Highlights
-
•
More than 96% of signet-ring cell carcinomas occur in the stomach.
-
•
Primary SRC carcinoma of the colon and rectum is very rare.
-
•
It spreads mainly to the lymph nodes and to the peritoneum and rarely to the liver.
-
•
It presents at advanced stages and has a dismal prognosis.
-
•
Upper endoscopy is the investigation of choice to exclude a primary gastric cancer.
Abbreviations: SRC, signet-ring cell
Keywords: Signet-ring cell carcinoma, Colorectal cancer, Bony metastases, Pathology, Appendicitis, Right hemicolectomy
Abstract
Introduction
More than 96% of signet-ring cell carcinomas occur in the stomach and the rest in other organs, including the gallbladder, pancreas, urinary bladder and breast. Primary signet-ring cell carcinoma of the colon and rectum is very rare, accounting for 0.1%–2.4% of all colorectal cancers.
Presentation of case
We report a case of a 55-year old man who is operated for a caecal mass evocative of an appendicitis abscess. Intraoperatively, we discover a large, ulcerated ilio-caecal mass with several lymphadenopathies. The further workup reveals a primary signet-ring cell carcinoma of the colon with multiple lymph nodes and osteolytic bony metastases.
Discussion
Primary signet-ring cell carcinoma of the colon and rectum presents usually as an advanced stage disease with a dismal prognosis. It spreads mainly to the lymph nodes and to the peritoneum and very rarely to the liver. The mean age of patients diagnosed with primary signet-ring cell carcinoma is significantly younger than for ordinary adenocarcinoma. The upper endoscopy is the investigation of choice to exclude a primary gastric pathology. There are very few reports about this type of cancer and no reports about this type of cancer associated with osteolytic bony metastases.
Conclusion
The characteristics and pathophysiology of a primary signet-ring cell carcinoma of the colon and rectum are not well understood. Usually only palliative treatment is possible. The importance of an early diagnosis of this tumor is mandatory to have a curative approach.
1. Introduction
More than 96% of signet-ring cell carcinomas occur in the stomach and the rest in other organs, including the gallbladder, pancreas, urinary bladder and breast [1]. Primary SRC carcinoma of the colon and rectum is very rare, accounting for 0.1%–2.4% of all colorectal cancers [2]. Compared to the colorectal adenocarcinoma, this tumor type is diagnosed at more advanced stages, presents at a younger age and has a worse prognosis than the common adenocarcinoma [3], [4]. It is characterized by a dismal prognosis. The dissemination pattern is chiefly peritoneal with a predominantly lymphatic invasion. Liver metastases are very rare [3], [4], [5], [6]. It has been described that its radiographic characteristics can mimic an inflammatory process [7].
We report a case of a primary SRC carcinoma of the caecum that presents with symptoms and radiologic images compatible with an acute appendicitis abscess. It is treated by surgical resection. The further work up reveals multiple osteolytic bony metastases (Fig. 1).
Fig. 1.
Intraoperative status with an abscessed ileo-caecal mass.
So far, there are very few reports about this tumor type presenting with bony metastases and because of the rarity of the SRC carcinoma, its characteristics and pathophysiology are not well understood.
2. Presentation of case
A 55-year old patient presents to our emergency department with right lower quadrant pain for the last 24 h accompanied by a subfebrile state. The patient is in excellent general condition without previous surgical history. He has a mild hypertension and diabetes on oral medication. The pain is accompanied by nausea without vomiting. He denies any weight loss, change in stool habits, hematochezia or melena. He does not report any previous history of abdominal pain.
Physical examination reveals a right lower quadrant tenderness. The bowel sounds are normal.
The lab tests show a CRP of 22 mg/l, and no leucocytosis. A low dose CT scan is performed because of a high suspicion of an appendicitis and shows an inflammatory thickening of the ceacal wall with a collection of the ileo-caecal zone which could correspond to an abscessed appendix. The appendix itself is not visualized. There are retroperitoneal lymphadenopathies to be found (Fig. 2).
