Abstract
Nonadherence, or not taking medications as prescribed, to antihypertensive medications has been associated with uncontrolled hypertension. The authors analyzed data from HealthStyles 2010 to assess medication nonadherence among adults with hypertension. The overall prevalence of hypertension was 27.4% and the prevalence of nonadherence was 30.5% among hypertensive adult respondents. Nonadherence rates were highest among younger adults (aged 18–44 years), Hispanics, those who reported lowest annual income (<$25,000), and those who reported depression. The most common reason stated for nonadherence was “I cannot afford the medication” (35.1%). A multivariate logistic regression model showed age, race, and household income to be associated with nonadherence. These findings suggest that certain subgroups are more likely to report barriers to adherence. Interventions to support the management of hypertension should consider the identification of certain at‐risk subgroups and utilize community and clinical evidenced‐based resources to improve long‐term control.
In the United States, nearly one third of adults have hypertension,1 and the estimated combined direct and indirect costs of hypertension in 2010 were more than $46.4 billion.2 The prevalence of awareness among adults with hypertension has increased to nearly 82%.1 Among those who were aware of their hypertension during 2011–2012, nearly 76% were taking antihypertensive medications for blood pressure (BP) control. Of those, 52% had controlled hypertension (<140 mm Hg systolic BP and 90 mm Hg diastolic BP).1 While awareness and treatment of hypertension has improved in recent years, the percentage of patients with controlled hypertension has remained relatively constant.1, 2, 3
Despite frequent interactions with the healthcare system and long‐standing national guidelines for hypertension diagnosis and management, a significant number of diagnosed hypertensive adults remained uncontrolled,3 potentially because of the challenges of medication adherence.4 Adherence is commonly defined as the extent to which a person's behavior complies with medical advice,5 such as lifestyle modifications or a medication regimen. This paper focuses on adherence to medications specifically; therefore, nonadherence in this study was defined as not taking medication as prescribed, missing doses for any reason, deliberately skipping doses, believing that one does not need to take prescribed medication, or being unable to obtain medication because of cost or other barriers. Nonadherence contributes to inadequate BP control, which has been associated with increased mortality rates.6 Examples of barriers to medication adherence include failure to remember to take medication, cost of medication, lack of health insurance, medication side effects, cultural beliefs, patient‐physician relationship, depression and other cognitive dysfunction (working memory, processing speed), low health literacy, comorbidities, patient motivation, coping, financial barriers, and lack of social support.7, 8, 9, 10, 11, 12 Sociodemographic characteristics were found to be associated with differences in medication adherence. Having lower socioeconomic status or being a younger adult, male, or black were associated with poor adherence or nonadherence in earlier studies.9, 10, 13, 14, 15 However, few studies have explored the rationales behind nonadherence, and only regional information was presented in some of the studies.
The Centers for Disease Control and Prevention (CDC) previously reported various barriers to medication adherence among adults with hypertension, using the 2005 HealthStyles survey.16 Because of significant changes in the US healthcare system, this report provides updated information on medication adherence and barriers to adherence.
Methods
Study Population
The Styles surveys, developed by Porter Novelli, are a series of consumer mail panel surveys with data collected by Synovate, Inc. The initial wave, ConsumerStyles, was fielded in April through May 2010. Stratified random sampling was used to generate a list of 20,000 potential respondents who received the ConsumerStyles survey. A total of 10,328 respondents, including a low‐income/minority supplement to ensure adequate representation, completed the ConsumerStyles survey. The second survey, HealthStyles, was sent to 6253 adults aged 18 years and older who completed the ConsumerStyles survey. Responses were received from 4198 (67%) adults. CDC aided with the questionnaire design, and all data were weighted by age, sex, race/ethnicity, income, and household size to replicate proportions in the 2009 Current Population Survey (http://www.census.gov/cps). Data were self‐reported and were provided in aggregate to the CDC.
Definition of Study Measurements
Respondents were chosen for our study if they answered “yes” to the question, “Are you currently taking prescribed medication for your high blood pressure?” Respondents were classified as nonadherent in taking antihypertensive medication if they chose any of the 12 answers listed in question 1: “What are the reasons that you are not taking your blood pressure medication exactly as prescribed?” (Table 1) More than one barrier could be reported. The perceived rationales for the reported barrier, “I do not think I need to control my blood pressure,” were explored using a series of responses related to behavioral changes or perceptions of need (Table 1).
Table 1.
