Abstract
Background
A behavioral lifestyle intervention program with goals of increasing physical activity (PA) and losing weight was shown to be efficacious for preventing type 2 diabetes and decreasing risk for cardiovascular disease in the U.S. Diabetes Prevention Program (DPP). Modified versions of the DPP lifestyle intervention are being translated into diverse community settings and have been successful in decreasing weight and improving metabolic markers. However, comprehensive evaluations of PA levels within these community translation intervention efforts are rare.
Purpose
To evaluate the effectiveness of a DPP-based community lifestyle intervention for improving PA levels.
Methods
223 overweight adults at-risk for type 2 diabetes and/or cardiovascular disease were randomized (immediate or 6-month delayed-start) to a 12-month DPP-based lifestyle intervention. Past-month PA level was assessed at baseline and post-intervention with the Modifiable Activity Questionnaire. Simple and mixed-effects regression models were used to determine changes in PA level between and within groups over time.
Results
The between-group mean difference for change in PA levels from baseline to 6 months indicated significantly greater improvement in the intervention compared to the delayed-start group [+6.72 (SE=3.01) MET-hrs/week; p=0.03]. Examining combined within-group change from baseline to post-intervention, mean PA levels significantly increased by +14.69 (SE=1.43) and +9.50 (SE= 1.40) MET-hrs/week at 6 and 12 months post-intervention, respectively. This PA change offset to approximately +10 MET-hrs/week at both 6 and 12 months after adjusting for baseline PA level and season (all; p<0.01). Other than season, sex impacted on change in PA level.
Conclusions
This community-based lifestyle intervention significantly increased PA levels among overweight adults at risk for type 2 diabetes and cardiovascular disease, even after adjusting for key variables.
Clinicaltrials.gov identifier
Keywords: translation, behavioral intervention, Group Lifestyle Balance
Introduction
The U.S. Diabetes Prevention Program (DPP) (11) and other clinical trials (19, 25, 32) demonstrated that intensive lifestyle interventions with goals of increasing PA and achieving modest weight loss can reduce the risk for type 2 diabetes and the metabolic syndrome. The DPP lifestyle intervention participants were shown to significantly increase self-reported leisure PA levels from baseline (8, 11), with nearly 70% of participants meeting the 150 minute per week PA goal after roughly 3 years of follow-up (40). In addition, in post-hoc analyses, for those not meeting the weight loss goal, achievement of the PA goal was associated with a 46% reduction in diabetes incidence over the same time period (8).
Since the end of the original DPP trial, its lifestyle intervention has been translated for delivery in a variety of community settings (39). Modified versions of the DPP lifestyle intervention vary in structure and content, but encourage the DPP lifestyle goals of 150 minutes/week of moderate intensity PA and 7% weight loss. In regard to the effectiveness of these studies, successful weight loss has been demonstrated in most of these community translation efforts (3, 4, 39). In contrast, much less is known about PA, the other primary intervention goal, as only a subset of published DPP translation efforts report results pertaining to PA change (5). In addition, even among translation studies that address PA and its change, there are inconsistencies in PA assessment and outcome reporting. As a result, the impact of DPP-based lifestyle intervention translation efforts on changing PA levels in the community setting is still not well documented.
This manuscript plans to address this hole in the translation literature regarding PA change in community efforts. Specifically, it will focus on examining the impact of an adapted DPP-based behavioral lifestyle intervention conducted in a worksite and three senior community centers on change in PA levels among adult participants at risk for diabetes and cardiovascular disease (CVD). It is hypothesized that leisure PA will significantly increase due to the lifestyle intervention. If the primary hypothesis is supported, a secondary examination of participant, program, and environmental characteristics and each of their potential to impact on PA levels will be conducted. This knowledge will help guide future community DPP translation intervention programs in their efforts to evaluate program effectiveness in regard to the PA goal.
Methods
This investigation is a secondary analysis of an NIH funded randomized intervention trial, the Healthy Lifestyle Project (PI: Dr. A. Kriska; clinicaltrials.gov identifier NCT01050205), evaluating the effectiveness of a DPP-based lifestyle intervention implemented in economically diverse community settings. The Consolidated Standards of Reporting Trials (CONSORT) checklist was used to guide reporting of this investigation (see Document, Supplemental Content 1, CONSORT checklist). The study intervention program, Group Lifestyle Balance ™ (GLB), is a 12-month, 22-session adaptation of the DPP that was developed by members of the original DPP Lifestyle Resource Core who are now faculty members of the University of Pittsburgh Diabetes Prevention Support Center (DPSC). The study investigators partnered with a worksite and three community centers from a range of socioeconomic neighborhoods to implement the DPP-GLB Program. The study protocol was approved by the University of Pittsburgh Institutional Review Board.
