Abstract
Introduction:
Epithelioid hemangioendothelioma (EHE) is a family of blood vessel tumors originating in blood vessels, bone, brain, kidney, liver, and lung. EHE is more common in women, and chemotherapy, radiation, and surgery have brought few successes.
Case presentation:
We present a case of a 28-year-old woman whose EHE recurred during pregnancy, suggesting hormonal involvement. We conducted a systematic review to provide analysis and interpretation of the potential significance of her disease recurring, with fatal outcome, during pregnancy.
Discussion:
Very little research has explored the use of individual hormonal markers. Strongly positive expression of placenta growth factor (PlGF) and 17-beta estradiol receptors have been reported. Expression of PlGF is noteworthy in our case, in that our patient’s disease quickly and dramatically flared in the 25th week of pregnancy, near the peak in maternal PlGF production. PlGF binds to vascular endothelial growth factor-1 (VEGF-1), and PlGF may accelerate VEGF-induced angiogenesis. Taken together, these factors may explain our patient’s EHE recurrence and rapid flare-up during pregnancy. Treatment of EHE with VEGF inhibition, potentially in combination with other antiangiogenic and tumor-inhibiting therapies such as lenalidomide, thalidomide, sorafenib, and sunitinib, may also hold promise.
INTRODUCTION
Epithelioid hemangioendothelioma (EHE) is a family of vascular tumors, originating in the endothelium and sharing clinical characteristics with both angiosarcoma and benign hemangioma. EHE was first identified in 19821 and is extremely rare, with an incidence rate of 0.1 per 100,000, and fewer than 200 cases ever reported in the medical literature.2 Because there is limited research on prognosis, a layperson registry has been established. The International Hemangioendothioma, Epithelioid Hemangioendothelioma, and Related Vascular Disorders Support Group has tracked more than 260 patients.3
The clinical presentation of EHE is quite varied; it can originate in bone, brain, kidney, liver, lung, and vascular and other soft tissues. Diagnosis is sometimes delayed owing to uncertainty about correct pathologic classification, which can significantly worsen prognosis.4 Little is known about prognostic factors for patients with EHE, although recent work has identified genetic alterations involving activation of the ROS1 receptor tyrosine kinase, which for other cancers has led to effective therapies working through ROS1 inhibition.5
Two case series have described the prognosis of patients with hepatic EHE. In a series from China (N = 33), survival was longer in patients younger than age 47 years (hazard ratio, 7.0; p = 0.035), in those without symptoms (hazard ratio, 86.5; p = 0.001), and in those with serum cancer antigen 19-9 below 37 units/mL (hazard ratio, 5.0; p = 0.018).6 In a series from the United Kingdom (N = 50), patients with bilateral hepatic disease had shorter 5-year survival (51%) compared with those with unilateral disease (81%), although the study size was too small to show a significant difference (p = 0.1). There was additionally nonsignificant lower 5-year survival in meta-static (69%) compared with localized (78.3%) disease (p = 0.7). Treatment with any chemotherapy decreased 5-year survival, compared with no chemotherapy (43.6% vs 82.9%; p = 0.02).7
Diagnostic approaches to EHE include computed tomography (CT),8 magnetic resonance imaging,9,10 CT and magnetic resonance imaging,9 and serial bone scintigraphy.11 (18)F-fluorodeoxyglucose-positron emission tomography with strong (18)F-fluorodeoxyglucose uptake has been used12 but is limited by lack of correlation between lesion size and maximum standardized uptake value.13
Little is known about efficacy of therapy because the low incidence of EHE precludes conduct of human clinical trials. Options currently include chemotherapy, radiation, hormone therapy, thermo-ablation, and surgery, although most do not change the usually poor prognosis of a diagnosis with EHE. In patients with primary hepatic EHE, overall survival is no different following liver resection or transcatheter arterial chemoembolization (p = 0.50).6 Although patients with hepatic EHE have longer median survival compared with those with other hepatic vascular tumors, in these patients surgical resection does not improve survival.14
Development and testing of newer therapies based on vascular endothelial growth factor (VEGF) inhibition is supported by recent studies showing positive expression of VEGF receptor in biopsied lesions.15,16 Additional case reports of success with lenalidomide,17 thalidomide,2 sorafenib (possessing both antiangiogenic and antiproliferative activity),18 and sunitinib19 suggest other targeted molecular therapies may also hold promise.
