). Finally, self-regulatory factors, including self-esteem, coping, and self-efficacy have also been found to be important predictors of resilience (Zolkoski & Bullock, 2012).
Using SAT, the present study explored what (i) contextual, (ii) social regulation, and (iii) self-regulation variables were associated with positive mental health outcomes in a population of young South African PHIV+ adolescents. The SAT model has been previously adapted and used in several studies of youth and adults infected and affected by HIV in the USA (Mellins et al., 2008; Traube, Dukay, Kaaya, Reyes, & Mellins, 2010). More specifically, using our adapted SAT model (see Figure 1), we hypothesize that behavioral health outcomes, including mental health, are influenced by context (e.g. socioeconomic status and caregiver health status), self-regulation (self-esteem, perceived illness stigma), and social regulation (e.g. family communication and supervision and social support) factors.
Figure 1.
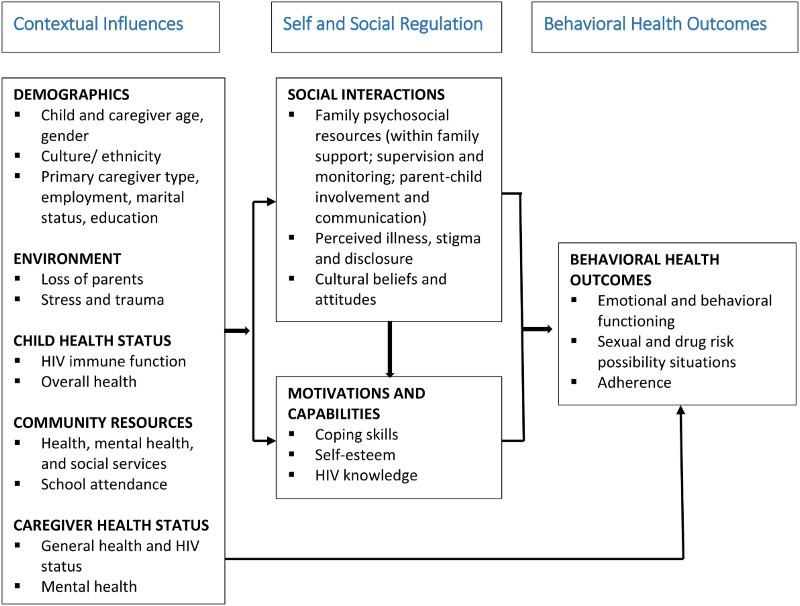
Modified SAT.
Methods
This study uses baseline data pooled from the baseline interviews of a pilot randomized controlled trial (RCT) and the larger RCT for the VUKA Family Program, both based in KwaZulu-Natal, SA. VUKA (“Let’s Wake Up” in isiZulu) is a cartoon-based family intervention aimed at reducing risk behaviors in PHIV+ youth in poverty-impacted areas and is based on an evidence-based family mental health and prevention program for uninfected youth, Collaborative HIV and Adolescent Mental Health Program (CHAMP), that has been tested in multiple RCTs, including one set in SA (Bell et al., 2008; Bhana, McKay, Mellins, Petersen & Bell, 2010). The development of the VUKA intervention and the pilot trial have been described in previous publications (Bhana et al., 2014; Mellins et al., 2014). For both the pilot and the larger RCT that is ongoing, participants completed an extensive baseline interview with variables on mental health and the SAT constructs that are the basis for this study.
Participants
Data from all participants who consented to be in the VUKA project and completed a baseline interview were included in these analyses. The VUKA pilot trial, conducted between 2008 and 2010, recruited participants from pediatric HIV clinics at two hospitals, one in Durban and one located near Durban in an urban area of KwaZulu-Natal. In the larger ongoing VUKA trial, initiated in 2012, participants were recruited from two large public hospitals located in Durban. Both the pilot and larger trial used the same recruitment procedures. Caregivers were referred to the study by medical staff and posters were placed in waiting areas for caregivers interested in enrolling. Staff also made announcements.
Inclusion criteria for both studies
To be eligible for VUKA, which targets younger adolescents (before most risk behaviors are initiated), youth had to meet the following criteria: (a) ages 9–14 years, (b) PHIV+, (c) aware of their HIV diagnosis (VUKA is a group-based intervention in which HIV is discussed), and (d) isiZulu speaking (the vast majority of patients in KwaZulu-Natal speak isiZulu). Caregivers included biological parents, guardians, relatives, and adoptive parents who had primary responsibility for the care of the youth and were isiZulu speaking.
Current sample
The pooled sample for these analyses contained 177 caregiver–child dyads who completed baseline interviews, 66 from the initial pilot trial and 111 from the larger RCT of the VUKA Family Project intervention trial. As seen in Table 1, the two samples did not differ significantly from each other with the only difference being a higher number of individuals experiencing food insecurity in the pilot intervention compared to the larger intervention trial.
