Abstract
Animals interact with humans in multiple ways, including as therapy and service animals, commercially as livestock, as wildlife, and in zoos. But the most common interaction is as companion animals in our homes, with an estimated 180 million cats and dogs living in US households. While pet ownership has been reported to have many health benefits, the findings are inconsistent. Cardiovascular risk factors such as lipids, glucose, obesity, and heart rate variability have improved, worsened, or remained the same in the limited number of studies considering companion animals. Physical activity increases have more consistently been linked with dog ownership, although whether this reflects antecedent motivation or direct benefit from the dog is unclear. Allergies and asthma also are variably linked to pet ownership and are confounded by family history of atopy and timing of exposure to pet dander. The benefits of companion animals are most likely to be through reduction in depression, anxiety, and social isolation, but these studies have been largely cross-sectional and may depend on degree of bonding of the owner with the animal. Positive relationships show measurably higher oxytocin with lower cortisol and alpha-amylase levels. Finally, pet ownership is also a marker of better socioeconomic status and family stability, and if companion animals are to provide cardiovascular risk benefit, the route should perhaps be through improved education and opportunity for ownership.
Keywords: Pets, Human-animal interaction, Asthma, Physical activity, Oxytocin, Depression
Introduction
Animals interact with humans in multiple ways, including as therapy and service animals, commercially as livestock, as wildlife, and in zoos. But the most common interaction is as companion animals in our homes. The American Veterinary Medical Association [1] estimated that in 2012, 36.5 % of the US households owned dogs, 30.4 % owned cats, 3.1 % owned birds, and 1.5 % owned horses; this translates to almost 70 million dogs and 74 million cats living with us. Of the most common pets, 30 % of owners have at least two dogs and 54 % of owners have at least two cats [2].
These companion animals play multiple roles in our lives and may affect human health. In 2013, the American Heart Association published a Scientific Statement about pet ownership and cardiovascular risk [3••], concluding that pet ownership, particularly dog ownership, is probably associated with decreased cardiovascular disease (CVD) risk, and that pet ownership, particularly dog ownership, may have some causal role in reducing CVD risk. However, both of these conclusions were based on limited populations and were derived either from a single randomized trial or nonrandomized studies. CVD risk was defined as systemic hypertension, hyperlipidemia, physical inactivity, obesity, autonomic function and cardiovascular reactivity, and survival in patients with or without established CVD. The most compelling evidence was on dog ownership and recreational physical activity, but the statement found that this benefit was not consistent and may only be via behavioral intention, motivation or social support rather than directly due to dog ownership. The committee's recommendations were that pet ownership, particularly dog ownership, may be reasonable for reduction in CVD risk, but that pet adoption should not be done with the primary purpose of reducing CVD risk.
Given this background, this review will summarize existing evidence briefly and discuss recent evidence of the role of pets in CVD risk, focusing on clinical CVD, current findings on CVD risk factors, depression, markers of stress and emotional attachment, and immunoglobulins and asthma.
Clinical Cardiovascular Disease
Some of the earliest reports relating to health benefits of companion animals have been in patients who have survived coronary heart disease. Friedmann et al. [4] looked at the effects of social isolation and social support in 92 white survivors of myocardial infarction or angina pectoris, and found that among pet owners, the one-year survival was 94 % as compared to 72 % among those who were not pet owners. The authors found that the benefits of pet ownership extended beyond physical activity among dog walkers and attributed the reduced mortality to emotional effects of companionship, with associated improvement in depression. They later replicated the results in 424 patients after acute myocardial infarction [5]. Friedmann et al. [6] extended their results to 460 participants enrolled in the international Psychosocial Responses in the Home Automated External Defibrillator Trial (PR-HAT) who were followed for a median of 2.8 years. In multivariable-adjusted Cox regression models, pet ownership was associated with lower mortality and was also part of a borderline statistically significant interaction with depression such that the inverse association between pet ownership and mortality was strongest in depressed patients.