The current case report documents diagnosis of recurrent EHE in a pregnant woman and discusses the case in the context of a systematic review of the current literature. This report was prepared in accordance with the CARE (CAse REport) guidelines.20
CASE PRESENTATION
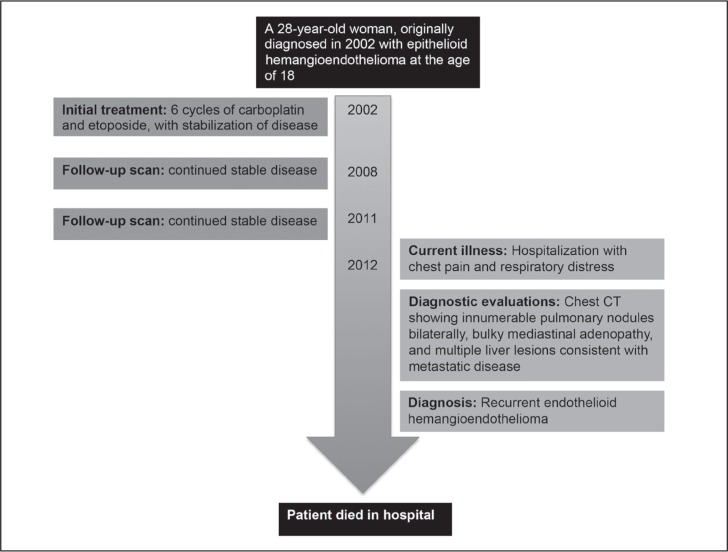
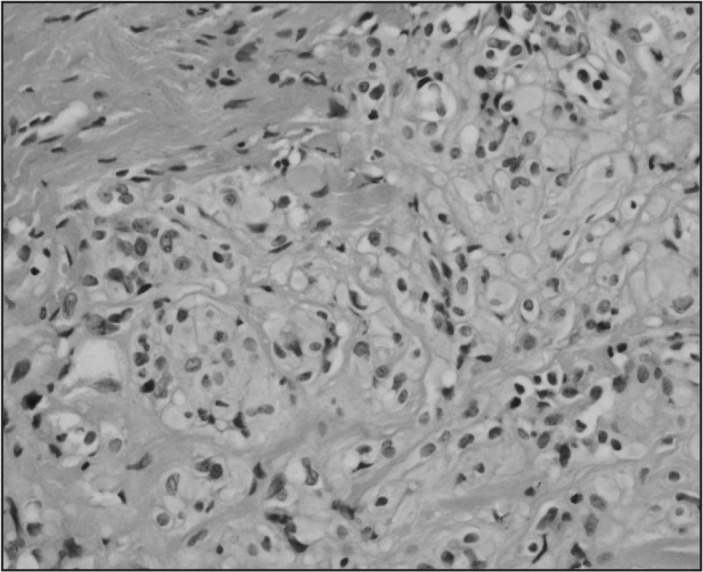
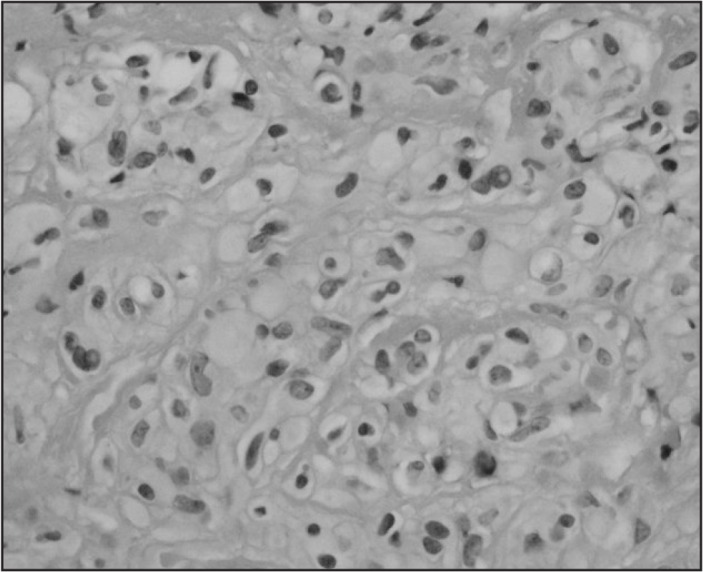
We report a case of a 28-year-old woman originally diagnosed with EHE in 2002, at age 18 years. CT-guided biopsy of 1 of her liver lesions revealed EHE based on hematoxylin/eosin and immunohistochemical stains (Figures 1–4). Repeated CT of her chest, abdomen, and pelvis 3 months later showed progression of disease. At that time she underwent 6 cycles of carboplatin and etoposide with stabilization of disease; however, significant chest pain remained, requiring high doses of opiates. She received 1 dose of interferon, which was not tolerated. The patient was then followed up with serial CT scan showing stable disease through 2011 (Figures 5 and 6).
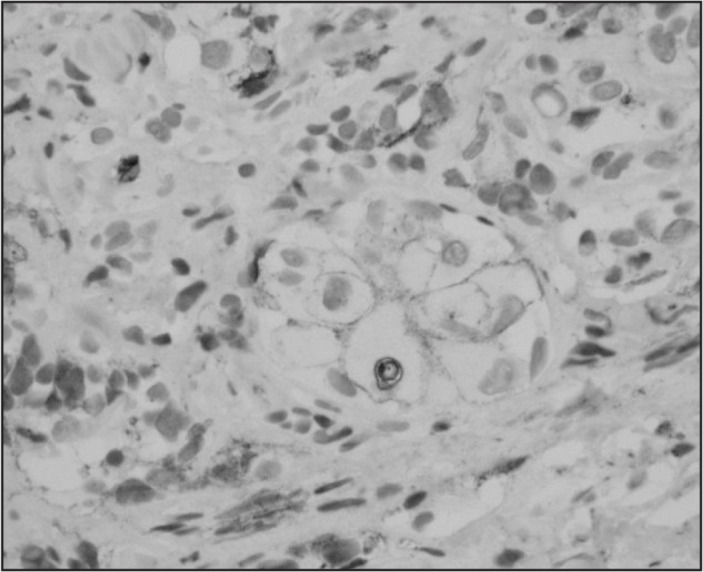
Figure 1.
