Abstract
Introduction
Little is known about how alcohol treatment rates vary across age or years since onset of an alcohol use disorder (AUD). We examined past-year treatment prevalence and associations across these important time metrics.
Method
Data on 22,278 adults ages 18–50 were from the National Epidemiologic Survey on Alcohol and Related Conditions-III (2012–2013). We examined the age-varying prevalence of alcohol treatment and associations of past-year AUD severity, MDD status, and DUD status with treatment. Additionally, for individuals with a lifetime AUD (N=7,089), we examined associations of severity, MDD, and DUD across years since AUD onset.
Results
Individuals with Moderate/Severe past-year AUD had significantly higher treatment rates at nearly all ages, compared to those with Mild or no AUD. For those with Moderate/Severe AUD, treatment rates were highest during late adolescence and middle adulthood and lowest during early adulthood. Mental health comorbidities were positively associated with treatment at certain age ranges in mid-adulthood. Among individuals with a lifetime AUD, those with Moderate/Severe past-year AUD had significantly higher past-year treatment rates across all years since onset. MDD and DUD were both positively associated with treatment at nearly all years since AUD onset.
Conclusions
Alcohol treatment rates varied notably by age and, to a lesser extent, by years since AUD onset. Greater AUD severity was consistently associated with higher rates of treatment, whereas Mild AUD had a much weaker relationship. MDD and DUD showed similar patterns of positive association with treatment. Our results highlight important subgroups where unmet treatment needs are highest.
Keywords: alcohol, alcohol treatment, comorbidities, depression, substance use disorder
1. INTRODUCTION
Alcohol use disorders (AUDs) are common in the population. Despite effective treatment for alcohol problems (Dawson et al., 2012; Jonas et al., 2012), utilization rates are low, indicating a profound unmet treatment need (Edlund et al., 2012; Hasin et al., 2007). Less than 10% of individuals with an AUD received treatment in the past year (Substance Abuse and Mental Health Services Administration (SAMHSA), 2014), and the lifetime probability of treatment for individuals with alcohol dependence is 54% (Blanco et al., 2015).
Despite our understanding that alcohol treatment is often an ongoing, dynamic process that varies across age and disease progression (Hser et al., 2007), time-varying trends in alcohol treatment are poorly understood. In this study we focus on two time metrics that we hypothesize may predict treatment need and, correspondingly, treatment seeking: age and years since AUD onset.
Temporal variations in alcohol treatment may occur for a number of reasons. First, at a population level, alcohol use varies notably across different ages and life stages, with alcohol use being most common during adolescence and early adulthood and declining throughout mid- to late-adulthood (SAMHSA, 2014). Age-varying trends in alcohol use may contribute to age-varying trends in alcohol treatment. Second, age is often a marker of life stage, reflecting differences in career development, family status, and societal expectations. Individuals often perceive greater consequences of their drinking as their professional, family, and societal responsibilities change, which may result in greater likelihood of treatment seeking. Existing studies of treatment utilization by age have yielded equivocal findings. In a national sample, Cohen et al. (2007) found that older adults had a higher lifetime probability of alcohol treatment. In contrast, Wang et al (2005) found that, among individuals with an AUD, younger individuals had higher odds of past treatment than older individuals. Choi et al (2014) found that older individuals had the lowest prevalence of past-year alcohol treatment. Additionally, several studies have reported that older individuals have longer delays to first treatment episode (Chapman et al., 2015; Chi et al., 2014; Wang et al., 2005).
Treatment rates may vary across the course of an individual’s disorder due to differences in severity and in perceived need for treatment. Alcohol use severity is one of the strongest and most consistent predictors of alcohol treatment utilization (e.g., Evans-Polce et al., 2014; Finney and Moos, 1995; Oleski et al., 2010) with greater severity being associated with a higher likelihood of alcohol treatment utilization. Onset is a central event in the course of an AUD (Hser et al., 2007), and time since onset is strongly associated with first treatment utilization. Treatment prevalence in the first year since onset is quite low: five percent for individuals with alcohol dependence and one percent for those with alcohol abuse (Blanco et al., 2015). Studies have found that individuals with an alcohol disorder typically first receive treatment between six and 18 years after disorder onset (Bruffaerts et al., 2007; Kessler et al., 2001; Keyes et al., 2010; Wang et al., 2005, 2007). Years since onset is typically examined as a predictor of first treatment episode; however, past-year treatment utilization trends by years since onset remain poorly understood.
The presence of a comorbid mental health disorder, particularly a drug use disorder (DUD) or major depressive disorder (MDD), are also strongly associated with alcohol treatment utilization (Cohen et al., 2007; Grella et al., 2009; Mojtabai et al., 2002; Kaufman et al., 2014; Ilgen et al., 2011). Mental health comorbidity may increase alcohol treatment utilization by contributing to greater overall disease severity and impaired functioning (Burns et al., 2005; Clark et al., 2009; Landheim et al., 2006). Additionally, individuals with a comorbid mental health problem may be referred to alcohol treatment services through a mental health service provider (Schuler et al., 2015). Studies have shown that lifetime MDD and lifetime DUD are both associated with lifetime alcohol treatment (Cohen et al., 2007; Kaufman et al., 2014). Individuals with either comorbid MDD (Blanco et al., 2015) or DUD (Ilgen et al., 2011) are significantly more likely to initiate alcohol treatment than individuals without these factors. While both alcohol severity and comorbid mental health disorders are strongly related to alcohol treatment utilization, it is not known whether the magnitude of the associations vary across age or years since AUD onset.
In this study, we examine how past-year alcohol treatment rates vary both across age and years since AUD onset, using data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). These time metrics were selected to elucidate different processes related to treatment utilization: age was selected to examine processes across the life stage, while years since AUD onset was selected to examine processes across the course of the disorder. Additionally, we assess whether AUD severity or comorbidity with either MDD or a DUD varies in its association with treatment utilization with respect to either age or years since AUD onset. We implement time-varying effect modeling (TVEM) to examine past-year treatment rates across ages 18 to 50 and across 0 to 30 years since AUD onset. We specifically examine trends in past-year treatment, rather than lifetime utilization or first treatment episode, in recognition that alcohol treatment is often a recurring process. Understanding alcohol treatment trends across both age and years since AUD onset, as well as whether comorbidity status differentially impacts treatment utilization, will help to further characterize which individuals are receiving treatment as well as when treatment need remains unmet.