The Healthy Lifestyle Project employed a randomized 6-month delayed control design. This design mimics the real-life circumstances facing many community-based providers in that resources may limit the frequency and capacity of programming, requiring interested participants to wait before they can begin the intervention program. Researchers used a stratified randomization scheme to assign participants within each intervention site to begin the DPP-GLB Program immediately (immediate) or after a 6 month delay (delayed) in a 2:1 ratio. The randomization allocation was balanced for each site using a simple randomized sampling procedure and programmed in SAS 9.3 (SAS Institute, Inc.; Cary, NC) by a single study researcher. The randomization assignment was distributed to each participant in a sealed envelope at the end of their baseline assessment visit. Participants and investigators were not blinded to the randomization assignment.
Study population
Recruitment was conducted in the Pittsburgh, Pennsylvania metropolitan area during September 2010–November 2010 at a worksite (30) and September 2011–December 2011 at the three community centers. Site-specific strategies were used to generate interest, including program flyers, ‘lunch and learn’ sessions, e-mail blasts, and mailings. On-site screening involved a finger stick for fasting plasma glucose, HbA1c, and lipid measurements as well as assessment of blood pressure, height and weight to determine BMI, and waist circumference. Eligible adults (age ≥18 years) had a BMI ≥ 24 kg/m2 (≥ 22 kg/m2 for Asians) and pre-diabetes [American Diabetes Association criteria; (10)] and/or the metabolic syndrome [National Cholesterol Education Program criteria; (6)], or treatment for hyperlipidemia and at least one additional component of the metabolic syndrome. Eligible and interested individuals provided written informed consent before enrolling in the study. Prior to engaging in the intervention, enrolled participants were required to obtain physician approval for increasing physical activity levels.
Intervention
The DPP-GLB curriculum has been described elsewhere (12, 14, 37) and program materials are available online (www.diabetesprevention.pitt.edu). In brief, the one-year, 22-session program focuses on healthy eating behaviors, increasing PA to at least 150 minutes of moderate intensity per week, and losing 7% of initial body weight. Participants were encouraged to self-monitor diet, PA, and weight information daily during the 12 month program.
At the time of randomization, participants were given the option of completing the first 12 weekly DPP-GLB sessions in face-to-face groups or to participate via individually-viewed DVD. One hour group sessions were conducted by a DPSC trained lifestyle coach. DVD participants were contacted weekly by the lifestyle coach and had the option of attending monthly group sessions. The remaining 10 bi-weekly and monthly sessions were delivered as face-to-face groups.
General health information was mailed to delayed participants periodically during the 6 month wait-control period. This included handouts on wearing proper shoes during activity, staying hydrated, and reducing salt in the diet. At the end of the 6 month wait-control period, delayed participants received the DPP-GLB program in its entirety in the delivery mode of their choice.
Assessment
All measures were collected by trained research staff following a standard protocol. Due to the study design, participants in the delayed arm attended one additional assessment visit at the end of the 6 month wait-control period during which the same measures completed at baseline were repeated. For the purposes of this evaluation, baseline is in reference to randomization and post-intervention time points (6, 12, 18 months) are in reference to time from an individual’s start of intervention, regardless of randomization assignment. Participants received a $25 gift card for each clinical assessment visit completed, but did not receive compensation for attending intervention sessions.
Demographic Information
Participant birth date (used to determine age), race, ethnicity, sex, and educational attainment was collected by interviewer-administered questionnaire at the on-site screening visit.
Physical Activity
PA levels were assessed via two interviewer-administered questionnaires. At baseline, 6, and 12 months the past month version of the Modifiable Activity Questionnaire (MAQ) was used to capture leisure PA levels. Specifically, the MAQ determines the frequency and duration of recreational activities that are primarily moderate or greater in intensity and occur in bouts of 10 minutes or more. The MAQ is a reliable and valid instrument for use in adult populations (9, 18, 26, 27, 29) with strong correlations (rho >0.60) to bouts of moderate-vigorous activity from accelerometer output (27). The intensity of each activity on the MAQ is estimated in metabolic equivalent tasks (METs), which are units that approximate energy cost (28). The MAQ uses standard MET values (1) to calculate the approximate energy cost in MET-hours per week of each reported activity [e.g. 150 minutes (2.5 hours) brisk walking (MET-equivalent~4) is approximately 10 MET-hours].
At baseline, 6, 12, and 18 months, a simple lifestyle questionnaire (LSQ) developed by members of the research team for use in community translation studies also queried PA. The LSQ asked participants about the frequency (<1 day/month or never; 2–3 days/month; or 1, 2, 3, 4, 5, 6, 7 days/week) and duration (average minutes/day) of typical PA. PA measured by the LSQ was expressed as minutes per week by multiplying frequency and duration, with the midpoint of the range divided by 4 to get days/week for reported frequencies of <1 day/week. The LSQ has not been previously validated. The PA level recorded by the LSQ was compared to the validated MAQ to see if PA trends detected by both were similar.