Hematoxylin/eosin stain showing epithelioid cells with cytoplasmic vacuoles (magnification ×400).
Figure 2.
Hematoxylin/eosin stain showing epithelioid cells with cytoplasmic vacuoles (magnification ×600).
Figure 3.
Immunohistochemical stain positive for vascular marker CD31 (magnification ×600).
Figure 4.
Immunohistochemical stain positive for vascular marker CD34 (magnification ×600).
Figure 5.

Computed tomography angiography of the chest, showing stable disease in 2008.
Figure 6.

Computed tomography angiography of the chest, showing stable disease in 2011.
In 2012, the patient presented to the Emergency Department with chest pain and in acute respiratory distress. A posterior-anterior/lateral chest radiograph revealed multiple pulmonary nodules bilaterally, confirmed as “innumerable” by chest CT, along with bulky mediastinal adenopathy and multiple liver lesions consistent with metastatic disease (Figure 7).
Figure 7.
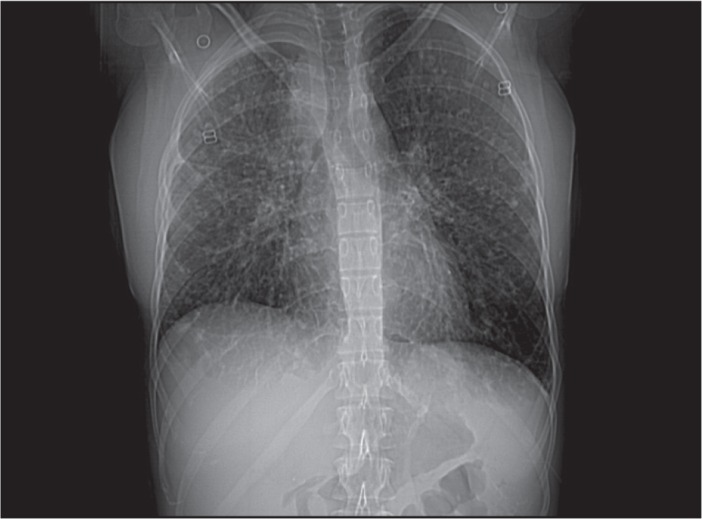
Computed tomography angiography of the chest, following disease recurrence in 2012.
In mid-2012, the patient presented with diffuse joint pain 6 months into her first pregnancy, and went into labor at 25 weeks. The baby was delivered and died 8 days later. The patient’s pain then continued to escalate and she developed severe cough. Repeat CT scan of her chest, abdomen, and pelvis revealed significant progression of disease, especially in the lungs and mediastinum. Biopsy of mediastinal adenopathy confirmed recurrent EHE, and the diffuse nature of disease precluded surgery.
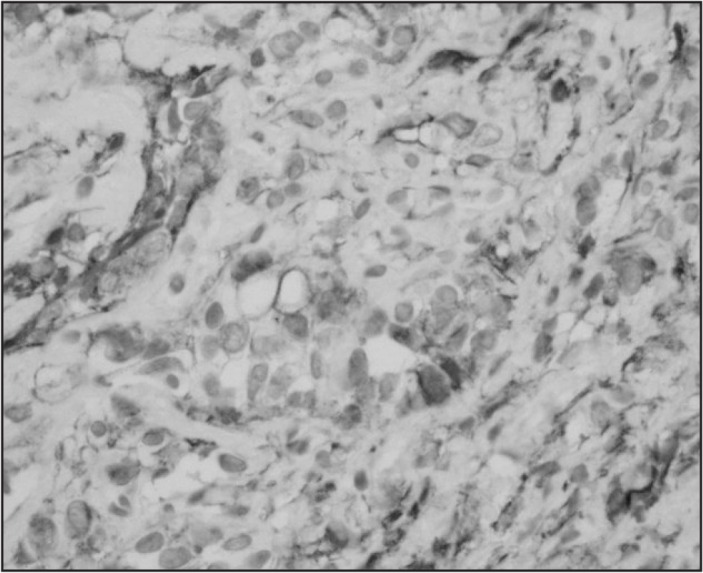
The patient’s diffuse joint and bone pain continued to worsen, resulting in hospitalization for pain control. Bone scan was consistent with hypertrophic osteoarthropathy. During this time her respiratory status continued to worsen: chest CT revealed compression of the right upper lobe bronchus and right pleural effusion. A right-sided chest tube was inserted with drainage of a large amount of pleural fluid and palliative radiation to the mediastinal adenopathy was started. Unfortunately the patient’s respiratory status continued to decline from progressive disease as well as pneumonia. She was intubated; her condition continued to decline; she was placed on comfort measures, and she subsequently died. A timeline showing progression of the case is provided in Figure 8.
Figure 8.
Timeline of the patient’s case.
CT = computed tomography scan.