2. METHODS
2. 1 Study population and design
This study used data from NESARC-III, a nationally representative study of 36,309 non-institutionalized civilian adults using a multistage, stratified, probability-sampling method (Grant et al., 2014). Trained interviewers conducted face-to-face interviews in 2012–2013 with a screener- and person-level response rate of 72% and 84%, respectively. For analyses examining associations across age, our sample consisted of all individuals ages 18 to 50 (N=22,278). For analyses examining associations since lifetime AUD onset, our sample consisted of individuals with a lifetime AUD diagnosis, and was restricted to individuals who did not have missing data on years since AUD onset and for whom years since onset was less than or equal to 30 years (due to sparseness), resulting in a sample size of 7,089.
2.2 Measures
Age was assessed by self-report and was coded to the nearest year (M=34.0, SD=9.4). Alcohol use disorder was assessed by the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5), a structured diagnostic interview that provides DSM-5 diagnoses and can be administered by non-clinician interviewers (Grant et al., 2015). Per DSM-5 diagnostic categories, individuals were classified as no AUD if they endorsed 0–1 of the 11 DSM-5 criteria, Mild AUD if they endorsed 2–3, and Moderate/Severe if they endorsed 4 or greater. Age of AUD onset was assessed by the AUDADIS-5, and years since AUD onset was calculated as age at interview minus age at onset of an AUD (M=10.2, SD=9.3). Years since onset analyses were truncated at 30 years due to sparseness of responses past 30 years.
Individuals were classified as having received past-year alcohol treatment if they responded affirmatively to the question “Have you ever gone anywhere or seen anyone for a reason that was related in any way to your drinking - a physician, counselor, Alcoholics Anonymous, or any other community agency or professional?” and reported that the treatment was received in the past 12 months (N=548).
Past-year MDD and past-year DUD status were also assessed using the AUDADIS-5. Ten drug categories were combined to create a measure of any (non-alcohol) DUD versus none: amphetamine, opioid, sedatives, tranquilizers, cocaine, inhalants/solvents, hallucinogens, cannabis, heroin, and other. To determine DUD status, individuals were asked to report on use “either without a doctor’s prescription or in greater amounts, more often, or longer than prescribed, or for a reason other than the doctor said you should use them.” In our sample, 12.0% (N=2,680) of individuals met criteria for a MDD in the past year, and 5.4% (N=1,207) met criteria for a DUD in the past year.
We included a number of control variables in our analyses: sex, race/ethnicity (White non-Hispanic, Black non-Hispanic, Asian/Native Hawaiian/Other Pacific Islander non-Hispanic, American Indian/Alaska Native non-Hispanic, Hispanic), education (high school diploma or greater vs. less than high school diploma), and other past-year mental health disorder (including dysthymia, bipolar disorder, specific phobia disorder, social phobia disorder, panic disorder, agoraphobia, generalized anxiety disorder, post-traumatic stress disorder, anorexia, bulimia nervosa, and binge-eating disorder). See Table 1 for descriptive statistics of the sample.
Table 1.
Descriptive statistics for those ages 18 to 50 years (Unweighted)
| Characteristic | %/M(SD) |
|---|---|
| Past year alcohol treatment | 2.26% |
| Age | 34.00 (9.35) |
| Years since onset of AUD* | 10.17 (9.30) |
| Male | 43.95 |
| Race/ethnicity | |
| White, non-Hispanic | 45.72 |
| Black, non-Hispanic | 23.16 |
| AIAN, non-Hispanic | 1.4 |
| Asian, non-Hispanic | 5.57 |
| Hispanic | 24.15 |
| High School Diploma | 86.22 |
| Past-year AUD | |
| no AUD | 81.68 |
| Mild AUD | 9.28 |
| Moderate/Severe AUD | 9.04 |
| Past-year MDD | 12.03 |
| Past-year DUD | 5.42 |
| Past-year other mental health disorder | 18.79 |
subset of those with a history of AUD, 0–30 years since onset
2.3 Analysis
Analyses were conducted using TVEM, a type of non-parametric spline regression that estimates how regression coefficients vary with respect to time (Hastie and Tibshirani, 1993; Tan et al., 2012). Specifically, the time-varying model is , where Tij denotes past-year alcohol treatment status for individual i at time j and β0 t denotes the time-varying logistic regression coefficient that expresses the log odds of past-year alcohol treatment as a smooth non-parametric function of t, the time metric (e.g., age or years since onset).
Nationally representative rates of past-year treatment across age, stratified by AUD severity, were estimated in the full sample using TVEM intercept-only models. We then examined the age-varying associations of past-year AUD severity, MDD status, and DUD status with past-year alcohol treatment. These models allowed us to assess if the salience of AUD severity or comorbidity status for predicting alcohol treatment varied across age. Each model controlled for sex, race/ethnicity, education, other mental health disorders, as well as the other two severity and comorbidity factors (i.e., AUD severity, MDD status, and DUD status) as time-invariant covariates. All models included NESARC-III sampling weights.
Similarly, we implemented TVEM in the subgroup of individuals with a lifetime AUD diagnosis to examine time-varying associations of past-year treatment use across years since onset. Again, we examined the rates of treatment across years since onset and time-varying associations of past-year AUD severity, MDD, and DUD status with past-year alcohol treatment use across years since onset. All models controlled for sex, race/ethnicity, education, other mental health disorder, age, and the other two AUD severity or comorbidity factors as time-invariant covariates; these analyses were unweighted.
