Abstract
Background: Acupuncture use is increasing worldwide for many conditions, including movement disorders. Clinical research in acupuncture has also increased to test anecdotal reports of clinical benefits empirically and investigate potential mechanisms.
Method: This article describes considerations for designing a double-blinded, randomized, placebo-controlled clinical trial of acupuncture for fatigue in Parkinson's disease (PD) and describes the current authors' experience in the implementation and early conduct of this trial. Relevant literature is also reviewed to provide guidance for other researchers seeking to perform clinical research relevant to PD and related disorders.
Results: Trial design should be driven by a well-defined research question and sufficient detail to meet Standards for Reporting Interventions in Clinical Trials of Acupuncture criteria when a trial is complete. Important items for review include: randomization and blinding; recruitment and participant selection; sham methodology choice; staff training; and practical implementation of study procedures. Sample forms used for the current authors' trial are shared.
Conclusions: High-quality clinical trials of acupuncture can provide valuable information for clinicians, patients, and policymakers. Acupuncture trials differ in critical ways from pharmaceutical trials and might require additional considerations regarding design and implementation. Adequate preparation for the unique challenges of acupuncture studies can improve trial implementation, design, efficiency, and impact.
Keywords: : Complementary and Alternative Medicine, Neurologic Disorders, Parkinson's Disease, Sham Acupuncture
Introduction
Acupuncture use is expanding in Western societies both in terms of numbers of patients and conditions treated.1,2 Studies of the clinical efficacy and mechanisms of acupuncture have also expanded.3 Unfortunately, most meta-analyses of acupuncture trials, including trials involving Parkinson's disease (PD), are inconclusive because of the lack of adequately powered high-quality studies.4 While reporting issues for acupuncture research trials have been addressed by Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines,5 there are few published guidelines on the conduct and design of acupuncture trials, with the most recent comprehensive guidelines being from 2002, and few articles offering practical guidance on trial conduct. This is important, as there are unique challenges in acupuncture research that frustrate efforts to simply substitute acupuncture for pills in standard pharmaceutical trial designs.6
This article discusses the planning, design, and implementation of a double-blinded, randomized placebo-controlled trial of acupuncture for fatigue in PD. There is also a review of relevant literature to offer guidance for researchers who want to perform clinical acupuncture trials. Readers who are interested in the outcomes of the PD study can check the results that were published.7
Study Design
The PD study was designed to determine whether or not acupuncture relieved symptoms of fatigue in patients with PD who had moderate-to-severe fatigue and who were already receiving standard medical treatments. Participants were randomized in a 1:1 ratio to receive 6 weeks of twice-weekly verum or sham acupuncture. A double-blinded, placebo-controlled, randomized trial design was chosen, given high placebo response rates in PD, including in prior acupuncture trials.4,8
General Design
Study design should be driven by a clearly articulated research question. Potential study objectives include determining the relative efficacy of acupuncture versus Western standards of care;9 determining if acupuncture augments standard of care;10–12 determining the efficacy of acupuncture as a stand-alone treatment; describing the efficacy of acupuncture in community practice;13 determining acupuncture mechanisms;14–16 or comparing specific acupuncture approaches. While randomization, blinding, and a sham control are necessary to address certain questions, these items are not always required and could add unnecessary expense and time.
Control and Randomization
Acupuncture research performed without a control group may have value for describing community practice patterns, novel approaches, case series of relatively rare conditions, or comparing acupuncture treatment to natural history data.17–20 Options for prospective control groups include standard/usual care, wait-list, comparison between two active treatment protocols, or use of a placebo/sham acupuncture method.21 To separate potential sources of therapeutic effects fully, it might be necessary to use multiple controls, for example, using a wait-list control to assess effects related to measurement and natural history; a sham treatment control to assess “nonspecific” acupuncture procedure effects; and a verum treatment group to assess acupuncture-specific effects.15,22 For prospective controlled trials, randomization is generally recommended to reduce bias and should follow Consolidated Standards for Reporting Trials (CONSORT) guidelines.23,24
Participants
Participants in the PD study were ages 40–100; diagnosed with PD using UK Brain Bank Criteria;25 and reported moderate-to-severe fatigue on the Movement Disorders Society Unified Parkinson's Disease Rating Scale (UPDRS) fatigue item.26 Participants were excluded if they had dementia or a Montreal Cognitive Assessment score below 2427; active depression or a Hospital Anxiety and Depression Scale depression subscale of ≥11;28 an untreated sleep disorder; other neurologic disorders, including moderate-to-severe neuropathy; or another medical condition associated with fatigue (e.g., heart failure). Initially, participants with any prior acupuncture exposure were excluded because of concerns that prior acupuncture experience could interfere with blinding.29 However, because of recruitment issues and low concerns regarding patients with few exposures, the study criteria were subsequently modified to allow participants with no acupuncture for the past 6 months. No bias was detected in these participants and all participants were monitored for treatment assignment perceptions.
