Abstract
Renal hyperparathyroidism (rHPT) is a common complication of chronic kidney disease characterized by elevated parathyroid hormone levels secondary to derangements in the homeostasis of calcium, phosphate, and vitamin D. Patients with rHPT experience increased rates of cardiovascular problems and bone disease. The Kidney Disease: Improving Global Outcomes guidelines recommend that screening and management of rHPT be initiated for all patients with chronic kidney disease stage 3 (estimated glomerular filtration rate, < 60 mL/min/1.73 m2). Since the 1990s, improving medical management with vitamin D analogs, phosphate binders, and calcimimetic drugs has expanded the treatment options for patients with rHPT, but some patients still require a parathyroidectomy to mitigate the sequelae of this challenging disease.
BACKGROUND
In the US, chronic kidney disease (CKD) affects 14% of the population,1,2 including approximately 660,000 patients with end-stage renal disease (ESRD) who are dialysis-dependent.2 Renal hyperparathyroidism (rHPT) is a common complication of CKD characterized by derangements in the homeostasis of calcium, phosphorus, and vitamin D.3 rHPT is associated with increased cardiovascular morbidity and mortality4–8 and has a significant economic burden on the US health care system.9
rHPT is classically broken into 2 types on the basis of the patient’s serum calcium level. Secondary hyperparathyroidism (2° HPT) is the elevation of parathyroid hormone (PTH) in response to hypocalcemia induced by phosphate retention and reduced calcitriol synthesis as a consequence of reduced renal function.10 In 2° HPT, all the parathyroid glands become enlarged owing to parathyroid hyperplasia. Because 2° HPT is a compensatory mechanism of the parathyroid glands, it commonly resolves with normalization of calcium and phosphorus homeostasis (eg, renal transplantation). Tertiary hyperparathyroidism (3° HPT) is seen when a patient with longstanding 2° HPT develops autonomous PTH secretion, often associated with hypercalcemia. This is observed in up to 30% of patients with ESRD, who then undergo renal transplant.11 3° HPT is classically thought to have come from parathyroid hyperplasia, but some studies have suggested that up to 20% of patients may have single or double adenomas.11,12
Since the 1990s, improving medical management with vitamin D analogs, phosphate binders, and calcimimetic drugs has expanded the treatment options for patients with rHPT, but parathyroidectomy remains necessary for many patients.
NORMAL CALCIUM AND PHOSPHORUS HOMEOSTASIS
Calcium and phosphorus homeostasis is maintained through a complex relationship between the bones, intestine, kidneys, and parathyroid glands. PTH is probably the most important regulator of calcium metabolism and functions primarily via 3 mechanisms:
PTH is thought to stimulate PTH receptors mainly on osteoblasts, which then, through multiple cell-to-cell mechanisms, stimulate osteoclast formation and bone resorption, leading to increased serum calcium and phosphorus levels.13
PTH activates 1-α-hydroxylase in the kidney, which catalyzes the conversion of nonactive 25-hydroxy (25-OH) vitamin D to activated 1,25 dihydroxy (1,25-OH) vitamin D. This leads to increased absorption of calcium and phosphorus in the gut.
PTH increases reabsorption of calcium and decreases reabsorption of phosphorus in the kidney.
Recently, there has been much interest in the role of fibroblast growth factor 23 (FGF-23), a protein secreted by bone in response to hyperphosphatemia, which functions primarily in maintaining phosphorus homeostasis. FGF-23 stimulates phosphorus excretion in the kidney mainly through reduced action of sodium-phosphate co-transporter in the proximal tubule. It also decreases 1-α-hydroxylase activity, leading to reduced 1,25-OH vitamin D levels.14,15 In CKD, FGF-23 levels progressively rise and are initially thought to be beneficial, given the phosphaturic effects. However, increasing FGF levels are also associated with increased cardiovascular mortality in patients with CKD.16
PATHOGENESIS
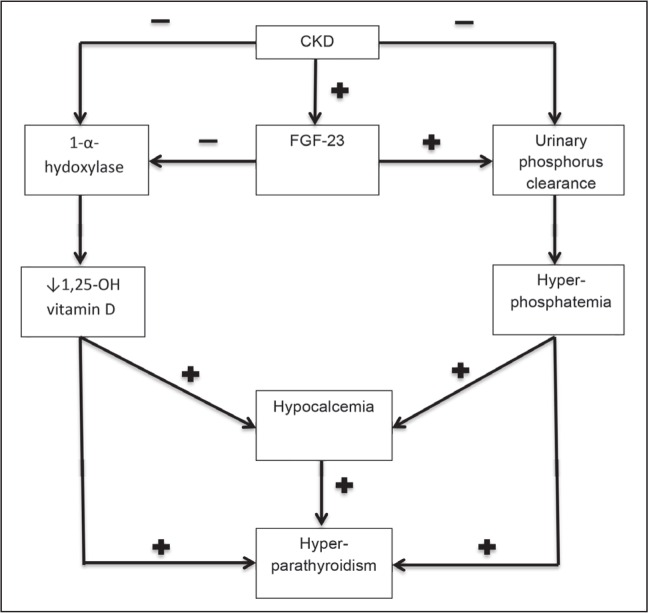