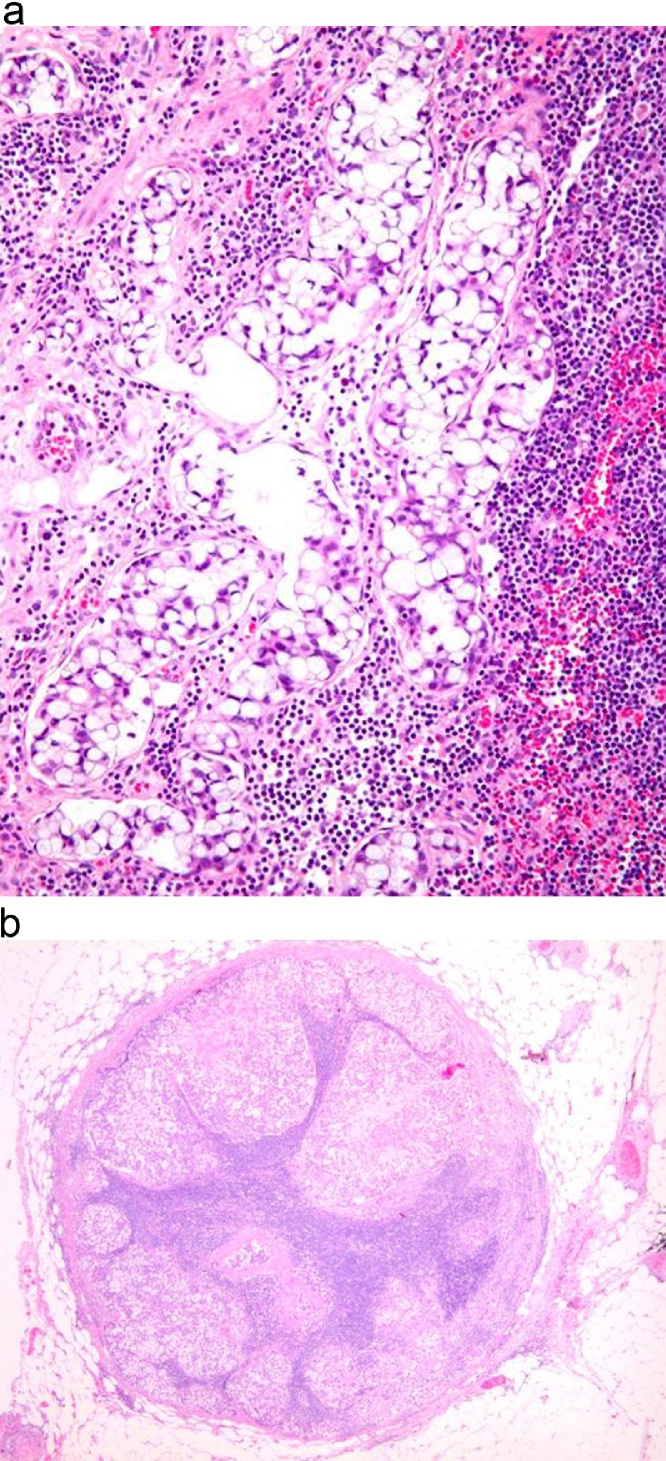
Fig. 2.
A. Histology. The tumor cells are ≪ signet ring ≫ shaped, with prominent intracytoplasmic mucin, which pushes the nucleus to the cell periphery. According to the WHO classification, the designation ≪ signet ring cell carcinoma ≫ is used if at least 50% of the tumor cells are signet ring-shaped. B. Massive regional lymph node metastasis from the signet ring cell carcinoma.
The clinical presentation and the image on the low-dose CT scan are highly evocative of an acute appendicitis with a small abscess. The patient is planned for a laparoscopic appendectomy. The abdominal exploration reveals a thickened ceacum patched together with the terminal ileum on the posterior abdominal wall. A conversion into a laparotomy is decided due to very inflammatory tissues and inability to carry on safely with the laparoscopic approach. We discover a large mass involving the ceacum and the terminal ileum. Frozen section reveals the presence of an adenocarcinoma. An oncologic right hemicolectomy is therefore permormed, which turns out to be extremely difficult because the mass is patched on the iliac vessels and on the right ureter. An ileo-transverse anastomosis is performed with uncomplicated postoperative recovery. The final pathologic analysis reveals a SRC carcinoma of 10,5 cm, infiltrating the serosa, with an extensive lymphatic invasion and 15 metastatic ganglions (15/15). The resection margins are without tumor and the K-RAS is tested positive.