Inclusion and Exclusion Criteria
Inclusion criteria may be based on Western medical diagnostic criteria, Eastern diagnosis, combined diagnoses, or stand-alone symptoms, such as tremor. Exclusion criteria may include medical conditions that make it difficult to receive treatments, complicate data interpretation, or when acupuncture is contraindicated. For example, some acupuncture points are contraindicated during pregnancy30 and patients with pacemakers should not receive electrical stimulation.31,32 People taking chronic anticoagulants may bruise or bleed slightly but are safe for most protocols.33 The current study included patients with deep brain stimulation without any noted adverse effects. Including participants with prior acupuncture experience is contentious. Some studies suggest that acupuncture-experienced participants might distinguish sham from verum acupuncture more easily, and these studies suggest that such individuals should be excluded from acupuncture trials.29,34 However, this practice could limit recruitment in areas of the country where acupuncture use is prevalent and could exclude participants who would be most interested in acupuncture. In either case, this issue should be addressed and the criteria should be justified.
Specific challenges to consider with movement disorders include tremor and dyskinesia, which could interfere with receiving treatments and/or blinding. In the current authors' experience, this was not an issue and patients often commented on the experience of “stillness” during treatment. Acupuncture staff may need to be trained regarding mobility and fall risk issues. Severe neuropathy may interfere with perception of both verum and sham treatments, and dementia may interfere with reliability of certain outcome measures.
Outcome Measures
Outcome measures were collected at baseline, 3-weeks into treatment, following the final treatment (6-weeks), and also at 3 and 6 weeks post-treatment to assess the durability of effects. The current study's primary outcome was the difference between the verum and sham groups in change from baseline to 6 weeks on the Modified Fatigue Impact Scale (MFIS). The MFIS was chosen because of its sensitivity to change, compared to other fatigue scales.35 Secondary outcome measures included results on: the Parkinson's Disease Questionnaire measure of health-related quality of life;36 the Parkinson's Disease Sleep Scale;37 the Epworth Sleepiness Scale;38 the Hospital Anxiety and Depression Scale;28 the Apathy Scale;39 the UPDRS to assess motor function and activities of daily living40; and clinical global impression of improvement scores from patients, caregivers, and clinicians.41
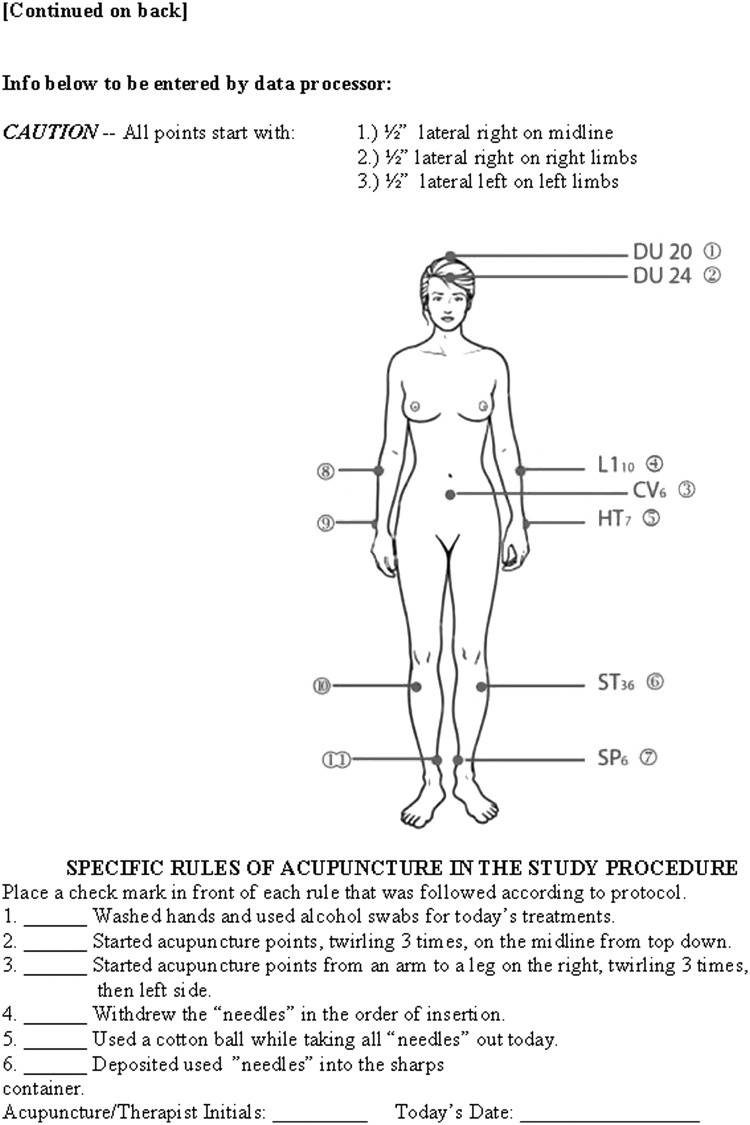
Acupuncture Procedure
Treatment in the current study consisted of twice-weekly sessions for 6 weeks and used a fixed-point prescription based on Traditional Chinese Medicine (TCM) theory and prior articles about PD and fatigued populations.42–44 Participants lay face up on the acupuncture table and were blindfolded. All acupuncture points were swabbed with alcohol. For verum treatment, acupuncture needles (Seirin®, 36 gauge, 1-inch) were inserted to a depth of 0.5–1 cun in the following order: Du 20 and Du 24, and Ren 6 (midline points); right LI 10 and right HT 7 (upper extremity points); right ST 36 and right SP 6 (lower extremity points); left LI 10 and left HT 7 (upper extremity points); and left ST 36 and left SP 6 (lower extremity points). For each point, the needle was twisted three times to the right. The De Qi sensation was not elicited explicitly because of the blinded nature of the study. After 15 minutes, the acupuncturist returned to the room to check on the participant. After 30 minutes, the acupuncturist removed the needles in the same order as they were inserted and swabbed each point with alcohol, dropping the needles into a sharps container at every three removals. Each patient received two treatments per week at least 1 day apart for 6 weeks. There were no other components to the treatment.