Cardiovascular benefits of pets have also been shown with physical and psychological stress. Allen et al. [7] examined the influence of having friends, spouses, and pets in 240 married couples, half with pets and half without, on mental arithmetic and cold pressor tests. They found that pet owners had lower heart rates and blood pressure at rest, and recovered faster from stress. Heart rate variability has been shown to be higher among post-myocardial infarction patients who also owned pets, including 5-minute averages and successive differences in normal-to-normal intervals. These effects were strongest for dog owners [8]. A more recent study examined 191 patients, mean age 69 years, with lifestyle-related conditions (diabetes, hypertension, and/or hyperlipidemia) [9] to determine if pet ownership was associated with cardiac autonomic nervous activity imbalance. Pet owners were defined by current pet ownership for at least 6 months prior to enrollment. Heart rate variability was recorded by 24-h Holter electrocardiogram, and 43 % of the sample had pets. After multivariable-adjustment, the pet owner group had statistically significantly higher high-frequency components for 24 h, daytime and nighttime as well as greater entropy, and lower low-frequency/high-frequency ratios at all times compared to nonowners. The authors concluded that pet ownership modulates cardiac autonomic nervous activity in patients without clinical cardiovascular disease but with lifestyle-related conditions. However, the data were cross-sectional and differences in patients who had pets compared to nonowners such as walking, type of pet, and bond with the pet could not be assessed due to small sample size. A more recent study designed to evaluate the effects of touching a dog, a stuffed dog or a person during a working memory task as a stressor [10] found no difference in heart rate variability in healthy university students ages 18 to 41 years.
Qureshi et al. [11] reported on risk of death due to myocardial infarction, combined cardiovascular disease (myocardial infarction or stroke), stroke and all-cause mortality over a 20-year follow-up using National Health and Nutrition Examination Study (NHANES II) Follow-up Study data. They identified 4435 participants who reported any kind of allergy and were subsequently asked about pet ownership. Of these, 2435 (55 %) were current or past owners of cats. Past cat ownership was associated with a statistically significant 37 % lower risk of fatal myocardial infarction after controlling for age, gender, race/ethnicity, systolic blood pressure, cigarette smoking, diabetes, cholesterol, and body mass index. The authors postulated that the protective effect may have been due to a relaxing effect on autonomic reactivity, or that personalities of cat owners may be protective toward cardiovascular disease. While intriguing, there were no associations of current cat ownership or dog ownership with fatal myocardial infarction, nor were there associations with stroke; the sample was derived only from those with self-reported allergies, limiting generalizability.
CVD Risk Factors
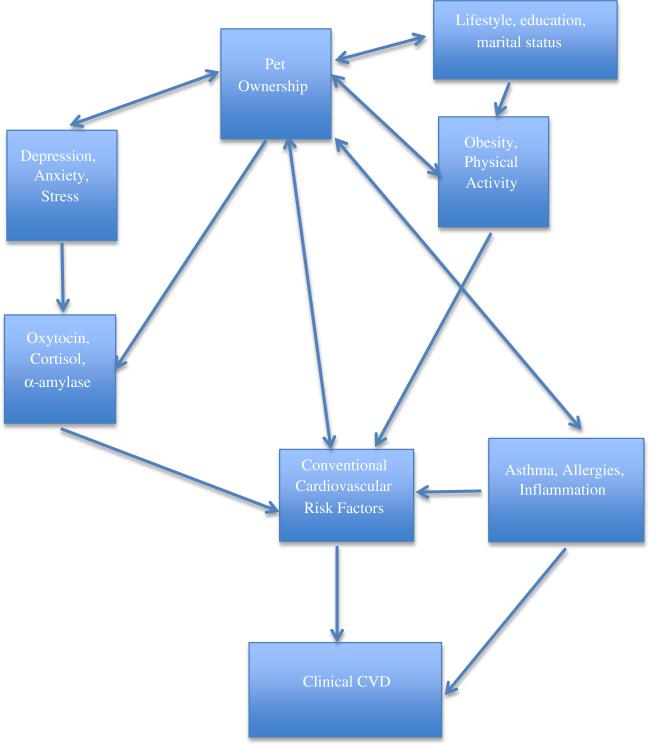
If the associations between pet ownership and cardiovascular disease are not directly related to the pet itself, then finding a potential pathway of companion animals that mediates risk factor reduction may be an alternate explanation, particularly given the potential that a lifestyle factor is likely to produce small improvements in modifiable risk factors affecting large numbers of people (Fig. 1). This would commonly produce changes in healthy individuals rather than in clinical cases with comorbidities and numerous medications for their conditions.
Fig. 1.
Conceptual model of how pet ownership may be related to cardiovascular disease through risk factors and lifestyle
The earliest studies on risk factor reduction associated with pet ownership were related to hypertension. A study of 48 hypertensive individuals in high-stress professions examined systolic blood pressure, diastolic blood pressure, heart rate, and plasma renin activity responses to mental stress delivered as a standard mental arithmetic task and speech [12]. Participants were assigned to pet ownership plus lisinopril (20 mg/day) or lisinopril only. Before drug therapy, responses to mental stress were the same in the two groups. ACE inhibitor therapy lowered resting blood pressure in both groups, but responses to mental stress were statistically significantly lower in pet owners compared to those who only used lisinopril, including blood pressure, heart rate, and plasma renin activity. The authors concluded that pet ownership increased social support and therefore lowered blood pressure response to mental stress. A more recent study on the presence of pets in older (50–83 years) pet owners with pre- to mild hypertension who were living independently used ambulatory monitoring to assess blood pressure at baseline, and after 1 and 3 months when pets were present or not present [13]. In 32 pet owners (24 dog owners, 11 cat owners), the presence of a dog was associated with lower systolic and diastolic blood pressure, and cats were associated with lower diastolic but higher systolic blood pressure. Both types of pets were associated with greater self-reported happiness and lower anger, frustration, and annoyance when the pet was in the room versus not.