In order to exclude a primary gastric pathology, we perform a gastroscopy, as this histology has most of the time a primary gastric localization. The gastroscopy is normal and a thoracic CT-scan shows the absence of secondary lesions. But the PET CT shows multiple osteolytic bone metastases: to the ribs, to the vertebral bodies, the right humerus and a destruction of the two omoplates, all of them associated with a high fracture risk.
His post-operative tumor marker CEA level is elevated at 251 μg/l and PSA and CA19-9 levels are negative. The alkaline phosphatase is at a normal level preoperatively (115 U/l) and rises up to 144 U/l 5 weeks later.
Folfox regimen with Irinotecan and Bevacizumab has been started and the patient is still undergoing treatment (Fig. 3).
Fig. 3.
A. Imaging of the patient. PET CT. Multiple osteolytic metastases to the vertebral bodies and to the left omoplate, associated with a fracture. B. Abdominal CT scan. A mass with a possible abscess is visualized in the ileo-caecal zone.
3. Discussion
SRC cancer is characterized by the abundant intracytoplasmatic mucin that pushes the nucleus to the periphery, creating a microscopic signet-ring appearance. The tumor must consist of at least 50% of these signet cells [8]: More than 96% of the SRC carcinomas occur in the stomach [1]. The incidence of the primary SRC carcinoma of the colon and rectum is reported 0.6 per 100 000 persons in the year 2000. The incidence rate is increasing with an annual percent change of 4.8% in contrast to the ordinary adenocarcinoma the incidence of which is slightly decreasing [6].
The mean age of patients diagnosed with primary SRC carcinoma is 39.6–60 − which is significantly younger than for an ordinary adenocarcinoma (70 years). [1], [5], [9].
Metastasis from gastric carcinoma is probably the most common secondary lesion in the colon and rectum [10]. They appear mostly in the transverse colon, while the primary SRC cancer of the colon appears predominantly in the rectum (32.9%), followed by the sigmoid colon (20.4%), the caecum (11.2%) and the ascending colon (10.5%). This can be a feature distinguishing a primary SRC carcinoma of the colon from the gastric SRC metastasis. The upper endoscopy is the investigation of choice to exclude a primary gastric pathology.
As to the tumor grade, the SRC carcinoma of the colon was found to present with high grade, poorly differentiated tumors (73.5% of G3 or G4) which is significantly different from the ordinary adenocarcinoma (only 17.5% of G3 or G4) [6].
The primary SRC carcinoma of the colon is more likely to present with later stage lesions or metastases. Significantly more patients suffer from distant metastases. 80.9% are diagnosed at stage III/IV compared with the 49.5% of the ordinary adenocarcinoma6. However, the dissemination patterns are quite different: SRC cancer dissemination is chiefly peritoneal with lymph node and peritoneal involvement [1], [3], [5]. The rate of liver metastases has been seen in 2.9%–14.3% of cases compared to the 32%–43% of the ordinary adenocarcinoma. The incidence of bone metastases from colorectal cancer is between 4.7%–10.9% [11], [12], [13]. There are extremely few case reports in the literature about the SRC carcinoma of the colon with diffuse bone metastases [14], [15]. Our patient didn’t present any liver nor lung metastases but many lymph node metastases and multiple osteolytic bone lesions. Because of the extremely rare evidence of the osteolytic bone lesions secondary to the SRC carcinoma of the colon in the literature, we need to exclude a synchronous prostate carcinoma. The PSA level is normal. The usual pathophysiology of the bony metastases is that the detached cancer cells reach the liver through the portal vein and then go to the lungs and to the arterial tree or reach the lungs directly through the inferior vena cava. In our patient, the absence of secondary lung and liver lesions suggests that the tumor cells reach the venous system directly through lymphatic ducts that drains into the venous system.