HealthStyles 2010 Survey Questions and Response Choices for the Ascertainment of Nonadherence in Respondents
| Question 1: What are the reasons that you are not taking your blood pressure medication exactly as prescribed? (Check all that apply) | Question 2: If you don't think you need your prescribed medication to control your blood pressure, why not? (Check all that apply) |
|---|---|
| Answers | Answers |
| 1. I forgot to take my medication. | 1. My blood pressure is now controlled so I do not need it. |
| 2. I don't like the side effects from the medication. | 2. I'm taking something else (eg, herbal supplement, natural remedy). |
| 3. I share the medication with someone else. | 3. I'm using an alternative therapy (eg, acupuncture, tai chi, massage). |
| 4. I do not think I need it to control my blood pressure. | 4. I'm trying to lose weight/I have lost weight. |
| 5. I think I should be taking a different medication. | 5. I'm changing my eating habits. |
| 6. I do not know how to take the medication. | 6. I do not know how to take the medication. |
| 7. I cannot afford the medication. | 7. I'm cutting down on salt. |
| 8. The medication is not working. | 8. I'm reducing alcohol. |
| 9. I feel okay without medication. | 9. I'm exercising more. |
| 10. I ran out of medication. | 10. I have quit smoking. |
| 11. Other reason. | 11. Other reason. |
| 12. Don't know. |
In the current study, data from HealthStyles and ConsumerStyles were linked to obtain descriptive information and health behaviors. The descriptive variables included sex, age, race/ethnicity, education, and income. The chronic health conditions included diabetes, congestive heart failure, atrial fibrillation, high cholesterol, cancer (except skin), depression, and migraines. Other risk factors included current smoking status, body mass index (divided into three categories: underweight/normal weight [<25.0 kg/m2], overweight [25.0–29.9 kg/m2], and obese [≥30 kg/m2]), and number of prescription medication(s) taken daily. The health behavior variables were (1) number of primary care visits, (2) time of last BP check, and (3) use of a monitor to check BP at home.
Data Analysis
Univariate associations were examined by selected characteristics for outcomes of nonadherence using the chi‐square or Fisher exact test, as appropriate. Univariate and multivariate logistic regression analysis were performed independently to further examine the association of nonadherence with the selected independent variables listed above. Both unadjusted odds ratios (ORs) and adjusted ORs (AORs) were estimated, along with 95% confidence intervals (CIs). The two‐tailed P values at level .05 were considered significant. All statistical analyses were performed with the statistical software package SAS 9.3 (SAS Institute, Inc, Cary, NC).
Results
Among 4198 adult respondents, 1366 (27.4%) had self‐reported hypertension, and 1180 (23.3%) reported that they were currently taking medication for hypertension. Among the hypertensive adults, 329 (30.5%) reported barriers to taking their antihypertensive medications and were, therefore, classified as nonadherent. Table 2 describes the distribution of the selected characteristics among this population by nonadherence. The percentage of nonadherence did not differ by sex or education level, but did differ by age (from 45.3% aged 18–44 years to 22.1% aged ≥65 years, P=.0009), race/ethnicity (25.4% in whites, 38.4% in blacks, 47.0% in Hispanics; P=.009) and household income (from 41.4% with income <$25,000 to 24.5% with income ≥$60,000, P=.009). Hypertensive adults with depression reported greater nonadherence than those without depression (37.8% vs 26.8%, respectively; P=.02). There were no significant differences in health behaviors between nonadherent and adherent hypertensive adults.
Table 2.
Percentage of Respondents Reporting Nonadherence in Taking High BP Medication, by Selected Characteristics—HealthStyles Survey, 2010
| Characteristic | No. (%) | Nonadherence in Taking BP Medication | ||
|---|---|---|---|---|
| No. | % (95% CI) | P Valuea | ||
| Overall | 1180 | 329 | 30.5 (26.7–34.3) | |
| Demographics | ||||