Other risk factors have been linked to pet ownership, although less consistently. Levine et al. [3••] summarized evidence for previous lipid changes over the past 20 years or so, and reported on a cross-sectional study with modest in differences in total cholesterol (201 versus 206 mg/dL) and triglycerides (108 versus 125 mg/dL) in male dog owners compared to nonowners, with no differences observed among female dog owners. Other studies have also been cross-sectional and small in size, and results have been inconsistent, with higher cholesterol and diabetes in dog owners reported in one study and beneficial results attenuated with control for BMI. Pet ownership has also not been consistently associated with reduced obesity. The underlying hypothesis is that dogs provide social support and motivation to make changes in lifestyle habits. It is difficult for observational studies to determine causality—do dog owners purchase dogs to help motivate them to exercise and lose weight? In that case, dog owners will likely be heavier, have a higher prevalence of diabetes, and be more sedentary than nonowners. A study that examined short-term interactions between ten female dog owners and their Labrador dogs found that when owners stroked, petted, and talked to their dogs for 3 minutes, their insulin levels went down in the first hour afterward. Insulin levels also went down in the control owners (no dogs present), but went up in the dogs themselves [14], suggesting differences in short-term hormone levels between humans and dogs, although heart rates decreased only in the owners and cortisol increased in the dogs.
Schreiner [15] found that there were no consistent cross-sectional differences in a wide array of cardiovascular risk factors, including lipids, blood pressure, diabetes, and inflammatory markers, between current dog owners, current cat owners, and past/never owners of either among middle-aged participants in the CARDIA Study. However, additional cross-sectional analyses did show that dog owners were more likely to engage in moderate physical activity such as walking even though there was no impact on either current weight or 25-year change in weight [16].
The one relatively consistent health benefit of pet ownership on cardiovascular risk is walking with dogs. Inactive dog owners in an intervention study that provided information about health benefits to both humans and dogs of walking compared to usual walking habits [17] walked more either with or without the dog, but those who were told about health benefits for the dogs had greater numbers of steps. Older participants, ages 71 to 82, in the Health, Aging and Body Composition Study (Health ABC) walked more, increased their walking speed over time, and had improved mobility compared to nonowners of dogs [18], and the RESIDential Environment (RESIDE) project also found that dog owners walked more than nonowners [19]. In both studies, however, only 36 % walked their dogs at least three times per week (Health ABC) or 23 % walked their dogs at least five times per week (RESIDE). Lentino et al. [20] examined 916 people over the age of 18 years recruited online who walked their dogs, owned dogs and did not walk them, or did not own dogs; dog owners were asked to recruit non-dog owners to try to balance sociodemographic characteristics. This cross-sectional study composed largely of educated white women showed that those who did not own dogs had greater odds of self-reported diabetes (OR = 2.53, 95 % CI (1.17–5.48)), hypertension (OR = 1.49 (1.03–2.83)), hypercholesterolemia (OR = 1.72 (1.06–2.81)), and depression (OR = 1.49 (1.09–2.05)) after controlling for age and moderate-to-high physical activity compared to those who regularly walked their dogs. Therefore, while dog ownership is associated with greater amounts of walking, the improvement is not universal and may reflect either greater motivation in the owners, better health or other markers of greater socioeconomic advantage, or a stronger bond with the pet. All of these may lead to health benefits that are not directly linked to the dog.
Depression and Psychological Characteristics
The INTERHEART study reported that psychological stress accounts for more than 30 % of the attributable risk for acute myocardial infarction [21], and that stress, depression, hostility, anxiety, and isolation are potent cardiovascular risk factors leading to chronic autonomic imbalance, abdominal obesity, increased cortisol, and other adverse physiological effects. One of their recommended cardioprotective responses is pet ownership, which provides social connectedness and altruistic benefits of caring for another life. Much of the research on the benefits of pets in the elderly has been in animal-assisted therapy and trials without controls, although any kind of pet has been shown to improve loneliness scores [22•] and has long been associated with better diet quality such as consuming more vegetable servings and eating at more regular intervals [23]. Pet ownership is most likely to benefit humans through reductions in depression, anxiety, and social isolation that lead to increased activity of the sympatho-adrenal-medullary system and the hypothalamic-pituitary-adrenal axis [24]. But to be effective, pets may need to alter the owners’ perceptions of the situations and people that are stressful, which also requires a bond, and lifestyle may drive the selection of the pet rather than the pet providing change.