For the sham procedure, each point was swabbed with alcohol and a sharp round toothpick in a guide tube was placed on the sham point and tapped on the skin.45 The toothpick was twisted three times to the right in the guide tube (the toothpicks were longer than the guide tubes). Then, each toothpick and guide tube was discarded into a trashcan located in the treatment room and covered with tissues. These toothpicks were mock inserted in the same order as the verum acupuncture protocol except that nonacupuncture points were used; these points were located 0.5 inches lateral to the traditional acupuncture points, or to the right for midline points. The acupuncturist mock removed the toothpicks by pressing a new toothpick into the sham point slowly and quickly removing it in the same order they were “inserted.” The toothpicks were discarded three at a time into a sharps container to mimic the sounds heard with verum treatment.
Acupuncture Treatment
There are numerous styles and approaches to acupuncture treatment including TCM, Five-Element, Japanese, Korean Hand, auricular, microsystems, and medical acupuncture.46 TCM is the style most commonly practiced by acupuncturists in the United States and is the basis of the board examination for the National Certification Commission of Acupuncture and Oriental Medicine.47 For prospective trials, fixed or fluid acupuncture-point prescriptions may be used.
A fixed-point prescription means the same combination of acupuncture points are used for all participants, typically based on prior research studies, common practice patterns, or theoretical considerations. Advantages of fixed-point prescriptions include reproducibility, ease of creating placebo controls, and reduced practitioner bias. The primary disadvantage is that acupuncture is typically practiced in a more nuanced and individualized manner, thus leading to the argument that fixed-point prescriptions may be suboptimal for many participants.
Fluid acupuncture point prescription allows different acupuncture points to be used for each participant. This may range from a core set of acupuncture points with additional optional points provided at the acupuncturist's discretion to completely individualized treatment plans.48,49 Advantages of fluid point prescriptions are individualized treatment for each participant and closer approximation of verum-world practice. Disadvantages include the burden of recording points for each treatment, difficulty in reproducing study results, potential for experimental bias, and difficulties in designing appropriate controls.
However, newer research needles capable of blinding acupuncturists may overcome many of these shortcomings.50 For both fixed and fluid prescriptions, treatments should be based on the best available clinical evidence, including the duration of treatments (e.g., 30–60 minutes) and the frequency and total number of sessions (e.g., 2 sessions per week for 6 weeks). Per STRICTA guidelines, specific aspects of needling should be described, including the needle brand, gauge, and length; the insertion order; depth; and any needle manipulations, such as twisting or thrusting.5 The prescription of adjunct therapies often used in TCM practice, such as moxibustion, cupping, or herbal prescriptions, should be noted if used.
Blinding and Sham Acupuncture Techniques
Blinding in acupuncture studies typically refers to the blinding of participants to their group assignments and/or blinding of raters with no blind required for the treating acupuncturist who is typically unblinded in order to perform study procedures accurately. However, several innovative needle devices allow blinding of the acupuncturist and can offer advantages in terms of reducing nonverbal cues and other potential sources of bias.50 At the end of the study, participants, evaluators, and acupuncturists (if blinded) should be queried to assess the adequacy of blinding.
Sham acupuncture may be characterized by whether the needles used are penetrating (breaking the skin) or nonpenetrating and whether they are placed on or off acupuncture points.51–53 Penetrating needles offer the advantage of nearly identical skin sensations and ease of use, but are potentially confounded by nonspecific needling effects (clinical benefits of needling unrelated to specific placement).54 Thus, most studies now utilize nonpenetrating sham devices.