DISCUSSION
Despite numerous publications, EHE remains a little-understood disease of poor prognosis. In the case of localized disease, prompt surgical resection appears to confer a survival advantage. Improvements in early clinical identification of suspected lesions may be accelerated by further research on the integration of tumor marker and/or hormonal testing.
In Table 1 we present results of a systematic search of treatment outcomes published since January 2011. Tumor marker expression in EHE has been reported for endothelial markers (CD31, CD34, and factor VIII-related antigen),21 VEGF and VEGF receptor 2,15 and strong expression of CD31 and vimentin.12 Errani et al22,23 reported that WWTR1-CAMTA1 fusion is a genetic hallmark of EHE, regardless of site of origin; they also used reverse transcription-polymerase chain reaction and gene sequencing to ascertain that in multifocal EHE, those multiple sites are monoclonal in nature, and therefore metastatic implants of the same tumor and not simultaneous occurrence of multiple neoplastic clones. Additionally, both CD31 and VEGF are overexpressed in non-small cell lung cancer,24 breast cancer,25 prostate cancer,26 renal cell carcinoma,27 mantle cell lymphoma,28 meningioma,29 pituitary adenomas,30 and uveal melanoma.31
Table 1.
Epithelioid hemangioendothelioma primary tumor sites, first-line therapy, and maximum reported survival with therapy
| Author, year | Primary tumor site | Extent of disease | First-line therapy | Patient(s) | Survival |
|---|---|---|---|---|---|
| Case series | |||||
| Angelini et al,1 2014 | Bone | Unifocal (49%); multifocal (13%) | Wide excision or intralesional surgery | N = 62; men, n = 39; women, n = 23; mean age = 39 years | Survival at 10 years: unifocal, 97%; multifocal, 74% |
| Zheng et al,2 2012 | Brain | Intracranial, with localized extension to bone and muscle | Surgery | 25-year-old man; 44-year-old woman |
9 years |
| Agulnik et al,3 2013 | Multifocal | Metastatic | Bevacizumab | N = 7 | Partial response, n = 2; stable disease, n = 4; progressive disease, n = 1 |
| Wang et al,4 2012 | Liver | Localized and extrahepatic | Liver resection, transcatheter arterial chemoembolization (TACE), resection and TACE, or liver transplantation | N = 33 | Up to 3 years of follow-up |
| Theodosopoulos et al,5 2013 | Intracranial | Metastatic | Surgery | N = 38; men, n = 23; women, n = 15 | 2 months–11 years |
| Case reports | |||||
| Gherman and Fodor,6 2011 | Bone | Localized | Wide surgical excision | 24-year-old man | No local recurrence or metastasis at 2 years |
| Sumrall et al,7 2010 | Brain | Intracranial, localized extension to skull, connective tissue | Lenalidomide | 31-year-old woman | 6 years, stable disease |
| Osawa et al,8 2012 | Carotid artery | Localized | Surgery | 59-year-old man; 14 years after embolization for carotid aneurysm | Rapid death |
| Tolkach et al,9 2012 | Kidney | Metastatic | Sunitinib | 53-year-old man | 3 years, stable disease |
| Harada et al,10 2011 | Liver | Localized | Transcatheter arterial chemoembolization | 83-year-old man | Metastatic recurrence after 3 months |
| Grenader et al,11 2011 | Liver | Localized | Pegylated liposomal doxorubicin | 32-year-old man | 2 years, stable disease with maintenance therapy at time of publication |
| Sangro et al,12 2012 | Liver | Metastatic to lungs | Sorafenib | 22-year-old man | 2 years |
| Salech et al,13 2011 | Liver | Metastatic to lungs | Thalidomide | 40-year-old woman | 9 years, stable disease |
| Mizota et al,14 2011 | Lung | Localized | Bevacizumab | 59-year-old woman | 3 months |
| Iimuro et al,15 2012 | Retroperitoneum | Localized, then distant lymph metastasis months later | Surgical removal of both occurrences | 48-year-old woman | No recurrence at 13 months after resection of metastasis |
| Kerry et al,16 2012 | Spinal region | Multifocal | Endovascular embolization, radiochemotherapy | 25-year-old man | 8 weeks |
| De Palma et al,17 2012 | Vascular | Localized | Surgical removal of entire azygos vein | 47-year-old man | No recurrence at 1 year |
| Wu et al,18 2014 | Vascular | Localized | Surgery | 58-year-old woman | 2 years, stable at time of publication |
| Demir et al,19 2013 | Liver | Parenchymal lesion with metastases to lung | Carboplatin, pharmorubucin | 24-year-old woman | |
| Kiratli et al,20 2013 | Eyelid | Localized | Excisional biopsy | 22-year-old woman | No recurrence at 44 months |
| Pálföldi et al,21 2013 | Lung | Metastatic to bone | Carboplatin, docetaxel, pharmorubucin | 49-year-old woman | Stable disease 1 year after diagnosis |
| Yu et al,22 2013 | Lung | Lung (localized to myocardium) | Carboplatin/etoposide, followed by surgical excision | 39-year-old woman | Alive 14 months after surgery |
Angelini A, Mavrogenis AF, Gambarotti M, Merlino B, Picci P, Ruggieri P. Surgical treatment and results of 62 patients with epithelioid hemangioendothelioma of bone. J Surg Oncol 2014 Jun;109(8):791–7. DOI: http://dx.doi.org/10.1002/jso.23587.