| Age, y | ||||
| 18–44 | 132 (22.4) | 54 | 45.3 (32.7–57.9) | .0009 |
| 45–64 | 576 (43.0) | 171 | 29.6 (25.5–33.8) | |
| ≥65 | 472 (34.7) | 104 | 22.1 (18.0–26.2) | |
| Sex | ||||
| Male | 650 (53.8) | 180 | 29.7 (24.7–34.8) | .66 |
| Female | 530 (46.2) | 149 | 31.4 (25.7–37.2) | |
| Race | ||||
| Non‐Hispanic white | 810 (68.5) | 193 | 25.4 (21.5–29.2) | .009 |
| Non‐Hispanic black | 162 (14.1) | 59 | 38.4 (27.2–49.6) | |
| Hispanic | 113 (11.5) | 44 | 47.0 (32.9–61.1) | |
| Non‐Hispanic other | 95 (5.9) | 33 | 39.7 (23.0–56.4) | |
| Household income, in $1000s | ||||
| <25 | 345 (30.0) | 127 | 41.4 (33.5–49.3) | .009 |
| 25–39.9 | 151 (16.4) | 38 | 28.8 (18.1–39.4) | |
| 40–59.9 | 176 (15.4) | 45 | 26.2 (18.8–33.6) | |
| ≥60 | 508 (38.1) | 119 | 24.5 (19.6–29.3) | |
| Education level (n=1174) | ||||
| High school graduate or less | 381 (31.1) | 117 | 33.2 (27.0–39.4) | .33 |
| Some college | 428 (39.3) | 121 | 31.1 (24.0–38.2) | |
| College graduate or more | 365 (29.6) | 89 | 26.8 (20.9–32.7) | |
| Health status | ||||
| Current smoker (n=1139) | ||||
| Yes | 176 (17.4) | 58 | 38.9 (26.8–51.1) | .13 |
| No | 963 (82.6) | 255 | 28.4 (24.7–32.2) | |
| BMI (n=1153) | ||||
| <25 | 211 (18.9) | 60 | 32.6 (23.3–41.9) | .44 |
| 25–30 | 384 (31.4) | 96 | 26.6 (19.5–33.7) | |
| ≥30 | 558 (49.7) | 162 | 31.8 (26.5–37.2) | |
| Diabetes | ||||
| Yes | 315 (26.7) | 86 | 31.7 (24.5–38.9) | .72 |
| No | 865 (73.3) | 243 | 30.1 (25.6–34.6) | |
| High cholesterol | ||||
| Yes | 581 (48.9) | 175 | 32.4 (27.3–37.5) | .35 |
| No | 599 (51.1) | 154 | 28.7 (23.0–34.5) | |
| Congestive heart failure | ||||
| Yes | 55 (4.9) | 18 | 48.8 (29.6–67.9) | .12 |
| No | 1125 (95.1) | 311 | 29.6 (25.8–33.4) | |
| Any cancer (except skin) | ||||
| Yes | 46 (4.0) | 13 | 32.0 (15.6–48.4) | .86 |
| No | 1134 (96.0) | 316 | 30.5 (26.6–34.4) | |
| Migraines | ||||
| Yes | 116 (11.4) | 42 | 42.2 (29.9–54.5) | .06 |
| No | 1064 (88.6) | 287 | 29.0 (25.1–33.0) | |
| Depression (n=971) | ||||
| Yes | 285 (29.6) | 99 | 37.8 (30.5–45.1) | .02 |
| No | 686 (70.4) | 157 | 26.8 (21.4–32.1) | |
| Number of medications taken (n=1160) | ||||
| One | 615 (54.4) | 172 | 29.0 (23.6–34.4) | .35 |
| Two | 330 (26.9) | 81 | 27.3 (21.2–33.4) | |
| More than two or combination drug | 215 (18.7) | 64 | 35.9 (26.5–45.3) | |
| Health behaviors | ||||
| Number of primary care provider visits in the past year | ||||
| 0 | 66 (7.5) | 28 | 50.6 (29.9–71.3) | .10 |
| 1–3 | 649 (53.7) | 168 | 26.9 (22.2–31.6) | |
| 4 or more | 465 (38.9) | 133 | 31.7 (26.0–37.3) | |
| Time of last BP check (n=1166) | ||||
| Within past 6 months | 1067 (90.6) | 288 | 29.6 (25.7–33.5) | .32 |
| More than 6 months earlier | 99 (9.4) | 35 | 38.0 (22.5–53.5) | |
| Using BP monitor to check BP at home (n=1085) | ||||
| Yes | 598 (52.8) | 157 | 29.2 (24.0–34.3) | .80 |
| No | 487 (47.2) | 143 | 30.1 (24.8–35.5) | |
Abbreviations: BMI, body mass index; BP, blood pressure; CI, confidence interval.
From chi‐square test to estimate the significant differences within each selected characteristic.
Among all the reported reasons for not taking BP medication exactly as prescribed, “I cannot afford the medication” was the most common (35.1%), followed by “I do not think I need it to control my blood pressure” (27.1%) and “I forgot to take the medication” (23.6%) (Figure 1). Fewer than 1% of hypertensive adults reported the reasons, “I share the medication with someone else” and “The medication is not working.” No respondent selected the response, “I do not know how to take medication.” The majority (74.3%) of nonadherent hypertensives provided a single response to the question of adherence.
Figure 1.
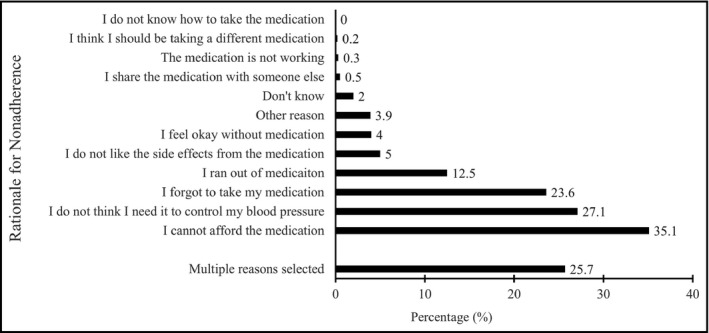
Reasons nonadherent hypertensive adults reported not taking blood pressure medications—HealthStyles Survey, 2010.
Among all the reported rationales for thinking that medications were not needed to control BP, the most commonly reported reasons were “I'm cutting down on salt” (53.1%), followed by “I'm changing my eating habits” (42.4%), “I'm trying to lose weight/I have lost weight” (41.7%), and “I'm exercising more” (39.2%) (Figure 2).
Figure 2.