The two most common nonpenetrating sham needle devices are the Park Sham Device and the Streitberger Placebo Needle.55,56 Both use blunted, telescopic needles that give the illusion of being inserted into the skin. The needle is either held in place with tape around the acupuncture point or with a base unit designed to hold the needle and guide tube. Studies support the validity of mimicking verum needle sensation without a need for physical blindfolding.55,57 Other devices, such as the skin-touch placebo needle, may additionally allow acupuncturist blinding.50 These needles may be cumbersome for the acupuncturist to use, require additional training, and add expense to a study. Another sham method involves toothpicks placed in guide tubes, and this method has also been validated to mimic acupuncture sensations, at least in acupuncture-naïve participants.29,58 This method is less expensive than manufactured sham needles but requires physical blindfolding and acupuncturist training.
Needle/sham placement may be done off acupuncture points/meridians, at identical points (with nonpenetrating needles), or at acupuncture points not indicated for the condition being researched.59,60 Placement at identical points, even with nonpenetrating needles, is generally not recommended because of the possibility of acupressure effects.61 Thus, the most appropriate sham points, even for nonpenetrating needles, are located away from verum acupuncture points, away from acupuncture meridians, and at locations that can be reproduced reliably.
Statistical Analysis and Power
Assuming a 10% dropout rate, a sample size of 105 patients was selected for the current study to provide at least 80% power at 0.05 significance to detect a previously defined, minimal clinically significant difference between groups of 10-points on the MFIS.62 Differences in change between groups for both primary and secondary outcomes will be assessed using repeated measures analysis of covariance.
Implementation
Budget and Study Setting
Acupuncturists may be paid per treatment, based on the average regional costs, or by percent of full-time effort. Funds should be set aside for acupuncture needles, sham devices, and other related supplies (e.g., eye covers, cotton balls, alcohol pads). Treatments can be administered at a private office, school of acupuncture, or medical facility. If multiple sites are used, efforts should be made to ensure consistency in clinic rooms as much as possible (e.g., music, lights).
Recruitment Challenges
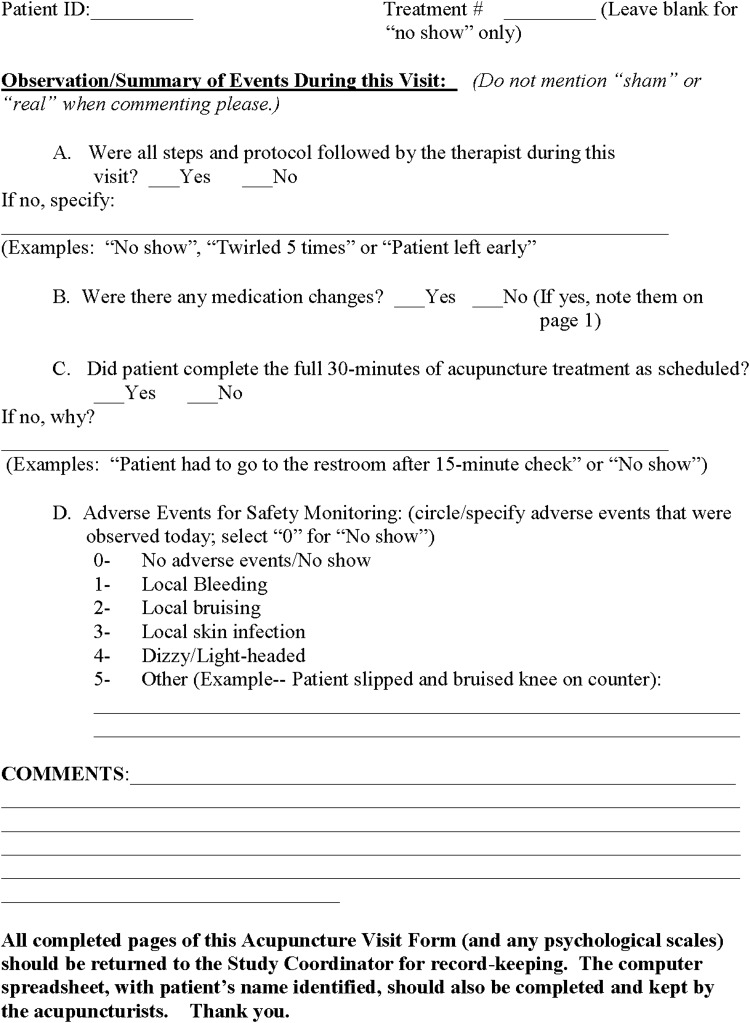
Compared to pharmacologic studies, most acupuncture studies involve multiple treatments over several weeks and thus place greater time and travel demands on participants. In the current study, travel to the University of Colorado Hospital Center for Integrative Medicine was a leading reason for screening failures leading the current authors to open several satellite sites. When determining recruitment numbers, the attrition rate should be considered, depending on the patient population and treatment regimen. The attrition rate in acupuncture studies can range from 10% to 75% with most studies having ∼10%–20% attrition.61,63 During the consent process, the current author inform patients clearly about the possibility of receiving a placebo form of acupuncture, without providing details on how this is to be performed. While this resulted in losing a small number of participants, it was preferable to misrepresenting the placebo as a “form of acupuncture” or biasing participants with additional information about the sham procedure.