Season
Winter season occurs in Pittsburgh, Pennsylvania during the months of January–March, when average monthly temperatures are 39.3F and average snowfall is 10.3 inches (23). Summer season occurs during the months of July–September, when average monthly temperatures are 81.4F and average rainfall is 3.48 inches (23). Calendar month of participant assessment visit determined which season was linked with participant data.
Anthropometric and Blood Marker Measurements
Weight, height (baseline only), waist circumference, and fasting (8–16 h) blood samples were collected at baseline, 6, and 12 months. Weight was recorded from a digital physician scale with participants in light clothing and without shoes. Height was recorded from a stadiometer to the nearest quarter inch and used to calculate body mass index (BMI). Waist circumference was measured at the mid-point between the bottom of the twelfth rib and top of the iliac crest. Blood samples were collected by venipuncture in to serum separating tubes and transported to Quest Diagnostics Laboratories (Pittsburgh, PA) for analysis. Samples were analyzed for glucose, hemoglobin A1c, and lipids (total cholesterol, HDL-c, LDL-c, triglycerides) using standard protocols. The results for these measures have been reported in other publications arising from this project (16, 17).
Analysis
Linear regression models compared least squares mean changes in PA levels between the immediate and delayed intervention arms during the 6 month wait-control period. Post intervention change in PA level was calculated as post-intervention PA at 6, 12, and 18 months minus PA at randomization (baseline). Linear mixed effects regression models were used to generate restricted maximum likelihood-based estimates for mean change in PA level at post-intervention time points using all available participant data (intention-to-treat). Models were fit with an unstructured covariance matrix to account for within-subject clustering of data from repeated measures over time (ICC=0.32–0.83) and provide less biased fixed effect estimates and standard errors (20). Residuals were examined to verify that model assumptions were fulfilled.
Participant demographic characteristics, including age, sex, and educational attainment, were tested in univariate and multivariate mixed effects regression models to examine modification in estimates of PA change by these factors. Univariate and multivariate mixed models were fit with binary indicators for season of PA measurement (winter or summer), community setting (worksite or community centers), and primary intervention delivery mode (face-to-face group or DVD) to determine if these factors had an independent effect on change in PA level. Covariates were selected for multivariate models based on univariate effects (p<0.25) and model fit evaluated by AIC and BIC criteria. Intervention site was included as a random effect to account for within-site clustering of the data for the outcomes reported (ICC=0.03–0.18). An alpha of 0.05 (two-sided) was used to determine significance for all statistical tests. SAS 9.4 (SAS Institute, Inc.; Cary, NC) was used to conduct all analysis.
Results
Enrollment and Baseline Characteristics
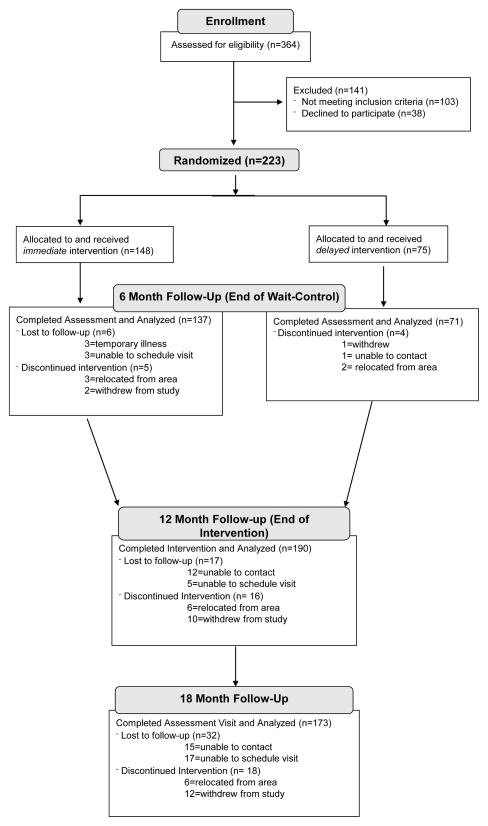
The study enrolled 223 participants at a worksite and three community centers (Figure 1). Participant enrollment and program implementation within each setting has been previously reported (16, 17). Since changes in physical activity were similar across settings, participants from the worksite and all three community centers were combined for this current evaluation. No harms or unintended effects occurred during the study.
Figure 1.
CONSORT Flow Diagram: Participants Enrolling in the Community Lifestyle Intervention Trial
Baseline characteristics for the entire study population and by randomization assignment are presented in Table 1. Demographic and behavioral characteristics were similar between the immediate and delayed intervention arms. The 6-month delayed control design created the opportunity to investigate the impact of season on attempts to increase PA as some of the participants began the lifestyle intervention in the winter season (with a 6 month assessment in the summer) while the rest began intervention during the summer season (with a 6 month assessment in the winter).