The pathogenesis of rHPT is complex and incompletely understood (Figure 1). An increase in PTH levels typically develops when the glomerular filtration rate (GFR) drops below 60 mL/min/1.73 m2. Abnormalities in serum levels of phosphorus and calcium tend to occur much later in the course of CKD (typically when the GFR drops below 40 mL/min/1.73 m2).17 Initially, the elevated PTH levels serve to increase renal phosphorus excretion. However, as the GFR declines further, serum phosphorus levels start to rise and induce hypocalcemia by binding bioavailable calcium as CaHPO4, which indirectly leads to a further rise in PTH production. CKD also leads to decreased activity of 1-α-hydroxylase, thereby decreasing 1,25-OH vitamin D. A lack of 1,25-OH vitamin D inhibits gastrointestinal absorption of calcium and also directly stimulates the parathyroid glands.14
Figure 1.
Schematic of the pathogenesis of renal hyperparathyroidism.
CKD = chronic kidney disease; FGF-23 = fibroblast growth factor 23.
In CKD, chronic stimulation of the parathyroid glands triggers diffuse polyclonal hyperplasia. As the chronic stimulation of CKD continues, the parathyroids begin to develop monoclonal nodules within a background of parathyroid hyperplasia. These nodules demonstrate increased resistance to vitamin D and calcimimetic medications and may be the etiology of the loss of negative feedback seen in 3° HPT.18,19
CLINICAL MANIFESTATIONS
The two most important sequelae of rHPT are 1) renal osteodystrophy and 2) cardiovascular disease. Recognizing that the bone and cardiovascular complications seen in CKD are manifestations of a broader interrelated syndrome, the National Kidney Foundation initiated the term “CKD-mineral and bone disorder” to describe the complex pathophysiology of the calcium, phosphorus, and PTH derangements seen in CKD. The paradigm of “think beyond the bones” is emphasized to bring early attention to the complications of rHPT in an attempt to improve morbidity and mortality.20
Renal osteodystrophy refers to a group of bone disorders caused by dysregulation of mineral metabolism in CKD, including osteomalacia, adynamic bone disease, and osteitis fibrosa cystica. Osteomalacia is a state of low bone turnover leading to poor mineralization. Adynamic bone disease is also a low-turnover pathology with normal mineralization that probably results from a low PTH state. The incidence of adynamic bone disease increasing is likely secondary to PTH oversuppression from vitamin D agents, calcimimetics, and phosphate binders.14,21 Osteitis fibrosis cystica is a high-turnover bone disease that stems from elevated PTH concentrations stimulating osteoclast activity, bone breakdown, and resorption. This can lead to subsequent bone pain and fractures.22 With longstanding bone resorption, patients may develop localized regions of bone loss that are then replaced by fibrous tissue, resulting in a brown tumor. These “tumors” appear as well-defined, lytic lesions on radiograph and may be mistaken for metastasis (Figure 2).
Figure 2.
Radiograph of the hands of a 55-year-old patient with renal osteodystrophy and brown tumors of the fourth metacarpal and third phalanx of the left hand (arrows). Image is courtesy of John Hunter, MD.
The derangements in calcium and phosphate that result from rHPT may accelerate vascular calcification, including coronary artery calcification. Calcification of the cardiovascular tissue can affect the myocardium, atrial-ventricular conduction, and valvular function.23 Furthermore, coronary calcification may put patients at an increased risk of cardiovascular events and death.24 It is difficult to distinguish the unique detrimental effects of rHPT from those of hyperphosphatemia, which is also associated with cardiovascular disease in patients with CKD. Some studies have suggested that FGF-23 may induce arterial smooth muscle myocytes to change into osteoblast-like cells that lead to vascular calcification.17 Moderate to severe hyperparathyroidism (PTH concentrations ≥ 600 pg/mL) may increase risk of cardiovascular death,7 though the causality of this association is debatable.