Acupuncturist Training
For controlled trials, additional training is needed, even for experienced acupuncturists, to ensure consistency of both verum and placebo treatments. Practice sessions involving other study personnel, acupuncture-naïve, and acupuncture-experienced volunteers helps ensure consistency of needling techniques, placement, adequacy of blinding procedures, and similarity between verum and placebo treatments. This training is particularly valuable for trials in which participants might be treated by multiple acupuncturists. As acupuncturists' interactions with patients may contribute to the therapeutic effect, these interactions should be rehearsed and staff should agree upon how to handle common questions.
For the current study, there are 3 acupuncturists with more than 15 years of clinical experience each, all licensed in the state of Colorado and trained in TCM. They were involved in the original study design, including a review of the literature, discussion, and agreement of point selection. They practiced patient intakes, the verum and sham procedures, and form completion with each other; this also helped validate the blinding procedure as these acupuncturists could not tell if they were receiving verum or sham acupuncture from their colleagues. We recommend acupuncturist training every 6–12 months, depending on the length of the study. We had a day to review protocol and procedures and to practice every 6 months for the current study.
Participant and Room Preparation
To ensure an efficient study, it is helpful to have visit checklists and to provide participants with instructions, including wearing loose fitting clothing, avoiding heavy meals or fasting before procedures, taking regular medications, and avoiding use of heavy lotions that can irritate acupuncture points (see Appendices 1 and 2).64 As multiple acupuncturists performed in the current study, each participant was also provided with a punch card to track treatments and provide additional assurance of receiving the correct number of treatments.
Each room should have a treatment table, alcohol swabs, cotton balls, a sharps container, two identical containers for acupuncture needles and sham devices, a box of facial tissues, and an eye mask. For comfort, a blanket or infrared lamp may be added. For safety, especially in studies requiring blindfolding of participants, there should be a mechanism by which the participant can call the acupuncturist into the room without needing to move, such as a baby monitor. A timer should be used to maintain consistency of needle-retention time.
Sham Needling and Removal Procedure
The sham procedure should mimic the verum procedure as much as possible including swabbing points with alcohol before insertion and after removal; order of point insertion and removal; sounds of needles being removed from packages and thrown in sharps containers; and a final swab with cotton at all points regardless of bleeding. The current authors' experience with trial participants confirmed that they pay close attention to somatic cues (e.g., noting if a placebo “needle” was “removed” from a different point from where it was inserted) and auditory cues (e.g., sounds of placebo “needles” being rattled in a sharps container).
Discussion
Acupuncture presents many distinctive challenges for clinical research.65 As with reporting, guidelines are needed for developing appropriate acupuncture treatment trials to improve the quality and reliability of data. It is hoped that the considerations described in this article will assist in planning future studies and improve the feasibility and credibility of future acupuncture research in general, as well as addressing special considerations for design of acupuncture trials for a population with PD. The current authors suggest using the materials presented here with the STRICTA guidelines5 and the CONSORT statement.24
The common practice of standardized treatment protocols runs contrary to the core philosophy of many forms of acupuncture, which are typically based on an individuals' unique manifestation of signs, symptoms, and imbalances. This creates a quandary between an optimal scientific study design of potentially suboptimal and routinized acupuncture and a suboptimal scientific study of optimized and individualized treatment. It is also possible that the design of sham-controlled acupuncture studies underestimate the benefits of acupuncture by subtracting “nonspecific” effects that are essential to the acupuncture experience, including interactions with acupuncturists, patient expectations, relaxation, and focusing on the body.65
Further research relevant to optimizing the design of acupuncture trials is needed to advance this field and improve the clinical relevance of research in this area. This includes approaches to study design, optimizing sham techniques, studies on whether or not acupuncture exposure biases results, and mechanistic studies to determine whether and how acupuncture effects differ from traditional placebo effects.66
Conclusions
There are numerous issues that need to be addressed when conducting blinded acupuncture randomized controlled trials (RCTs) on patients with PD. This article expanded upon the components of study design and implementation, provided insight into how evaluation of acupuncture for the symptom of fatigue in patients with PD was carried out, and relevant forms for quick reference. The guidelines for design and implementation of acupuncture RCTs in this article will be useful for scientists who are interested in conducting such research.
Appendix 1. Sample Checklist for Participants
Appendix 2. Sample Acupuncturist Study Visit Checklist.
Acknowledgments
This work was supported by the Michael J. Fox Foundation Grant # 5264, the National Institutes of Health/Colorado Clinical and Translational Sciences Institute KL2 program (NIH/NCATS 8 KL2 TR000156-05), the Center for Integrative Medicine at the University of Colorado Hospital, and the Colorado School of Traditional Chinese Medicine. The authors would also like to thank Veronica Parra, Ted J. Kaptchuk, MD, and Etta Abaca for their assistance on this project and the manuscript for this article.