While companion animals are thought to be largely beneficial, they are not without adverse psychological effects. A study of 177 clients from 14 randomly selected veterinary practices found that pet death was associated with severe grief in 30 % of the participants. One of the main factors was attachment to the pet, which is also one of the characteristics that provide health benefits [25]. Grief was characterized by sleeplessness, loss of appetite, and depression; however, most could maintain daily activities such as going to work, eating, sleeping, and parenting. In a Finnish cross-sectional study of a population-based random sample of over 21,000 people stratified by gender and age groups 20–24, 30–34, 40–44, and 50–54, pet owners had higher BMIs and were older, and lower social class [26]. Depression, panic attacks, migraines, and rheumatoid arthritis were more common in women pet owners, but social class explained most of these relatively weak associations. The authors concluded that a pet may help with coping of difficult life situations, and that cross-sectional data cannot determine causality. In a study of 17 men and women ages 62–88 years who had survived a stroke, animals provided both physical and psychosocial motivation for recovery after the stroke to walk dogs, to provide companionship to their animals, and as a social lubricant to encourage interaction with others [27]. But the fear of losing companion animals, being unable to take care of a new pet, and the accompanying grief among the elderly who live alone was also noted as a strong adverse effect.
Cortisol, Oxytocin, and Alpha-amylase: Markers of Stress and Emotional Attachment
Physical and psychological stress can be measured with biomarkers from blood, urine, and saliva. Salivary cortisol has been used as a measure of the hypothalamus-pituitary-adrenal (HPA) axis response to stressors. Cortisol has large diurnal variation and may be associated with longer latency between the stressor and its response [28]. Elevated cortisol has been associated with risk of glucose intolerance, insulin resistance and type 2 diabetes [29] as well as endothelial damage, visceral fat accumulation, and impaired lipid metabolism in individuals with subclinical hypercortisolism [30]. As a measure, salivary cortisol has been shown to detect individual differences in activity of the HPA axis, to be reduced with positive touch, and to be increased with distinct stressors such as depression, social or economic hardship, and acute stressors such as math challenges. As an established measure, cortisol has been validated against instruments that measure stress. While cortisol is widely used, concerns with the measure include its variation by age, sex, food, and pregnancy, as well as marked diurnal variation.
Acting in conjunction with the HPA axis is the sympatho-adrenal-medullary (SAM) system, which is the sympathetic response to stressors. The biomarker that has recently been measured to assess SAM activity is alpha-amylase. Alpha-amylase shows heightened autonomic nervous system activity similar to the hormone norepinephrine, is increased in response to both physiological and psychological stress, and is measurable in saliva. Unlike cortisol, salivary alpha-amylase (sAA) is relatively constant across the day, and measures sympathetic activation for conditions such as chronic pain and state anxiety. The two measures capture different components of the stress response, and studies that have used the beta-blocker propranolol to suppress stress responses have shown an effect on sAA without affecting cortisol [31]. Compared to salivary cortisol, sAA represents short-term latency to stressors [28, 32, 33]. Its levels are also increased with exercise and caffeine intake and are correlated with norepinephrine levels during short duration response to psychological stress. sAA is thought to be a marker of autonomic dysregulation, with levels higher in atopic diseases such as asthma and dermatitis [34].
Both salivary cortisol and sAA levels may be reduced based on positive associations with companion animals [14], and sAA reactions to acute psychological stressors may be attenuated by bonding with pets. However, given the transitory nature of these stress biomarkers, and the variety of relationships that people have with animals sharing their environments, determining these associations is extremely difficult.
The latest salivary marker of stress that has been linked to the human-animal bond is oxytocin, a hypothalamic hormone that is a neuromodulator of emotional attachment, positive physical contact, and social cognitive processes [35]. Oxytocin is increased with lactation, parturition, sexual activity, touch, and warmth. Higher levels have been associated with lower heart rate, depression, and perception of pain. Like cortisol and sAA, oxytocin is associated with both acute and chronic stimuli, and like sAA, does not appear to exhibit diurnal variation.