For all analyses, we present the estimated functions of treatment prevalence or time-varying log odds regression coefficients, along with the corresponding 95% confidence interval, graphically. All models were implemented in SAS 9.3 using the %TVEM_logistic macro (TVEM Macro Suite, 2015; Li et al., 2015). An unpenalized B-spline option was used for weighted models, using information criteria to select the optimal model, and penalized spline smoothing (p-spline option) was used for unweighted models.
3. RESULTS
3.1 Time-varying associations across age
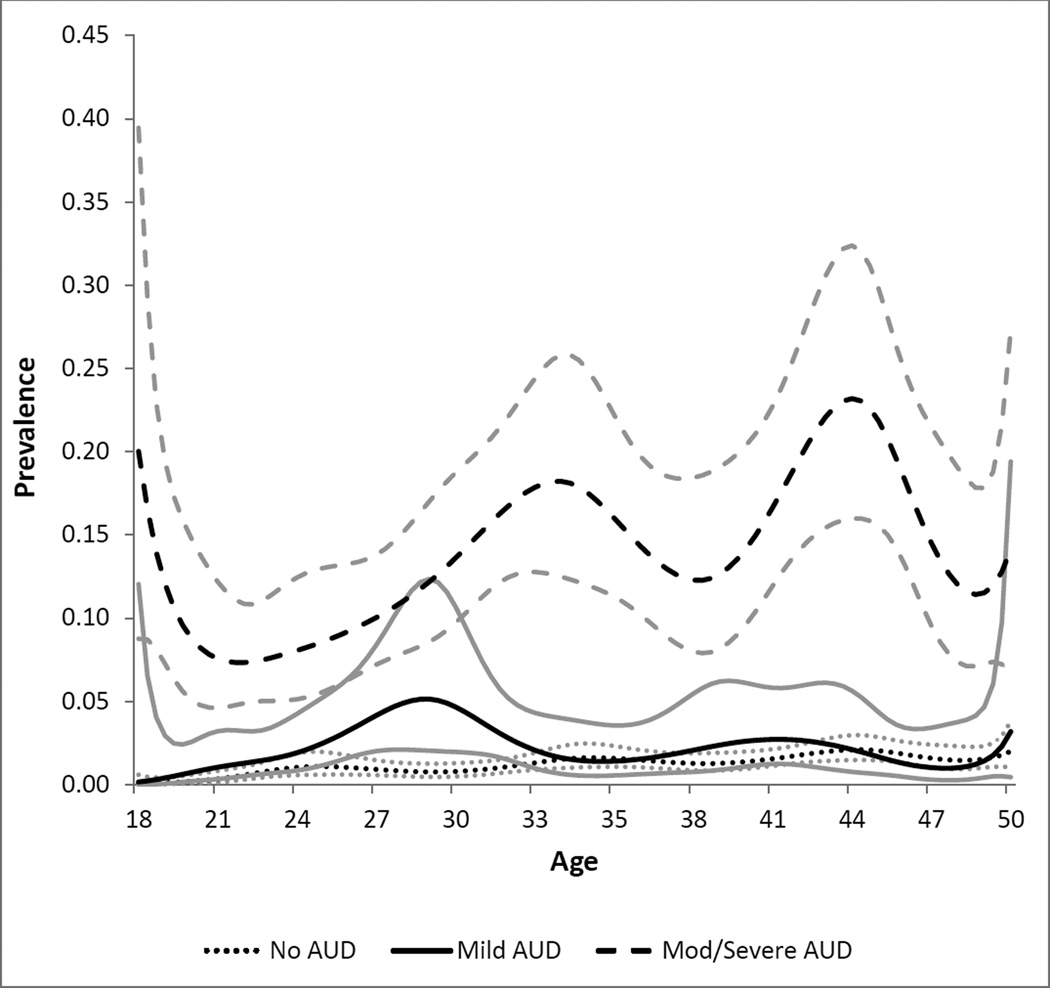
Among a nationally representative sample of US adults, 2.5% reported receiving alcohol treatment in the past year. Figure 1 shows past-year treatment prevalence by age, stratified by past-year AUD severity (none, Mild, or Moderate/Severe). Treatment utilization trends across age differed notably by AUD severity. For nearly all ages, individuals with Moderate/Severe AUD had significantly higher treatment rates. Among those with Moderate/Severe AUD, treatment utilization varied across age, with the highest utilization occurring at age 18 (20% treatment rate), at age 33 (18%), and at age 44 (23%). For these individuals, treatment rates were lowest in the early and mid-20s, and were increasing, although variable, throughout the 30s and 40s. Individuals with Mild AUD had quite low utilization across ages 18–50, with treatment rates peaking at age 29 (5% rate). Likewise, individuals with no AUD disorder also had very low treatment rates – utilization never exceeded 3%. Notably, treatment utilization rates between the No and Mild AUD rates did not statistically differ at most ages, with the exception of ages 26–31, during which Mild AUD rates were significantly higher than no AUD rates.
Figure 1.
Alcohol Treatment Prevalence by Alcohol Severity across Ages 18 to 50.
