Introduction
Iris mammillation is an uncommon congenital anomaly of the eye that is rarely reported in the literature; initial reports describe iris mammillations using different terminology, such as bilateral iris melanosis, dotted Swiss iris, and bilateral diffuse iris nodular nevi.1 Microscopic examination finds focal nesting of spindle-shaped melanocytes, hence, the name diffuse iris nodular nevi.1, 2 The etiology of iris mammillations is unknown and when coexisting with ocular melanocytosis, it has been associated with choroidal melanoma.2 Cowden syndrome (CS) is a hereditary cancer syndrome characterized by the development of multiple hamartomas and an increased risk of malignant neoplasms in multiple organs.3 Here we report on identical twins with CS in association with iris mammillations. To our knowledge, this is the first time this association has been reported.
Case report
An otherwise healthy 22-year-old Hispanic woman presented to the dermatology clinic for evaluation of a 3-mm pedunculated growth on the right nasal ala. Physical examination found, in addition to her alar growth, innumerable skin-colored, 1- to 2-mm papules on the face (Fig 1), gingival cobblestoning (Fig 2), palmar pits, and macrocephaly (head circumference, 64 cm; >97th percentile). Histopathologic findings from the pedunculated papule on the right nasal ala and 2 other facial papules were consistent with trichilemmomas. The patient was referred for genetic testing, which found a deleterious mutation in the phosphatase and tensin homolog (PTEN) gene, confirming CS. After her diagnosis, she was referred to the breast, gynecology, gastroenterology, and endocrine clinics for thyroid and adrenal workups; she was found to have fibrocystic disease and fibroadenomas of the breast, multiple colonic polyps, and thyroid nodules. No evidence of adrenal abnormality was found. During slit-lamp examination performed when she was evaluated for lesions consistent with trichilemmoma of her eyelid, an incidental finding of bilateral iris mammillations was noted (Fig 3).
Fig 1.
Innumerable, 1- to 2-mm skin-colored, round papules scattered on the face.
Fig 2.
Gingival cobblestoning with subtle lip cobblestoning and upper right central tooth pitting.
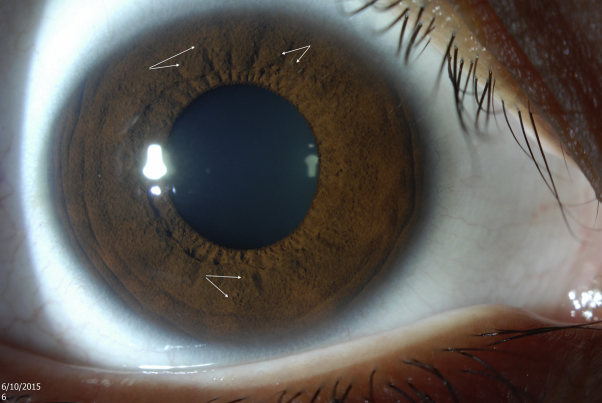
Fig 3.
White arrows point to multiple, round, equally spaced, projections on the iris representing iris mammillations.
Given the above information, the patient's identical twin sister was offered a full skin examination, which had similar findings of innumerable facial papules, gingival cobblestoning, and macrocephaly. After ophthalmology referral, she was also found to have bilateral iris mammillations on slit-lamp examination. Genetic testing confirmed a deleterious mutation in PTEN, thus, also establishing the diagnosis of CS in her twin. Both twins are under close surveillance by multiple specialties given their underlying diagnosis and clinical presentation.
Discussion
Iris mammillation is a congenital anomaly consisting of multiple dark brown, mound-shaped excrescences arising from the anterior surface of the iris.1, 2, 4, 5 In contrast to Lisch nodules, which are an important differential diagnosis, iris mammillations uniformly appear on the iris surface and do not differ significantly in pigmentation from the surrounding iris tissue. Histologically, the latter represent spindle-shaped nevoid melanocytes, usually interspersing pigmented iris stroma.2, 5 Iris mammillations may be unilateral or bilateral, familial or sporadic, and found either as an isolated finding or in association with ocular and extraocular diseases, such as phakomatosis pigmentovascularis type IIb, neurofibromatosis, and congenital adrenal hyperplasia.5, 6 Iris mammillations with coexistent ocular melanocytosis is a precancerous condition associated with an increased incidence of intraocular melanoma.2, 5 PTEN-deficient melanocytes were found to be larger in mouse models,7 and reduced nuclear PTEN expression in human acquired melanocytic nevi has been established8; we speculate that PTEN mutation may have played a role in iris mammillations development in our patients.