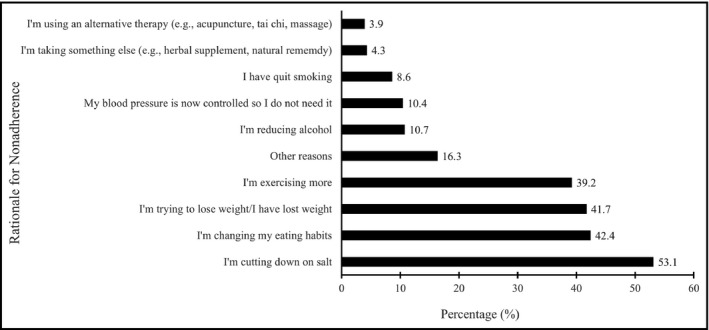
Rationales nonadherent hypertensive adults reported nonadherence—HealthStyles Survey, 2010.
We further looked at the demographic features among the respondents who reported the most common reasons for not taking antihypertensives exactly as prescribed. The percentage of nonadherent hypertensives aged 18 to 44 years (49.3%) who reported “I cannot afford the medication” was significantly greater than the percentages of those aged 45 to 64 years (32.6%) and 65 years and older (20.4%; P=.02) (Table 3). The percentage of the non‐Hispanic other race/ethnicity group who reported “I do not think I need it to control my blood pressure” (61.9%) was significantly greater than the percentages of non‐Hispanic whites (20.3%) and non‐Hispanic blacks (15.7%; P=.02). The percentage of those with a household income <$25,000 who reported “I cannot afford the medication” (48.6%) was significantly greater than the percentages of those with a household income $25,000 to $59,999 (31.4%) and ≥$60,000 (20.5%; P=.02). However, the percentage of those with a household income <$25,000 who reported “I forgot to take the medication” (14.2%) was significantly lower than the percentages of those with a household income $25,000 to $59,999 (30.1%) and ≥$60,000 (29.9%; P=.02).
Table 3.
Percentage of Nonadherent Respondents Reporting Specific Reasons for Not Taking BP Medications Exactly as Prescribed, by Selected Characteristics—HealthStyles Survey, 2010
| Characteristics | Cannot Afford | Don't Need | Forgot | |||
|---|---|---|---|---|---|---|
| % (95% CI) | P Valuea | % (95% CI) | P Value | % (95% CI) | P Value | |
| Age, y | ||||||
| 18–44 | 49.3 (29.1–69.4) | .02 | 27.5 (11.3–43.7) | .13 | 24.6 (11.7–37.5) | .97 |
| 45–64 | 32.6 (24.8–40.5) | 22.1 (15.2–29.1) | 23.3 (16.3–30.4) | |||
| ≥65 | 20.4 (12.2–28.7) | 34.8 (24.8–44.9) | 22.6 (13.8–31.3) | |||
| Sex | ||||||
| Male | 31.2 (21.1–41.3) | .34 | 31.7 (22.3–41.2) | .15 | 20.9 (13.5–28.3) | .32 |
| Female | 39.4 (26.2–52.5) | 22.0 (13.0–31.0) | 26.5 (17.9–35.1) | |||
| Race | ||||||
| Non‐Hispanic white | 28.4 (18.7–38.2) | .33 | 20.3 (13.9–26.7) | .02 | 21.8 (15.2–28.3) | .81 |
| Non‐Hispanic black | 33.0 (17.1–48.9) | 15.7 (5.7–25.7) | 27.4 (13.0–41.9) | |||
| Hispanic | 55.9 (32.1‐79.8) | 45.5 (21.1‐69.8) | 22.6 (6.5‐38.6) | |||
| Non‐Hispanic other | 41.3 (12.9‐69.7) | 61.9 (39.0‐84.8) | 30.2 (8.0‐52.3) | |||
| Household income, in $1000s | ||||||
| <25 | 48.6 (34.2–63.0) | .02 | 31.3 (18.7–43.8) | .09 | 14.2 (7.2–21.3) | .02 |
| 25–59.9 | 31.4 (19.3–43.6) | 30.9 (18.6–43.1) | 30.1 (17.9–42.4) | |||
| ≥60 | 20.5 (7.7–33.3) | 18.0 (10.7–25.2) | 29.9 (20.4–39.3) | |||
| Education level | ||||||
| High school graduate or less | 33.3 (20.9–45.7) | .22 | 30.1 (19.2–41.1) | .65 | 19.9 (10.9–28.9) | .52 |
| Some college | 42.7 (27.7–57.8) | 26.1 (14.4–37.7) | 22.5 (13.5–31.5) | |||
| College graduate or more | 24.1 (8.6–39.5) | 22.9 (12.6–33.3) | 28.0 (17.1–38.9) | |||
| Current smoker | ||||||
| Yes | 53.9 (31.6–76.3) | .09 | 22.7 (5.9–39.4) | .72 | 16.5 (5.7–27.4) | .19 |
| No | 28.8 (21.3–36.3) | 26.1 (19.3–32.9) | 26.3 (19.7–32.8) | |||
| BMI | ||||||
| <25 | 44.2 (23.9–64.5) | .32 | 19.2 (7.2–31.1) | .37 | 18.0 (6.3–29.8) | .59 |
| 25–30 | 40.8 (22.0–59.6) | 31.8 (18.7–44.9) | 23.6 (12.2–34.9) | |||
| ≥30 | 29.1 (20.4–37.8) | 27.4 (17.6–37.3) | 25.8 (17.9–33.6) | |||
| Number of primary care provider visits in the past year | ||||||
| 0 | 71.2 (48.4–94.1) | .09 | 27.4 (2.4–52.5) | .87 | 20.1 (2.2–37.9) | .90 |