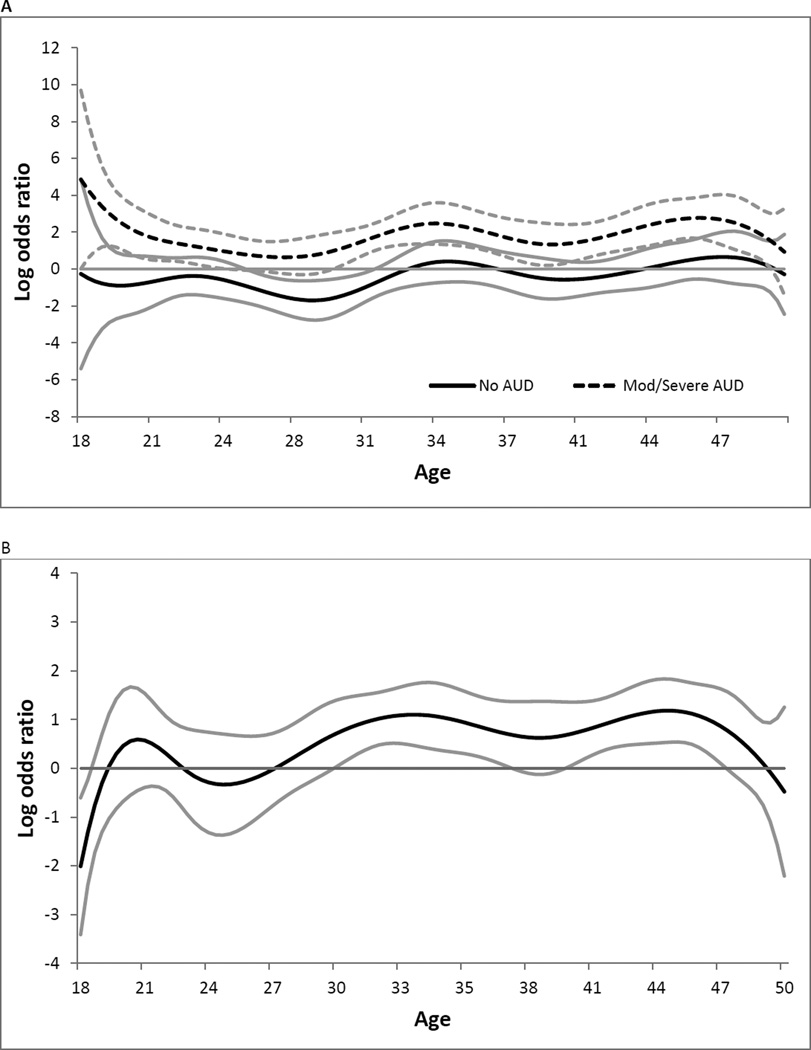
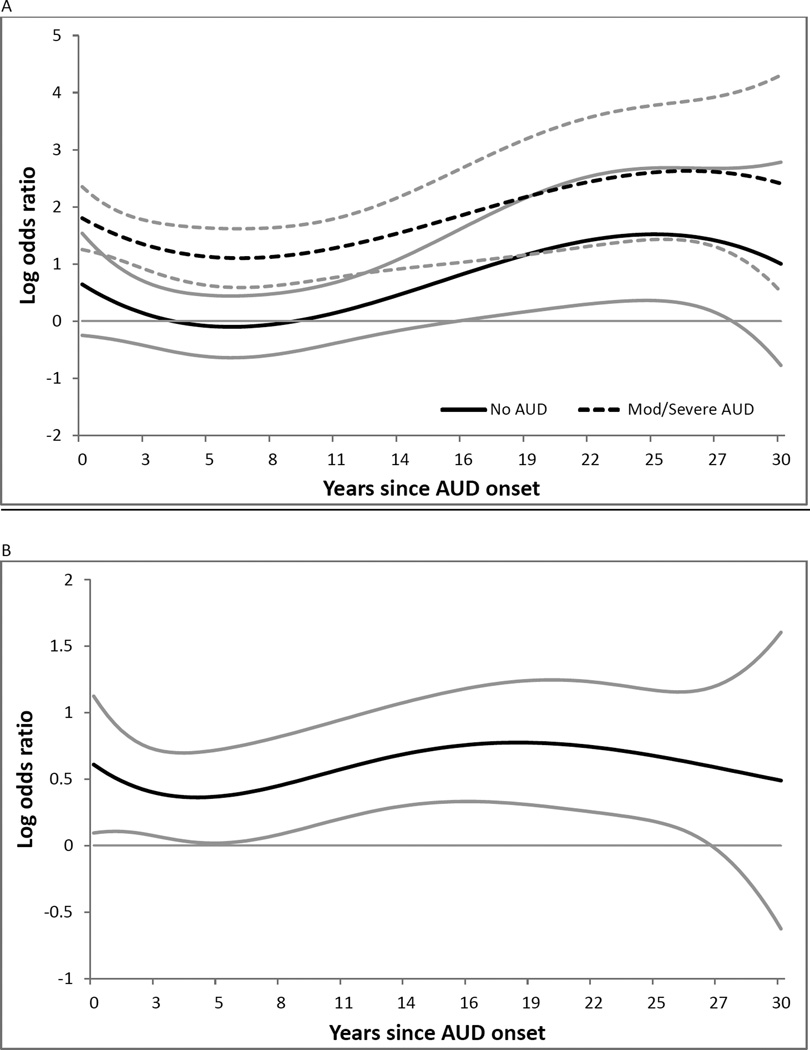
Figure 2 shows the age-varying associations of AUD severity (Panel A), MDD status (Panel B), and DUD status (Panel C) with treatment utilization, while adjusting for potential confounders. Panel A presents the age-varying regression coefficient (as the log odds) for the association between AUD severity status and past-year treatment. In contrast to Figure 1, Figure 2 Panel A presents age-varying associations adjusted for potential confounders. Relative to those with Mild AUD, individuals with Moderate/Severe AUD had significantly higher odds of past-year treatment at all ages except ages 25–30. The magnitude of this association varied across age, and was weakest in the early 20s (age 21 OR = 6.3), and peaked in the mid-30s (age 34 OR = 11.9) and mid-40s (age 46 OR = 16). We observe no significant difference in treatment rates between those with no AUD and Mild AUD after covariate adjustment, except during ages 26–31. Treatment utilization for those with Mild AUD was highest at age 29, yielding an OR=5.5 relative to those with no AUD. Overall, the adjusted associations in Panel A show very similar trends to the unadjusted prevalence differences in Figure 1, indicating that demographics and comorbid conditions were not strongly confounding the age-varying relationship between treatment utilization and severity.
Figure 2.
Panel A. Age-varying association between past-year AUD severity and past-year treatment, adjusted for sex, race/ethnicity, education, past-year MDD, past-year DUD, other past-year mental health disorder.
Panel B. Age-varying association between past-year MDD status and past-year treatment, adjusted for sex, race/ethnicity, education, AUD severity, past-year DUD, other past-year mental health disorder
Panel C. Age-varying association between past-year DUD status and past-year treatment, adjusted for sex, race/ethnicity, education, AUD severity, past-year MDD, other past-year mental health disorder.