CS, also known as PTEN hamartoma syndrome is an autosomal dominant genodermatosis associated with a PTEN gene mutation on chromosome 10 in approximately 80% of cases. Other gene mutations including killin (KLLN), mitochondrial succinate dehydrogenase B or D (SDH B/D), phosphatidylinositol 3-kinase (PIK3), and V-Akt murine thymoma viral oncogene homolog 1 (AKT1) are thought to be the underlying gene mutations in the other 20% of cases. CS usually presents in the second or third decade of life with a prevalence rate of 1 in 200,000.3, 9, 10
PTEN hamartoma syndrome encompasses a group of syndromes (CS, Bannayan-Riley- Ruvalcaba, Lhermitte-Duclos disease, Proteus and Proteus-like syndrome) that share overgrowth of various ectodermal, mesodermal, and endodermal cells.10 Cutaneous manifestations such as trichilemmomas, mucosal and gingival cobblestoning, lipomas, acral keratosis, and pits are seen. Thyroid diseases and neoplasms are common among CS patients as well as breast diseases and breast cancers. Other malignancies such as gastrointestinal, renal, and endometrial cancers and malignant melanoma are manifested in CS patients with various percentages in previous reports.3, 9, 10
To our knowledge, this is the first reported association of CS with iris mammillations. Our patient has an identical twin with genetically confirmed CS, also displaying iris mammillations. It is unclear whether the presence of iris mammillations in the twin sisters is from a separate familial cause or related to the underlying CS. Careful and detailed eye examination in patients with CS may reveal further individuals with this similar association, which adds to the CS-associated hamartomas. This potential new association of CS with iris mammillations may also have implications for the individual if there is also coexistent ocular melanocytosis, as there is an increased risk of intraocular melanoma in these cases. In addition, even in the absence of ocular melanocytosis, iris mammillations that occur in the setting of PTEN mutation may have a theoretical increased risk for malignant transformation given that malignant melanoma was prevalent in 6% of CS patients in one case series3 and PTEN-deficient melanocytes were found to be susceptible to carcinogen-induced invasive spindle cell melanoma in a mouse model.7 Therefore, detailed ocular screening may be warranted in CS individuals.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
Presented at the New England Dermatology Society Meeting held at Boston University, December 5, 2015.
References
- 1.Ticho B.H., Rosner M., Mets M.B., Tso M.O. Bilateral diffuse iris nodular nevi. Clinical and histopathologic characterization. Ophthalmology. 1995;102(3):419–425. doi: 10.1016/s0161-6420(95)31006-8. [DOI] [PubMed] [Google Scholar]
- 2.Gunduz K., Shields C.L., Shields J.A., Eagle R.C., Jr., Singh A.D. Iris mammillations as the only sign of ocular melanocytosis in a child with choroidal melanoma. Arch Ophthalmol. 2000;118(5):716–717. doi: 10.1001/archopht.118.5.716. [DOI] [PubMed] [Google Scholar]
- 3.Porto A.C., Roider E., Ruzicka T. Cowden Syndrome: report of a case and brief review of literature. An Bras Dermatol. 2013;88(6 Suppl 1):52–55. doi: 10.1590/abd1806-4841.20132578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peyman M., Ong M.J., Iqbal T., Subrayan V. Iris mammillations in two female siblings with congenital adrenal hyperplasia. BMJ Case Reports. 2010;2010 doi: 10.1136/bcr.08.2010.3266. bcr0820103266. http://dx.doi.org/10.1136/bcr.08.2010.3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ragge N.K., Acheson J., Murphree A.L. Iris mammillations: significance and associations. Eye (Lond) 1996;10(Pt 1):86–91. doi: 10.1038/eye.1996.13. [DOI] [PubMed] [Google Scholar]
- 6.Gilliam A.C., Ragge N.K., Perez M.I., Bolognia J.L. Phakomatosis pigmentovascularis type IIb with iris mammillations. Arch Dermatol. 1993;129(3):340–342. [PubMed] [Google Scholar]
- 7.Inoue-Narita T., Hamada K., Sasaki T. Pten deficiency in melanocytes results in resistance to hair graying and susceptibility to carcinogen-induced melanomagenesis. Cancer Res. 2008;68(14):5760–5768. doi: 10.1158/0008-5472.CAN-08-0889. [DOI] [PubMed] [Google Scholar]
- 8.Tsao H., Mihm M.C., Jr., Sheehan C. PTEN expression in normal skin, acquired melanocytic nevi, and cutaneous melanoma. J Am Acad Dermatol. 2003;49(5):865–872. doi: 10.1016/s0190-9622(03)02473-3. [DOI] [PubMed] [Google Scholar]
- 9.Salem O.S., Steck W.D. Cowden's disease (multiple hamartoma and neoplasia syndrome). A case report and review of the English literature. J Am Acad Dermatol. 1983;8(5):686–696. doi: 10.1016/s0190-9622(83)70081-2. [DOI] [PubMed] [Google Scholar]
- 10.Monga E., Gupta P.K., Munshi A., Agarwal S. Multiple hamartoma syndrome: clinicoradiological evaluation and histopathological correlation with brief review of literature. Indian J Dermatol. 2014;59(6):598–601. doi: 10.4103/0019-5154.143535. [DOI] [PMC free article] [PubMed] [Google Scholar]