Zheng J, Liu L, Wang J, Wang S, Cao Y, Zhao J. Primary intracranial epithelioid hemangioendothelioma: a low-proliferation tumor exhibiting clinically malignant behavior. J Neurooncol 2012 Oct;110(1):119–27. DOI: http://dx.doi.org/10.1007/s11060-012-0945-x.
Agulnik M, Yarber JL, Okuno SH, et al. An open-label, multicenter, phase II study of bevacizumab for the treatment of angiosarcoma and epithelioid hemangioendotheliomas. Ann Oncol 2013 Jan;24(1):257–63. DOI: http://dx.doi.org/10.1093/annonc/mds237.
Wang LR, Zhou JM, Zhao YM, et al. Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg 2012 Nov;36(11):2677–83. DOI: http://dx.doi.org/10.1007/s00268-012-1714-x.
Theodosopoulos T, Dellaportas D, Tsangkas A, et al. Clinicopathological features and management of hepatic vascular tumors. A 20-year experience in a Greek University Hospital. J BUON 2013 Oct–Dec;18(4):1026–31.
Gherman CD, Fodor D. Epithelioid hemangioendothelioma of the forearm with radius involvement. Case report. Diagn Pathol 2011 Dec 6;6:120. DOI: http://dx.doi.org/10.1186/1746-1596-6-120.
Sumrall A, Fredericks R, Berthold A, Shumaker G. Lenalidomide stops progression of multifocal epithelioid hemangioendothelioma including intracranial disease. J Neurooncol 2010 Apr;97(2):275–7. DOI: http://dx.doi.org/10.1007/s11060-009-0017-z.
Osawa S, Saito A, Shimizu H, Ogawa T, Watanabe M, Tominaga T. A case of intravascular epithelioid hemangioendothelioma occurring 14 years after coil embolization for an extracranial internal carotid artery aneurysm. J Vasc Surg 2012 Jan;55(1):230–3. DOI: http://dx.doi.org/10.1016/j.jvs.2011.06.108.
Tolkach Y, Petrov S, Lerut E, Van Poppel H. Epithelioid hemangioendothelioma of the kidney treated with sunitinib. Onkologie 2012;35(6):376–8. DOI: http://dx.doi.org/10.1159/000338944.
Harada J, Yoshida H, Ueda J, et al. Malignant hepatic epithelioid hemangioendothelioma with abdominal pain due to rapid progression. J Nippon Med Sch 2011;78(4):246–51. DOI: http://dx.doi.org/10.1272/jnms.78.246.
Grenader T, Vernea F, Reinus C, Gabizon A. Malignant epithelioid hemangioendothelioma of the liver successfully treated with pegylated liposomal doxorubicin. J Clin Oncol 2011 Sep 1;29(25):e722–4. DOI: http://dx.doi.org/10.1200/jco.2011.35.5891.
Sangro B, Iñarrairaegui M, Fernández-Ros N. Malignant epithelioid hemangioendothelioma of the liver successfully treated with Sorafenib. Rare Tumors 2012 Apr 12;4(2):e34. DOI: http://dx.doi.org/10.4081/rt.2012.e34.
Salech F, Valderrama S, Nervi B, et al. Thalidomide for the treatment of metastatic hepatic epithelioid hemangioendothelioma: a case report with a long term follow-up. Ann Hepatol 2011 Jan–Mar;10(1):99–102.
Mizota A, Shitara K, Fukui T. Bevacizumab chemotherapy for pulmonary epithelioid hemangioendothelioma with severe dyspnea. J Thorac Oncol 2011 Mar;6(3):651–2. DOI: http://dx.doi.org/10.1097/jto.0b013e31820b9e23.
Iimuro Y, Nakai N, Asano Y, et al. Primary epithelioid hemangioendothelioma of the retroperitoneum: report of a case. Surg Today 2012 Oct;42(10):1026–31. DOI: http://dx.doi.org/10.1007/s00595-012-0173-1.
Kerry G, Marx O, Kraus D, et al. Multifocal epithelioid hemangioendothelioma derived from the spine region: case report and literature review. Case Rep Oncol 2012 Jan;5(1):91–8. DOI: http://dx.doi.org/10.1159/000336947.
De Palma A, Pagliarulo V, Ardò N, Loizzi D. Surgical treatment of a rare case of epithelioid hemangioendothelioma of the azygos vein. Interact Cardiovasc Thorac Surg 2012 Jan;14(1):91–3. DOI: http://dx.doi.org/10.1093/icvts/ivr064.
Wu XN, Chen MJ, Li DQ, Hu JG, Yu FL. Pulmonary artery pseudoaneurysm caused by a rare vascular tumor: epithelioid hemangioendothelioma. Thorac Cardiovasc Surg 2014 Feb;62(1):92–4. DOI: http://dx.doi.org/10.1055/s-0031-1299588.
Demir L, Can A, Oztop R, et al. Malignant epithelioid hemangioendothelioma progressing after chemotherapy and Interferon treatment: a case presentation and a brief review of the literature. J Cancer Res Ther 2013 Jan–Mar;9(1):125–7. DOI: http://dx.doi.org/10.4103/0973-1482.110386.