Table 1. Demographic characteristics.
| Pilot sample (N = 66)a | VUKA sample (N = 111)a | P* | ||||
|---|---|---|---|---|---|---|
| HIV+ adolescents | HIV+ adolescents | |||||
| Gender | N | % | Gender | N | % | .71 |
| Male | 33 | 51 | Male | 48 | 47 | |
| Female | 32 | 49 | Female | 55 | 53 | |
| Age mean ± SD | 11.57 ± 1.16 | Age mean ± SD | 11.75 ± 1.57 | .40 | ||
| Caregiver characteristics | Caregiver characteristics | |||||
| Live in own place | Live in own place | .18 | ||||
| Yes | 38 | 59 | Yes | 49 | 47 | |
| No | 27 | 41 | No | 56 | 53 | |
| Receiving a grant for child | Receiving a grant for child | .26 | ||||
| Yes | 52 | 81 | Yes | 76 | 72 | |
| No | 12 | 19 | No | 29 | 28 | |
| Household Income | Household Income | .92 | ||||
| At least one person has job | 20 | 32 | At least one person has job | 33 | 32 | |
| At least one person has pension | 19 | 30 | At least one person has pension | 35 | 34 | |
| At least one person has job + | At least one person has job + | |||||
| one person has pension | 21 | 33 | one person has pension | 30 | 29 | |
| No one has job or pension | 3 | 5 | No one has job or pension | 6 | 6 | |
| Gone without food in past month | Gone without food in past month | .00 | ||||
| More than six times | 11 | 17 | More than six times | 1 | 1 | |
| 4–6 times | 10 | 16 | 4–6 times | 2 | 2 | |
| 2–3 times | 12 | 19 | 2–3 times | 14 | 13 | |
| One time | 5 | 8 | One time | 2 | 2 | |
| Never | 25 | 40 | Never | 86 | 82 | |
| Current regular employment | Current Regular employment | .06 | ||||
| Yes | 19 | 30 | Yes | 17 | 16 | |
| No | 45 | 70 | No | 88 | 84 | |
| Education | Education | .22 | ||||
| Eighth grade or less | 22 | 35 | <than eighth grade | 26 | 25 | |
| greater than eighth grade | 41 | 65 | >than eighth grade | 79 | 75 | |
| Caregiver HIV status | Caregiver HIV status | .33 | ||||
| Positive | 39 | 74 | Positive | 65 | 64 | |
| Negative | 14 | 26 | Negative | 36 | 36 | |
aValid sample size for each variable varies due to missingness.
*P-value: t-test for continuous variables and Chi-squared test for categorical variables (with continuity correction for 1 degree of freedom test).
Procedures
In both studies, eligible, recruited participants were contacted by study staff, who described study procedures, and invited them to return for the first study assessment, if interested. Caregivers provided informed, written consent for themselves and their child; children provided written assent. Families were only enrolled if both consent and assent were obtained. For the baseline assessment, caregivers and adolescents were interviewed individually or in groups of 2–3 individuals (pilot only) with interviews lasting approximately one hour. The same procedures and selection criteria were used at baseline in the pilot and the larger study. The adults and adolescents were assessed separately from one another to ensure privacy. All responses were self-reported and recorded on paper (for the pilot study) or electronic tablets (for the larger trial). Participants were reimbursed for transportation and provided with a meal at each interview. Institutional Review Board approvals were obtained from all participating SA and US institutions.
Measures
Youth behavioral outcomes
Prosocial strengths and total difficulties were assessed with the parent version of the Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1997; Goodman, 2001). This 25-item scale is a well-validated and globally used measure of emotional and behavioral functioning that has been translated into multiple languages, including isiZulu (Youth in Mind, http://www.sdqinfo.com). It includes four subscales (emotional problems, conduct problems, hyperactivity, peer-relationship problems) that are used to calculate a total difficulty score, as well as a prosocial behavior score. Previous studies have found more than adequate psychometric properties, including validity, internal consistency, and tests–retest reliability (Goodman, 2001). (Cronbach’s α = 0.560 and 0.714 for prosocial strengths and total difficulties respectively in the combined sample.)
Child depression was measured using the short form of the Children’s Depression Inventory (CDI), a widely used measure with excellent reported psychometrics (Kovacs, 1985). The CDI includes 10-items, each rated on the degree of depression symptomatology experienced in the last two weeks (0–2). A total score is used. (Cronbach’s α = 0.299 in the combined sample.)
Contextual factors
Caregiver HIV status was determined by self-report
Caregiver depression was measured using the Beck Depression Inventory II (BDI-II; Beck, Brown, & Steer, 1996) in the VUKA pilot and the Center for Epidemiologic Studies Depression (CES-D) scale (Radloff, 1977) in the larger intervention trial. For the present analysis, clinically recommended cut-off scores for each measure were used to indicate if the caregiver showed positive symptoms of depression (depressed or not depressed) on whichever scale they completed.
BDI-II
Caregivers in the pilot study completed the 21-item BDI-II, rating characteristics and symptoms of depression. The measure has been used in locations and languages around the world, including SA, with excellent internal consistency (Beck et al., 1996; Steele & Edwards, 2008). (Cronbach’s α = 0.846 in the pilot sample).
CES-D
Caregivers in the larger intervention trial completed the 20-item CES-D Scale, which contains questions about depressive symptomatology in the past week. The CES-D Scale has shown strong psychometric properties in the USA and in SA, where it has been used with various populations, including HIV-infected adults, and has been translated into isiXhosa, Afrikaans, and isiZulu (Kuo & Operario, 2011; Myer et al., 2008). A cutoff score of 16 was used on this measure of depression. (Cronbach’s α = 0.894 in the larger trial.)