Table 1.
Baseline Characteristics for Participants Enrolled in the DPP-based Community Lifestyle Intervention Program
| Randomization Assignment: | Total (N=223) | Immediate (n=148) | Delayed (n=75) | Between Group p-value |
|---|---|---|---|---|
|
| ||||
| Age (years); mean (SD) | 58.4 (11.5) | 59.0 (11.4) | 57.2 (11.6) | 0.28 |
|
| ||||
| Sex; n (%) Female | 139 (62.3) | 92 (62.6) | 47 (62.7) | 0.94 |
|
| ||||
| Ethnicity; n (%) Non-Caucasian | 14 (6.3) | 10 (6.8) | 4 (5.3) | 0.78 |
|
| ||||
| Education: n (%) | 0.73 | |||
| H.S./Some College | 82 (36.8) | 57 (38.5) | 25 (33.3) | |
| B.S. Degree | 68 (30.5) | 45 (30.4) | 23 (30.7) | |
| Graduate Degree | 73 (32.8) | 46 (31.1) | 27 (36.0) | |
|
| ||||
| Employment Status: n (%) | 0.90 | |||
|
| ||||
| Full-time/Part-time | 147 (65.9) | 98 (66.2) | 49 (65.3) | |
|
| ||||
| Weight (lbs); mean (SD) | 208.8 (41.8) | 209.2 (43.9) | 208.1 (37.6) | 0.85 |
|
| ||||
| BMI (kg/m2); mean (SD) | 33.8 (6.0) | 34.0 (6.5) | 33.5 (5.0) | 0.50 |
|
| ||||
| MET-hrs/week LPA (Median, IQR; MAQ) | 7.88 (2.19–16.69) | 8.69 (2.19–19.57) | 6.31 (2.38–12.66) | 0.20 |
|
| ||||
| Minutes/Week Usual PA (Median, IQR; LSQ) | 120 (30–210) | 120 (30–240) | 120 (20–180) | 0.13 |
BS, Bachelor of Science; DPP, Diabetes Prevention Program; HS, High School; IQR, Interquartile range; LPA, Leisure Physical Activity; LSQ, Lifestyle Questionnaire; MAQ, Modifiable Activity Questionnaire; PA, Physical Activity; SD, Standard Deviation
6-Month Wait-Control Behavioral Changes
Participants in the immediate arm reported significantly greater improvements in PA level at the end of the 6-month wait-control period than the delayed participants (Table 2). Model estimated mean leisure PA, as determined by the MAQ, increased in the immediate and delayed arms by +18.75 MET-hrs/week and +12.23 MET-hrs/week, respectively, with a significant intervention effect of +6.72 [standard error (SE)=3.01; p=0.03]. Similar trends in PA were observed based on the LSQ, in which immediate participants reported a non-significant greater mean increase in minutes of usual PA per week compared to the delayed participants.
Table 2.
Model-estimated Least Squares Mean Changes in Physical Activity for the Immediate and Delayed arms at 6 Months
| 6 Month Change (Immediate-Intervention); n=137 Mean (SE) |
6 Month Change (Delayed-wait-control); n=71 Mean (SE) |
Intervention Effect Mean (SE) |
Between group p-value | |
|---|---|---|---|---|
| Leisure PA (MET-hours per week; MAQ) | + 18.75 (1.76)* | +12.23 (2.44)* | +6.72 (3.01) | 0.03 |
| Usual PA (minutes per week; LSQ) | +59.25 (19.86)* | +44.37 (27.68) | +14.88 (34.06) | 0.66 |
IQR, Interquartile Range; LSQ, Lifestyle Questionnaire; MAQ, Modifiable Activity Questionnaire; PA, Physical Activity; SE, Standard Error
p<0.05 change from baseline
Baseline to Post-Intervention Behavioral Changes
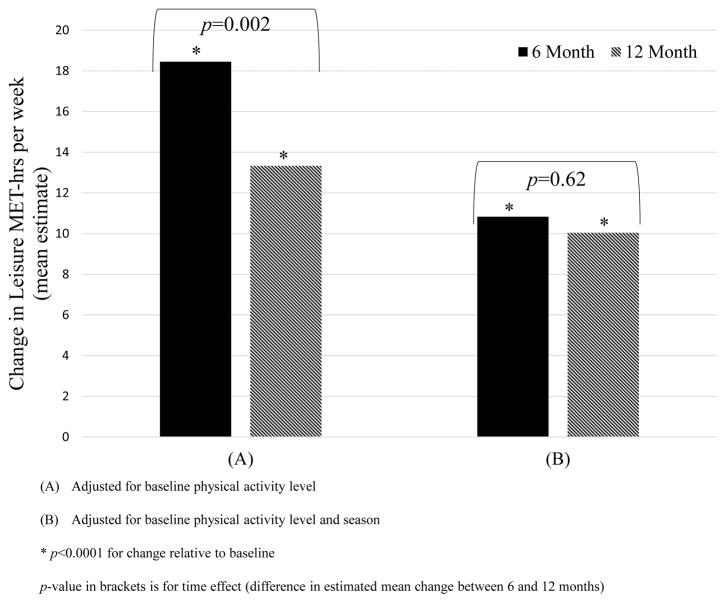
The intervention was successful for increasing PA in both randomized arms at 6 and 12 months post-intervention relative to study baseline (data not shown). Therefore, immediate and delayed arms were combined to describe and evaluate changes in PA as a result of the intervention. Examining baseline to post-intervention PA levels, the unadjusted mean estimate of change in past month leisure PA determined from the MAQ was +14.69 (SE=1.43) MET-hrs/week and +9.50 (SE=1.40) MET-hrs/week at 6 and 12 months, respectively (both p<0.0001; Table 3). This unadjusted mean change in PA was significantly greater at 6 months compared to 12 months (p=0.002). Adjusting for baseline PA level alone resulted in similar trends (Table 3). However, further adjusting for season significantly attenuated the change in PA from baseline to approximately +10 to +11 MET-hrs per week at both 6 and 12 months (Figure 2; Table 3).