Inhaled oxytocin enhances trusting behavior and emotional bonding when introduced as a nasal spray in dogs compared to saline spray [35]. Intranasal oxytocin decreases stress hormone levels, is anti-inflammatory, decreases pain perception, and increases with touch [36]. Oxytocin is increased in humans with petting animals, particularly with bonded dogs [14]. In a study that examined the role of bonded dogs with workplace stress assessed by either interacting with dogs at the end of a day or reading nonfiction materials, Miller et al. [37] found statistically significant increases in oxytocin among women interacting with their dogs, but not among men, suggesting either an estrogen effect or differences in interpersonal relationships that were not measured in the study.
Others have suggested that while the biochemistry of responding to stressors should be the same in men and in women, there may be differences in perception through the sympathetic nervous system via the hypothalamus, with increases in heart rate and blood pressure, as well as triggering different releases of corticotrophin-releasing factor from the paraventricular nucleus and concomitant cortisol increase [38]. In rats, oxytocin leads to reductions in sympathetic activity and blood pressure. As described above, in humans, much of the research has been experimental rather than in companion animals, and the results have been positive, negative, and neutral. In married couples that did and did not own pets, those with pets had lower baseline blood pressure and heart rates than those without pets, and stressors such as the cold pressor test and arithmetic challenges were associated with smaller blood pressures increases and faster recovery in those with pets. These differences were small, in the order of 6 mmHg and 3 beats/min for blood pressure and heart rate, respectively, but statistically significant. The impact of pets was greater than that of a friend or a spouse, reflecting the potential lack of critical judgment by the pet. A review by Beetz et al. [39•] suggests that oxytocin may be the underlying mechanism behind the human-animal interaction effects, which in turn may be driven by the degree of bonding.
Allergies, Asthma, and Immune Response
The hygiene hypothesis, attributed to Strachan [40], states that lack of early childhood exposure to infectious agents, certain microbiota, and parasites can increase susceptibility to future allergies and asthma by suppressing the natural development of the immune system. Allergies and asthma may be directly associated with CVD risk through greater levels of inflammation or indirectly through lower levels of physical activity, more social isolation, depression, and obesity. Wegienka et al. [41•] found that exposure to dogs during the first year of life was associated with a relative risk of 0.50 (0.27, 0.92) for sensitization (defined as animal-specific IgE ≥ 0.35 kU/L) at age 18 for boys. This association was not found in girls, perhaps reflective of the different prevalence of asthma and allergies in boys and girls, as well as different pet interactions. They found that for both sexes, early exposure to cats was associated with a 48 % lower relative risk of sensitization at age 18. Cumulative exposure or other ages of exposure to pets were not associated with reduced sensitization. Sensitization is linked to recurrent asthma exacerbation and suggests a role for pets in reducing asthma incidence in susceptible children.
The allergen found in cat dander protein, Fel d 1, and that found in dog saliva, Can f 6, are potent allergens that provoke severe allergic responses. They belong to a group of allergen immunomodulatory proteins that promote airway hypersensitivity reactions such as asthma, making the potential of avoiding or reducing sensitization appealing [42]. Individual response to these allergens, as well as susceptibility, is still poorly understood, but may be modulated by Toll-like receptor 4 (TLR4) and its gene, which are responsible for pathogen recognition and immune system activation. TLR4 may help to explain the wide variability in response to dander and why atopy appears in families.
The association of pets with asthma has been hindered by methodological issues, most prominently the selective avoidance or removal of cats because of allergic symptoms or family history of allergies. Pet ownership's effects on immune function and asthma appear to be a combination of genetic susceptibility and timing of exposure, and that sensitization in both childhood and adulthood can lead to future asthma, inflammation, and multiple allergies.
Asthma prevalence differs greatly by race, with data from NHANES III on 18,825 US adults ages 20 years and greater reporting a 4.5 % prevalence of current asthma, but a 5.1 % prevalence among non-Hispanic blacks [43]. After controlling for multiple risk factors, including self-reported pet ownership, the odds of asthma in blacks compared to whites was 9 % higher but no longer statistically significant. A report by the Pet Food Institute [44] found that 22 % of black households had dogs or cats compared to 61 % of white households. Schreiner [45] found that in the CARDIA cohort, cat ownership was positively related to white race and lower age in cross-sectional multivariable models, while white race, having children, physical activity, working full-time, and being married were positively associated with dog ownership. Other factors such as BMI, smoking, education, and sex were not independently associated with either cat or dog ownership. Socioeconomic opportunity may certainly be tied to asthma through the environment and through access to health care as well as discretionary income, which also may impact the ability to own or retain a companion animal. All of these may contribute to CVD risk.
