Abstract
Introduction
Milrinone is an inotrope widely used for treatment of cardiac failure. Because previous meta-analyses had methodological flaws, we decided to conduct a systematic review of the effect of milrinone in critically ill adult patients with cardiac dysfunction.
Methods
This systematic review was performed according to The Cochrane Handbook for Systematic Reviews of Interventions. Searches were conducted until November 2015. Patients with cardiac dysfunction were included. The primary outcome was serious adverse events (SAE) including mortality at maximum follow-up. The risk of bias was evaluated and trial sequential analyses were conducted. The quality of evidence was assessed by the Grading of Recommendations Assessment, Development and Evaluation criteria.
Results
A total of 31 randomised clinical trials fulfilled the inclusion criteria, of which 16 provided data for our analyses. All trials were at high risk of bias, and none reported the primary composite outcome SAE. Fourteen trials with 1611 randomised patients reported mortality data at maximum follow-up (RR 0.96; 95% confidence interval 0.76–1.21). Milrinone did not significantly affect other patient-centred outcomes. All analyses displayed statistical and/or clinical heterogeneity of patients, interventions, comparators, outcomes, and/or settings and all featured missing data.
Discussion
The current evidence on the use of milrinone in critically ill adult patients with cardiac dysfunction suffers from considerable risks of both bias and random error and demonstrates no benefits. The use of milrinone for the treatment of critically ill patients with cardiac dysfunction can be neither recommended nor refuted. Future randomised clinical trials need to be sufficiently large and designed to have low risk of bias.
Electronic supplementary material
The online version of this article (doi:10.1007/s00134-016-4449-6) contains supplementary material, which is available to authorized users.
Keywords: Milrinone, Systematic review, Heart failure, Trial sequential analysis
Introduction
Milrinone (Corotrope®/Primacor®) is a type III phosphodiesterase inhibitor primarily used for inotropic support in the treatment of cardiac dysfunction. Although milrinone is implemented in several guidelines, its efficacy and safety profile remain controversial [1, 2].
Three meta-analyses have evaluated milrinone in critically ill patients [3–5]. One meta-analysis included adult cardiac surgery patients and observed that milrinone was associated with a significant increase in mortality while an update of the review found no significant effects [4, 5]. One other meta-analysis evaluated milrinone for the treatment of acute heart failure after acute myocardial infarction and suggested that milrinone might be safe and effective in these patients [3]. Unfortunately, only four trials with a limited number of 303 patients were included.
None of these meta-analyses met all key methodological criteria for being a systematic review [6]. None of them were based upon a previously published protocol [3–5]. They lacked or had insufficient assessment of the risk of bias, and bias risks were insufficiently incorporated in the analyses and conclusions. They also lacked sufficient evaluation of the risks of random errors [7–9]. Just one domain having unclear risk of bias or high risk of bias is potentially sufficient to bias the findings. Furthermore, none of the previous meta-analyses assessed the outcomes according to the patients’ perspective following the Grading of Recommendations Assessment, Development and Evaluation (GRADE) [10]. GRADE assesses the quality of evidence by evaluating risk of bias, heterogeneity, indirectness, imprecision and publication bias [10].
Our objective was to perform a systematic review with meta-analyses and trial sequential analysis (TSA) of randomised clinical trials (RCTs) according to The Cochrane Handbook for Systematic Reviews of Interventions and The Cochrane Hepato-Biliary Group Module comparing the benefits and harms of milrinone in critically ill adult patients with cardiac dysfunction [6, 7].
Methods
This systematic review was conducted according to our published protocol following the recommendations of The Cochrane Handbook for Systematic Reviews of Interventions and The Cochrane Hepato-Biliary Group Module and reported according to the PRISMA statement [6, 7, 11]. The protocol for this systematic review was registered at PROSPERO (no. CRD42014009061) [12].