| 1–3 | 33.5 (22.3–44.7) | 25.4 (16.5–34.3) | 24.6 (16.9–32.3) | |||
| 4 or more | 25.9 (17.1–34.7) | 29.0 (18.9–39.1) | 23.4 (14.6–32.1) | |||
| Time of last BP check | ||||||
| Within past 6 months | 35.4 (26.3–44.5) | .98 | 28.7 (21.4–35.9) | .11 | 22.3 (16.6–28.1) | .36 |
| More than 6 months earlier | 35.0 (12.5–57.6) | 13.9 (1.8–25.9) | 31.9 (10.3–53.5) | |||
| Using BP monitor at home to check BP | ||||||
| Yes | 28.3 (18.1–38.5) | .23 | 28.8 (19.1–38.5) | .74 | 25.5 (17.0–34.1) | .85 |
| No | 37.4 (26.6–48.2) | 26.5 (17.2–35.9) | 24.4 (16.2–32.6) | |||
| Migraines | ||||||
| Yes | 67.6 (50.7–84.5) | .005 | 23.2 (5.1–41.3) | .64 | 26.6 (10.5–42.7) | .67 |
| No | 29.0 (20.1–38.0) | 27.8 (20.7–34.9) | 23.0 (17.1–28.9) | |||
| Depression | ||||||
| Yes | 55.2 (42.7–67.7) | .01 | 26.4 (14.8–38.0) | .69 | 32.9 (21.6–44.1) | .03 |
| No | 30.5 (16.9–44.1) | 23.3 (13.7–32.9) | 18.4 (11.3–25.5) | |||
Abbreviations: BMI, body mass index; BP, blood pressure; CI, confidence interval.
From chi‐square test to estimate the significant differences within each selected characteristic.
Finally, we examined the factors associated with nonadherence by using both univariate and multiple logistic regression. Age, race, and household income were significantly associated with nonadherence (Table 4). The results from multivariate analysis showed adults aged 18 to 44 years (AOR, 3.33; 95% CI, 1.78–6.23) and aged 45 to 64 years (AOR, 1.53; 95% CI, 1.05–2.22) were more likely to be nonadherent than were those aged 65 years and older. Hispanics were significantly more likely to be nonadherent than non‐Hispanic whites (AOR, 2.13; 95% CI, 1.20–3.77). The adults who reported a household income of <$25,000 were twice as likely to be nonadherent as were those reporting ≥$60,000 (AOR, 1.92; 95% CI, 1.20–3.08).
Table 4.
Univariate and Multivariate Logistic Regression on Nonadherence in Taking High Antihypertensive Medications, by Selected Characteristics—HealthStyles, 2010
| Characteristic | Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|
| Age, y | ||
| 18–44 | 2.92 (1.67–5.11) | 3.33 (1.78–6.23) |
| 45–64 | 1.49 (1.09–2.02) | 1.53 (1.05–2.22) |
| ≥65 | Reference | Reference |
| Sex | ||
| Male | Reference | Reference |
| Female | 0.92 (0.64–1.32) | 1.00 (0.67–1.49) |
| Race | ||
| Non‐Hispanic whites | Reference | Reference |
| Non‐Hispanic black | 1.84 (1.10–3.07) | 1.71 (0.97–3.01) |
| Hispanic | 2.61 (1.43–4.77) | 2.13 (1.20–3.77) |
| Non‐Hispanic other | 1.94 (0.94–4.01) | 1.44 (0.60–3.47) |
| Household income, in $1000s | ||
| <25 | 2.18 (1.44–3.32) | 1.92 (1.20, 3.08) |
| 25–59.9 | 1.17 (0.77–1.79) | 1.09 (0.68–1.75) |
| ≥60 | Reference | Reference |
| Depression | ||
| Yes | 1.66 (1.10–2.51) | 1.33 (0.87–2.03) |
| No | Reference | Reference |
Abbreviation: CI, confidence interval.
Discussion
In our study of hypertensive US adults, the overall self‐reported nonadherence percentage was 30.5%. Age, race/ethnicity, and income were significant factors associated with nonadherence to prescribed antihypertensive medications. The top three most commonly reported barriers or reasons (cannot afford, don't need, and forgot) for nonadherence were also associated with age, race, and household income. Furthermore, the reported rationales for nonadherence among those who did not think they should control their BP were “I'm cutting down on salt,” “I'm changing my eating habits,” and “I'm trying to lose weight/I have lost weight.”