Conclusions
While cardiovascular disease epidemiology tends to focus on high-risk individuals, those with high relative risk of events represent a small proportion of the population. Pet ownership, on the other hand, is a common lifestyle factor among free-living individuals. As such, while the impact of any type of pet ownership is likely to be small, the population-attributable risk may be large. Pets provide both positive (exercise, companionship, structured lifestyle and health habits) and negative (allergies, grief over their loss) impact on lives. Some of this depends on why a person chooses to adopt a pet, the level of bonding that an individual has with the pet, or the underlying personality of the pet owner. Herzog [46] states that research on the health effects of animals is inconclusive because of difficulties determining why people choose to live with pets, and that pets may not cause individuals to be happier or healthier. Many studies rely on self-report rather than objective measures of health, and there are a lack of appropriately designed studies that address the biases associated with both investigator belief in the benefits of human-animal interaction and participation by animal-friendly volunteers.
Nonetheless, improvement in depression and social support can impact immune response and motivation to make positive health changes. Data from the UK Biobank in almost 500,000 participants [47] have confirmed what we have seen repeatedly in public health: that self-reported quality of life measures are some of the strongest predictors of all-cause mortality, including CVD. If pet ownership is associated with improved quality of life through social support, reduced depression, and other psychosocial predictors of health, perhaps the question is not whether to get a pet or not, but how to make pets more available to those with financial or housing limitations.
Footnotes
This article is part of the Topical Collection on Cardiovascular Risk Health Policy
Compliance with Ethical Standards
Conflict of Interest Dr. Schreiner has no conflicts of interest to disclose.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by the author.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.U.S. Pet Ownership & Demographics Sourcebook. 2012 https://www.avma.org/kb/resources/statistics/pages/market-research-statistics-us-pet-ownership-demographics-sourcebook.aspx.
- 2.American Pet Products Association. 2012 http://www.humanesociety.org/issues/pet_overpopulation/facts/pet_ownership_statistics.html.
- 3••.Levine GN, Allen K, Braun LT, Christian JE, Friedmann E, Taubert KA, et al. Pet ownership and cardiovascular risk. A scientific statement from the American Heart Association. Circulation. 2013;127:2353–63. doi: 10.1161/CIR.0b013e31829201e1. [This scientific statement provides an evidence-based overview of pet ownership and hypertension, hyperlipidemia, physical activity, obesity, autonomic function, and cardiovascular reactivity, and survival in people with and without established cardiovascular disease. The studies are displayed based on level of evidence and the authors conclude that pet ownership is probably associated with decreased CVD risk and that this role may be causal.] [DOI] [PubMed] [Google Scholar]
- 4.Friedmann E, Katcher AH, Lynch JL, Thomas SA. Animal companions and one-year survival of patients after discharge from a coronary care unit. Public Health Rep. 1980;95(4):307–12. [PMC free article] [PubMed] [Google Scholar]
- 5.Friedmann E, Thomas S. Pet ownership, social support, and one-year survival after acute myocardial infarction in the Cardiac Arrhythmia Suppression Trial (CAST). Am J Cardiol. 1995;76:1213–7. doi: 10.1016/s0002-9149(99)80343-9. [DOI] [PubMed] [Google Scholar]
- 6.Friedmann E, Thomas SA, H S, for the HAT Investigators Pets, depression and long-term survival in community living patients following myocardial infarction. Anthrozoös. 2011;24(3):273–85. doi: 10.2752/175303711X13045914865268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen K, Blascovich J, Mendes WB. Cardiovascular reactivity and the presence of pets, friends, and spouses: the truth about cats and dogs. Psychosom Med. 2002;64:727–39. doi: 10.1097/01.psy.0000024236.11538.41. [DOI] [PubMed] [Google Scholar]
- 8.Friedmann E, Thomas SA, Stein PK, Kleiger RE. Relation between pet ownership and heart rate variability in patients with healed myocardial infarctions. Am J Cardiol. 2003;91:718–21. doi: 10.1016/s0002-9149(02)03412-4. [DOI] [PubMed] [Google Scholar]
- 9.Aiba N, Hotta K, Yokoyam M, Wang G, Tabata M, Shimizu R, et al. Usefulness of pet ownership as a modulator of cardiac autonomic imbalance in patients with diabetes mellitus, hypertension, and/or hyperlipidemia. Am J Cardiol. 2012;109:1164–70. doi: 10.1016/j.amjcard.2011.11.055. [DOI] [PubMed] [Google Scholar]