Kiratli H, Tarlan B, Ruacan S. Epitheloid hemangioendothelioma of the palpebral lobe of the lacrimal gland. Orbit 2013 Apr;32(2):120–3. DOI: http://dx.doi.org/10.3109/01676830.2013.764443.
Pálföldi R, Radács M, Csada E, et al. Pulmonary epithelioid haemangioendothelioma studies in vitro and in vivo: new diagnostic and treatment methods. In Vivo 2013 Mar–Apr;27(2):221–5.
Yu L, Gu T, Xiu Z, Shi E, Zhao X. Primary pleural epithelioid hemangioendothelioma compressing the myocardium. J Card Surg 2013 May;28(3):266–8. DOI: http://dx.doi.org/10.1111/jocs.12094.
EHE is more common in women, and there are 3 prior case reports of its diagnosis during pregnancy,17 with ours being the fourth. A case report has also been published of successful management of multifocal hepatic infantile hemangioendothelioma with tamoxifen-based therapy.32 Tamoxifen (20 mg daily) was part of the management strategy used for our patient over a 9-day course during her acute disease recurrence.
Very little research has explored the clinical utility of individual hormonal markers in EHE. There was strongly positive expression of placenta growth factor (PlGF) in 1 case,33 positive expression of 17-beta estradiol receptors in only 1 of a series of 5 EHE patients,34 and no estrogen or progesterone receptors in another case.35 Expression of PlGF is noteworthy in our case, in that our patient’s disease quickly and dramatically flared in the 25th week of pregnancy, near the peak in maternal PlGF production. Although in our patient’s case PlGF was not tested, we did note an abnormally low human chorionic gonadotropin level during the second trimester of pregnancy of 23 IU/mL.
A translocation involving PlGF has also been discovered in a case of EHE.15 Furthermore, it is known that there is binding of PlGF to VEGF receptor-1, and that PlGF may influence VEGF-induced angiogenesis,36 which may explain our patient’s rapid disease flare-up.
Although the scarcity of cases impedes rapid progress in histochemical characterization of EHE, a composite picture has begun to emerge that may aid researchers in its early identification, perhaps leading to earlier diagnosis and more definitive treatment. VEGF expression15 and hormonal receptor expression have been reported in EHE. Furthermore, there are multiple reports of successful management of this vascular cancer with antiangiogenic therapy (lenalidomide,17,18 thalidomide,2,37–39 and sorafenib18). We therefore suggest it is possible that combination therapy of EHE with sequenced or concurrent anti-angiogenic, hormonal, and anti-VEGF agents has value as an avenue of future clinical investigation.
Acknowledgments
Mary Corrado, ELS, provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
All Attempts at a Rational Method of Cure
The main part of the science of disease is of a purely descriptive character, a scientific interpretation of facts and a clear insight into the intimate connection subsisting between different phenomena, which may precede all attempts at a rational method of cure, having been attained in a few instances only. … Therapeutic researchers must be regulated in the same manner as pathological. … The more careful tracing of the progress of morbid processes, and the insight into their modes of origin and retrogression, enable us to determine the principles of treatment with greater clearness than formerly.
— Friedrich Theodor von Frerichs, 1819–1885, German pathologist
References
- 1.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer. 1982 Sep 1;50(5):970–81. doi: 10.1002/1097-0142(19820901)50:5<970::aidcncr2820500527>3.0.co;2-z. . [DOI] [PubMed] [Google Scholar]
- 2.Salech F, Valderrama S, Nervi B, et al. Thalidomide for the treatment of metastatic hepatic epithelioid hemangioendothelioma: a case report with a long term follow-up. Ann Hepatol. 2011 Jan-Mar;10(1):99–102. [PubMed] [Google Scholar]
- 3.Lau K, Massad M, Pollak C, et al. Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: insights from an internet registry in the study of a rare cancer. Chest. 2011 Nov;140(5):1312–8. doi: 10.1378/chest.11-0039. . [DOI] [PubMed] [Google Scholar]
- 4.Osawa S, Saito A, Shimizu H, Ogawa T, Watanabe M, Tominaga T. A case of intravascular epithelioid hemangioendothelioma occurring 14 years after coil embolization for an extracranial internal carotid artery aneurysm. J Vasc Surg. 2012 Jan;55(1):230–3. doi: 10.1016/j.jvs.2011.06.108. . [DOI] [PubMed] [Google Scholar]