Figure 2 Panel B presents the age-varying association of past-year MDD status with treatment. MDD status was significantly associated with higher odds of treatment during most of mid-adulthood (ages 30–37 and ages 40–47). The magnitude of this association was strongest at age 33 (OR=3.0) and age 44 (OR=3.3). Conversely, MDD was not associated with higher treatment utilization prior to age 30, and was negatively associated with treatment at age 18 (OR=0.13). Figure 2 Panel C shows the age-varying associations of past-year DUD status with treatment. DUD status was positively associated with treatment utilization at ages 18–20, ages 27–36, and ages 46–48. This magnitude of this association was strongest at age 18 (OR=5.8) and weaker in mid-adulthood (age 32 OR=3.8; age 47 OR=2.8). While MDD and DUD exhibited opposite relationships with treatment at ages 18–20, they exhibited generally similar associations with treatment across ages 20–50.
3.2 Time-varying associations across years since AUD onset
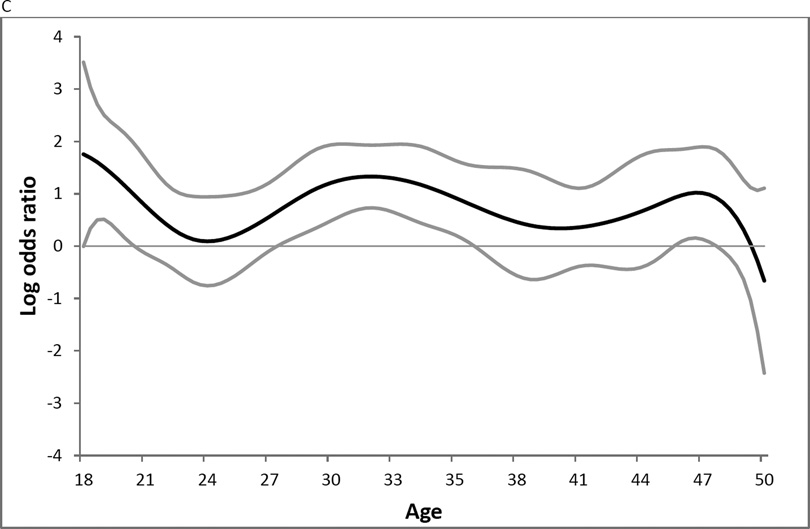
Figure 3 presents past-year treatment rates across years since AUD onset, stratified by past-year AUD severity. These analyses are limited to those with lifetime history of an AUD, but who may or may not report a past-year AUD. In general, treatment rates were somewhat less variable by years since onset than by age. For those with Moderate/Severe AUD, approximately 9% of individuals who were within the first year since onset obtained treatment; utilization increased until approximately eight years after onset (rate=17%). Treatment prevalence remained relatively constant at around 20% until 25 years after diagnosis, when utilization rates increased. Treatment rates for individuals with Mild AUD were much lower – only 1.5% of individuals utilized treatment within the first year of diagnosis. Similarly, rates gradually increased across the first eight years since diagnosis, peaking at 5% utilization, and then treatment rates declined steadily after eight years. Treatment rates for individuals with no AUD were also low and did not statistically differ from the treatment utilization for those with Mild AUD.
Figure 3.
Alcohol Treatment Prevalence by Alcohol Disorder Severity across Years since AUD Onset.
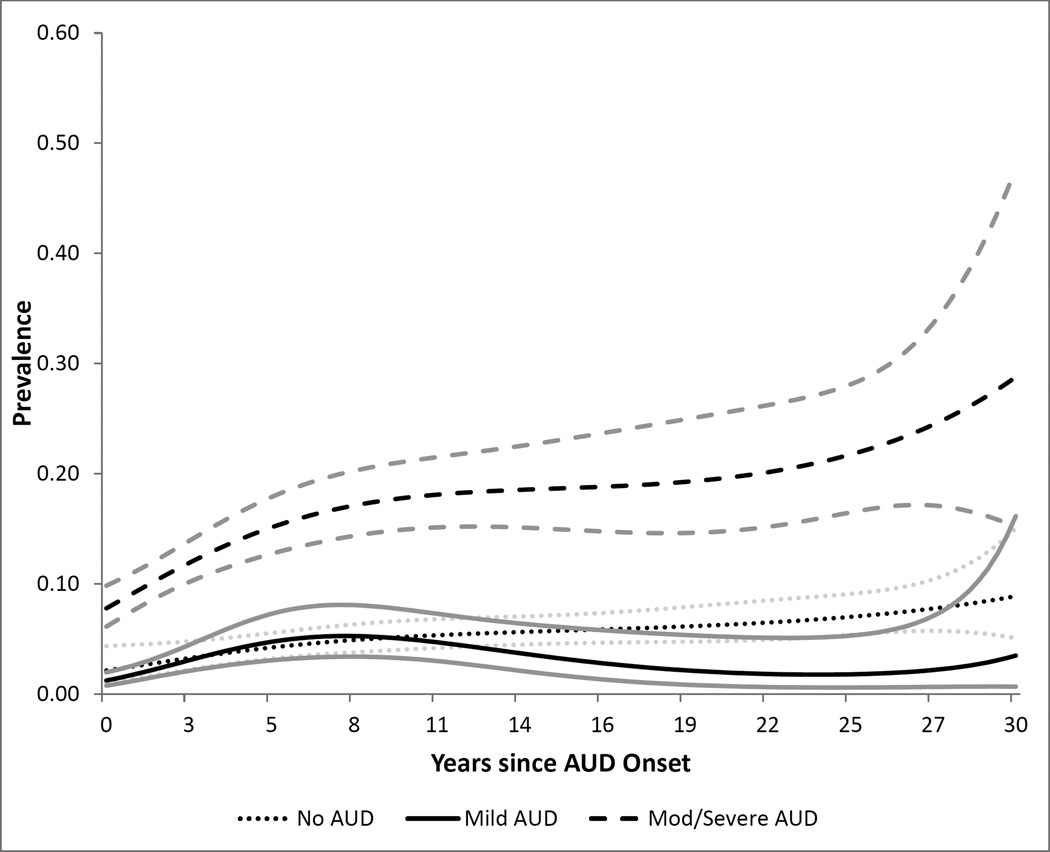
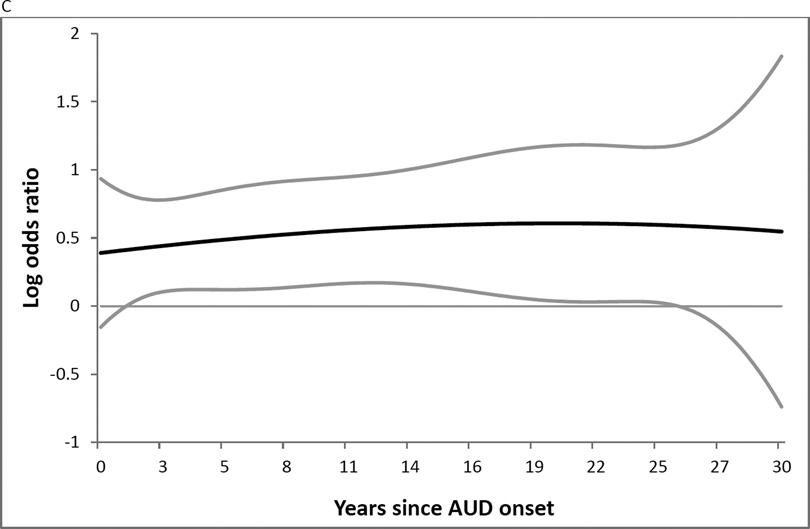
Figure 4 shows the time-varying associations of treatment utilization with AUD severity (Panel A), MDD status (Panel B), and DUD status (Panel C), while adjusting for potential confounders and age. Panel A presents the time-varying regression coefficient (as log odds) for the association between AUD severity and past-year treatment. Moderate/Severe AUD was consistently associated with greater odds of treatment compared to Mild AUD; the strength of this association was stronger in later years since AUD onset (OR=3.1 at 5 years, OR=9.7 at 20 years). In contrast, those with no AUD did not have significantly different odds of treatment compared to those with Mild AUD during the first 16 years since onset. Furthermore, during 17 to 28 years since onset, those with Mild AUD had lower odds of treatment than those with no AUD (OR=0.29 at 20 years).
Figure 4.
Panel A. Time-varying association between past-year AUD severity and past-year treatment, adjusted for sex, race/ethnicity, education, past-year MDD, past-year DUD, other past-year mental health disorder, age.
Panel B. Time-varying association between past-year MDD status and past-year treatment, adjusted for sex, race/ethnicity, education, AUD severity, past-year DUD, other past-year mental health disorder, age.
Panel C. Time-varying association between past-year DUD status and past-year treatment, adjusted for sex, race/ethnicity, education, AUD severity, past-year MDD, other past-year mental health disorder, age.
