Abstract
Background
A 28-y-old athletic woman was diagnosed with vulvodynia and long-term irritable bowel syndrome (IBS) and was treated successfully with an elimination diet.
Case/Intervention
In the course of 6 mo of nutrition therapy utilizing an elimination diet, specific foods triggering abdominal bloating and pain, and vulvovaginal pain were identified. In the course of treatment, the nutrition and supplement program instituted for this patient allowed her to return to her prior functional level without pain (including sexual activity) and resolution of her IBS. She has remained symptom free for at least 6 mo posttreatment.
Conclusion
This case demonstrates the potential usefulness of incorporating a customized nutritional approach to determine proinflammatory foods in patients with chronic vulvodynia and overlapping IBS. Long-term pain resolution and healthy sexual functioning in this case was supported by food elimination and nutritional supplementation.
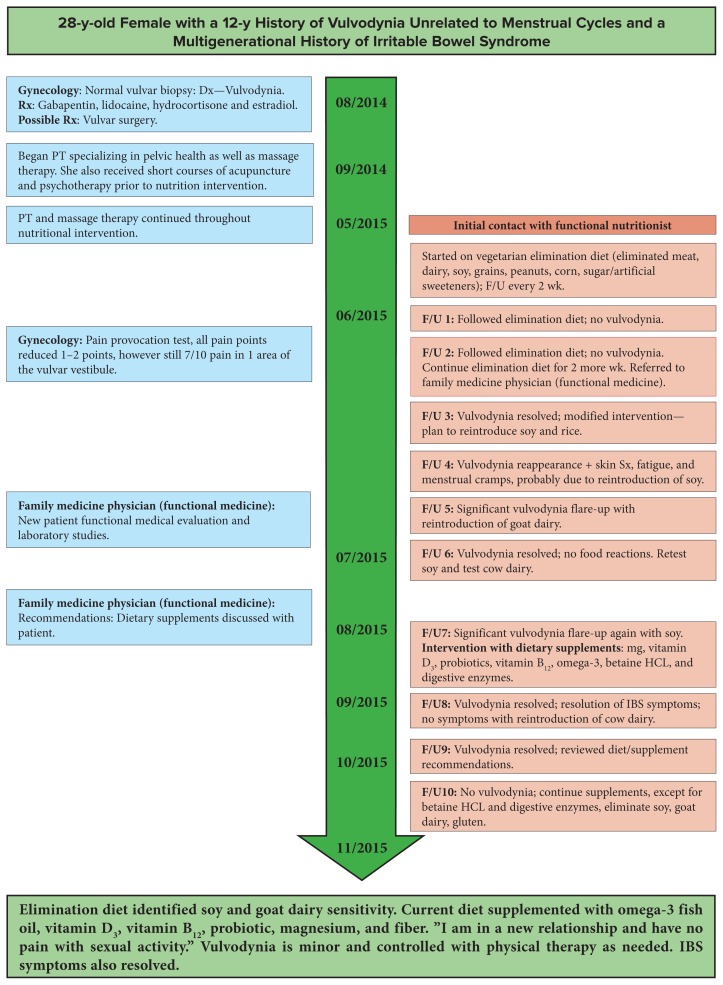
Vulvodynia is chronic pain of the vulva (external female genitalia) in the absence of localized infection. It is often associated with irritable bowel syndrome (IBS).1,2,3 This case report describes the use of a customized elimination diet and nutritional supplements that resolved her recurrent vulvodynia and multigenerational IBS—present since at least adolescence. She combined physical therapy, psychotherapy, and functional medicine including comprehensive laboratory testing with a nutritional intervention. See Figure 1.
Figure 1.
Patient Timeline
Abbreviations: IBS, irritable bowel syndrome; PT, physical therapy; F/U, follow-up, HCL, hydrochloric acid.
Patient Narrative
This patient reported vulvovaginal pain dating back to when she began menstruating and using tampons. Initially the pain was ignored. In the subsequent decade, she noticed an itching and a burning pain slightly inside of the vaginal canal that would come and go several times per year. At age 21 years, she became sexually active and experienced increasingly painful intercourse, which was eventually present with every sexual encounter.