Social regulation factors
Caregiver supervision was measured using an instrument tapping caregiver supervision and monitoring created for previous trials of CHAMP in the US and SA with HIV− youth (Bell et al., 2008; McKay & Paikoff, 2007) that was completed by both caregivers and children. The caregiver and child versions include 17 and 14 items, respectively, which address rules, how parents keep track of their child’s whereabouts, and how often children are left in charge of the home. Inter-item reliabilities of the subscales in a sample of 500 urban parents of pre and young adolescent males ranged from .68 (rules) to .81 (extent of involvement/supervision) (Bell et al., 2008). (Cronbach’s α = 0.742 in the combined sample.)
Youth and caregiver frequency and comfort in communication was measured with two scales (comfort and frequency) each of which includes seven topics that caregivers and children often find hard to discuss, including drugs/alcohol, puberty, sex, STDs, and HIV/AIDS. Respondents rate the frequency of discussion about each topic and their level of comfort discussing each topic. The measure has been successfully used in previous CHAMP programs with good psychometric properties (Bell et al., 2008; Bhana et al., 2014). (Cronbach’s α = 0.771–0.815 in the combined sample.)
Stigma was examined as caregivers and children completed a measure of both externalized and internalized stigma related to HIV and AIDS that was originally developed for pediatric epilepsy (Westbrook, Bauman, & Shinnar, 1992) and used in the US version of CHAMP+ (McKay & Paikoff, 2007). It consists of eight items related to feelings about HIV and perceptions about how HIV affects social relationships. (Cronbach’s α = 0.472–0.869 in the combined sample.)
Self-regulation factors
Self-concept was measured with the short form of the child version of the Tennessee Self Concept Scale (TSCS-2), Second Edition (Fitts & Warren, 1996), which assesses components of self-esteem (identity, satisfaction, and behavior) over 6 specific domains of self-concept (physical, moral, personal, family, social, and academic) using 20 items. Good psychometric properties have been found in studies in SA and Uganda (Ssewamala, Han, & Neilands, 2009). (Cronbach’s α = 0.735 in the combined sample.)
Coping was only assessed in the pilot study using the Kidcope, a 15-item self-report measure (Spirito, Stark, & Williams, 1988). These items examine 10 subcategories indicating whether problem-solving, distraction, social support, social withdrawal, cognitive restructuring, self-criticism, blaming others, emotional expression, wishful thinking, or resignation mechanism was used. Each coping category refers to a primary description of a way of coping.
Analysis
First, we used descriptive statistics to describe the sample characteristics of caregivers and PHIV+ adolescents. Differences between the two samples were statistically established using t-tests for continuous variables and Chi-squared tests for categorical variables, with a continuity correction for 1-degree of freedom test. Next, we used a simple pooling method to combine the two datasets and constructed a simple linear regression analysis to examine the bivariate association between the participants’ SDQ scores (which measured total difficulties and prosocial strengths) and contextual, social regulation and self-regulation factors in the modified SAT model (See Fig. 1). Additional adjusted analyses were also conducted. The independent variables in the adjusted model included one factor of interest, age, gender, and study indicator (pilot intervention versus larger VUKA intervention trial) to adjust for potential confounding. We then used CDI scores as the dependent variable and repeated all of the above bivariate and adjusted analyses. We reported the unadjusted and adjusted regression coefficient (β) for each factor in the regression model which represents the magnitude change of the outcome variable by one unit increase of the factor under consideration (unconditionally and conditionally, respectively). We declared the findings as statistically significant if the corresponding p-values were ≤.05. All statistical analyses were conducted using IBM SPSS Statistics 23.
Results
Participants
In the combined sample at baseline, the mean child age was 11.68 years (SD = 1.42) across studies; 56% lived with their mother, while others lived with fathers, siblings, or extended family members. The average caregiver age was 40 years (SD = 13.75) and 91% of caregivers were female. Table 1 presents the demographic composition of the participants from the pilot and larger trial separately and as noted previously, there were minimal differences.
Findings from the regression analysis suggested that factors from each level of influence in the SAT model are significantly associated with child resilience outcomes.
Total difficulties score
In the bivariate analysis, we found that lower total difficulties scores among children were associated with lower caregiver depression (β = 3.851, p < .001), less frequent caregiver-reported communication about difficult topics (β = 1.871, p = .007), more caregiver-reported supervision (β = −0.198, p = .041), and higher youth self-concept scores (β = −0.133, p = .006). These associations remained significant in the same direction after adjusting for age, gender, and study indicator (caregiver depression (β = 3.906, p < .001), caregiver-reported communication (β = 1.882, p = .009), and youth self-concept scores (β = −0.119, p = .020)), with the exception of caregiver supervision, which became non-significant (see Table 2).