Figure 4 Panel B shows the time-varying association of past-year MDD status with treatment. For the majority of time, past-year MDD was associated with greater odds of treatment compared to those without MDD. The magnitude of this association ranges from OR=1.4 at 5 years after onset to OR=2.2, which occurred at 19 years after onset. Similarly, when examining the time-varying association of past-year DUD status with alcohol treatment (Figure 4 Panel C), DUD was generally associated with greater odds of treatment. The magnitude of this association ranged from OR=1.5 to OR=1.8. This association was nonsignificant both during the first year since onset and after 26 years since onset. In general, both MDD and DUD exhibit similar positive time-varying associations with treatment utilization.
4. DISCUSSION
While alcohol treatment is often an ongoing, dynamic process that varies across age and disease progression (Hser et al., 2007), time-varying trends in alcohol treatment remain poorly understood. In this study, we examined variation in past-year alcohol treatment rates with respect to two particularly salient time metrics: age and years since AUD onset. Our results highlight that alcohol treatment rates varied by both time metrics. Additionally, we found time-varying associations with treatment for AUD severity and MDD and DUD comorbidity status.
Age trends in treatment utilization showed notable variation across AUD severity status. Among those with Moderate/Severe AUD, treatment peaked in late adolescence, in the mid-30s, and in the mid-40s. However, those with Mild AUD had the highest treatment rates in the late-20s, suggesting that factors related to treatment utilization may differ by AUD severity status. While trends in past-year treatment and first treatment utilization are not directly comparable, this heterogeneity across age by AUD severity may shed light on previous findings that the average age of first alcohol treatment is in the early 30s (Hasin et al., 2007; SAMHSA, 2014). This average age may reflect the composite of separate and distinct surges in treatment seeking among those with Mild AUD and those with Moderate/Severe AUD.
The multiple peaks in utilization in late adolescence and mid-adulthood among those with Moderate/Severe AUD may reflect different paths to treatment across the life course. The peak around age 18 may reflect the influence of parents/guardians, schools, or the juvenile justice system on young adults (Caldeira et al., 2009; Winders and Stinchfield, 1995). Increasing rates of treatment in the mid-40s may reflect increasing pressures from one’s spouse or children and an increased perceived need for treatment due to an accruement or intensification of family, work, or financial difficulties (Cohen et al., 2007). Importantly, among this most severe AUD group with arguably the highest need for treatment, treatment rates were low throughout the 20s. At these ages, external pressure from parents, spouses, or children may be absent, contributing to the lower rates of treatment. Additionally, heavy and disordered alcohol use is more prevalent and normative in the mid-20s compared to mid-adulthood (SAMHSA, 2014); thus individuals may not experience as many negative consequences of drinking or perceive a need for treatment at this age. Yet, even at ages in which treatment was most prevalent, it did not exceed 25% in the Moderate/Severe AUD group. These results are consistent with previous research showing that approximately 8% of individuals with a past-year AUD receive treatment, and only 11% of treatment-naïve individuals with an AUD perceive a need for treatment (SAMHSA, 2014; Schuler et al., 2015). Perceived barriers to treatment, including stigma and attitudinal barriers, and lack of access to treatment contribute to low treatment rates (Kaufman et al., 2014; Motjabai and Crum 2013; Schuler et al., 2015). Given these age-varying patterns, access to and perceived barriers to treatment may substantially differ by AUD severity and age.