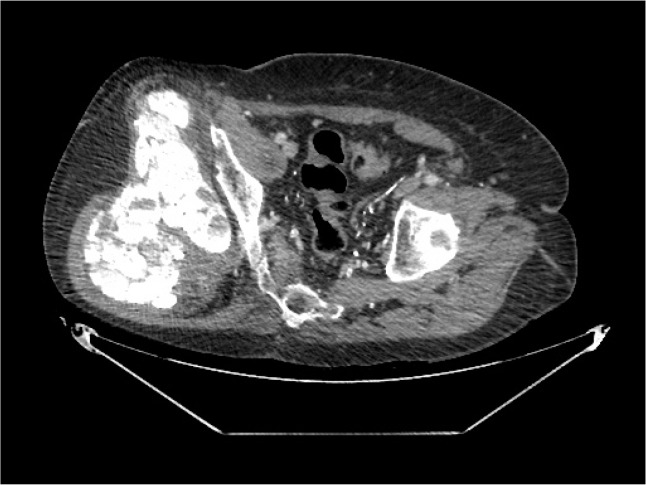
There is an association between CKD and medial calcification in the arterioles of the skin and soft tissue leading to vascular compromise and ulceration. This constellation of complications was formerly called calciphylaxis but is now termed calcific uremic arteriolopathy, and it is associated with an eight-fold increase in mortality rate.25 Tumoral calcinosis is an uncommon complication of longstanding rHPT and is classically associated with high serum levels of calcium and phosphorus. In tumoral calcinosis, the patient can develop soft-tissue calcium deposits that can appear to be soft-tissue malignant tumors on imaging studies (Figure 3).26
Figure 3.
Radiograph of the right hip of a 63-year-old man with tumoral calcinosis.
DIAGNOSIS AND MANAGEMENT
The Kidney Disease: Improving Global Outcomes work group recommends screening and management of rHPT be initiated for all patients with CKD stage 3 (estimated GFR < 60 mL/min). The frequency of monitoring for serum calcium, phosphorus, and PTH are listed in Table 1.27
Table 1.
Summary of National Kidney Foundation guidelines on evaluation of calcium and phosphorus metabolism and parathyroid hormone
| CKD stage | GFR range (mL/min/1.73 m2) | Measure PTH | Measure calcium and phosphorus | Target PTH (pg/mL) |
|---|---|---|---|---|
| Progressive stage 3 | 30–59 | Baseline | 6–12 months | < the upper limit of normal for assay |
| Stage 4 | 15–29 | 6–12 months | 3–6 months | < the upper limit of normal for assay |
| Stage 5 | < 15 or dialysis | 3–6 months | 1–3 months | 2–9 x the normal limit of the assay |
CKD = chronic kidney disease; GFR = glomerular filtration rate; PTH = parathyroid hormone.
The initial management of rHPT follows a stepwise approach with the goal of optimizing serum phosphorus and calcium levels through a combination of a low phosphorus diet, phosphate binders, vitamin D derivatives, and calcimimetic medications.
Low Phosphorus Diet
A low phosphorus diet is recommended for patients with CKD and 2° HPT with hyperphosphatemia.27 Dietary restriction of phosphorus in patients without elevated levels of phosphorus, but with elevated PTH levels only, is controversial. Unfortunately, this is very difficult given the high prevalence of phosphorus in Western diets. Dietary phosphorus comes from 2 sources: 1) protein-rich food groups such as meat and milk; and 2) phosphorus additives, which are used to process meats and cheeses. Phosphorus used as an additive is often only implied in the ingredients list, and not individually reported on the food label. Therefore, the true amount of phosphorus contained in a product may be underestimated.14 Patient education regarding this distinction may help them avoid phosphorous-rich foods. The National Kidney Foundation previously recommended that patients with CKD restrict dietary phosphorus to 800 to 1000 mg/day. However, it should be noted that there is a paucity of good quality data regarding dietary phosphorus restriction and outcomes in CKD.
Phosphate Binders
Because of the difficulty in maintaining a low phosphorus diet, phosphate binders are usually an essential part of medical therapy for patients with CKD. Phosphate binders have been shown to decrease serum phosphorous and PTH levels.28 Isakova et al29 reported that treatment with phosphorus binders was independently associated with decreased mortality when compared with no treatment.