In the summer of 2014, a gynecologist obtained a vaginal biopsy, diagnosed vulvodynia, and suggested that the local removal of the vaginal mucosa was one potential treatment for vulvodynia. Her gynecologist prescribed 4 medications: gabapentin and lidocaine ointment nightly, and hydrocortisone and estradiol suppositories alternating nightly. These medications were discontinued by the patient in June 2015.
In September 2014, she began physical therapy with a physical therapist specializing in disorders of the pelvic floor including vulvodynia. In addition to vulvodynia, this patient had a multigenerational history of IBS—her mother and her grandmother had gastrointestinal (GI) symptoms for “as long as she or they can remember.” This physical therapist referred her to a nutritional specialist in May 2015.
The nutritionist recommended an individualized, vegetarian elimination diet to this patient (who had been a vegetarian since age 12 y) to assess potential connections between food sensitivities and her vulvodynia. Her diet eliminated meat, fish, dairy, soy, all grains (except quinoa), peanuts, corn, sugar, and artificial sweeteners. She also eliminated caffeine and limited alcohol to 1 drink per day or less with food. She continued to eat eggs and legumes (except for peanuts). Patient was instructed to not limit calories and to eat when she felt hungry. A copy of the patient’s nutritional plan can be viewed in Table 1.
Table 1.
Patient Nutritional Plan—Elimination Diet
| Foods to Avoid | Breakfast Sample Recipes | Lunch and Dinner Sample Recipes | Snacks |
|---|---|---|---|
| Dairy | Coconut Yogurt Bowl: Combine coconut yogurt with any combination of nuts (walnuts, pecans, almonds, cashews, etc—may be toasted for flavor), seeds (pumpkin seeds, hemp seeds, chia seeds, flax seeds, sesame seeds, etc), fruit (berries, chopped green apple or chopped pear, chopped stone fruit such as peaches, plums, or apricots), and/or toasted coconut. Yogurt recommendations: coconut yogurt, or cashew yogurt, or buy it |
|
|
| Soy |
Smoothie: Combine:
|
|
— |
| Grains (except quinoa) | Breakfast hash (can serve over quinoa, but avoid other grains for now) |
|
— |
| Corn | — |
|
— |
| Peanuts | — |
|
— |
| Sugar | — |
|
— |
| Artificial Sweeteners | — |
|
— |
Patient maintained the elimination diet consistently for 7 days, after which time she reported resolution of her pelvic pain. She lost 1.36 kg during the first week of her elimination diet and reported that she was hungry all of the time with multiple food cravings. Prior to her second nutrition follow-up visit, her gynecologist did a pain provocation test and noted improvement of 1 to 2 points in all areas that were tested.
She returned for her second nutrition follow-up visit and reported craving rice and corn, but she continued adherence to her elimination diet. She agreed to reintroduce and test her reaction to soy beginning on June 16 and then rice the following week. At this visit, the nutritionist referred her to a family medicine physician specializing in functional medicine for additional evaluation.
When the patient returned for her third nutrition follow up, she reintroduced soy to have an additional protein source. Soy reintroduction caused significant symptoms including a skin rash, fatigue through the day, and painful menstrual cramps unrelieved by medication. The patient denied symptoms related to reintroducing rice and reported that she had lost a total of 2.27 kg since beginning the elimination diet.
Corn reintroduction provoked no symptoms; however, the reintroduction of goat cheese caused increased gas, bloating, and other IBS symptoms that had previously improved with the elimination diet. She also experienced a significant vulvovaginal pain flare that lasted for 4 days and peaked at 8/10 pain. Removing goat cheese again from her diet for several days resulted in significant improvement of her pain. Her diet remained free from goat dairy through the duration of her nutrition therapy.