Table 2. Factors associated with total difficulties score (SDQ).
| Variable | Unstandardized β | Standardized β | t-score | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Unadj.a | Adj.b | Unadja | Adj.b | Unadja | Adj.b | Unadja | Adj.b | |
| Contextual influences | ||||||||
| Caregiver depressed | 3.851 | 3.906 | 0.338 | 0.341 | 4.377 | 4.269 | <0.001 | <0.001 |
| Social regulation | ||||||||
| Caregiver-reported communication frequency | 1.871 | 1.882 | 0.220 | 0.222 | 2.753 | 2.658 | 0.007 | 0.009 |
| Caregiver-reported supervision total score | −0.198 | −0.155 | −0.166 | −0.122 | −2.058 | −1.365 | 0.041 | 0.174 |
| Self-regulation | ||||||||
| Self-concept score (child reported) | −0.133 | −0.119 | −0.228 | −0.205 | −2.784 | −2.363 | 0.006 | 0.020 |
aUnadjusted results represented the findings from simple linear regression analysis in which only one independent variable was included in the model.
bAdjusted results were obtained from multiple linear regression analysis. In each adjusted model, independent variables included one factor of interest and three potential confounders (i.e., age, gender, and study indicator) to adjust for potential confounding.
Prosocial strengths score
As shown in Table 3, simple linear regression analysis revealed that greater prosocial strengths were associated with greater caregiver-reported frequency of communication with children about difficult topics (β = 0.649, p < .001) and communication comfort (β = 0.437, p = .037), as well as youth use of wishful thinking as a coping method (β = 5.390, p = .009). After adjusting for age, gender, and study indicator, greater frequency of communication about difficult topics (β = 0.722, p = .020) and use of wishful thinking (β = 5.532, p = .009) were still significantly associated with stronger prosocial strengths; however, communication comfort just fell short of significance (β = 0.417, p = .064).
Table 3. Factors associated with Prosocial strengths score (SDQ).
| Variable | Unstandardized β | Standardized β | t-score | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Unadj.a | Adj.b | Unadja | Adj.b | Unadja | Adj.b | Unadja | Adj.b | |
| Contextual factors | ||||||||
| Receive any grants for children | 0.638 | 0.552 | 0.151 | 0.130 | 1.943 | 1.572 | 0.054 | 0.118 |
| Social regulation | ||||||||
| Caregiver-reported communication frequency | 0.649 | 0.722 | 0.251 | 0.278 | 3.284 | 3.472 | 0.001 | 0.020 |
| Caregiver-reported communication comfort | 0.437 | 0.417 | 0.165 | 0.155 | 2.105 | 1.867 | 0.037 | 0.064 |
| Self-regulation | ||||||||
| Wishful thinking coping mechanism (pilot only) | 5.390 | 5.532 | 0.332 | 0.343 | 2.684 | 2.690 | 0.009 | 0.009 |
aUnadjusted results represented the findings from simple linear regression analysis in which only one independent variable was included in the model.
bAdjusted results were obtained from multiple linear regression analysis. In each adjusted model, independent variables included one factor of interest and three potential confounders (i.e., age, gender, and study indicator) to adjust for potential confounding.
CDI score
The unadjusted findings suggested that lower level of depression in children was associated with higher caregiver education (β = −0.412, p = .010), lower household density (β = 0.092, p = .041), and greater food security (i.e., less reported hunger in the past month) (β = 0.254, p = .029). Social regulation factors were also associated with depression in children. Lower levels of youth-reported supervision by caregiver (β = −1.667, p < .001) and less likelihood of youth seeking social support (β = −0.429, p = .003) were associated with higher levels of youth depression. Within self-regulation factors, higher self-concept scores (β = −0.076, p < .001) and lower levels of internal stigma (β = 0.655, p = .027) were associated with lower levels of youth depression, while the use of social withdrawal (β = 1.297, p = .022) and resignation (β = 1.156, p = .036) as coping methods were associated with higher levels of depression. Adjusting for age, gender and study indicator, caregiver education (β = −0.399, p = .010), as well as the social regulation factors (caregiver supervision (β = −1.261, p = .012) and likelihood of seeking social support (β = −0.453, p = .002)) and self-regulation factors (self-concept scores (β = −0.067, p < .001), internal stigma (β = 0.608, p = .040), and use of resignation as coping method (β = 1.152, p = .041)) still remained significantly associated with child depression in the same direction as unadjusted findings (see Table 4).
Table 4. Factors associated with CDI score.
| Variable | Unstandardized β | Standardized β | t-score | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Unadj.a | Adj.b | Unadj a | Adj.b | Unadj a | Adj.b | Unadja | Adj.b | |
| Contextual factors | ||||||||
| Caregiver education | −0.412 | −0.399 | −0.204 | −0.198 | −2.611 | −2.603 | 0.010 | 0.010 |
| How many people share house? | 0.092 | 0.081 | 0.162 | 0.144 | 2.065 | 1.849 | 0.041 | 0.066 |
| In the past month, how often have you or your family gone without enough food to eat? | 0.254 | 0.074 | 0.174 | 0.051 | 2.202 | 0.573 | 0.029 | 0.568 |
| Social regulation | ||||||||
| Youth-−reported supervision | −1.667 | −1.261 | −0.336 | −0.254 | −4.550 | −2.554 | <0.001 | 0.012 |
| Youth likelihood of seeking support | −0.429 | −0.453 | −0.231 | −0.244 | −3.009 | −3.177 | 0.003 | 0.002 |
| Self-regulation | ||||||||
| Tennessee self-concept score | −0.076 | −0.067 | −0.389 | −0.343 | −5.414 | −4.624 | <0.001 | <0.001 |
| Youth-reported internal stigma | 0.655 | 0.608 | 0.173 | 0.162 | 2.226 | 2.070 | 0.027 | 0.040 |
| Social withdrawal coping mechanism (pilot only) | 1.297 | 1.068 | 0.293 | 0.241 | 2.356 | 1.863 | 0.022 | 0.068 |
| Resignation coping mechanism (pilot only) | 1.156 | 1.152 | 0.262 | 0.261 | 2.138 | 2.084 | 0.036 | 0.041 |
aUnadjusted results represented the findings from simple linear regression analysis in which only one independent variable was included in the model.