- 10.Gee NR, Friedmann E, Stendahl M, Fisk A, Coglitore V. Heart rate variability during a working memory task: does touching a dog or person affect the response? Anthrozoös. 2014;27(4):513–28. [Google Scholar]
- 11.Qureshi AI, Memon MA, Vazquez G, Suri MFK. Cat ownership and risk of fatal cardiovascular diseases. Results from the second national health and nutrition examination study mortality follow-up study. J Vasc Interv Neurol. 2009;2(1):132–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Allen K, Shykoff BE, Izzo Jr JL. Pet ownership, but not ACE inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38:815–20. [PubMed] [Google Scholar]
- 13.Friedmann E, Thomas SA, Son H, Chapa D, McCune S. Pet's presence and owner's blood pressures during the daily lives of pet owners with pre- to mild hypertension. Anthrozoös. 2013;26(4):535–50. [Google Scholar]
- 14.Handlin L, Hydbring-Sandberg E, Nilsson A, Ejdeback M, Jansson A, Uvnas-Moberg K. Short-term interaction between dogs and their owners: effects of oxytocin, cortisol, insulin and heart rate—an exploratory study. Anthrozoös. 2011;24(3):301–15. [Google Scholar]
- 15.Schreiner P. Pet ownership and factors associated with cardiovascular health: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Epidemiol. 2012;175(suppl 11):s108. [Google Scholar]
- 16.Schreiner P. HAI and health outcomes: associations of pet ownership with adiposity in middle age: the CARDIA study. International Society for Anthrozoology Annual Meeting; Chicago: 2013. [Google Scholar]
- 17.Rhodes RE, Murray H, Temple VA, Tuokko H, Wharf Higgins J. Pilot study of a dog walking randomized intervention: effects of a focus on canine exercise. Prev Med. 2012;54:309–12. doi: 10.1016/j.ypmed.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Thorpe RJ, Simonsick EM, Brach JS, Ayonayon H, Satterfield S, Harris TB, et al. Dog ownership, walking behavior, and maintained mobility in late life. J Am Geriatr Soc. 2006;54:1419–24. doi: 10.1111/j.1532-5415.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 19.Cutt H, Giles-Corti B, Knuiman M, Timperio A, Bull F. Understanding dog owners' increased levels of physical activity: results from RESIDE. Am J Public Health. 2008;98(1):66–9. doi: 10.2105/AJPH.2006.103499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lentino C, Visek AJ, McDonnell K, DiPietro L. Dog walking is associated with a favorable risk profile independent of a moderate to high volume of physical activity. J Phys Act Health. 2012;9:414–20. doi: 10.1123/jpah.9.3.414. [DOI] [PubMed] [Google Scholar]
- 21.Das S, O'Keefe JH. Behavioral cardiology: recognizing and addressing the profound impact of psychosocial stress on cardiovascular health. Curr Atheroscler Rep. 2006;8:111–8. doi: 10.1007/s11883-006-0048-2. [DOI] [PubMed] [Google Scholar]
- 22•.Cherniack EP, Cherniack AR. The benefits of pets and animal-assisted therapy to the health of older individuals. Curr Gerontol Geriatr Res. 2014;2014:623203. doi: 10.1155/2014/623203. [This is a balanced review of the benefits of pets on mental and physical health in the elderly that also addresses negative effects of pets.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dembicki D, Anderson J. Pet ownership may be a factor in improved health of the elderly. J Nutr Elder. 1996;15(3):15–31. doi: 10.1300/J052v15n03_02. [DOI] [PubMed] [Google Scholar]
- 24.Friedmann E, Son J. The human-companion animal bond: how humans benefit. Vet Clin Small Anim. 2009;39:293–326. doi: 10.1016/j.cvsm.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 25.Adams CL, Bonnett BN, Meek AH. Predictors of owner response to companion animal death in 177 clients from 14 practices in Ontario. JAVMA. 2000;217(9):1303–9. doi: 10.2460/javma.2000.217.1303. [DOI] [PubMed] [Google Scholar]
- 26.Koivusilta LK, Ojanlatva A. To have or not to have a pet for better health? PLoS ONE. 2006;1:e109. doi: 10.1371/journal.pone.0000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johansson M, Ahlstrom G, Jonsson A-C. Living with companion animals after stroke: experiences of older people in community and primary care nursing. Br J Community Nurs. 2014;19(12):578–84. doi: 10.12968/bjcn.2014.19.12.578. [DOI] [PubMed] [Google Scholar]
- 28.Maruyama Y, Kawano A, Okamoto S, Ando T, Ishitobi Y, Tanaka Y, et al. Differences in salivary alpha-amylase and cortisol responsiveness following exposure to electrical stimulation versus the Trier Social Stress Tests. PLoS ONE. 2012;7(7):e39375. doi: 10.1371/journal.pone.0039375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siddiqui A, Madhu SV, Sharma SB, Desai NG. Endocrine stress responses and risk of type 2 diabetes mellitus. Stress. 2015;13:1–9. [PubMed] [Google Scholar]