Table 3.
Linear Mixed-Effectsa Model Estimated Mean Change in MET-hrs leisure PA per week (MAQ) at 6 and 12 Months
| 6 Month Mean (SE) Estimate of Change (MET-hrs per week) | 12 Month Mean (SE) Estimate of Change (MET-hrs per week) | p-value for time effectb | |
|---|---|---|---|
| Model 1: Unadjusted | 14.69 (1.43)* | 9.50 (1.40)* | 0.002 |
| Model 2: Adjusted for baseline PA level | 18.45 (1.69)* | 13.33 (1.62)* | 0.002 |
| Model 3: Adjusted for baseline PA level, season | 10.83 (1.94)* | 10.04 (1.66)* | 0.62 |
| Model 4: Adjusted for baseline PA level, season, and sexc | 12.41 (2.71)* | 11.67 (2.56)* | 0.64 |
MAQ, Modifiable Activity Questionnaire; MET, Metabolic Equivalent; PA, Physical Activity; SE, Standard Error
intervention site included as random effect
time effect is the difference in estimated mean change between 6 and 12 months
interaction term for sex and baseline PA level included
p<0.0001 change from baseline
Figure 2.
Linear Mixed Model Estimated Baseline to Post-Intervention Mean Change in MET-hrs per week Leisure Physical Activity (PA) from the Modifiable Activity Questionnaire (MAQ)
Adjusting for demographic characteristics, the effect of sex was significant (p<0.05) and contributed to improved fit of the model. Specifically, men reported greater increases in PA level then women. The effects of age and education were not significant. Program characteristics, including setting and delivery mode, did not significantly modify the effect of intervention on change in PA level. The estimates of mean change in PA level from the final model, which includes baseline PA, season, and sex, are presented in Table 3.
The improvement in PA levels demonstrated by the past month MAQ was reflected in the level of typical weekly PA captured by the simple lifestyle questionnaire (LSQ). The model-based mean estimate of change in usual PA was +52.2 minutes per week (SE=12.6; p<0.0001) at 6 months post-intervention, with sustained increases of +45.0 (SE=14.9) minutes per week and +51.5 (SE=17.9) minutes per week at 12 and 18 months post-intervention, respectively (both p=0.004). Adjusting for season attenuated the estimated change to +41.5 (SE=14.8) minutes at 6 months, +40.7 (SE=12.9) minutes at 12 months, and +40.4 (SE=19.2) minutes at 18 months (all; p<0.05). Finally, the estimates of PA levels in minutes per week from the LSQ corresponded to 62.0%, 57.1%, and 52.2% of participants at goal (150 minutes per week or more of usual PA) at 6, 12, and 18 months, respectively.
Discussion
These findings document the effectiveness of a DPP-based community program at increasing PA levels across several community settings. This is one of the few DPP-based translation efforts to report on PA-related outcomes in a large sample and the only known diabetes prevention translation effort to examine the impact of participant, program, and environmental factors on changes in PA level. The results from this study can help guide future assessment and evaluation of the physical activity component of lifestyle change programs offered in community settings.