On July 28, 2015, the patient returned for her fifth nutrition follow-up appointment. She reported a mild, short-term, vulvar pain flare that did not seem to be related to anything in particular. She reintroduced peanuts with no symptoms. The patient reported having intercourse with minimal pain just prior to this appointment. The patient planned to revisit challenging soy (without wheat contamination) next. Upon the reintroduction of soy, she experienced a painful vulvovaginal flare peaking at 7/10 pain, lasting more than 1 week and associated with increased gas and bloating.
She has continued a soy-free diet since, and her symptoms resolved a few days after eliminating soy. After the soy challenge and symptom resolution, she began taking a natural boric acid suppository (“yeast arrest”) and a homeopathic yeast remedy recommended by her functional medicine physician. Then, she reintroduced cow dairy (plain organic yogurt and cheese) with no vulvar pain symptoms. In addition, she reported noticing that her IBS related bloating was decreasing in frequency to less than once per week as the elimination diet progressed. She then followed up with her functional medicine physician and added additional dietary supplements.
During her nutrition follow-up visit on September 22, 2015, the patient reported that she was feeling well with minor discomfort related to the betaine hydrochloric acid (HCL) and digestive enzyme supplement. These were discontinued. At this time, no other foods were reintroduced. Three weeks later, she reported that she felt almost no pain during her internal pelvic floor physical therapy appointment during the previous week. A timeline of this patient’s case is provided in Figure 1.
Patient’s final nutrition appointment was on November 10, 2015. She continued omega-3 fatty acid, vitamin D3, vitamin B12, magnesium, and prebiotic and probiotic supplements (see Table 2) and she consistently maintaining a lacto-ovo vegetarian diet free from meat, fish, goat dairy, soy, and gluten. She reports complete resolution of her IBS symptoms and very minimal vulvovaginal pain including remaining pain free during intercourse.
Table 2.
Interpretation of Functional Testing and Supplement Recommendations
| Test Result | Diagnoses | Interventions (including dose) | Time Frame for Continuing Supplementation |
|---|---|---|---|
| — | Painful menstruation4 | Omega-3 fatty acid EPA/DHA (1 g QD) | Monitor and continue as needed |
| Low vitamin D,25-OH (31 ng/mL) | Vitamin D insufficiency | Vitamin D3 (5000 IU QD) | Monitor and continue as needed |
| Elevated serum homocysteine (10.5 μmol/L) and MTHFR C677T | Decreased methylation efficiency, B12 deficiency | Sublingual vitamin B12 2000 mg (methylcobalamim) | Monitor and continue as needed |
| Low magnesium, RBC (3.3 mg/dL) | Magnesium deficiency | Magnesium (360 mg daily) | Monitor and continue as needed |
|
Signs of bowel inflammation and low immune function in the bowel mucosa | TruFiber prebiotic plus Probiotic (Prescript Assist) | Monitor and continue as needed |
| Low pancreatic elastase (122 μg/mL) | Inefficient digestive enzyme function | Betaine HCL and digestive enzymes | September–October 2015, discontinued |
Abbreviations: EPA/DHA, eicosapentaenoic acid/docosahexaenoic acid; QD, 1 per day; HCL, hydrochloric acid.
Patient sent an e-mail follow-up note that she was able to resume eating gluten prior to and during a vacation to France in December without any increase in symptoms. She continues to tolerate small and occasional amounts of high-quality bread products without any increase in symptoms. She is very happy with her results and continues to feel well with minimal to no pain. When she does increase her consumption of food irritants, her pain level and IBS symptoms do worsen. However, because she is very aware of her symptoms and the impacts of nutrition on her symptoms, she is maintaining her nutrition program independently 5 months postdischarge from nutrition services.
Patient Perspective
My pain has been incredibly decreased overall since I started this program and my irritable bowel symptoms are much better!
I am not presently using any vaginal creams and I did not feel an increase in pain. I think soy was a major trigger and since eliminating it from my diet, my pain level has significantly decreased. Now when I get a flare, the worst it gets is about 3 out of 10, whereas before it could be an 8 or 9 out of 10.