Several phosphate binders are available, including aluminum hydroxide, calcium salts, sevelamer hydrochloride, sevelamer carbonate, and lanthanum carbonate. In general, aluminum hydroxide should be limited to a short period because of the risk of aluminum toxicity. Newer agents such as lanthanum have unknown long-term effects of bone deposition. Iron-based binders such as sucroferric oxyhydroxide are also available to lower serum phosphorous. The Kidney Disease Outcomes Quality Initiative recommends for patients with CKD stages 3 and 4, that phosphate binders be used if phosphorus levels cannot be controlled within the target range despite dietary phosphorus restriction. In patients who remain hyperphosphatemic despite initiation of a single phosphate binder, combination therapy can be used.23 It is interesting to note that lanthanum, being a heavy metal, commonly shows up as radiopaque in noncontrast radiologic studies of the gastrointestinal tract.30
Vitamin D Analogs
As described above, 1,25-OH vitamin D deficiency is a major mechanism of rHPT, and vitamin D replacement has been shown to effectively suppress PTH secretion.31–34 Several forms of vitamin D are available, including ergocalciferol (which requires activation in the kidney to 1,25-OH vitamin D), as well as activated forms such as calcitriol, paricalcitol, and doxercalciferol. Although observational studies have suggested improved survival in patients treated with vitamin D analogs, a 2007 meta-analysis showed no difference in mortality, bone pain, vascular disease, or rate of parathyroidectomy when comparing patients on vitamin D analogs versus those not taking vitamin D.14,35
The Kidney Disease: Improving Global Outcomes work group recommends that in patients with CKD stages 3 to 5 (not on dialysis), attempts to control hyperphosphatemia, hypocalcemia, and vitamin D deficiency be made first. If PTH remains elevated or is progressively rising, treatment with calcitriol or vitamin D analogs is suggested. Close attention must be paid to serum levels of calcium and phosphorus, which if greater than 10.2 mg/dL and 4.6 mg/dL, respectively, may warrant modification in therapy. In patients with CKD stage 5 on dialysis, active vitamin D sterols (such as calcitriol, paricalcitol, or doxercalciferol) are used to control hyperparathyroidism.
Calcimimetics
Cinacalcet HCL is a calcimimetic agent that exhibits allosteric modulation of the calcium receptor on the parathyroid gland, increasing sensitivity to extracellular calcium and thereby suppressing PTH secretion.36 The effectiveness of cinacalcet in lowering PTH concentrations in ESRD patients has been demonstrated in multiple studies. Combined analysis of these studies showed that cinacalcet decreases rates of parathyroidectomy, fractures, and cardiovascular hospitalization. Patients receiving cinacalcet treatment rather than placebo also have improvements in self-reported physical function and less bodily pain.37
In 2012, the Evaluation of Cinacalcet Hydrochloride Therapy to Lower Cardiovascular Events Trial randomized patients with ESRD and moderate to severe rHPT to cinacalcet or placebo and found that cinacalcet did not significantly reduce overall or cardiovascular mortality.38 A recent Cochrane review corroborated these findings but did find that patients taking cinacalcet had a significant increase in the rate of nausea, vomiting, and hypocalcemia, suggesting that the potential risks associated with cinacalcet use in ESRD patients may outweigh the benefits.39 These clinical uncertainties further bring into question the costs of cinacalcet treatment. Currently the US spends $260 million annually on cinacalcet, accounting for the largest single drug cost in dialysis patients.40 Despite maximal medical interventions, surgical parathyroidectomy is still required for many patients.41
Indications for Surgical Treatment
As stated in the Clinical Practice Guidelines for Bone Metabolism and Disease in Chronic Kidney Disease, published in 2003 by the Kidney Disease Outcomes Quality Initiative, the indications for parathyroidectomy are not well defined. High-quality studies are currently lacking to evaluate which patients might benefit from parathyroidectomy. In lieu of such data, the National Kidney Foundation recommends that the criteria in the Sidebar: Indications for Consideration for Parathyroidectomy be used to merit referral to an experienced surgeon for evaluation.42
Indications for Consideration for Parathyroidectomy.
| Medical management of rHPT > 6 months with Hypercalcemia or hyperphosphatemia |
| PTH > 800 pg/mL |
| Calciphylaxis with documented elevated PTH levels |
| Osteoporosis (T-score > 2.5 SD below mean), pathologic bone fracture |
| Symptoms/signs |
| Pruritus |
| Bone pain |
| Severe vascular calcifications |
| Myopathy |
PTH = parathyroid hormone; rHPT = renal hyperparathyroidism, SD = standard deviation.