We found that treatment rates were very low among those with no past-year AUD and those with Mild AUD, and were not significantly different at most ages and years since AUD onset. Specifically, treatment utilization for those with Mild AUD never exceeds 5% across ages 18–50. While low past-year treatment rates would be expected for those with no past-year AUD, the low rates for those with Mild AUD suggest a notable unmet treatment need.
When examining trends with respect to years since onset, we controlled for age as age may confound the association of years since onset and treatment. After controlling for age, treatment trends showed less variability with respect to years since AUD onset. Our observed treatment rates by years since AUD onset were consistent with recent work finding that treatment rates among those in the first year after onset are low (less than 5%; Blanco et al., 2015; Chapman et al., 2015). Individuals with Mild AUD and Moderate/Severe AUD both showed a steady increase in treatment prevalence and a peak around 8–10 years after onset; this is consistent with previous research that found the average treatment delay of approximately eight years from AUD onset (Hasin et al., 2007). While past-year treatment utilization includes both first-time use and ongoing use, the peak around 8–10 years could represent an increased number of first-time treatment seekers at this time point. Additionally, treatment utilization remained relatively constant for those with Moderate/Severe AUD from 10–25 years after onset. This stability may represent long-term AA or 12-step utilization, although retention rates in these programs tend to be low (Tonigan et al., 2003). Finally, while treatment rates increase after the first year since onset, even in the most severe AUD group treatment rates did not exceed 30% across 30 years since onset, again highlighting unmet treatment need.
Additionally, consistent with previous literature, we found that those who had a comorbid mental health disorder (DUD or MDD) were more likely to obtain alcohol treatment. The salience of comorbidity status only held for certain ages but was consistently and positively associated with treatment across nearly all years since onset. In general, comorbid MDD and DUD may be associated with greater alcohol treatment utilization because the comorbid condition exacerbates the severity of the alcohol disorder, creating greater treatment need. Additionally, individuals with a comorbid condition may be referred to alcohol treatment when receiving treatment for MDD or DUD. MDD status and DUD status were particularly important predictors of treatment during the mid-30s. This is the peak age range when individuals receive treatment for both MDD and DUD (Kessler et al., 2005), suggesting that individuals may be more likely to be referred to alcohol treatment through treatment encounters for other comorbid disorders.
While this study highlights important time-varying trends in alcohol treatment, there are some limitations to note. First, measures of alcohol and mental health disorder status as well as age of AUD onset are self-reported, and thus may be subject to misclassification due to recall bias or social desirability bias. However, the NESARC implemented private, computer-based assessment to improve data accuracy. Additionally, the use of past-year, rather than lifetime, indicators of treatment and comorbidity status reduces the likelihood of recall bias. Second, it was beyond the scope of this study to examine other factors including individual’s health insurance benefits, accessibility/affordability of treatment services, local/state/federal policies that may shape treatment seeking behavior. Future research in this area should consider these factors and how their effect on treatment may vary with age and years since AUD onset.
This study demonstrated that alcohol treatment utilization varied as a function of both age and years since AUD onset. Moderate/Severe AUD was consistently strongly associated with treatment utilization, whereas Mild AUD showed a much weaker association. Furthermore, comorbid MDD and DUD status showed a positive association with treatment across nearly all years since onset and during most of mid-adulthood. Our results indicate that individuals in their mid-20s and the first couple years since AUD onset have particularly low treatment rates, and may represent unmet treatment need. Focusing on this population for Screening, Brief Intervention, and Referral to Treatment (SBIRT) interventions in healthcare setting and increasing screening and alcohol treatment options on college campuses may help to increase treatment-seeking in this population. Additionally, the low treatment rates among those with Mild AUD should be explored further to understand perceptions of treatment need and barriers to treatment among this group.
Highlights.
Alcohol treatment rates varied across age and less so by years since onset
Treatment rates were lowest in the mid-20s and in the first year since AUD onset
Those with no AUD and Mild AUD showed few differences in treatment rates
We found age-varying differences in treatment rates by comorbidity status
Mental health comorbidities were associated with higher odds of treatment
Acknowledgments
We wish to thank Amanda Applegate for her help with final formatting and editing of the manuscript. This work was funded by awards P50DA010075, P50 DA039838, and T32DA017629 from the National Institute on Drug Abuse. This manuscript was prepared using a limited access data set obtained from the National Institute on Alcoholism and Alcohol Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA, NIDA or the NIH.
Role of funding source
Funding for this study was provided by P50DA010075, P50 DA039838, and T32DA017629 from the National Institute on Drug Abuse. This manuscript was prepared using a limited access data set obtained from the National Institute on Alcoholism and Alcohol Abuse. These organizations had no further role in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Dr. Evans-Polce helped formulate the research question, conducted the statistical analyses, and wrote and edited significant portions of the manuscript. Dr. Schuler helped formulate the research question, and drafted and edited significant portions of the manuscript. All authors have read and approved the final version of the manuscript.
Conflict of Interest.
No conflict declared.
All coauthors have no conflicts of interest to report.