Younger adults, Hispanics, and those with the lowest income were more likely to be nonadherent compared with their counterparts. Prior reports have demonstrated associations between nonadherence and demographic factors such as age, race, and income.7, 8, 9, 10, 11, 12, 14 A potential mechanism proposed by the health belief model17 relates adherence to age, suggesting that the oldest group of adults, often having greater severity of disease(s), are more motivated to adhere to taking their prescribed medications.17 Older adults may also be more likely to receive support from caregivers at home to aid in their medication adherence.18 In addition, better insurance coverage, such as Medicare Part D for those aged 65 years and older,19 is a plausible explanation for higher adherence. In our study, the association between nonadherence and age not only persisted but showed that younger adults (aged 18–44 years) were three times as likely to be nonadherent, after controlling for race/ethnicity, income, and depression. However, there are few new intervention strategies specifically targeting younger hypertensives, underscoring the need for further research.18
In the current study, Hispanic respondents were more likely to be classified as nonadherent than were non‐Hispanic blacks or whites. This outcome is consistent with previous studies finding that Hispanics have the highest percentage of uncontrolled hypertension, largely attributed to nonadherence.20, 21 In our study, more than half of hypertensive Hispanics reported that they did not need to control their BP. A number of potential factors have been reported that could explain these findings, including language barriers, cultural beliefs, a lack of health insurance or a usual source of care, lower income, lower baseline health literacy, and younger age distribution.21, 22 The Institute of Medicine recommends that community health workers (also known as health promoters or promotores de salud) be part of comprehensive multidisciplinary teams as a strategy for improving care delivery, implementing secondary prevention strategies, and enhancing risk reduction.23 Interventions designed specifically for Hispanics, such as Health for Your Heart (Salud Para Su Corazon) and Community Health Workers for Hypertension Control (Salud Contra la Hipertensión), use health promoters to address issues of socioeconomic status and healthcare access related to hypertension management. Such interventions can reduce cultural, language, and access barriers to adherence and improve hypertension control.24, 25
Our findings, consistent with results from previous studies,10, 16 also demonstrated that those with the lowest reported household income were more nonadherent than were those in higher‐income categories. Other studies19, 26 have recommended strategies for reducing cost barriers, including once‐daily dosing of low‐cost medications, 90‐day prescription fills, and expansion of health insurance coverage.
A previous report showed a statistically significant association between mental health—including the diagnosis of depression, migraines, and/or anxiety—and nonadherence.16 Several studies have indicated a significant association between depression and nonadherence.27, 28, 29, 30 Our study focused solely on the association between self‐reported depression and nonadherence. Depression was associated with nonadherence in univariate analysis but the relationship was not statistically significant in our multivariate analysis. The marginal significance on depression obtained in the multivariate analysis might indicate a lack of power because of the small sample size. It would be worthwhile to examine this relationship in future appropriately powered studies and to provide interventions for the management of hypertension among populations with mental health issues.
The most prevalent of the commonly reported barriers to adherence was cost, which is likely correlated with household income. Numerous studies have emphasized cost as a significant barrier to medication adherence.10, 31 One report demonstrated that a comprehensive hypertension management program that included education and no‐cost medication was associated with significant improvements in hypertension control during the 6‐month study period.32 Likewise, another report showed that lower yearly income was associated with nonadherence.16 The Institute of Medicine recommends partnering with the business community to help reduce the costs of antihypertensive medications in order to improve adherence.31 Furthermore, implementation of the Affordable Care Act (ACA) may help waive cost‐sharing (the portion of healthcare costs paid by the patient) for preventive services and increase prescription‐drug coverage.33 Because the ACA was implemented after our study, it would be interesting for future studies to observe how the ACA has affected medication adherence.19
The second most commonly reported barrier was the belief that one did not need to take the medication. The most frequent rationales observed in our study were “I'm cutting down on salt” (53.1%), “I'm changing my eating habits” (42.4%), “I'm trying to lose weight/I have lost weight” (41.7%), and “I'm exercising more” (39.2%). These rationales might be related to the misconception that substituting lifestyle changes is the best or only modality for hypertension control and to a lack of understanding about the importance and effectiveness of antihypertensive therapy. To address this knowledge gap, some researchers have recommended the use of motivational interviewing by healthcare providers to gain a better perspective on their patients' understanding of their health or health beliefs, which, in turn, could help patients use medications better.34, 35 Hypertension management protocols should also take these factors into consideration, even as healthcare providers continue to individualize care to improve adherence among hypertensive adults and prevent the development of serious negative consequences of hypertension such as heart attack, congestive heart failure, stroke, and chronic kidney disease. Our findings provide meaningful insight for healthcare providers to understand different aspects of antihypertensive medication nonadherence among hypertensive adults. Findings from this study could be used by clinicians and public health practitioners when developing interventions for increasing adherence or when providing education and counseling to clarify that starting medications is required in addition to continuing lifestyle modifications.