Eligibility criteria
We considered all randomised clinical trials for inclusion, irrespective of language, blinding, publication status or sample size for assessment of benefits and harms. Quasi-randomised studies and observational studies with more than 500 patients were not included regarding assessment of benefits, but were considered for inclusion regarding assessment of harms and were planned to be analysed separately from the randomised trials [6].
Only trials with adult patients having cardiac dysfunction were considered. Cardiac dysfunction was defined as left ventricular ejection fraction (LVEF) below 40 % and/or low cardiac output. Low cardiac output syndrome was defined as a pre-existing or developing state of cardiac insufficiency with underlying left or right ventricular systolic dysfunction requiring inotrope support [13]. We accepted the definitions of the diagnoses according to the criteria used in each individual randomised trial. Milrinone was considered the experimental intervention. There were no restrictions on dose, continuous or intermittent administration, or duration of treatment. However, trials with oral and/or inhaled milrinone were excluded as such routes of administration were judged inappropriate for critically ill patients.
All trials were included independent the type of control intervention, i.e., no intervention, placebo, dobutamine, levosimendan, or any other inotrope or vasopressor. While this may introduce heterogeneity, subgroup comparisons were preplanned according to inactive (placebo or no intervention) and potentially active control interventions (e.g., other inotropes or vasopressors).
All outcomes were graded according to the patients’ perspective following GRADE [9]. The primary outcome was serious adverse events (SAE). SAE is a composite outcome summarising all serious events necessitating an intervention, operation, prolonged hospital stay or mortality according to ICH-GCP definitions [14]. This outcome was chosen for balancing the potential benefits and harms. The secondary outcomes were all-cause mortality, myocardial infarction, arrhythmia (including supra- and ventricular tachycardia and ventricular fibrillation) and duration of mechanical ventilation. Time-specific analyses of mortality were conducted according to availability of data (e.g. 30, 90 and/or 180 days). Length of stay (both intensive care unit and total hospital stay) is a potentially highly biased surrogate outcome for recovery and was therefore not considered.
Search strategy
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library, PubMed/MEDLINE, EMBASE, Web of Science and CINAHL until November 2015 (see supplements). We searched the references of the identified trials and systematic reviews to identify any further relevant trials, i.e. backward snowballing. We also searched the WHO’s trial platform and ClinicalTrials.gov for ongoing trials and contacted the FDA and EMA.
Study selection and data extraction
Two authors independently identified the trials for inclusion. Excluded studies were listed with reasons for exclusion. The following data was extracted: year of publication, country in which the trial was conducted, year of conduct of the trial, single-centre or multicentre trial, inclusion and exclusion criteria, all outcomes, details on interventions and characteristics of the trials, e.g. baseline imbalance, early stopping and other than intention-to-treat analysis. The authors of the individual trials were contacted in case of any unclear or missing information.
Bias risk assessment
Two authors independently assessed the risks of bias of the trials following instructions in The Cochrane Handbook for Systematic Reviews of Interventions [6]. The following risk of bias domains were extracted from each trial: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and other bias including bias due to vested interest and/or academic bias [15–20]. Trials were classified as low risk of bias if all the domains were assessed as low risk. Trials were considered to have high risk of bias if one or more of these bias risk domains were scored as unclear or high risk of bias.
Error matrix approach
Data on the outcomes of all trials were assessed for the risks of bias (measured by the level of evidence), the risks of random error (measured by standard error) and design errors (measured by GRADING the outcomes) [21]. The three-dimensional Manhattan error matrix was used to facilitate the overview of available evidence at a glance [21].
Statistical analysis
We performed the meta-analyses according to The Cochrane Handbook for Systematic Reviews of Interventions [6] and The Cochrane Hepato-Biliary Group Module [7] and used the software package Review Manager 5.30 [22]. For TSA, the TSA program v.0.9beta (http://www.ctu.dk/tsa) was used [23].