The three most common surgical procedures used in the treatment of rHPT are total parathyroidectomy (TPX) alone, TPX with auto-transplantation, and subtotal parathyroidectomy.21 Each of these procedures may be accompanied by a bilateral cervical thymectomy to minimize the risk of recurrence.43
TPX involves identification and removal of all parathyroid glands. This operation may be associated with the lowest rate of recurrent hyperparathyroidism.44 The clear disadvantage of TPX is permanent hypoparathyroidism, and patients undergoing TPX require lifelong calcium and vitamin D replacement. In TPX with autotransplantation, all 4 glands are removed, followed by autologous reimplantation of 20 mg to 70 mg of the most normal-appearing gland into the sternocleidomastoid muscle, pectoralis major muscle, or forearm brachioradialis muscle. This implant typically takes 3 to 4 weeks to revascularize and resume function. The advantage of removal and reimplantation of parathyroid tissue into an ectopic site is ease of access in the event of recurrence and reoperation. This avoids the morbidity associated with re-exploration of the neck. Subtotal parathyroidectomy entails removal of 3½ parathyroid glands, leaving the remaining partial gland intact in its original anatomic location. Subtotal parathyroidectomy has the advantage of minimizing the period of postoperative hypoparathyroidism and therefore likely shortens a patient’s hospital course, but it requires reoperation in the neck in the event of a recurrence. This may be associated with an increased risk of injury to the recurrent laryngeal nerve. All 3 operations are accepted surgical treatment options for rHPT, and each is associated with specific advantages and disadvantages.45
Successful parathyroidectomy can dramatically improve symptoms, including bone pain, arthralgia, muscle weakness, and psychological disturbances.45,46 Biopsy-proven changes in trabecular bone mineral content and accelerated bone formation have been demonstrated within 1 week after surgery.47 Parathyroidectomy is associated with a 30-day postoperative mortality of 3.1% throughout the US.48 Other risks of surgery include recurrent laryngeal nerve injury (< 2%) and hematoma requiring re-exploration (< 1 %).
Several studies have suggested a survival benefit from parathyroidectomy in the treatment of rHPT, including significant reductions in the incidence of major cardiovascular events and all-cause mortality.49,50 Long-term relative risks of death are reduced by 10% to 15%, and long-term survival is improved compared with those not undergoing surgery.50 Parathyroidectomy is effective in improving hemoglobin levels for ESRD-associated anemia,51 and it has beneficial effects on the immune system and overall nutrition.52 Parathyroidectomy has also been shown to be more cost-effective than cinacalcet in nearly all dialysis patient subgroups, with the exception of those with high operative mortality risk, patients remaining on dialysis for less than 7 months, and/or individuals expecting kidney transplant quickly.
CONCLUSION
rHPT is a common complication of CKD that stems from hypocalcemia, reduced bioactivity of vitamin D, and elevated levels of FGF-23. rHPT leads to a host of bone and cardiovascular problems that ultimately can cause fractures, decreased quality of life, and an increased risk of death. A range of nonsurgical options are available, including initiating a low phosphorus diet, phosphate binders, vitamin D analogs, and calcimimetic agents, but unfortunately the data on the efficacy of these treatments at improving overall and cardiovascular mortality are mixed. Some patients require parathyroidectomy, which may improve symptoms and reduce cardiovascular and overall mortality, but it carries the expected risks of surgery.
Acknowledgments
Mary Corrado, ELS, provided editorial assistance.
Footnotes
Author Contributions
Noah K Yuen, MD, provided study conception and design and participated in analysis and interpretation of data and writing the manuscript. Shubha Ananthakrishnan, MD, participated in writing the manuscript and in critical revision of the manuscript. Michael J Campbell, MD, provided study conception and design and participated in analysis and interpretation of data, writing the manuscript, and the decision to submit for publication.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
A Small Organ Hardly as Big as a Hemp Seed
About three years ago I found on the thyroid gland … a small organ, hardly as big as a hemp seed, which was enclosed in the same connective tissue capsule as the thyroid, but could be distinguished therefrom by a lighter color. A superficial examination revealed an organ of totally different structure from that of the thyroid, and with a very rich vascularity. … [I] suggest the use of the name Glandulae parathyreoidea; a name in which the characteristic of being bye-glands to the thyroid is expressed.