Author Disclosure Statement
None of the authors have any conflicts of interests.
References
- 1.Barnes PM BB, Nahin RL. Complementary and Alternative Medicine Use Among Adults and Children. Hyattsville, MD: National Center for Health Statistics; 2008 [PubMed] [Google Scholar]
- 2.Burke A. Upchurch DM, Dye C, Chyu L. Acupuncture use in the United States: Findings from the National Health Interview survey. J Altern Complement Med. 2006;12(7):639–648 [DOI] [PubMed] [Google Scholar]
- 3.Lewith GT, White PJ, Kaptchuk TJ. Developing a research strategy for acupuncture. Clin J Pain. 2006;22(7):632–638 [DOI] [PubMed] [Google Scholar]
- 4.Lee MS, Shin BC, Kong JC, Ernst E. Effectiveness of acupuncture for Parkinson's disease: A systematic review. Mov Disord. 2007;23(11):1505–1515 [DOI] [PubMed] [Google Scholar]
- 5.Macpherson H, White AR, Cummings M, Jobst KA, Rose K, Niemtzow RC; STRICTA Group. Standards for Reporting Interventions in Controlled Trials of Acupuncture: The STRICTA recommendations. J Altern Complement Med. 2002;8(1):85–89 [DOI] [PubMed] [Google Scholar]
- 6.Langevin HM. Wayne PM, Macpherson H, et al. . Paradoxes in acupuncture research: Strategies for moving forward. Evid Based Complement Alternat Med. 2011;2011:180805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kluger BM, Rakowski D, Christian M, et al. . Randomized, controlled trial of acupuncture for fatigue in Parkinson's disease. Mov Disord. 2016;31(7):1027–1032 [DOI] [PubMed] [Google Scholar]
- 8.Goetz CG, Wuu J, McDermott MP, et al. ; Parkinson Study Group, Leurgans S. Placebo response in Parkinson's disease: Comparisions among 11 trials covering medical and surgical interventions. Mov Disord. 2008;23(5):690–699 [DOI] [PubMed] [Google Scholar]
- 9.Giles LGF, Muller R. Chronic spinal pain: A randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine. 2003;28(14):1490–1502 [DOI] [PubMed] [Google Scholar]
- 10.Hammerschlag R, Morris MM. Clinical trials comparing acupuncture with biomedical standard care: A criteria-based evaluation of research design and reporting. Complement Ther Med. 1997;5(3):133–140 [Google Scholar]
- 11.Yang DH, Chen H, Fang Z. Observations on the efficacy of acupuncture plus Western drug on rehabilitation treatment of Parkinson's disease. J Clin Acupunct Med. 2006;22(6):16–18 [Google Scholar]
- 12.Chen XH, Li Y, Kui Y. Clinical observation on abdominal acupuncture plus Madopa for treatment of Parkinson's disease [article in Chinese]. Zhongguo Zhen Jiu 2007;27(8):562–564 [PubMed] [Google Scholar]
- 13.Nesheim BI, Kinge R. Performance of acupuncture as labor analgesia in the clinical setting. Acta Obstet Gynecol Scand. 2006;85(4):441–443 [DOI] [PubMed] [Google Scholar]
- 14.Wang L, He C, Lui Y, Zhu L. Effect of acupuncture on the auditory evoked brain stem potential in Parkinson's disease. J Tradit Chin Med. 2002;22(1):15–17 [PubMed] [Google Scholar]
- 15.Xu B, Shen MH, Chen GZ. Effects of acupuncture and point-injection on central neuropeptide and nitric oxide in patients with primary Parkinson disease. Chin J Clin Rehabil. 2004;8(34):7858–7560 [Google Scholar]
- 16.Chae Y, Lee H, Kim H, Kim CH, Chang DI, Kim KM. Parsing brain activity associated with acupuncture treatment in Parkinson's diseases. Mov Disord. 2009;24(12):1794–1802 [DOI] [PubMed] [Google Scholar]
- 17.Berle CA, Cobbin D, Smith N, Zaslawski C. A novel approach to evaluate Traditional Chinese Medicine treatment outcomes using pattern identification. J Altern Complement Med. 2010;16(4):357–367 [DOI] [PubMed] [Google Scholar]
- 18.Shulman LM, Wen X, Weiner WJ, Bateman D, Minagar A, Duncan R, Konefal J. Acupuncture therapy for the symptoms of Parkinson's disease. Mov Disord. 2002;17(4):799–802 [DOI] [PubMed] [Google Scholar]
- 19.Stellon A. Neurogenic pruritus: An unrecognized problem? A retrospective case series of treatment by acupuncture. Acupunct Med. 2002;20(4):186–190 [DOI] [PubMed] [Google Scholar]
- 20.Abuaisha BB, Costanzi JB, Boulton AJ. Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy: A long-term study. Diabetes Res Clin Pract. 1998;39(2):115–121 [DOI] [PubMed] [Google Scholar]
- 21.Cherkin DC, Sherman KJ, Abins A, et al. . A randomized trial comparing acupuncture, stimulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169(9):858–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haake M, Muller HH, Schade-Brittinger C, Basler HD, Schäfer H, Maier C, et al. . German Acupuncture Trials (GERAC) for chronic low back pain: Randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167(17):1892–1898 [DOI] [PubMed] [Google Scholar]