Results were presented as relative risks (RR) with 95 % confidence interval (CI) if there were two or more trials for an outcome. For rare events (<5 % in the control group) we calculated odds ratios (OR) and for very rare events (<2 % in the control group) we calculated Peto’s OR with 95 % CI [24]. We also reported risk differences (RD) if conclusions were different from risk ratio. P values less than TSA-adjusted significance levels were considered statistically significant.
We calculated both a fixed-effect [25] and a random-effects [26] model for meta-analysis and presented both models in case of discrepancy. Considering the anticipated clinical heterogeneity we emphasised the random-effects model except if one or two trials dominated the available evidence [27]. Heterogeneity was explored by the Chi-squared test with significance set at a P value of 0.10, and the quantity was measured by I2 [6, 28].
Analyses were performed on intention-to-treat [6]. In case of statistically significant RR, we calculated the number needed to treat (NNT) or number needed to harm (NNH) with 95 % CI.
Predefined subgroup analyses were conducted according to (1) the bias risk of trials (low risk of bias compared to trials with unclear and high risk of bias; hypothesis: trials with unclear or high risk of bias are associated with more favourable beneficial effects); (2) the control intervention (inactive compared to potentially active; hypothesis: milrinone appears more favourable when compared to an inactive control intervention than potentially active control intervention); (3) clinical setting (patients having cardiac surgery compared to patients not having cardiac surgery; hypothesis: milrinone shows benefit in patients having cardiac surgery and not in other patients).
Funnel plots were used to explore small trial bias when data of more than ten randomised trials were available [6, 29, 30].
Trial sequential analysis (TSA)
We conducted TSA to control the statistically significance levels when data are reanalysed repetitively or are too sparse to draw firm conclusions, and accordingly, appropriately widen the confidence intervals [8, 9, 31–33]. TSA depends on the quantification of the required information size (the meta-analysis sample size). We calculated the diversity (D2)-adjusted required information size (DARIS) for a random-effects meta-analysis [34]. Trial sequential monitoring boundaries cannot be calculated when less than 5 % of the DARIS has been accrued. We conducted TSA with the intention to maintain an overall 5 % risk of a type I error and a power of 90 %. We used the unweighted control event proportion in the control group and we anticipated an intervention effect of a 10 % relative risk reduction (RRR). Sensitivity analyses were conducted using an RRR of 20 % as well as the lower confidence limit of the RRR of the intervention effect suggested by the meta-analysis of the trials with low risk of bias [27]. We intended to provide the CI adjusted for sparse data and repetitive testing, which we describe as the TSA-adjusted CI.
GRADE approach
We used the GRADE system to assess the quality of the body of evidence associated with each of the major outcomes in our review using GRADE software (ims.cochrane.org/revman/other-resources/gradepro) [10]. The quality measure of a body of evidence considers within-study risk of bias, indirectness, heterogeneity, imprecision and risk of publication bias.