The third most commonly reported barrier to adherence, also supported by previous findings, was forgetting to take antihypertensive medications.36, 37 Findings from several studies support the use of various intervention strategies that have improved adherence by addressing this issue. These strategies include home visits, education, special dosing devices, small group training, telephone reminders, simplification of dosing regimen (one dose per day when possible), and 90‐day prescriptions and counseling,38, 39 alone or in combination. In fact, several studies have supported the efficacy of a combined approach. A recent study showed multifactorial interventions where the healthcare provider counted patients' pills, designated a family member to support adherence, and provided education to patients were more effective than simple mailing or educational efforts.40 In addition, another study showed that pharmacists in face‐to‐face settings and nurses at hospital discharge were more effective in intervening and improving adherence.41
Study Limitations
Limitations to our study include the response rate of 67.1% to the HealthStyles mail survey, which might lead to nonresponse bias. Although the HealthStyles survey is a population survey designed to match the characteristics of the US adult population, survey participants volunteered to participate and were not a random sample; thus, our findings are subject to selection bias. In addition, the survey requires literacy in the English language and a mailing address, which excludes some households from participation. The survey questions pertaining to barriers to adherence, although covering a broad range of factors, may still have missed some important reasons for nonadherence. Lastly, because of the self‐reported nature of the survey, recall bias or underreporting or overreporting attributable to social desirability is likely and could affect estimates of nonadherence.
Conclusions
Our study found that overall nonadherence was 30.5% and was more prevalent among younger adults, Hispanics, and those with lower income. Affordability was the top reason reported for nonadherence. Promoting public health and health policy interventions might be needed to minimize the cost of medications. Our study also identified the need for clinicians to explore patients' rationales and perceptions regarding their hypertension medications, and reinforced the importance of consistent medication use to control hypertension. Interventions that support the management of hypertension, particularly in at‐risk populations, and that use community‐based and clinical evidenced‐based resources to improve medication adherence should be considered.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the CDC.
J Clin Hypertens (Greenwich). 2016;18:892–900. DOI: 10.1111/jch.12786. Published 2016. This article is a U.S. Government work and is in the public domain in the USA.
References
- 1. Nwankwo T, Yoon SS, Burt V, et al. Hypertension among adults in the United States: national health and nutrition examination survey, 2011–2012. NCHS Data Brief. 2013;133:1–8. [PubMed] [Google Scholar]
- 2. Go AS, Mozaffarian D, Roger VL, et al. American Heart Association statistics committee and stroke statistics committee. Heart disease and stroke statistical update 2014: a report from the American Heart Association. Circulation. 2014;129:e28–e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 4. Chobanian AV, Bakris G, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 5. Sanson‐Fisher RW, Clover K. Compliance in the treatment of hypertension. A need for action. Am J Hypertens. 1995;8:82S–88S. [DOI] [PubMed] [Google Scholar]
- 6. Gu Q, Dillon CF, Burt VL, et al. Association of hypertension treatment and control with all‐cause and cardiovascular disease mortality among US adults with hypertension. Am J Hypertens. 2010;23:38–45. [DOI] [PubMed] [Google Scholar]
- 7. Levinthal BR, Morrow DG, Tu W, et al. Cognition and health literacy in patients with hypertension. J Gen Intern Med. 2008;23:1172–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lewis LM, Ogedegbe G. Understanding the role and nature of spirituality in reference to medication adherence: a proposed conceptual model. Holist Nurs Pract. 2008;22:261–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Monane M, Bohn RL, Gurwitz JH, et al. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86:1805–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ndumele CD, Shaykevich S, Williams D, et al. Disparities in adherence to hypertensive care in urban ambulatory settings. J Health Care Poor Underserved. 2010;21:132–143. [DOI] [PubMed] [Google Scholar]
- 11. Ogedegbe G, Harrison M, Robbins L, et al. Barriers and facilitators of medication adherence in hypertensive African‐Americans: a qualitative study. Ethn Dis. 2004;14:158. [PubMed] [Google Scholar]
- 12. Polinski JM, Kesselheim A, Frolkis JP, et al. A matter of trust: patient barriers to primary medication adherence. Health Educ Res. 2014;29:755–763. [DOI] [PubMed] [Google Scholar]
- 13. Gerin W, Tobin JN, Schwartz JE, et al. The medication adherence and blood pressure control (ABC) trial: a multi‐site randomized controlled trial in a hypertensive, multi‐cultural, economically disadvantaged population. Contemp Clin Trials. 2007;28:459–471. [DOI] [PubMed] [Google Scholar]
- 14. Marentette MA, Gerth WC, Billings DK, et al. Antihypertensive persistence and drug class. Can J Cardiol. 2002;18:649–656. [PubMed] [Google Scholar]