The radiographic findings of the SRC carcinoma include the thickening of the bowel wall with a “target appearance” and perirectal/pericolic infiltration [16]. Its radiographic characteristics can mimic an inflammatory process [7]. Also in our patient, the radiographic features together with the clinical presentation were evocative of an acute appendicitis.
The SRC carcinoma of the colon has a significantly poorer prognosis with five-year survival of 26.8% compared to the 62.9% of the ordinary adenocarcinoma [6]. The median and mean survival time is respectively 20 and 45 months [8], [17], [18]. In consequence, the SRC carcinoma can be regarded as an independent prognostic factor for poorer outcomes [3], [6], [17], [18].
There are some reports that suggest an association between the SRC carcinoma of the colon with the inflammatory bowel disease with 12–14% of patients with SRC having a history of IBD [2], [19].
4. Conclusion
In conclusion, the primary colorectal SRC carcinoma is characterized by younger age, more advanced stages at presentation, higher tumor grade, more frequent distant metastasis that involve mainly the lymph nodes and the peritoneum and rarely the liver, a dismal prognosis and radiographic features that can mimic an inflammatory process. Usually only a palliative surgery is possible. The importance of an early diagnosis of this tumor should be stressed. The role of resection for late stage SRC should be carefully evaluated.
Consent
All the authors confirm that the manuscript represents our own work, is original and has not been copyrighted, published, submitted, or accepted for publication elsewhere. The authors further confirm that theyall have fully read the manuscript and give consent to be co-authors of the manuscript.
Conflict of interest statement
There is no conflict of interests.
Sources of funding
The was no involvement of any sort of funding for our case report.
Ethical approval
Our case report is not a research study and thus it does not require an ethical approval. You may contact the Ethics Committee of Geneva if you wish to obtain further information. Reference Number: Req-2016-00067. Contact: Prof. Bernard Hirschel Président, Commission cantonale d'éthique de la recherche, 1211 Genève 14, Tél. +41 79 553 3491.
Author contribution
All of the authors contributed equally to the paper concept, design, data collection, data analysis and interpretation and writing the paper.
Guarantor
Paulina Kuczma, MD, Geneva University Hospital, Switzerland.
Contributor Information
Paulina Kuczma, Email: pkuczma@gmail.com.
Jordi Vidal Fortuny, Email: jordi.vidalfortuny@hcuge.ch.
Saiji Essia, Email: essia.saiji@hcuge.ch.
Ariane de Lassus, Email: ariane.delassus@hcuge.ch.
Philippe Morel, Email: philippe.morel@hcuge.ch.
Frédéric Ris, Email: frederic.ris@hcuge.ch.
References
- 1.Tung S.Y., Wu C.S., Chen P.C. Primary signet ring cell carcinoma of colorectum: an age- and sex-matched controlled study. Am. J. Gastroenterol. 1996;91:2195–2199. [PubMed] [Google Scholar]
- 2.Anthony T., George R., Rodriguez-Bigas M., Petrelli N.J. Primary signet-ring cell carcinoma of the colon and rectum. Ann. Surg. Oncol. 1996;3:344–348. doi: 10.1007/BF02305663. [PMID: 8790846] [DOI] [PubMed] [Google Scholar]
- 3.Psathakis D., Schiedeck T.H., Krug F., Oevermann E., Kujath P., Bruch H.P. Ordinary colorectal adenocarcinoma vs primary colorectal signet-ring cell carcinoma: study matched for age, gender, grade, and stage. Dis. Colon Rectum. 1999;42:1618–1625. doi: 10.1007/BF02236218. [PMID: 10613484] [DOI] [PubMed] [Google Scholar]