bAdjusted results were obtained from multiple linear regression analysis. In each adjusted model, independent variables included one factor of interest and three potential confounders (i.e., age, gender, and study indicator) to adjust for potential confounding.
Discussion
This is one of the few studies examining theoretically informed (SAT) correlates of mental health outcomes in PHIV+ early adolescents growing up in a low- to middle-income country. With the advent of antiretroviral treatment, concerns about child and adolescent survival has naturally shifted to the well-being and social implications of having a stigmatizing and transmittable disease (Lowenthal et al., 2014). In this context, while a number of studies have reported on the negative consequences associated with PHIV+ status (Mellins & Malee, 2013; Mellins et al., 2009; Mellins et al., 2012), it is just as important to examine those elements that contribute to the positive development of PHIV+ youth (Mellins et al., 2014; Sherr, Croome, Parra Castaneda, & Bradshaw, 2014).
Using the results from baseline data of two RCTs of the VUKA family intervention, the study set out to examine the contextual, social, and self-regulation factors that are associated with positive mental health outcomes among PHIV+ youth. The data indicated that there are factors from each of three SAT domains that were associated with youth prosocial behaviors, total difficulties and depression, providing guidance for much-needed evidence-based interventions for PHIV+ children reaching adolescence, worldwide.
Contextual factors appeared to have a significant influence on PHIV+ adolescent resilience, including household size and caregiver factors. Household size may reflect caregiver burden arising from a crowded household as well as emotional and financial burden (DSD, SASSA, & UNICEF, 2012). Conversely, as has been found in other studies of vulnerable youth affected by HIV, caregiver factors, such as better education and more limited depression symptoms may increase caregiver capacity to provide emotional support to PHIV+ adolescents (Cluver, Boyes, et al., 2013; Cluver, Orkin, et al., 2013).
Social regulation factors within family contexts were also associated with positive youth outcomes particularly the frequency with which caregivers communicated and provided supervision for their children. Also, greater supervision by caregivers was inversely associated with mental health (lower depression) among youth. Social regulation factors that include parental warmth and care and supervision by a caregiver may prove to be vital to promoting resilience among youth (Fergus & Zimmerman, 2005). However, less communication about difficult topics was associated with fewer total behavioral problems. It is possible that youth who have fewer behavioral difficulties may require less discussion about problems with their caregivers.
Finally, self-regulation is closely related to achieving healthy cognitive, behavioral, emotional, and mental health functioning (National Research Council and Institute of Medicine, 2009) and has implications for how PHIV+ adolescents manage their chronic illness. The coping methods employed by PHIV+ adolescents included resignation and wishful thinking. While these avoidant coping strategies may not be viewed as health-promoting in themselves, as they are reactive and lack active problem-solving components, they may be appropriate for some youth in a limited resource context filled with stressors out of the control of children. It is also possible that they may later become the basis of youth developing more active coping responses. It is also likely a feature of the developmental status of early adolescents in this study. Actively seeking support from others, higher self-concept, and less internalized stigma were all correlated with better mental health among PHIV+ adolescents. The development of a healthy sense of self (self-concept) and greater acceptance of their HIV status has been found to be important in other vulnerable youth (Ungar et al., 2007) and thus, may also be important to promoting resilience in PHIV+ adolescents.
The study has a number of limitations that affect the generalizability of our findings. First, even though the original samples were randomized, they do represent a sample of convenience for the purposes of this paper. It is likely that given that we drew our samples from those in care and who consented to participate in the RCTs, it may not reflect the larger PHIV+ adolescent population. Also, the data are cross-sectional and consists of self-report data which further limits the conclusions that can be drawn. Nor is it possible to disentangle the factor of time between the pilot and the larger trial. Finally, in an effort to minimize discomfort to respondents, we endeavored to keep our measurement battery to less than an hour and many other important factors in understanding PHIV+ adolescent resilience may not have been assessed.
Conclusion
In spite of the limitations, this study highlights the importance of studying high-risk populations, particularly in ways that avoid promoting only deficit-focused perspectives on PHIV+ adolescents. Despite the context of poverty and few resources, this study suggests that the mechanisms with which PHIV+ adolescents and their caregivers adapt and respond to a chronic illness are as much a function of the familial and community resources to which they have access as it is to the availability of early treatment. Participating families demonstrate resilience in various ways which appear to be nested within various contextual and social arrangements. Although longitudinal studies with larger samples will be critical to determine pathways of causality, these findings are encouraging and align with existing findings from other vulnerable populations, namely that parental supervision and communication, and youth self-esteem and low internalized stigma are factors that may promote resilience in PHIV+ youth. Thus, our data provide an important base for much-needed evidence-based interventions that are health- and mental health-promoting among PHIV+ youth and their caregivers.