This current large-scale community translation effort showed that PA levels increased approximately two-fold as a result of the behavioral lifestyle intervention. In conjunction with increased PA, 62% of the participants reported achieving the PA goal at 6 months based upon general lifestyle questions about usual PA. This is comparable to results showing 41–78% of participants reporting to have met the PA goal in other translation programs of similar length that presented PA data (2, 7, 13, 15, 34, 35, 38). The PA level increases in this study likely contributed to the significant weight loss and improvements in diabetes and CVD risk factors observed at 6, 12, and 18 months, which have been previously described (16, 17). The finding that men increased PA more than women during intervention replicates earlier observations from the DPP and, more recently, a community DPP translation effort in which men were more likely to meet the PA goal than women (2, 40).
The influence of season on PA levels had been previously demonstrated in observational studies (21, 22, 24, 31) but has not previously been considered in community-based translation efforts. The results of this investigation suggested that, after adjusting for season, the mean increase in past month leisure PA at 6 and 12 months post-intervention was attenuated relative to the unadjusted values. The magnitude of the PA change due to the community DPP-based intervention after adjustment for season was similar to that observed in the DPP at 1 year (11). This adds credibility to our finding as PA levels in the DPP were assessed with the past year version of the MAQ, which is not as susceptible to season influence.
This current translation finding identifies the importance of accounting for season when determining intervention impact on PA levels, as weather shifts related to seasonal change often occur during the course of intervention in temperate zones. These results also have important implications for implementation of these community programs such that participants who engage in an intervention during the winter months may need extra encouragement and strategies to increase or maintain PA levels.
This evaluation has a few limitations that should be noted. Physical activity data was self-reported via questionnaire and thus subject to recall and reporting bias. The addition of objective measures such as accelerometers can provide less biased estimates of total time spent at different intensities of PA. However, accelerometers are not always feasible in community translation efforts and they do not provide complete information regarding the context of movement which can be valuable to interventionists in order to provide participant feedback. In addition, although our communities varied by socioeconomic status, the racial and ethnic composition of the sample was representative of the communities surrounding the intervention sites (33); which, unfortunately is low in racial and ethnic diversity. This restricted the ability to investigate the potential differences by race/ethnicity for observed changes in PA levels and limits the generalizability of these findings.
Finally, due to the study timeline, season of PA measurement at any given post-intervention time-point (i.e. 6 or 12 months) was pre-determined by randomization assignment. Although it cannot be certain that randomization assignment did not impact estimates of PA change, the evidence from observational (21, 22, 31) and experimental (24) studies supports the idea that season may impact changes in PA levels during an intervention. Furthermore, as reported in other evaluations of this current effectiveness study (16, 17, 36), baseline to post-intervention changes in weight and risk factors for type 2 diabetes and CVD were similar in each randomization arm, contributing to the notion that an intervention delay does not impact on the success of the program. Future investigations using study designs that enable a more discriminate investigation of season effects on measured PA changes during a behavioral lifestyle intervention are needed.
Conclusions
This investigation provides evidence that a behavioral lifestyle intervention, modified from the successful DPP for delivery in multiple community settings, significantly improves PA levels in addition to resulting in successful weight loss among individuals at-risk for diabetes and CVD. This evaluation allowed for the impact of the intervention on increasing PA levels to be considered independently from the changes in PA level possibly due to season. Future evaluations should include not only a thorough assessment of PA levels but also a careful consideration of the calendar season in which PA is measured, especially in temperate areas, in order to fully understand the impact of the intervention on improving PA behaviors and related health outcomes.
Supplementary Material
Acknowledgments
The authors would like to thank the DPP-GLB participants, community and worksite partners, and staff for their time and continued commitment to this project.
Source of Funding:
Funding support was provided by the National Institutes of Health through grant number R18 DK081323-04; Clinicaltrials.gov number NCT01050205. This funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health nor do the results of the present study constitute endorsement by ACSM.
Footnotes
Conflicts of Interest
The study authors have no conflicts of interest to declare.