- 23.Sackett DL, Rosenberg WM. The need for evidence-based medicine. J R Soc Med. 1995;88(11):620–624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moher D, Schulz KF, Altman DG; CONSORT. The CONSORT statement: Revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Methodol. 2001;1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: A clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55(3):181–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goetz C, Fahn S, Martinez-Martin P, et al. . Movement Disorder Society–sponsored revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS): Process, format, and clinimetric testing plan. Mov Disord. 2007;22(1):41–47 [DOI] [PubMed] [Google Scholar]
- 27.Dalrymple-Alford JC, MacAskill MR, Nakas CT, et al. . The MoCA: Well-suited screen for cognitive impairment in Parkinson disease. Neurology. 2010;75(19):1717–1725 [DOI] [PubMed] [Google Scholar]
- 28.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370 [DOI] [PubMed] [Google Scholar]
- 29.Dilli CR, Childs R, Berk J, Christian MK, Nguyen N, Brown RP, Kluger BM. Does prior acupuncture exposure affect perception of blinded real or sham acupuncture? Acupunct Med. 2014;32(2):155–159 [DOI] [PubMed] [Google Scholar]
- 30.Betts D, Budd S. “Forbidden points” in pregnancy: Historical wisdom? Acupunct Med. 2011;29(2):137–139 [DOI] [PubMed] [Google Scholar]
- 31.Thompson JW, Cummings M. Investigating the safety of electroacupuncture with a Picoscope. Acupunct Med. 2008;26(3):133–139 [DOI] [PubMed] [Google Scholar]
- 32.British Medical Acupuncture Society. Right of appeal. In: Code of Practice & Complaints Procedure. London: The Royal London Homeopathic Hospital; 2006:16 [Google Scholar]
- 33.Miller C, Hopperstad B, Johnson P, Dusek J. P02.51: Acupuncture treatment for hospitalized patients on anticoagulant therapy—a safety study. BMC Complement Altern Med. 2012;12(suppl1):10722827934 [Google Scholar]
- 34.Park J, Park H, Lee H, Lim S, Ahn K, Lee H. Deqi sensation between the acupuncture-experienced and the naïve: A Korean study II. Am J Chinese Med. 2005;33(2):329–337 [DOI] [PubMed] [Google Scholar]
- 35.Téllez N, Rio J, Tintoré M, Nos C, Galán I, Montalban X. Does the Modified Fatigue Impact Scale offer a more comprehensive assessment of fatigue in MS? Mult Scler J. 2005;11(2):198–202 [DOI] [PubMed] [Google Scholar]
- 36.Peto V, Jenkinson C, Fitzpatrick R, Greenhall R. The development and validation of a short measure of functioning and well being for individuals with Parkinson's disease. Qual Life Res. 1995;4(3):241–248 [DOI] [PubMed] [Google Scholar]
- 37.Chaudhuri KR, Pal S, DiMarco A, et al. . The Parkinson's disease sleep scale: A new instrument for assessing sleep and nocturnal disability in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2002;73(6):629–635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14(6):540–545 [DOI] [PubMed] [Google Scholar]
- 39.Starkstein SE, Mayberg HS, Preziosi TJ, Andrezejewski P, Leiguarda R, Robinson RG. Reliability, validity, and clinical correlates of apathy in Parkinson's disease. J Neuropsychiatry Clin Neurosci. 1992;4(2):134–139 [DOI] [PubMed] [Google Scholar]
- 40.Fahn S, Elton RL. Unified Parkinson's disease rating scale. In: Fahn S, Marsden CD, Caine DB, Goldstein M, eds. Recent Development in Parkinson's Disease. Florham Park, NJ: Macmillan Healthcare Information; 1987:153–163 [Google Scholar]
- 41.Guy W; National Institute of Mental Health (U.S.), Psychopharmocology Research Branch, Division of Extramural Research Programs. Clinical Global Impression (CGI). In: ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976:218–222 [Google Scholar]
- 42.Molassiotis A, Sylt P, Diggins H. The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: A randomised controlled trial. Complement Ther Med. 2007;15(4):228–237 [DOI] [PubMed] [Google Scholar]
- 43.Wang T, Zhang Q, Xue X, Yeung A. A systematic review of acupuncture and moxibustion treatment for chronic fatigue syndrome in China. Am J Chin Med. 2008;36(1):1–24 [DOI] [PubMed] [Google Scholar]
- 44.Lam YC, Kum WF, Durairajan SS, et al. . Efficacy and safety of acupuncture for idiopathic Parkinson's disease: A systemic review. J Altern Complement Med. 2008;14(6):663–671 [DOI] [PubMed] [Google Scholar]