REFERENCES
- American Psychiatric Association. Diagnostic And Statistical Manual Of Mental Disorders: DSM-IV. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Blanco C, Iza M, Rodríguez-Fernández JM, Baca-Garcia E, Wang S, Olfson M. Probability and predictors of treatment-seeking for substance use disorders in the U.S. Drug Alcohol Depend. 2015;149:136–144. doi: 10.1016/j.drugalcdep.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruffaerts R, Bonnewyn A, Demyttenaere K. Delays in seeking treatment for mental disorders in the Belgian general population. Soc. Psychiatry Psychiatr. Epidemiol. 2007;42:937–944. doi: 10.1007/s00127-007-0239-3. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M, O'Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100:787–796. doi: 10.1111/j.1360-0443.2005.001069.x. [DOI] [PubMed] [Google Scholar]
- Caldeira KM, Kasperski SJ, Sharma E, Vincent KB, O'Grady KE, Wish ED, Arria AM. College students rarely seek help despite serious substance use problems. J. Subst. Abuse Treat. 2009;37:368–378. doi: 10.1016/j.jsat.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman C, Slade T, Hunt C, Teesson M. Delay to first treatment contact for alcohol use disorder. Drug Alcohol Depend. 2015;147:116–121. doi: 10.1016/j.drugalcdep.2014.11.029. [DOI] [PubMed] [Google Scholar]
- Chi FW, Weisner C, Grella CE, Hser Y, Moore C, Mertens J. Does age at first treatment episode make a difference in outcomes over 11 years? J. Subst. Abuse Treat. 2014;46:482–490. doi: 10.1016/j.jsat.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM, Marti CN. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug Alcohol Depend. 2014;145:113–120. doi: 10.1016/j.drugalcdep.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Clark RE, Samnaliev M, McGovern MP. Impact of substance disorders on medical expenditures for Medicaid beneficiaries with behavioral health disorders. Psychiatric Serv. 2009;60:35–42. doi: 10.1176/ps.2009.60.1.35. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Factors associated with first utilization of different types of care for alcohol problems. J. Stud. Alcohol. 2012;73:647–656. doi: 10.15288/jsad.2012.73.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J. Stud. Alcohol Drugs. 2012;73:635–646. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce RJ, Doherty EE, Ensminger ME. Taking a life course approach to studying substance use treatment among a community cohort of African American substance users. Drug Alcohol Depend. 2014;142:216–223. doi: 10.1016/j.drugalcdep.2014.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney JW, Moos RH. Entering treatment for alcohol abuse: a stress and coping model. Addiction. 1995;90:1223–1240. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, Pickering RP, Ruan WJ, Huang B, Saha TD, Aivadyan C, Greenstein E, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend. 2015;148:27–33. doi: 10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, Goldstein R. Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC III) Rockville, MD: National Institute on alcohol Abuse and Alcoholism; 2014. [Google Scholar]
- Grella CE, Karno MP, Warda US, Moore AA, Niv N. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatric Serv. 2009;60:1068–1074. doi: 10.1176/appi.ps.60.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Arch. Gen. Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hastie T, Tibshirani R. Varying-coefficient models. J. R. Stat. Soc. Series B Stat. Methodol. 1993;55:757–779. [Google Scholar]
- Tan X, Shiyko MP, Li R, Li Y, Dierker L. A time-varying effect model for intensive longitudinal data. Psychol. Methods. 2012;17:61–77. doi: 10.1037/a0025814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Longshore D, Anglin MD. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval. Rev. 2007;31:515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Price AM, Burnett-Zeigler I, Perron B, Islam B, Zivin K. Longitudinal predictors of addictions treatment utilization in treatment naive adults with alcohol use disorders. Drug Alcohol Depend. 2011;113:215–221. doi: 10.1016/j.drugalcdep.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Viera AJ, Wilkins TM, Schwartz CJ, Richmond EM, Yeatts J, Swinson Evans T, Wood SD, Harris RP. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2012;157:645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaufman CN, Chen LY, Crum RM, Mojtabai R. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:1489–1499. doi: 10.1007/s00127-013-0740-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Berglund PA, Caraveo-Anduaga JJ, DeWit DJ, Greenfield SF, Vega WA. Patterns and predictors of treatment seeking after onset of a substance use disorder. Arch. Gen. Psychiatry. 2001;58:1065–1071. doi: 10.1001/archpsyc.58.11.1065. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Blanco C, Hasin DS. Telescoping and gender differences in alcohol dependence: new evidence from two national surveys. Am. J. Psychiatry. 2010;167:969–976. doi: 10.1176/appi.ajp.2009.09081161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landheim AS, Bakken K, Vaglum P. Impact of comorbid psychiatric disorders on the outcome of substance abusers: a six year prospective follow-up in two Norwegian counties. BMC Psychiatry. 2006;6:44. doi: 10.1186/1471-244X-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R, Dziak JD, Tan X, Huang L, Wagner AT, Yang J. TVEM (time-varying effect model) SAS macro users’ guide (Version 3.1.0) University Park, PA: 2015. Retrieved from http://methodology.psu.edu. [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch. Gen. Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: results from a longitudinal study. Drug Alcohol Depend. 2013;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleski J, Mota N, Cox BJ, Sareen J. Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatr. Serv. 2010;61:1223–1231. doi: 10.1176/ps.2010.61.12.1223. [DOI] [PubMed] [Google Scholar]
- Schuler MS, Puttaiah S, Motjabai R, Crum R. Barriers to accessing treatment for alcohol problems: a latent class analysis. Psychiatr. Serv. 2015;66:1221–1228. doi: 10.1176/appi.ps.201400160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: 2014. Results from the 2013 National Survey On Drug Use And Health: Summary Of National Findings. NSDUH series H-48 (HHS Publication no SMA 14-4863) [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Participation and involvement in Alcoholics Anonymous. In: Babor TF, Del Boca FK, editors. Matching Alcoholism Treatments To Client Heterogeneity: The Results of Project MATCH. New York: Cambridge University Press; 2003. [Google Scholar]
- TVEM SAS Macro Suite (Version 3.1.0) [Software] Penn State, University Park: The Methodology Center; 2015. Retrieved from https://methodology.psu.edu. [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wang PS, Angermeyer M, Borges G, Bruffaerts R, TatChiu W, Girolamo G, Fayyad J, Gureje O, Haro JM, Huang Y, Kessler RC, Kovess V, Levinson D, Nakane Y, Oakley Broan MA, Ormel JH, Posada-Villa J, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell BE, Chatterji S, Ustun TB. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:177–185. [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD. Current Issues And Future Needs In The Assessment Of Adolescent Drug Abuse (No. 156) Rockville, MD: NIDA Research Monograph; 1995. [PubMed] [Google Scholar]