References
- 1.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Jr, Tudor-Locke C, et al. Compendium of Physical Activities: a second update of codes and MET values. Medicine and Science in Sports and Exercise. 2011;43(8):1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 2.Amundson HA, Butcher MK, Gohdes D, Hall TO, Harwell TS, Helgerson SD, et al. Translating the diabetes prevention program into practice in the general community: findings from the Montana Cardiovascular Disease and Diabetes Prevention Program. The Diabetes Educator. 2009;35(2):209–10. 13–4, 16–20. doi: 10.1177/0145721709333269. passim. [DOI] [PubMed] [Google Scholar]
- 3.Baker MK, Simpson K, Lloyd B, Bauman AE, Singh MA. Behavioral strategies in diabetes prevention programs: a systematic review of randomized controlled trials. Diabetes Res Clin Pr. 2011;91(1):1–12. doi: 10.1016/j.diabres.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 4.Cardona-Morrell M, Rychetnik L, Morrell SL, Espinel PT, Bauman A. Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition interventions feasible and are the outcomes from reference trials replicable? A systematic review and meta-analysis. BMC Public Health. 2010;10:653. doi: 10.1186/1471-2458-10-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eaglehouse YL, Kramer MK, Rockette-Wagner B, Arena VC, Kriska AM. Evaluation of physical activity reporting in community Diabetes Prevention Program lifestyle intervention efforts: A systematic review. Prev Med. 2015;77:191–9. doi: 10.1016/j.ypmed.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 6.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–8. doi: 10.1161/01.cir.0000111245.75752.c6. [DOI] [PubMed] [Google Scholar]
- 7.Guyse LA, McHugh BR, Meszaros JF, Vanderwood KK, Hall TO, Arave D, et al. Collaborative approach to implementing an adapted Diabetes Prevention Program lifestyle intervention. Diabetes Spectrum. 2011;24(3):138–43. doi: 10.2337/diaspect.24.3.138. [DOI] [Google Scholar]
- 8.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes care. 2006;29(9):2102–7. doi: 10.2337/dc06-0560. Epub 2006/08/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobi D, Charles MA, Tafflet M, Lommez A, Borys JM, Oppert JM. Relationships of self-reported physical activity domains with accelerometry recordings in French adults. European Journal of Epidemiology. 2009;24(4):171–9. doi: 10.1007/s10654-009-9329-8. Epub 2009/03/14. [DOI] [PubMed] [Google Scholar]
- 10.Kerner W, Bruckel J. Definition, classification and diagnosis of diabetes mellitus. Experimental and Clinical Endocrinology & Diabetes. 2014;122(7):384–6. doi: 10.1055/s-0034-1366278. [DOI] [PubMed] [Google Scholar]
- 11.Knowler WC, Barnett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or Metformin. New Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al. Translating the Diabetes Prevention Program: A comprehensive model for prevention training and program delivery. American Journal of Preventive Medicine. 2009;37(6):505–11. doi: 10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Kramer MK, McWilliams JR, Chen HY, Siminerio LM. A community-based diabetes prevention program: evaluation of the group lifestyle balance program delivered by diabetes educators. The Diabetes Educator. 2011;37(5):659–68. doi: 10.1177/0145721711411930. [DOI] [PubMed] [Google Scholar]
- 14.Kramer MK, Venditti EM, Semler LN, Kriska AM, Miller RG. Long-term Strategies for Diabetes Prevention: Evaluation of the Group Lifestyle Balance Post-Core Sessions Focusing on Carbohydrate and Hunger Management. Journal of Diabetes & Metabolism. 2012;S2(01) doi: 10.4172/2155-6156.s2-006. [DOI] [Google Scholar]
- 15.Kramer MK, Cepak YP, Venditti EM, Semler LN, Kriska AM. Evaluation of the Group Lifestyle Balance programme for diabetes prevention in a Hispanic Women, Infants and Children (WIC) Programme population in the USA. Diversity and Equality in Health and Care. 2013;10:73–82. [Google Scholar]
- 16.Kramer MK, Vanderwood K, Eaglehouse Y, Miller RG, Arena V, Venditti E, et al. Diabetes prevention efforts in the community are effective for older, at-risk adults. Diabetes. 2014;63(Suppl 1):A1–A102. doi: 10.2337/db14-1-388. [DOI] [Google Scholar]
- 17.Kramer MK, Molenaar DM, Arena VC, Venditti EM, Meehan RJ, Miller RG, et al. Improving employee health: evaluation of a worksite lifestyle change program to decrease risk factors for diabetes and cardiovascular disease. Journal of Occupational and Environmental Medicine. 2015;57(3):284–91. doi: 10.1097/jom.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kriska AM, Knowler WC, LaPorte RE, Drash AL, Wing RR, Blair SN, et al. Development of questionnaire to examine relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990;13(4):401–11. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 19.Lindstrom J, Peltonen M, Eriksson JG, Ilanne-Parikka P, Aunola S, Keinanen-Kiukaanniemi S, et al. Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS) Diabetologia. 2013;56(2):284–93. doi: 10.1007/s00125-012-2752-5. Epub 2012/10/25. [DOI] [PubMed] [Google Scholar]