Acknowledgements
The authors want to acknowledge the time and contributions of the children and caregivers who participated in this study and the research staff who worked with them to collect the data. In addition, we wish to thank our collaborators at the Human Sciences Research Council and University of KwaZulu-Natal.
Funding Statement
This work was supported by several grants from the National Institutes of Health, including, “Adapting Champ+ For South Africa: Supporting HIV-Infected Youth and Families” [R21 NR010474; PI: Mellins] and “VUKA Family Program: Supporting Perinatally HIV+ Youth in South Africa” [R01 HD074052; PI: McKay]. The research was also supported by an NIMH center grant to the HIV Center for Clinical and Behavioral Studies at the New York State Psychiatric Institute and Columbia University [P30-MH43520;PI: Remien].
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Bachmann M. O., Booysen F. L. 2003 Health and economic impact of HIV/AIDS on South African households: A cohort study. BMC Public Health, 3, 14. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12667263.
- Bauermeister J. A., Elkington K. S., Robbins R. N., Kang E., Mellins C. A. A prospective study of the onset of sexual behavior and sexual risk in youth perinatally infected with HIV. Journal of sex research. 2012;(5):413–422. doi: 10.1080/00224499.2011.598248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A. T., Brown G., Steer R. A. Beck depression inventory II manual. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Bell C. C., Bhana A., Petersen I., McKay M. M., Gibbons R., Bannon W., Amatya A. Building protective factors to offset sexually risky behaviors among black youths: A randomized control trial. Journal of the National Medical Association. 2008;(8):1–9. doi: 10.1016/S0027-9684(15)31408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzies K., Mychasiuk R. Fostering family resiliency: A review of the key protective factors. Child & Family Social Work. 2009;(1):103–114. doi: 10.1111/j.1365-2206.2008.00586.x. [DOI] [Google Scholar]
- Bhana A., McKay M. M., Mellins C., Petersen I., Bell C. Family-based HIV prevention and intervention services for youth living in poverty-affected contexts: The CHAMP model of collaborative, evidence-informed programme development. Journal of the International AIDS Society. 2010;(Suppl 2):S8. doi: 10.1186/1758-2652-13-S2-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhana A., Mellins C. A., Petersen I., Alicea S., Myeza N., Holst H., McKay M. The VUKA family program: Piloting a family-based psychosocial intervention to promote health and mental health among HIV infected early adolescents in South Africa. AIDS Care. 2014;(1):1–11. doi: 10.1080/09540121.2013.806770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birungi H., Mugisha J. F., Obare F., Nyombi J. K. Sexual behavior and desires among adolescents perinatally infected with human immunodeficiency virus in Uganda: Implications for programming. Journal of Adolescent Health. 2009;(2):184–187. doi: 10.1016/j.jadohealth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Bomba M., Nacinovich R., Oggiano S., Cassani M., Baushi L., Bertulli C., Badolato R. Poor health-related quality of life and abnormal psychosocial adjustment in Italian children with perinatal HIV infection receiving highly active antiretroviral treatment. AIDS Care. 2010;(7):858–865. doi: 10.1080/09540120903483018. [DOI] [PubMed] [Google Scholar]
- Catalano R. F., Hawkins J. D., Berglund M. L., Pollard J. A., Arthur M. W. Prevention science and positive youth development: Competitive or cooperative frameworks? Journal of Adolescent Health. 2002;(6 Suppl.):230–239. doi: 10.1016/S1054-139X(02)00496-2. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12470920. [DOI] [PubMed] [Google Scholar]
- Cluver L., Boyes M., Orkin M., Sherr L. Poverty, AIDS and child health: Identifying highest-risk children in South Africa. South African Medical Journal. 2013;(12):910–915. doi: 10.7196/samj.7045. [DOI] [PubMed] [Google Scholar]
- Cluver L., Orkin M., Boyes M. E., Sherr L., Makasi D., Nikelo J. Pathways from parental AIDS to child psychological, educational and sexual risk: Developing an empirically-based interactive theoretical model. Social Science & Medicine. 2013:185–193. doi: 10.1016/j.socscimed.2013.03.028. [DOI] [PubMed] [Google Scholar]
- Davies M. A., Phiri S., Wood R., Wellington M., Cox V., Bolton-Moore C. IeDEA Southern Africa Steering Group Temporal trends in the characteristics of children at antiretroviral therapy initiation in Southern Africa: The IeDEA-SA collaboration. PLoS ONE. 2013;(12):e81037. doi: 10.1371/journal.pone.0081037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DSD, SASSA, & UNICEF 2012 The South African child support grant impact assessment: Evidence from a survey of children, adolescents and their households. Retrieved from Pretoria: http://www.unicef.org/southafrica; http://www.dsd.gov.za and http://www.sassa.gov.za.