— Ivar Victor Sandström, 1852–1889, Swedish physician
References
- 1.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 suppl 1):S1–S266. [PubMed] [Google Scholar]
- 2.US Renal Data System. USRDS 2015 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2015. [Google Scholar]
- 3.Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007 Jan;71(1):31–8. doi: 10.1038/sj.ki.5002009. [DOI] [PubMed] [Google Scholar]
- 4.De Boer IH, Gorodetskaya I, Young B, Hsu CY, Chertow GM. The severity of secondary hyperparathyroidism in chronic renal insufficiency is GFR-dependent, race-dependent, and associated with cardiovascular disease. J Am Soc Nephrol. 2002;13(11):2762–9. doi: 10.1097/01.asn.0000034202.91413.eb. [DOI] [PubMed] [Google Scholar]
- 5.Fellner SK, Lang RM, Neumann A, Bushinsky DA, Borow KM. Parathyroid hormone and myocardial performance in dialysis patients. Am J Kidney Dis. 1991 Sep;18(3):320–5. doi: 10.1016/s0272-6386(12)80090-4. [DOI] [PubMed] [Google Scholar]
- 6.Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004 Aug;15(8):2208–18. doi: 10.1097/01.ASN.0000133041.27682.A2. [DOI] [PubMed] [Google Scholar]
- 7.Kalantar-Zadeh K, Kuwae N, Regidor DL, et al. Survival predictability of time-varying indicators of bone disease in maintenance hemodialysis patients. Kidney Int. 2006 Aug;70(4):771–80. doi: 10.1038/sj.ki.5001514. [DOI] [PubMed] [Google Scholar]
- 8.Ganesh SK, Stack AG, Levin NW, Hulbert-Shearon T, Port FK. Association of elevated serum PO(4), Ca x PO(4) product, and parathyroid hormone with cardiac mortality risk in chronic hemodialysis patients. J Am Soc Nephrol. 2001 Oct;12(10):2131–8. doi: 10.1681/ASN.V12102131. [DOI] [PubMed] [Google Scholar]
- 9.Lee A, Belozeroff V, Song X, Diakun D, Goodman W. Costs of treatment and clinical events for secondary hyperparathyroidism. Am J Pharm Benefits. 2013;5(2):e24–e35. [Google Scholar]
- 10.Martin KJ, Gonzalez EA. Metabolic bone disease in chronic kidney disease. J Am Soc Nephrol. 2007 Mar;18(3):875–85. doi: 10.1681/ASN.2006070771. . [DOI] [PubMed] [Google Scholar]
- 11.Kerby J, Rue LW, Blair H, Hudson S, Sellers MT, Diethelm AG. Operative treatment of tertiary hyperparathyroidism: a single-center experience. Ann Surg. 1998 Jun;227(6):878–86. doi: 10.1097/00000658-199806000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilgo M, Pirsch J, Warner T, Starling JR. Tertiary hyperparathyroidism after renal transplantation: surgical strategy. Surgery. 1998 Oct;124(4):677–83. doi: 10.1067/msy.1998.91483. discussion 683–4. [DOI] [PubMed] [Google Scholar]
- 13.Li X, Qin L, Bergenstock M, Beyelock LM, Novack DV, Partridge NC. Parathyroid hormone stimulates osteoblastic expression of MCP-1 to recruit and increase the fusion of pre/osteoclasts. J Biol Chem. 2007 Nov 9;282(45):3098–106. doi: 10.1074/jbc.M611781200. [DOI] [PubMed] [Google Scholar]
- 14.Slaiba W, El-Haddad B. Secondary hyperparathyroidism: pathophysiology and treatment. J Am Board Fam Med. 2009 Sep-Oct;22(5):574–81. doi: 10.3122/jabfm.2009.05.090026. [DOI] [PubMed] [Google Scholar]
- 15.Weinman EJ, Lederer ED. NHERF-1 and the regulation of renal phosphate reabsoption: a tale of three hormones. Am J Physiol Renal Physiol. 2012 Aug;303(3):F321–7. doi: 10.1152/ajprenal.00093.2012. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quarles LD. Role of FGF23 in vitamin D and phosphate metabolism: implications in chronic kidney disease. Exp Cell Res. 2012 May 15;318(9):1040–8. doi: 10.1016/j.yexcr.2012.02.027. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int Jan. 2007;71(1):31–8. doi: 10.1038/sj.ki.5002009. [DOI] [PubMed] [Google Scholar]
- 18.Madorin C, Owen RP, Fraser WD, et al. The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol. 2012 Jun;269(6):1565–76. doi: 10.1007/s00405-011-1833-2. . [DOI] [PubMed] [Google Scholar]