I have started physical therapy (PT) again and am working on reducing the tension in the pelvic floor. I was able to jump back into the PT with more ease and bring in new breathing techniques and stretches now that we don’t have to spend as much time on the muscles. Everything is going in a good direction!
The elimination diet is definitely a challenge. However, it is completely worth trying if it means it can help heal your body after so many years of pain. In order to really receive the benefits of the elimination diet, you definitely need to be committed to the plan, which can be hard (especially for very active, busy women). But it is really all possible with the help of a knowledgeable and patient nutritionist, advice from a team of other medical professionals who care about you, and support from your friends and family. And finally, the most important part of successfully completing the elimination diet, is giving yourself permission to focus on yourself, because you deserve to live a happy, healthy, and pain-free life.
Discussion
Chronic vulvar pain or discomfort, vulvodynia, is a multifactorial gynecological condition for which no obvious etiology has been found. 5 Vulvodynia, present in 16% of all women, can significantly affect the quality of life due to pain, physical disabilities, psychological distress, and sexual dysfunction.6 The gynecologist has a primary role in excluding other causes for vulvar pain, including screening for psychosexual and pelvic floor dysfunction and working with other licensed health care providers.
A review of the literature supports a multidisciplinary approach to the diagnosis and management of a woman presenting with chronic vulvar pain, addressing the biological, psychological, and social/interpersonal factors that contribute.7,8,9,10,11 Women commonly seek complementary treatment for the chronic pain. These treatments include acupuncture (8%), special foods or diets (22%), herbs (27%), and vitamins and minerals (29%). During follow-up surveys conducted annually for 4 years, a substantial proportion of women (44.8%) used complementary health approaches.12 In addition, a current systematic review of the comparative effectiveness of therapies for chronic pelvic pain found insufficient evidence for common surgical (eg, hysterectomy, laparoscopic uterosacral nerve ablation) and nonsurgical approaches (eg, hormonal therapies) but rather found the need to address local injury or inflammation, microbiology (Candida albicans, interleukin-6, and prostaglandin E2 as well as B and T cells arranged in such a pattern to suggest local immune activation), pharmacology, psychotherapy and physiotherapy, and peripheral and or central sensitization of the nervous system.13,14,15 Immune cells, neurons, and shared immune and nervous system signaling molecules form an integrated network. The immune responses can modulate the sensitivity of the nervous system to pain.16,17
Vulvodynia patients are 2 to 4 times more likely to be diagnosed with IBS.3 Food sensitivities are found in nearly one-half of people with IBS with the vast majority of IBS patients believing that certain food items are important triggers of their GI symptoms.18 Further, the typical steroid medications and antibiotics used to address chronic vulvar pain upset the flora balance and add to GI and microbial dysbiosis. Dietary restriction of fermentable oligo, di, monosaccharides, and polyols (FODMAPs) is addressed in the literature as the common dietary intervention for the IBS patient. Current research suggests embracing dietary treatments for IBS with “functional foods.”19
Nutrition therapy from a functional perspective seeks to restore proper functioning of the body by supporting nutritionally and with lifestyle recommendations the body’s innate ability to heal. It is a comprehensive, case-based approach to patient care that focuses on identifying root causes and system imbalances by addressing antecedents, triggers, and mediators that underlie symptoms, signs, illness behaviors, and demonstrable pathology to significantly improve patient health outcomes.20 The functional team approach respects the uniqueness of the individual’s interconnectedness to environment, lifestyle, and community by embracing patient participation to maximize healing opportunities.21
Elimination diets are commonly used by functional nutritionists as an affordable diagnostic tool and/or therapy intervention when seeking the underlying cause of symptoms, especially for those conditions that are idiopathic or multifactorial. Elimination diets are frequently used with suspected food sensitivity or allergy, or GI disorders, and can also set the stage for nutritional education and the implementation of lifestyle changes needed to reduce chronic inflammation. These diets are very customizable to meet the food preferences of the client. Because 95% of known food allergens are from 6 common foods—gliadin (wheat), casein (dairy), soy, corn, eggs, and peanuts—cow’s milk, soy, and wheat being the 3 most common GI food allergens,22 the elimination of these foods is a cornerstone of the healing protocol. In this case, the diet was also “clean,” consisting of organic whole foods with avoidance of processed, refined products, artificial sweeteners, xenobiotic toxins, and genetically modified organisms (GMOs) as much as possible.