- 30.Di Dalmazi G, Pasquali R, Beuschlein F, Reincke M. Subclinical hypercortisolism: a state, a syndrome, or a disease? Eur J Endocrinol. 2015;173:M61–71. doi: 10.1530/EJE-15-0272. [DOI] [PubMed] [Google Scholar]
- 31.Van Stegeren A, Rohleder N, Everaerd W, Wolf OT. Salivary alpha amylase as marker for adrenergic activity during stress: effect of betablockade. Psychoneuroendocrinology. 2006;31:137–41. doi: 10.1016/j.psyneuen.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Noto Y, Sato T, Kudo M, Kurata K, Hirota K. The relationship between salivary biomarkers and state-trait inventory score under mental arithmetic stress: a pilot study. Anesth Analg. 2005;101:1873–6. doi: 10.1213/01.ANE.0000184196.60838.8D. [DOI] [PubMed] [Google Scholar]
- 33.Engert V, Vogel S, Efanov SI, Duchesne A, Corbo V, Ali N, et al. Investigation into the cross-correlation of salivary alpha-amylase responses to psychological stress. Psychoneuroendocrinology. 2011;36:1294–302. doi: 10.1016/j.psyneuen.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 34.Nater UM, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology. 2009;34:486–96. doi: 10.1016/j.psyneuen.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 35.Romero T, Nagasawa M, Mogi K, Hasegawa T, Kikusui T. Oxytocin promotes social bonding in dogs. PNAS Early Edition. 2014:1–6. doi: 10.1073/pnas.1322868111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morelius E, Ortenstrand A, Theodorsson E, Frostell A. A randomized trial of continuous skin-to-skin contact after preterm birth and the effects on salivary cortisol, parental stress, depression, and breastfeeding. Early Hum Dev. 2015;91:63–70. doi: 10.1016/j.earlhumdev.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 37.Miller SC, Kennedy C, DeVoe D, Hickey M, Nelson T, Kogan L. An examination of changes in oxytocin levels in men and women before and after interaction with a bonded dog. Anthrozoös. 2009;22(10):31–42. [Google Scholar]
- 38.Pickering TG. Men and from Mars, women are from Venus: stress, pets, and oxytocin. J Clin Hypertens. 2003;5(1):86–8. doi: 10.1111/j.1524-6175.2003.01922.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39•.Beetz A, Uvnas-Moberg K, Julius H, Kotrschal K. Psychosocial and psychophysiological effects of human-animal interactions: the possible role of oxytocin. Front Psychol. 2012;3:1–15. doi: 10.3389/fpsyg.2012.00234. [This article discusses how improvements in stress-related parameters, immune system function, heart rate and blood pressure attributed to companion animals are mainly through psychological benefits that lead to activation of the oxytocin system.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299(6710):1259–60. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41•.Wegienka G, Johnson CC, Havstad S, Ownby DR, Nicholas C, Zoratti EM. Lifetime dog and cat exposure and dog- and cat-specific sensitization at age 18 years. Clin Exp Allergy. 2011;41:979–86. doi: 10.1111/j.1365-2222.2011.03747.x. [This article investigates the time window during which exposure to dog and cat dander influences sensitization, and finds that the first year of life is critical, but that cumulative exposure or exposure at other ages is not associated with reduced allergies or asthma.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Herre J, Gronlund H, Brooks H, Hopkins L, Waggoner L, Murton B, et al. Allergens as immunomodulatory proteins: the cat dander protein Fel d 1 enhances TLR activation by lipid ligands. J Immunol. 2013;191:1529–35. doi: 10.4049/jimmunol.1300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arif AA, Delclos GL, Lee ES, Tortolero SR, Whitehead LW. Prevalence and risk factors of asthma and wheezing among US adults: an analysis of the NHANES III data. Eur Respir J. 2003;21:827–33. doi: 10.1183/09031936.03.00054103a. [DOI] [PubMed] [Google Scholar]
- 44.US dog or cat ownership rates by race/ethnicity. Pet Food Institute; http://www.statista.com/statistics/250858/dog-or-cat-ownership-rates-of-us-households-by-race-ethnicity/ [Google Scholar]
- 45.Schreiner P. Characteristics of pet ownership in a population-based cohort: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 2012;175(suppl 11):s55. [Google Scholar]
- 46.Herzog H. The impact of pets on human health and psychological well-being: fact, fiction, or hypothesis? Curr Dir Psychol Sci. 2011;20:236–9. [Google Scholar]
- 47.Ganna A, Ingelsson E. 5 year mortality predictors in 498,103 UK Biobank participants: a prospective population-based study. Lancet. 2015;386(9993):533–40. doi: 10.1016/S0140-6736(15)60175-1. [DOI] [PubMed] [Google Scholar]