- 5.Davies KD, Doebele RC. Molecular pathways: ROS1 fusion proteins in cancer. Clin Cancer Res. 2013 Aug 1;19(15):4040–5. doi: 10.1158/1078-0432.ccr-12-2851. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang LR, Zhou JM, Zhao YM, et al. Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg. 2012 Nov;36(11):2677–83. doi: 10.1007/s00268-012-1714-x. . [DOI] [PubMed] [Google Scholar]
- 7.Thomas RM, Aloia TA, Truty MJ, et al. Treatment sequencing strategy for hepatic epithelioid haemangioendothelioma. HPB (Oxford) 2014 Jul;16(7):677–85. doi: 10.1111/hpb.12202. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marchiori E, Hochhegger B, Zanetti G. Optimizing the utility of computed tomography in diagnosing pulmonary epithelioid hemangioendothelioma. Isr Med Assoc J. 2012 Jun;14(6):403. [PubMed] [Google Scholar]
- 9.Lin J, Ji Y. CT and MRI diagnosis of hepatic epithelioid hemangioendothelioma. Hepatobiliary Pancreat Dis Int. 2010 Apr;9(2):154–8. [PubMed] [Google Scholar]
- 10.Rocha Oliveira PC, Alcantara FP, de Souza-Vianna PE, Brito AP. Cerebral epithelioid hemangioendothelioma with thoracic simultaneous involvement: advanced MRI features. Arq Neuropsiquiatr. 2012 Aug;70(8):637–8. doi: 10.1590/s0004-282x2012000800015. . [DOI] [PubMed] [Google Scholar]
- 11.Swainson I, Chan WL, Abbati D. Serial bone scintigraphy in a case of malignant epithelioid hemangioendothelioma. Clin Nucl Med. 2012 Apr;37(4):396–9. doi: 10.1097/rlu.0b013e31823eaac4. . [DOI] [PubMed] [Google Scholar]
- 12.Iimuro Y, Nakai N, Asano Y, et al. Primary epithelioid hemangioendothelioma of the retroperitoneum: report of a case. Surg Today. 2012 Oct;42(10):1026–31. doi: 10.1007/s00595-012-0173-1. . [DOI] [PubMed] [Google Scholar]
- 13.Dong A, Dong H, Wang Y, Gong J, Lu J, Zuo C. MRI and FDG PET/CT findings of hepatic epithelioid hemangioendothelioma. Clin Nucl Med. 2013 Feb;38(2):e66–73. doi: 10.1097/rlu.0b013e318266ceca. . [DOI] [PubMed] [Google Scholar]
- 14.Groeschl RT, Miura JT, Oshima K, Gamblin TC, Turaga KK. Does histology predict outcome for malignant vascular tumors of the liver? J Surg Oncol. 2014 Apr;109(5):483–6. doi: 10.1002/jso.23517. . [DOI] [PubMed] [Google Scholar]
- 15.Matsuzawa S, Kanazawa T, Yamaguchi T, Nishino H, Kawada K, Ichimura K. Case of high-risk epithelioid hemangioendothelioma of the neck. Head Neck. 2013 Oct;35(10):E317–20. doi: 10.1002/hed.23160. . [DOI] [PubMed] [Google Scholar]
- 16.Park MS, Ravi V, Araujo DM. Inhibiting the VEGF-VEGFR pathway in angiosarcoma, epithelioid hemangioendothelioma, and hemangiopericytoma/solitary fibrous tumor. Curr Opin Oncol. 2010 Jul;22(4):351–5. doi: 10.1097/cco.0b013e32833aaad4. . [DOI] [PubMed] [Google Scholar]
- 17.Sumrall A, Fredericks R, Berthold A, Shumaker G. Lenalidomide stops progression of multifocal epithelioid hemangioendothelioma including intracranial disease. J Neurooncol. 2010 Apr;97(2):275–7. doi: 10.1007/s11060-009-0017-z. . [DOI] [PubMed] [Google Scholar]
- 18.Sangro B, Iñarrairaegui M, Fernández-Ros N. Malignant epithelioid hemangioendothelioma of the liver successfully treated with Sorafenib. Rare Tumors. 2012 Apr 12;4(2):e34. doi: 10.4081/rt.2012.e34. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tolkach Y, Petrov S, Lerut E, Van Poppel H. Epithelioid hemangioendothelioma of the kidney treated with sunitinib. Onkologie. 2012;35(6):376–8. doi: 10.1159/000338944. . [DOI] [PubMed] [Google Scholar]
- 20.Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, CARE Group The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014 Jan;67(1):46–51. doi: 10.1016/j.jclinepi.2013.08.003. . [DOI] [PubMed] [Google Scholar]
- 21.Zhao AL, Zhou LX, Li XH. [Hepatic epithelioid hemangioendothelioma in needle biopsy specimens: report of 5 cases with review of literature]. [Article in Chinese] Zhonghua Bing Li Xue Za Zhi. 2011 Jan;40(1):23–6. [PubMed] [Google Scholar]