The second step to the elimination diet, “the challenge,” is the most critical part of the puzzle and must be done with accuracy and patience, reintroducing 1 food at a time—1 (0.5-cup) serving—and monitor symptoms for 3 days, then 1-2-3—1 serving, 2 times per day, for 3 days, then monitor symptoms for 7 days. Symptoms are unique with each case so patients are instructed to document any changes that they notice. Common symptoms indicative of underlying inflammation include any changes in energy levels, bowel movements, stiffness, pain, skin, weight, respiratory congestion/heat, and/or abdominal distention. If a symptom reoccurs, the reintroduction is stopped, and the patient must wait 7 days before introducing another food, allowing the inflammation to subside. Goat cheese was reintroduced first because it is considered less reactive.23
This patient was willing to be an active participant in her recovery. Although patient reported, her story provided important clues to her case. She remained consistent and compliant throughout a dietary protocol that is challenging for many patients. Given that this was one individual whose chronic conditions dramatically improved utilizing a systematic elimination diet, we cannot be certain how much was due to the elimination diet verses physical therapy and massage therapy. Also, it is well documented that nutritional supplementation is useful for barrier integrity and general health due to nutrient sufficiency—probiotics for IBS; vitamin D3 and pain; omega-3s and inflammation; and B12 and the nervous system. Nutritional supplementation was added toward the end of the patient’s food challenge period. It is important to note that the patient’s vulvodynia and IBS resolved prior to starting the supplement regimen; however, her supplement regimen may be a possible contributor to the maintenance of her pain free state due to improved immune, digestive, and nervous systems functioning. More research needs to be done to be sure that these results can be replicated.
Conclusion
This case demonstrates the potential usefulness of incorporating a functional nutrition approach (elimination diet) to identify foods associated with chronic vulvodynia with overlapping IBS for this patient. In addition, supporting long-term pain resolution by continuing to eliminate foods found that appeared to be associated with chronic inflammation for at least 6 months. Dietary supplements in this patient may have provided multisystem support (digestive, immune, and nervous system) and contributed to long term vulvar pain relief, postprandial pelvic pain relief, and healthy sexual functioning.
Acknowledgements
This case report was written following the CARE guidelines. The authors wish to acknowledge David Riley, md for his support and help in assembling this case report.
References
- 1.Fenton BW, Brobeck L, Witten E, Von Gruenigen V. Chronic pelvic pain syndrome-related diagnoses in an outpatient office setting. Gynecol Obstet Invest. 2012;74(1):64–67. doi: 10.1159/000336768. [DOI] [PubMed] [Google Scholar]
- 2.Fenton BW, Durner C, Fanning J. Frequency and distribution of multiple diagnoses in chronic pelvic pain related to previous abuse or drug-seeking behavior. Gynecol Obstet Invest. 2008;65(4):247–251. doi: 10.1159/000113048. [DOI] [PubMed] [Google Scholar]
- 3.Leusink P, Kaptheijns A, Laan E, van Boven K, Lagro-Janssen A. comorbidities among women with vulvovaginal complaints in family practice. J Sex Med. 2016;13(2):220–225. doi: 10.1016/j.jsxm.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Rahbar N, Asgharzade N, Ghorbani R. Effect of omega-3 fatty acids on intensity of primary dysmenorrhea. Int J Gynaecol Obstet. 2012;117(1):45–47. doi: 10.1016/j.ijgo.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Aroya Z, Edwards L. Vulvodynia. Semin Cutan Med Surg. 2015;34(4):192–198. doi: 10.12788/j.sder.2015.0181. [DOI] [PubMed] [Google Scholar]