- 19.Tominaga Y, Tanaka Y, Sato K, Nagasaka T, Takagi H. Histopathology, pathophysiology, and indications for surgical treatment of renal hyperparathyroidism. Semin Surg Oncol. 1997 Mar-Apr;13(2):78–86. doi: 10.1002/(sici)1098-2388(199703/04)13:2<78::aid-ssu3>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 20.Moe S, Drueke T, Cunningham J, et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006 Jun;69(11):1945–53. doi: 10.1038/sj.ki.5000414. [DOI] [PubMed] [Google Scholar]
- 21.Andress DL. Adynamic bone in patients with chronic kidney disease. Kidney Int. 2008 Jun;73(12):1345–54. doi: 10.1038/ki.2008.60. . [DOI] [PubMed] [Google Scholar]
- 22.Pitt S, Sipple R, Chen H. Secondary and tertiary hyperparathyroidism, state of the art surgical management. Surg Clin North Am. 2009 Oct;89(5):1227–39. doi: 10.1016/j.suc.2009.06.011. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodman WG. The consequences of uncontrolled secondary hyperparathyroidism and its treatment in chronic kidney disease. Semin Dial. 2004 May-Jun;17(3):209–16. doi: 10.1111/j.0894-0959.2004.17308.x. [DOI] [PubMed] [Google Scholar]
- 24.Wilkieson TJ, Rahman MO, Gangji AS, et al. Coronary artery calcification, cardiovascular events, and death: a prospective cohort study of incident patients on hemodialysis. Can J Kidney Health Dis. 2015 Aug 12;2:29. doi: 10.1186/s40697-015-0065-6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazhar A, Johnson R, Gillen D, et al. Risk factors and mortality associated with calciphylaxis in end-stage renal disease. Kidney Int. 2001 Jul;60(1):324–32. doi: 10.1046/j.1523-1755.2001.00803.x. [DOI] [PubMed] [Google Scholar]
- 26.Cohen RA, Parikh SM. Images in clinical medicine. Calcinosis associated with renal failure. N Engl J Med. 2007 Dec 20;357(25):2615. doi: 10.1056/NEJMicm067693. [DOI] [PubMed] [Google Scholar]
- 27.Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD-MBD) Kidney Int Suppl. 2009 Aug;76(113):S1–130. doi: 10.1038/ki.2009.188. . [DOI] [PubMed] [Google Scholar]
- 28.Slatopolsky EA, Burke SK, Dillon MA. RenaGel, a nonabsorbed calcium- and aluminum-free phosphate binder, lowers serum phosphorus and parathyroid hormone. The RenaGel Study Group. Kidney Int. 1999 Jan;55(1):299–307. doi: 10.1046/j.1523-1755.1999.00240.x. [DOI] [PubMed] [Google Scholar]
- 29.Isakova T, Gutierrez OM, Chang Y, et al. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol. 2009 Feb;20(2):388–96. doi: 10.1681/ASN.2008060609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cerny S, Kunzendorf U. Images in clinical medicine. Radiographic appearance of lanthanum. N Engl J Med. 2006 Sep 14;355(11):1160. doi: 10.1056/NEJMicm050535. [DOI] [PubMed] [Google Scholar]
- 31.Costa AF, dos Reis LM, Ribeiro MC, Moysés RM, Jorgetti V. Effects of calcitriol on parathyroid function and on bone remodeling in secondary hyperparathyroidism. Nephrol Dial Transplant. 2003 Apr;18(4):743–49. doi: 10.1093/ndt/gfg017. [DOI] [PubMed] [Google Scholar]
- 32.Gallieni M, Brancaccio D, Padovese P, et al. Low-dose intravenous calcitriol treatment of secondary hyperparathyroidism in hemodialysis patients. Italian Group for the Study of Intravenous Calcitriol. Kidney Int. 1992 Nov;42(5):1191–8. doi: 10.1038/ki.1992.404. [DOI] [PubMed] [Google Scholar]
- 33.Martin KJ, Gonzalez EA, Gellens M, Hamm LL, Abboud H, Lindberg J. 19-Nor-1-alpha-25-dihydroxyvitamin D2 (Paricalcitol) safely and effectively reduces the levels of intact parathyroid hormone in patients on hemodialysis. J Am Soc Nephrol. 1998 Aug;9(8):1427–32. doi: 10.1681/ASN.V981427. [DOI] [PubMed] [Google Scholar]
- 34.Andress DL, Norris KC, Coburn JW, Slatopolsky EA, Sherrard DJ. Intravenous calcitriol in the treatment of refractory osteitis fibrosa of chronic renal failure. N Engl J Med. 1989 Aug;321(5):274–9. doi: 10.1056/NEJM198908033210502. [DOI] [PubMed] [Google Scholar]
- 35.Palmer SC, McGregor DO, Macaskill P, Craig JC, Elder GJ, Strippoli GE. Meta-analysis: vitamin D compounds in chronic kidney disease. Ann Intern Med. 2007 Dec 18;147(12):840–53. doi: 10.7326/0003-4819-147-12-200712180-00004. [DOI] [PubMed] [Google Scholar]