- 22.Errani C, Sung YS, Zhang L, Healey JH, Antonescu CR. Monoclonality of multifocal epithelioid hemangioendothelioma of the liver by analysis of WWTR1-CAMTA1 breakpoints. Cancer Genet. 2012 Jan-Feb;205(1–2):12–7. doi: 10.1016/j.cancergen.2011.10.008. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Errani C, Zhang L, Sung YS, et al. A novel WWTR1-CAMTA1 gene fusion is a consistent abnormality in epithelioid hemangioendothelioma of different anatomic sites. Genes Chromosomes Cancer. 2011 Aug;50(8):644–53. doi: 10.1002/gcc.20886. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mineo TC, Ambrogi V, Baldi A, et al. Prognostic impact of VEGF, CD31, CD34, and CD105 expression and tumour vessel invasion after radical surgery for IB-IIA non-small cell lung cancer. J Clin Pathol. 2004 Jun;57(6):591–7. doi: 10.1136/jcp.2003.013508. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arihiro K, Kaneko M, Fujii S, Inai K. Loss of CD9 with expression of CD31 and VEGF in breast carcinoma, as predictive factors of lymph node metastasis. Breast Cancer. 1998 Apr 25;5(2):131–8. doi: 10.1007/bf02966685. . [DOI] [PubMed] [Google Scholar]
- 26.Ding GF, Li JC, Xu YF, Sun Y, Tao L. [Correlation between the expression of VEGF-C mRNA, VEGFR-3, CD31 and tumor metastases in Chinese with prostate cancer]. [Article in Chinese] Shi Yan Sheng Wu Xue Bao. 2005 Jun;38(3):257–64. [PubMed] [Google Scholar]
- 27.Yilmazer D, Han U, Onal B. A comparison of the vascular density of VEGF expression with microvascular density determined with CD34 and CD31 staining and conventional prognostic markers in renal cell carcinoma. Int Urol Nephrol. 2007;39(3):691–8. doi: 10.1007/s11255-006-9123-4. . [DOI] [PubMed] [Google Scholar]
- 28.Molinský J, Klánová M, Maswabi B, et al. In vivo growth of mantle cell lymphoma xenografts in immunodeficient mice is positively regulated by VEGF and associated with significant up-regulation of CD31/PECAM1. Folia Biol (Praha) 2013;59(1):26–31. [PubMed] [Google Scholar]
- 29.Lewy-Trenda I, Omulecka A, Janczukowicz J, Papierz W. The morphological analysis of vasculature and angiogenic potential in meningiomas: immunoexpression of CD31 and VEGF antibodies. Folia Neuropathol. 2003;41(3):149–53. [PubMed] [Google Scholar]
- 30.Cristina C, Perez-Millan MI, Luque G, et al. VEGF and CD31 association in pituitary adenomas. Endocr Pathol. 2010 Sep;21(3):154–60. doi: 10.1007/s12022-010-9119-6. . [DOI] [PubMed] [Google Scholar]
- 31.Mouriaux F, Sanschagrin F, Diorio C, et al. Increased HIF-1α expression correlates with cell proliferation and vascular markers CD31 and VEGF-A in uveal melanoma. Invest Ophthalmol Vis Sci. 2014 Mar 4;55(3):1277–83. doi: 10.1167/iovs.13-13345. . [DOI] [PubMed] [Google Scholar]
- 32.Sondhi V, Kurkure PA, Vora T, et al. Successful management of multi-focal hepatic infantile hemangioendothelioma using TACE/surgery followed by maintenance metronomic therapy. BMJ Case Rep. 2012 Mar;8:2012. doi: 10.1136/bcr.12.2011.5456. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haruki T, Arai T, Nakamura H, Nosaka K, Shomori K, Ito H. Pulmonary epithelioid hemangioendothelioma with PlGF expression: report of a case. Thorac Cardiovasc Surg. 2011 Mar;59(2):128–30. doi: 10.1055/s-0030-1250086. . [DOI] [PubMed] [Google Scholar]
- 34.Ohori NP, Yousem SA, Sonmez-Alpan E, Colby TV. Estrogen and progesterone receptors in lymphangioleiomyomatosis, epithelioid hemangioendothelioma, and sclerosing hemangioma of the lung. Am J Clin Pathol. 1991 Oct;96(4):529–35. doi: 10.1093/ajcp/96.4.529. [DOI] [PubMed] [Google Scholar]
- 35.Bollinger BK, Laskin WB, Knight CB. Epithelioid hemangioendothelioma with multiple site involvement. Literature review and observations. Cancer. 1994 Feb;73(3):610–5. doi: 10.1002/1097-0142(19940201)73:3<610::aidcncr2820730318>3.0.co;2-3. . [DOI] [PubMed] [Google Scholar]
- 36.He M, Das K, Blacksin M, Benevenia J, Hameed M. A translocation involving the placental growth factor gene is identified in an epithelioid hemangioendothelioma. Cancer Genet Cytogenet. 2006 Jul 15;168(2):150–4. doi: 10.1016/j.cancergencyto.2006.02.010. . [DOI] [PubMed] [Google Scholar]
- 37.Bölke E, Gripp S, Peiper M, et al. Multifocal epithelioid hemangioendothelioma: case report of a clinical chamaeleon. Eur J Med Res. 2006 Nov 30;11(11):462–6. [PubMed] [Google Scholar]
- 38.Mascarenhas RC, Sanghvi AN, Friedlander L, Geyer SJ, Beasley HS, Van Thiel DH. Thalidomide inhibits the growth and progression of hepatic epithelioid hemangioendothelioma. Oncology. 2004;67(5–6):471–5. doi: 10.1159/000082932. . [DOI] [PubMed] [Google Scholar]
- 39.Raphael C, Hudson E, Williams L, Lester JF, Savage PM. Successful treatment of metastatic hepatic epithelioid hemangioendothelioma with thalidomide: a case report. J Med Case Rep. 2010 Dec 22;4:413. doi: 10.1186/1752-1947-4-413. . [DOI] [PMC free article] [PubMed] [Google Scholar]