- 6.Thornton AM, Drummond C. Current concepts in vulvodynia with a focus on pathogenesis and pain mechanisms. Australas J Dermatol. 2015 Jul; doi: 10.1111/ajd.12365. [e-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Khandker M, Brady SS, Stewart EG, Harlow BL. Is chronic stress during childhood associated with adult-onset vulvodynia? J Womens Health. 2014;23(8):649–656. doi: 10.1089/jwh.2013.4484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khandker M, Brady SS, Vitonis AF, Maclehose RF, Stewart EG, Harlow BL. The influence of depression and anxiety on risk of adult onset vulvodynia. J Womens Health. 2011;20(10):1445–1451. doi: 10.1089/jwh.2010.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindstrom S, Kvist LJ. Erratum to: Treatment of provoked vulvodynia in a Swedish cohort using desensitization exercises and cognitive behavioral therapy. BMC Womens Health. 2015;15(1):121. doi: 10.1186/s12905-015-0280-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadownik LA. Etiology, diagnosis, and clinical management of vulvodynia. Int J Womens Health. 2014;6:437–449. doi: 10.2147/IJWH.S37660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ventolini G. Measuring treatment outcomes in women with vulvodynia. J Clin Med Res. 2011;3(2):59–64. doi: 10.4021/jocmr526w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chao MT, Abercrombie PD, Nakagawa S, Gregorich SE, Learman LA, Kuppermann M. Prevalence and use of complementary health approaches among women with chronic pelvic pain in a prospective cohort study. Pain Med. 2015;16(2):328–340. doi: 10.1111/pme.12585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andrews J, Yunker A, Reynolds WS, Likis FE, Sathe NA, Jerome RN. Noncyclic Chronic Pelvic Pain Therapies for Women: Comparative Effectiveness. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [PubMed] [Google Scholar]
- 14.Reed BD, Legocki LJ, Plegue MA, Sen A, Haefner HK, Harlow SD. Factors associated with vulvodynia incidence. Obstet Gynecol. 2014;123(2 Pt 1):225–231. doi: 10.1097/AOG.0000000000000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foster DC, Falsetta ML, Woeller CF, Pollock SJ, Song K, Bonham A, Phipps RP. Site-specific mesenchymal control of inflammatory pain to yeast challenge in vulvodynia-afflicted and pain-free women. Pain. 2015;156(3):386–396. doi: 10.1097/01.j.pain.0000460320.95267.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verma V, Sheikh Z, Ahmed AS. Nociception and role of immune system in pain. Acta Neurol Belg. 2015;115(3):213–220. doi: 10.1007/s13760-014-0411-y. [DOI] [PubMed] [Google Scholar]
- 17.Ren K, Dubner R. Interactions between the immune and nervous systems in pain. Nat Med. 2010;16(11):1267–1276. doi: 10.1038/nm.2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bohn L, Storsrud S, Tornblom H, Bengtsson U, Simren M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108(5):634–641. doi: 10.1038/ajg.2013.105. [DOI] [PubMed] [Google Scholar]
- 19.Chey WD. Food: The main course to wellness and illness in patients with irritable bowel syndrome. Am J Gastroenterol. 2016;111(3):366–371. doi: 10.1038/ajg.2016.12. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Functional Medicine. What is functional medicine? [Accessed March 5, 2016]. https://www.functionalmedicine.org/page.aspx?id=781#sthash.ho48OvMz.dpuf.
- 21.Benson D. David Jones, MD: Shaping the practice of medicine. Integrat Med Clin J. 2014;13(5):14–16. [PMC free article] [PubMed] [Google Scholar]
- 22.Heine RG. Gastrointestinal food allergies. Chem Immunol Allergy. 2015;101:171–180. doi: 10.1159/000371700. [DOI] [PubMed] [Google Scholar]
- 23.Tomotake H, Katagiri M, Fujita M, Yamato M. Preparation of fresh cheese from caprine milk as a model for the reduction of allergenicity. J Nutr Sci Vitaminol (Tokyo) 2009;55(3):296–300. doi: 10.3177/jnsv.55.296. [DOI] [PubMed] [Google Scholar]