- 4.Makino T., Tsujinaka T., Mishima H., Ikenaga M., Sawamura T., Nakamori S., Fujitani K., Hirao M., Kashiwazaki M., Masuda N., Takeda M., Mano M. Primary signet-ring cell carcinoma of the colon and rectum: report of eight cases and review of 154 Japanese cases. Hepatogastroenterology. 2006;53:845–849. [PMID: 17153438] [PubMed] [Google Scholar]
- 5.Bittorf B., Merkel S., Matzel K., Wein A., Dimmler A., Hohenberger W. Primary signet-ring cell carcinoma of the colorectum. Langenbecks Arch. Surg. 2004;389:178–183. doi: 10.1007/s00423-004-0474-y. [DOI] [PubMed] [Google Scholar]
- 6.Kang H., O’Connell J.B., Maggard M.A., Sack J., Ko C.Y. A 10-year outcomes evaluation of: mucinous and signet-ring cell carcinoma of the colon and rectum. Dis. Colon Rectum. 2005;6(June 48):1161–1168. doi: 10.1007/s10350-004-0932-1. [DOI] [PubMed] [Google Scholar]
- 7.Bonello J.C., Quan S.H., Sternberg S.S. Primary linitis plastica of the rectum. Dis. Colon Rectum. 1980;23:337–342. doi: 10.1007/BF02586841. [PMID: 6249557] [DOI] [PubMed] [Google Scholar]
- 8.Messerini L., Palomba A., Zampi G. Primary signet-ring cell carcinoma of the colon and rectum. Dis. Colon Rectum. 1995;38(11):189–1192. doi: 10.1007/BF02048335. [DOI] [PubMed] [Google Scholar]
- 9.Tandon M., Sostek M., Klein M.A. Focus of signet ring cell carcinoma in an adenoma of the sigmoid colon. Arch. Pathol. Lab. Med. 1999;123:957–959. doi: 10.5858/1999-123-0957-FOSRCC. [PMID: 10506454] [DOI] [PubMed] [Google Scholar]
- 10.Amorn Y., Knight W.A., Jr. Primary linitis plastica of the colon: report of two cases and review of the literature. Cancer. 1978;41:2420–2425. doi: 10.1002/1097-0142(197806)41:6<2420::aid-cncr2820410648>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 11.Baker L.H., Vaitkevicius V.K., Figiel S.J. Bony metastasis from adenocarcinoma of the colon. Am. J. Gastroenterol. 1974;62:139–144. [PubMed] [Google Scholar]
- 12.Besbeas S., Stearns M.W. Osseous metastasis from carcinoma of colon and rectum. Dis. Colon Rectum. 1978;21:266–268. doi: 10.1007/BF02586701. [DOI] [PubMed] [Google Scholar]
- 13.Bonnheim D.C., Petrelli N.J., Herrera L. Osseous metastasis from colorectal cancer. Am. J. Surg. 1986;151:457–459. doi: 10.1016/0002-9610(86)90102-9. [DOI] [PubMed] [Google Scholar]
- 14.Kobayashi M., Ito M., Kato M., Uchikawa Y., Takagi S. Primary colonic signet ring cell carcinoma presenting with carcinocythemia: an autopsy case. Case Rep. Gastroenterol. 2008;30(September (3)):301–307. doi: 10.1159/000155146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta R.S., Ennis P., Whitten J. Ureterosigmoidostomy associated signet ring colon cancer presenting as hip pain. J. Gastrointest. Cancer. 2012;43(March (1)):122–127. doi: 10.1007/s12029-010-9184-6. [DOI] [PubMed] [Google Scholar]
- 16.Kim H.J., Ha H.K., Cho K.S. CT features of primary colorectal signet-ring cell carcinoma. J. Comput. Assisted Tomogr. 2001;25:225–230. doi: 10.1097/00004728-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Nissan A., Guillem J.G., Paty P.B., Wong W.D., Cohen A.M. Signet-ring cell carcinoma of the colon and rectum: a matched control study. Dis. Colon Rectum. 1999;42:1176–1180. doi: 10.1007/BF02238570. [DOI] [PubMed] [Google Scholar]
- 18.Ooi B.S., Ho Y.H., Eu K.W., Seow Choen F. Primary colorectal signet-ring cell carcinoma in Singapore. ANZ J. Surg. 2001;71:703–706. doi: 10.1046/j.1445-1433.2001.02269.x. [DOI] [PubMed] [Google Scholar]
- 19.Ojeda V.J., Mitchell K.M., Walters M.N., Gibson M.J. Primary colo-rectal linitis plastica type of carcinoma: report of two cases and review of the literature. Pathology (Phila.) 1982;14:181–189. doi: 10.3109/00313028209061292. [PMID: 6285255] [DOI] [PubMed] [Google Scholar]