- Elkington K. S., Bauermeister J. A., Brackis-Cott E., Dolezal C., Mellins C. A. Substance Use and sexual risk behaviors in perinatally human immunodeficiency virus-exposed youth: Roles of caregivers, peers and HIV status. Journal of Adolescent Health. 2009;(2):133–141. doi: 10.1016/j.jadohealth.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewart C. K. Social action theory for a public health psychology. American Psychologist. 1991;(9):931–946. doi: 10.1037/0003-066X.46.9.931. [DOI] [PubMed] [Google Scholar]
- Fergus S., Zimmerman M. A. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health. 2005:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- Fitts W. H., Warren W. L. Tennessee self-concept scale, TSCS:2. Manual. 2nd ed. Los Angeles: Western Psychological Services; 1996. [Google Scholar]
- Gadow K. D., Angelidou K., Chernoff M., Williams P. L., Heston J., Hodge J., Nachman S. Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. Journal of Developmental & Behavioral Pediatrics. 2012;(6):456–468. doi: 10.1097/DBP.0b013e31825b8482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow K. D., Chernoff M., Williams P. L., Brouwers P., Morse E., Heston J., Nachman S. Co-occurring psychiatric symptoms in children perinatally infected with HIV and peer comparison sample. Journal of Developmental & Behavioral Pediatrics. 2010;(2):116–128. doi: 10.1097/DBP.0b013e3181cdaa20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Kapetanovic S., Wiegand R. E., Dominguez K., Blumberg D., Bohannon B., Wheeling J., Consortium L. Associations of medically documented psychiatric diagnoses and risky health behaviors in highly active antiretroviral therapy-experienced perinatally HIV-infected youth. AIDS Patient Care and STDs. 2011;(8):493–501. doi: 10.1089/apc.2011.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kia-Keating M., Dowdy E., Morgan M. L., Noam G. G. Protecting and promoting: An integrative conceptual model for healthy development of adolescents. Journal of Adolescent Health. 2011;(3):220–228. doi: 10.1016/j.jadohealth.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The children’s depression, inventory (CDI) Psychopharmacol Bull. 1985;(4):995–998. [PubMed] [Google Scholar]
- Kuo C., Operario D. Health of adults caring for orphaned children in an HIV-endemic community in South Africa. AIDS care. 2011;(9):1128–1135. doi: 10.1080/09540121.2011.554527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowenthal E. D., Bakeera-Kitaka S., Marukutira T., Chapman J., Goldrath K., Ferrand R. A. Perinatally acquired HIV infection in adolescents from Sub-Saharan Africa: A review of emerging challenges. The Lancet Infectious Diseases. 2014;(7):627–639. doi: 10.1016/S1473-3099(13)70363-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S. S., Sawyer J. A., Brown P. J. Conceptual issues in studies of resilience: Past, present, and future research. Annals of the New York Academy of Sciences. 2006:105–115. doi: 10.1196/annals.1376.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay M., Paikoff R., editors. Community collaborative partnerships: The foundation for HIV prevention research efforts in the United States and internationally. New York: Haworth Press; 2007. [Google Scholar]
- Mellins C. A. 2013 Behavioral challenges in perinatally HIV youth (Invited paper) Paper presented at the 20th conference on Retroviruses and Opportunistic Infections (CROI), Atlanta.
- Mellins C. A., Brackis-Cott E., Dolezal C., Leu C. S., Valentin C., Meyer-Bahlburg H. F. L. Mental health of early adolescents from high-risk neighborhoods: The role of maternal HIV and other contextual, self-regulation, and family factors. Journal of Pediatric Psychology. 2008;(10):1065–1075. doi: 10.1093/jpepsy/jsn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Elkington K. S., Bauermeister J. A., Brackis-Cott E., Dolezal C., McKay M., Abrams E. J. Sexual and drug use behavior in perinatally HIV-infected youth: Mental health and family influences. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;(8):810–819. doi: 10.1097/CHI.0b013e3181a81346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Elkington K. S., Leu C.-S., Santamaria E. K., Dolezal C., Wiznia A., Abrams E. J. Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care. 2012;(8):953–962. doi: 10.1080/09540121.2012.668174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Malee K. M. Understanding the mental health of youth living with perinatal HIV infection: Lessons learned and current challenges. Journal of the International AIDS Society. 2013:18593. doi: 10.7448/ias.16.1.18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Nestadt D., Bhana A., Petersen I., Abrams E. J., Alicea S., McKay M. Adapting evidence-based interventions to meet the needs of adolescents growing up with HIV in South Arica: The VUKA case example. Global Social Welfare. 2014 doi: 10.1007/s40609-014-0023-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Tassiopoulos K., Malee K., Moscicki A.-B., Patton D., Smith R., Seage G. R. Behavioral health risks in perinatally HIV-exposed youth: Co-occurrence of sexual and drug Use behavior, mental health problems, and nonadherence to antiretroviral treatment. AIDS patient care and STDs. 2011;(7):413–422. doi: 10.1089/apc.2011.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mofenson L. M., Cotton M. F. Perinatally HIV-infected adolescents. Journal of International AIDS Society. 2013;(Special issue):1–3. doi: 10.7448/IAS.16.1.18778. [DOI] [Google Scholar]