- 36.Cunningham J, Danese M, Olson K, Klassen P, Chertow GM. Effects of the calcimimetic cinacalcet HCl on cardiovascular disease, fracture, and health-related quality of life in secondary hyperparathyroidism. Kidney Int. 2005 Oct;68(4):1793–800. doi: 10.1111/j.1523-1755.2005.00596.x. [DOI] [PubMed] [Google Scholar]
- 37.Block GA, Martin KJ, De Francisco AL, et al. Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis. N Engl J Med. 2004 Apr 8;350(15):1516–25. doi: 10.1056/NEJMoa031633. [DOI] [PubMed] [Google Scholar]
- 38.EVOLVE Trial Inestigators. Chertow GM, Block GA, Correa-Rotter R, et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012 Dec 27;367(26):2482–94. doi: 10.1056/NEJMoa1205624. . [DOI] [PubMed] [Google Scholar]
- 39.Ballinger AE, Palmer SC, Nistor I, Craig JC, Strippoli GF. Calcimimetics for secondary hyperparathyroidism in chronic kidney disease patients. Cochrane Database Syst Rev. 2014;12:CD006254. doi: 10.1002/14651858.CD006254.pub2. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urologic, and Hematologic Diseases . 2012 USRDS annual data report volume one: atlas of chronic kidney disease in the United States. Bethesda, MD: National Institutes of Health; 2012. [Google Scholar]
- 41.Li S, Chen Y, Peng Y, Foley RN, St Peter WL. Trends in parathyroidectomy rates in US hemodialysis patients from 1992 to 2007. Am J Kidney Dis. 2007 Apr;57(4):602–11. doi: 10.1053/j.ajkd.2010.10.041. . [DOI] [PubMed] [Google Scholar]
- 42.National Kidney Foundation K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003 Oct;42(4 Suppl 3):S1–201. [PubMed] [Google Scholar]
- 43.Schneider R, Bartsch DK, Schlosser K. Relevance of bilateral cervical thymectomy in patients with renal hyperparathyroidism: analysis of 161 patients undergoing reoperative parathyroidectomy. World J Surg. 2013 Sep;37(9):2155–61. doi: 10.1007/s00268-013-2091-9. . [DOI] [PubMed] [Google Scholar]
- 44.Higgins RM, Richardson AJ, Ratcliffe PJ, Woods CG, Oliver DO, Morris PJ. Total parathyroidectomy alone or with autograft for renal hyperparathyroidism? Q J Med. 1991 Apr;79(288):323–32. [PubMed] [Google Scholar]
- 45.Dumasius V, Angelos P. Parathyroid surgery in renal failure patients. Otolaryngol Clin North Am. 2010 Apr;43(2):433–40. x–xi. doi: 10.1016/j.otc.2010.01.010. . [DOI] [PubMed] [Google Scholar]
- 46.Tominaga Y. Surgical management of secondary hyperparathyroidism in uremia. Am J Med Sci. 1999 Jun;317(6):390–7. doi: 10.1097/00000441-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 47.Yajima A, Ogawa Y, Takahashi HF, Tominaga Y, Inou T, Otsubo O. Changes of bone remodeling immediately after parathyroidectomy for secondary hyperparathyroidism. Am J Kidney Dis. 2003 Oct;42(4):729–38. doi: 10.1016/s0272-6386(03)00909-0. [DOI] [PubMed] [Google Scholar]
- 48.Kestenbaum B, Andress DL, Schwartz SM, et al. Survival following parathyroidectomy among United States dialysis patients. Kidney Int. 2004 Nov;66(5):2010–6. doi: 10.1111/j.1523-1755.2004.00972.x. [DOI] [PubMed] [Google Scholar]
- 49.Costa-Hong V, Jorgetti V, Gowdak LHW, Moyses RM, Krieger EM, De Lima JJ. Parathyroidectomy reduces cardiovascular events and mortality in renal hyperparathyroidism. Surgery. 2007 Nov;142(5):699–703. doi: 10.1016/j.surg.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 50.Sharma J, Raggi P, Kutner N, et al. Improved long-term survival of dialysis patients after near-total parathyroidectomy. J Am Coll Surg. 2012 Apr;214(4):400–7. doi: 10.1016/j.jamcollsurg.2011.12.046. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chow TL, Chan TT, Ho YW, Lam SH. Improvement of anemia after parathyroidectomy in Chinese patients with renal failure undergoing long-term dialysis. Arch Surg. 2007 Jul;142(7):644–8. doi: 10.1001/archsurg.142.7.644. [DOI] [PubMed] [Google Scholar]
- 52.Yasunaga C, Nakamoto M, Matsuo K, Nishihara G, Yoshida T, Goya T. Effects of a parathyroidectomy on the immune system and nutritional condition in chronic dialysis patients with secondary hyperparathyroidism. Am J Surg. 1999 Oct;78(4):332–6. doi: 10.1016/s0002-9610(99)00194-4. [DOI] [PubMed] [Google Scholar]