- 20.Mallinckrodt CH, Kaiser CJ, Watkin JG, Molenberghs G, Carroll RJ. The effect of correlation structure on treatment contrasts estimated from incomplete clinical trial data with likelihood-based repeated measures compared with last observation carried forward ANOVA. Clin Trials. 2004;1(6):477–89. doi: 10.1191/1740774504cn049oa. [DOI] [PubMed] [Google Scholar]
- 21.McCormack GR, Friedenreich C, Shiell A, Giles-Corti B, Doyle-Baker PK. Sex- and age-specific seasonal variations in physical activity among adults. Journal of Epidemiology and Community Health. 2010;64(11):1010–6. doi: 10.1136/jech.2009.092841. [DOI] [PubMed] [Google Scholar]
- 22.Merchant AT, Dehghan M, Akhtar-Danesh N. Seasonal variation in leisure-time physical activity among Canadians. Canadian Journal of Public Health (Revue Canadienne de Sante Publique) 2007;98(3):203–8. doi: 10.1007/BF03403713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Weather Service. 1981–2010 Climate Normals. Pittsburgh, PA: 2015. Available from: http://www.weather.gov/media/pbz/normals/PIT_MonthlyAve.pdf. [Google Scholar]
- 24.Newman MA, Pettee KK, Storti KL, Richardson CR, Kuller LH, Kriska AM. Monthly variation in physical activity levels in postmenopausal women. Medicine and Science in Sports and Exercise. 2009;41(2):322–7. doi: 10.1249/MSS.0b013e3181864c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ning F, Wang S, Wang Y, Sun J, Zhang L, Gao W, et al. Weight change in association with the incidence of type 2 diabetes in adults from Qingdao, China. Zhonghua liu xing bing xue za zhi. 2014;35(7):764–8. [PubMed] [Google Scholar]
- 26.Pettee Gabriel K, McClain JJ, Lee CD, Swan PD, Alvar BA, Mitros MR, et al. Evaluation of physical activity measures used in middle-aged women. Medicine and Science in Sports and Exercise. 2009;41(7):1403–12. doi: 10.1249/MSS.0b013e31819b2482. [DOI] [PubMed] [Google Scholar]
- 27.Pettee Gabriel K, McClain JJ, Schmid KK, Storti KL, Ainsworth BE. Reliability and convergent validity of the past-week Modifiable Activity Questionnaire. Public Health Nutr. 2011;14(3):435–42. doi: 10.1017/s1368980010002612. [DOI] [PubMed] [Google Scholar]
- 28.Pettee KK, Storti KL, Ainsworth BE, Kriska AM. Measurement of physical activity and inactivity in epidemiologic studies. In: Lee IM, editor. Epidemiologic Methods in Physical Activity Studies. New York, New York: Oxford University Press; 2009. [Google Scholar]
- 29.Schulz LO, Harper IT, Smith CJ, Kriska AM, Ravussin E. Energy intake and physical activity in Pima Indians: comparison with energy expenditure measured by doubly-labeled water. Obes Res. 1994;2(6):541–8. doi: 10.1002/j.1550-8528.1994.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 30.Taradash J, Kramer M, Molenaar D, Arena V, Vanderwood K, Kriska AM. Recruitment for a Diabetes Prevention Program translation effort in a worksite setting. Contemporary Clinical Trials. 2015;41c:204–10. doi: 10.1016/j.cct.2015.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tucker P, Gilliland J. The effect of season and weather on physical activity: a systematic review. Public Health. 2007;121(12):909–22. doi: 10.1016/j.puhe.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 32.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50. doi: 10.1056/nejm200105033441801. [DOI] [PubMed] [Google Scholar]
- 33.United States Census Bureau. State & County QuickFacts. 2015 [updated 24-Mar-2015]. Available from: quickfacts.census.gov.
- 34.Vadheim LM, Brewer KA, Kassner DR, Vanderwood KK, Hall TO, Butcher MK, et al. Effectiveness of a lifestyle intervention program among persons at high risk for cardiovascular disease and diabetes in a rural community. The Journal of Rural Health. 2010;26(3):266–72. doi: 10.1111/j.1748-0361.2010.00288.x. [DOI] [PubMed] [Google Scholar]
- 35.Vanderwood KK, Hall TO, Harwell TS, Butcher MK, Helgerson SD, et al. Montana Cardiovascular D. Implementing a state-based cardiovascular disease and diabetes prevention program. Diabetes Care. 2010;33(12):2543–5. doi: 10.2337/dc10-0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vanderwood KK, Kramer MK, Arena VC, Miller RG, Meehan RJ, Kriska AM. Does Waiting Matter? The Effects of Weight Change During Intervention Delay on Participants’ Success in a Community Diabetes Prevention Effort. Diabetes. 2014;63(Suppl 1):A179. [Google Scholar]
- 37.Venditti EM, Kramer MK. Necessary components for lifestyle modification interventions to reduce diabetes risk. Curr Diab Rep. 2012;12(2):138–46. doi: 10.1007/s11892-012-0256-9. [DOI] [PubMed] [Google Scholar]
- 38.Whittemore R, Melkus G, Wagner J, Dziura J, Northrup V, Grey M. Translating the diabetes prevention program to primary care: a pilot study. Nursing Research. 2009;58(1):2–12. doi: 10.1097/NNR.0b013e31818fcef3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whittemore R. A systematic review of the translational research on the Diabetes Prevention Program. Translational Behavioral Medicine. 2011;1(3):480–91. doi: 10.1007/s13142-011-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004;12(9):1426–34. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.