- Myer L., Smit J., Roux L. L., Parker S., Stein D. J., Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS patient care and STDs. 2008;(2):147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- Nassen R., Donald K., Walker K., Paruk S., Vujovic M., Duncan W., Wilmshurst J. Management of mental health disorders and central nervous system sequelae in HIV-positive children and adolescents. Southern African Journal of HIV Medicine. 2014;(3):81–96. doi: 10.7196/sajhivmed.1091. [DOI] [Google Scholar]
- National Research Council and Institute of Medicine 2009Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Committee on prevention of mental disorders and substance abuse among children, youth and young adults: Research advances and promising interventionshttp://www.ncbi.nlm.nih.gov/books/NBK32775/
- Petersen I., Bhana A., Myeza N., Alicea S., John S., Holst H., Mellins C. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: A qualitative investigation. AIDS Care. 2010;(8):970–978. doi: 10.1080/09540121003623693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puthanakit T., Siberry G. K. Bone health in children and adolescents with perinatal HIV infection. Journal of the International AIDS Society. 2013:1–10. doi: 10.7448/IAS.16.1.18575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L. S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Sherr L., Croome N., Parra Castaneda K., Bradshaw K. A systematic review of psychological functioning of children exposed to HIV: Using evidence to plan for tomorrow’s HIV needs. AIDS and Behavior. 2014;(11):2059–2074. doi: 10.1007/s10461-014-0747-6. [DOI] [PubMed] [Google Scholar]
- Sohn A. H., Hazra R. The changing epidemiology of the global paediatric HIV epidemic: Keeping track of perinatally HIV-infected adolescents. Journal of the International AIDS Society. 2013;(1):18555. doi: 10.7448/IAS.16.1.18555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sopena S., Evangeli M., Dodge J., Melvin D. Coping and psychological adjustment in adolescents with vertically acquired HIV. AIDS Care. 2010;(10):1252–1258. doi: 10.1080/09540121003668110. [DOI] [PubMed] [Google Scholar]
- Spirito A., Stark L. J., Williams C. Development of a brief coping checklist for use with pediatric populations. Journal of Pediatric Psychology. 1988;(4):555–574. doi: 10.1093/jpepsy/13.4.555. [DOI] [PubMed] [Google Scholar]
- Ssewamala F. M., Han C. K., Neilands T. B. Asset ownership and health and mental health functioning among AIDS-orphaned adolescents: Findings from a randomized clinical trial in rural Uganda. Social Science and Medicine. 2009;(2):191–198. doi: 10.1016/j.socscimed.2009.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele G. I., Edwards D. J. Development and validation of the Xhosa translations of the Beck Inventories: 2. Item analysis, internal consistency and factor analysis. Journal of Psychology in Africa. 2008;(2):217–226. [Google Scholar]
- Stein A., Desmond C., Garbarino J., Van I. M. H., Barbarin O., Black M. M., Richter L. M. Predicting long-term outcomes for children affected by HIV and AIDS: Perspectives from the scientific study of children’s development. AIDS. 2014;(Suppl. 3):S261–S268. doi: 10.1097/QAD.0000000000000328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassiopoulos K., Moscicki A. B., Mellins C., Kacanek D., Malee K., Allison S., Pediatric H. I. V. A. C. S. Sexual risk behavior among youth with perinatal HIV infection in the United States: Predictors and implications for intervention development. Clinical Infectious Diseases. 2013;(2):283–290. doi: 10.1093/cid/cis816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traube D., Dukay V., Kaaya S., Reyes H., Mellins C. Cross-cultural adaptation of the child depression inventory for use in Tanzania with children affected by HIV. Vulnerable Children and Youth Studies. 2010;(2):174–187. doi: 10.1080/17450121003668343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS 2014 90–90–90 An ambitious treatment target to help end the AIDS epidemic. Retrieved from http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf.
- Ungar M., Brown M., Liebenberg L., Othman R., Kwong W. M., Armstrong M., Gilgun J. Unique pathways to resilience across cultures. Adolescence. 2007;(166):287–310. [PubMed] [Google Scholar]
- Van Dyke R. B., Patel K., Kagan R. M., Karalius B., Traite S., Meyer W. A., Hazra R. Antiretroviral drug resistance among children and youth in the U.S. with perinatal HIV. Clinical Infectious Diseases. 2016 doi: 10.1093/cid/ciw213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook L. E., Bauman L. J., Shinnar S. Applying stigma theory to epilepsy: A test of a conceptual model. Journal of Pediatric Psychology. 1992;(5):633–649. doi: 10.1093/jpepsy/17.5.633. [DOI] [PubMed] [Google Scholar]
- Williams P. L., Leister E., Chernoff M., Nachman S., Morse E., Di Poalo V., Gadow K. D. Substance use and its association with psychiatric symptoms in perinatally HIV-infected and HIV-affected adolescents. AIDS and Behavior. 2010;(5):1072–1082. doi: 10.1007/s10461-010-9782-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youth in Mind doi: 10.1111/j.1475-3588.2007.00443_2.x. SDQ. Information for researchers and professionals about the Strengths & Difficulties Questionnaires. Retrieved April, 2016, from http://www.sdqinfo.com/ [DOI] [PubMed]
- Zolkoski S. M., Bullock L. M. Resilience in children and youth: A review. Children and Youth Services Review. 2012:2295–2303. doi: 10.1016/j.childyouth.2012.08.009. [DOI] [Google Scholar]