- 45.Sherman KJ, Hogeboom CJ, Cherkin DC, Deyo RA. Description and validation of a noninvasive placebo acupuncture procedure. J Altern Complement Med. 2002;8(1):11–19 [DOI] [PubMed] [Google Scholar]
- 46.Ahn AC, Kaptchuk TJ. Advancing acupuncture research. Altern Ther Health Med. 2005;11(3):40–45 [PubMed] [Google Scholar]
- 47.NCCAOM.org National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) Fact Sheet: NCCAOM Certification and Testing Program. Online document at: www.nccaom.org/nccaom-certification-and-testing-program/ Accessed May25, 2016
- 48.Yin C, Seo B, Park HJ, et al. . Acupuncture, a promising adjunctive therapy for essential hypertension: A double-blind, randomized, controlled trial. Neurol Res. 2007;29(suppl1):S98–S103 [DOI] [PubMed] [Google Scholar]
- 49.Park YC, Chang DI, Lee YH, Park DS. The study on the effect of acupuncture treatment in patients with idiopathic Parkinson's disease. J Korean Acupunct Moxibust Soc. 2007;24(4):43–54 [Google Scholar]
- 50.Takakura N, Yajima H. A double-blind placebo needle for acupuncture research. BMC Complement Altern Med. 2007;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsukayama H, Yamashita H, Kimura T, Otsuki K. Factors that influence the applicability of sham needle in acupuncture trials- Two randomized, single-blind, crossover trials with acupuncture-experienced subjects. Clin J Pain. 2006;22(4):346–349 [DOI] [PubMed] [Google Scholar]
- 52.White AR, Filshie J, Cummings TM; International Aupuncture Research Forum. Clinical trials of acupuncture: Consensus recommendations for optimal treatment, sham controls and blinding. Complement Ther Med. 2001;9(4):237–245 [DOI] [PubMed] [Google Scholar]
- 53.White P, Lewith G, Hopwood V, Prescott P. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single-blind, cross-over, pilot trial. Pain. 2003;106(3):401–409 [DOI] [PubMed] [Google Scholar]
- 54.Birch S. Controlling for non-specific effects of acupuncture in clinical trials. Clin Acupunct Oriental Med. 2003;4(2–3):59–70 [Google Scholar]
- 55.Park JB, White A, Lee H, Yamashita H, Ernst E. Credibility of a newly developed sham needle. J Jpn Soc Acupunct Moxibust. 2000;50(1):111–114 [Google Scholar]
- 56.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;353(9125):364–365 [DOI] [PubMed] [Google Scholar]
- 57.Sherman KJ, Hogeboom CJ, Cherkin DC, Deyo RA. Description and validation of a noninvasive placebo acupuncture procedure. J Altern Complement Med. 2002;8(1):11–19 [DOI] [PubMed] [Google Scholar]
- 58.Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: Two randomised controlled trials. Acupunct Med. 2002;20(4):168–174 [DOI] [PubMed] [Google Scholar]
- 59.Birch S, Jamison RN. Controlled trial of Japanese acupuncture for chronic myofascial neck pain: Assessment of specific and nonspecific effects of treatment. Clin J Pain. 1998;14(3):248–255 [DOI] [PubMed] [Google Scholar]
- 60.Birch S. A review and analysis of placebo treatments, placebo effects, and placebo controls in trials of medical procedures when sham is not inert. J Altern Complement Med. 2006;12(3):303–310 [DOI] [PubMed] [Google Scholar]
- 61.Kos D, Duportail M, D'Hooghe M, Nagels G, Kerckhofs E. Multidisciplinary fatigue management programme in multiple sclerosis: A randomized clinical trial. Mult Scler. 2007;13(8):996–1003 [DOI] [PubMed] [Google Scholar]
- 62.Washburn AM, Fullilove RE, Fullilove MT, et al. . Acupuncture heroin detoxification: A single-blind clinical trial. J Subst Abuse Treat. 1993;10(4):345–351 [DOI] [PubMed] [Google Scholar]
- 63.White A, Hayhoe S, Hart A, Ernst E. Adverse effects following acupuncture: Prospective survey of 32,000 consultations with doctors and physiotherapists. BMJ. 2001;323(7311);485–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Birch S, Hesselink JK, Jonkman FA, Hekker TA, Bos A. Clinical research on acupuncture: Part 1. What have reviews of the efficacy and safety of acupuncture told us so far? J Altern Complement Med. 2004;10(3):468–480 [DOI] [PubMed] [Google Scholar]
- 65.Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ. 2005;330(7501):1202–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dhond R, Kettner N, Napadow V. Do the neural correlates of acupuncture and placebo effects differ? Pain. 2007;128(1–2):8–12 [DOI] [PMC free article] [PubMed] [Google Scholar]