- 15. Miller NH, Hill M, Kottke T, et al. The multi‐level compliance challenge: recommendations for a call to action. A statement for healthcare professionals. Circulation. 1997;95:1085–1090. [DOI] [PubMed] [Google Scholar]
- 16. Vawter L, Tong X, Gemilyan M, et al. Barriers to antihypertensive medication adherence among adults—United States, 2005. J Clin Hypertens (Greenwich). 2008;10:922–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11:1–47. [DOI] [PubMed] [Google Scholar]
- 18. AHRQ Report , Medication Adherence Interventions: Comparative Effectiveness, Closing the Quality Gap: Revisiting the State of the Science: Evidence Report No. 208. AHRQ Publication. 2012. 12(E010). [PMC free article] [PubMed] [Google Scholar]
- 19. Gap CtC, Closing the Coverage Gap—Medicare Prescription Drugs are Becoming More Affordable. Department of Health and Human Services. 2015. [Google Scholar]
- 20. Gu Q, Burt VL, Dillon CF, et al. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension. Circulation. 2012;126:2105–2114. [DOI] [PubMed] [Google Scholar]
- 21. Stewart SH, Silverstein MD. Racial and ethnic disparity in blood pressure and cholesterol measurement. J Gen Intern Med. 2002;17:405–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Traylor AH, Schmittdiel JA, Uratsu CS. Adherence to cardiovascular disease medications: does patient‐provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25:1172–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine; 2002. [PubMed] [Google Scholar]
- 24. Balcazar H, Alvarado M, Cantu F, et al. A promotora de salud model for addressing cardiovascular disease risk factors in the US‐Mexico border region. Prev Chronic Dis. 2009;6:A02. [PMC free article] [PubMed] [Google Scholar]
- 25. Balcazar HG, de Heer H, Rosenthal L, et al. A promotores de salud intervention to reduce cardiovascular disease risk in a high‐risk Hispanic border population. Prev Chronic Dis. 2010;7:A28. [PMC free article] [PubMed] [Google Scholar]
- 26. Morrison VL, Holmes EA, Parveen S, et al. Predictors of self‐reported adherence to antihypertensive medicines: a multinational, cross‐sectional survey. Value Health. 2015;18:206–216. [DOI] [PubMed] [Google Scholar]
- 27. Cha E, Erlen JA, Kim KH, et al. Mediating roles of medication‐taking self‐efficacy and depressive symptoms on self‐reported medication adherence in persons with HIV: a questionnaire survey. Int J Nurs Stud. 2008;45:1175–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dempe C, Junger J, Hoppe S, et al. Association of anxious and depressive symptoms with medication nonadherence in patients with stable coronary artery disease. J Psychosom Res. 2013;74:122–127. [DOI] [PubMed] [Google Scholar]
- 29. Gonzalez JS, Safren SA, Cagliero E, et al. Depression, self‐care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Weidenbacher HJ, Beadles CA, Maciejewski ML, et al. Extent and reasons for nonadherence to antihypertensive, cholesterol, and diabetes medications: the association with depressive symptom burden in a sample of Americans veterans. Patient Prefer Adherence. 2015;9:327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fleming D, Koh H, Roux AVD, et al. A Population‐Based Policy and Systems Change Approach to Prevent and Control Hypertension. Institute of Medicine. 2010. [PubMed] [Google Scholar]
- 32. Applegate BW, Ames SC, Mehan DJ Jr, et al. Maximizing medication adherence in low‐income hypertensives: a pilot study. J La State Med Soc. 2000;152:349–356. [PubMed] [Google Scholar]
- 33. Friden TR, Berwick DM. The “million hearts” initiative—preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. [DOI] [PubMed] [Google Scholar]
- 34. Clark NM, Nothwehr F, Gong M, et al. Physician‐patient partnership in managing chronic illness. Acad Med. 1995;70:957–958. [DOI] [PubMed] [Google Scholar]
- 35. Clark NM, Gong M. Management of chronic disease by practitioners and patients: are we teaching the wrong things? Br Med J. 2000;320:572–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Odegard PS, Carpinito G, Christensen DB. Medication adherence program: adherence challenges and interventions in type 2 diabetes. J Am Pharm Assoc (2003). 2013;53:267–272. [DOI] [PubMed] [Google Scholar]
- 37. Odegard PS, Gray SL. Barriers to medication adherence in poorly controlled diabetes mellitus. Diabetes Educ. 2008;34:692–697. [DOI] [PubMed] [Google Scholar]
- 38. Leenen FH, Wilson TW, Bolli P, et al. Patterns of compliance with once versus twice daily antihypertensive drug therapy in primary care: a randomized clinical trial using electronic monitoring. Can J Cardiol. 1997;13:914–920. [PubMed] [Google Scholar]
- 39. Morisky DE, DeMuth NM, Field‐Fass M, et al. Evaluation of family health education to build social support for long‐term control of high blood pressure. Health Educ Q. 1985;12:35–50. [DOI] [PubMed] [Google Scholar]
- 40. Pladevall M, Brotons C, Gabriel R, et al. A multi‐center cluster‐randomized trial of a multi‐factorial intervention to improve antihypertensive medication adherence and blood pressure control among patients at high cardiovascular risk (the COM99 study). Circulation. 2010;122:1183–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cutrona SL, Choudhry NK, Fischer MA, et al. Modes of delivery for interventions to improve cardiocvascular medication adherence: review. Am J Manag Care. 2010;16:929–942. [PMC free article] [PubMed] [Google Scholar]