Results
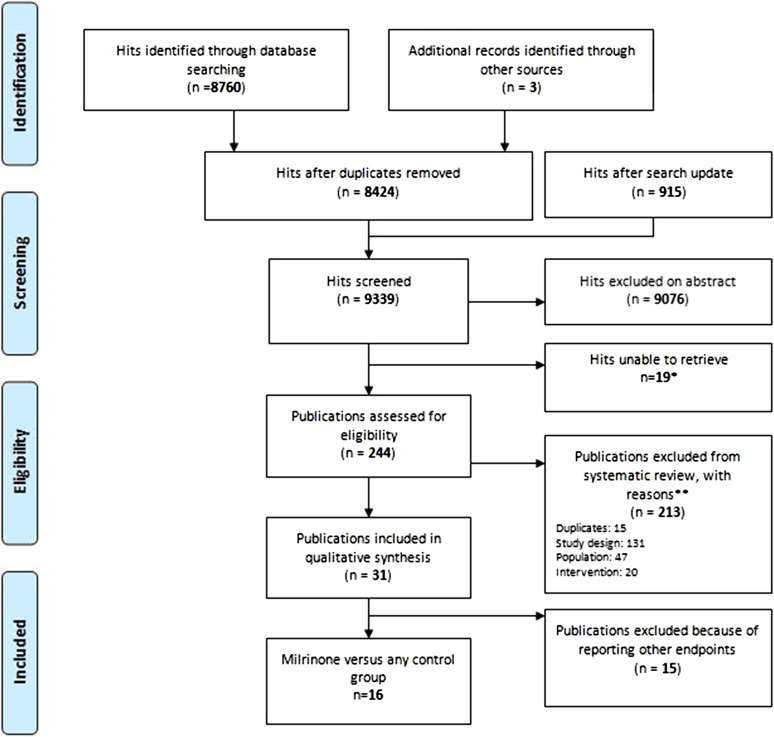
The search strategy identified 9336 hits (Fig. 1). Three additional publications were identified by backward snowballing: two could be included [35, 36] and one was irretrievable [37]. After removal of duplicates and screening, 244 hits remained. Of the 244 hits, 213 were excluded after full text evaluation. The remaining 31 publications were included in this systematic review. All authors of the 31 publications were contacted for missing data; only three authors responded [38–40], but no additional data was obtained. Of the 31 publications, 15 evaluated only surrogate outcomes (such as haemodynamic variables). Accordingly, only 16 randomised trials provided data for analyses [35, 36, 38, 40–52].
Fig. 1.
PRISMA flow diagram. Asterisk not available at Dutch libraries or the universities linked through the University of Groningen. Double asterisk study design: no RCT or prospective non-randomised <500 patients. Population: no cardiac dysfunction or low cardiac output syndrome. Intervention: not milrinone
No ongoing trials, quasi-randomised studies or observational studies were identified.
Characteristics of the included trials
The characteristics of the 16 randomised trials that provided data for analyses are listed (Table 1). Two trials used a three-arm parallel group design; all others had a two-arm parallel group design. There were five multicentre trials.
Table 1.
Baseline characteristics of included trials
| Trial | Patients | Clinical setting | Milrinone bolus and infusion rate | Comparator | Outcomes |
|---|---|---|---|---|---|
| Cardiac surgery setting | |||||
| Doolan [46] | 30 | CHF, ONCAB and valve surgery | 50 µg/kg | Placebo (67 % received open label milrinone) | Primary: none Secondary: arrhythmia Other: none Surrogate: failure of weaning from CPB, haemodynamic and biochemical parameters |
| 0.5 µg/kg/min for minimum 4 h | |||||
| Feneck [38] | 120 | AHF, cardiac surgery | 50 µg/kg | Dobutamine 10 up to 20 µg/kg/min if clinically indicated | Primary: none Secondary: MI, arrhythmias, hypotension Other: adverse events, severe low output state Surrogate: haemodynamic parameters |
| 0.5–0.75 µg/kg/min | |||||
| Möllhoff [51] | 30 | CHF, cardiac surgery | No bolus | Nifedipine 0.2 µg/kg/min for at least 24 h (dobutamine or epinephrine added when needed; no data) | Primary: mortality (1 year) Secondary: arrhythmias Other: hospital stay, angina pectoris at 1 year, NYHA at 1 year Surrogate: haemodynamic and biochemical parameters |
| 0.375 µg/kg/min for at least 24 h (dobutamine or epinephrine added when needed; no data) | |||||
| Al-Shawaf [41] | 30 | CHF, cardiac (valve) surgery | 50 µg/kg | Levosimendan bolus 12 µg/kg followed by 0.1–0.2 µg/kg/min for 24 h | Primary: mortality (48 h) Secondary: MI, arrhythmias, mechanical ventilation Other: renal replacement therapy Surrogate: haemodynamic parameters |
| 0.3–0.5 µg/kg/min for 24 h | |||||
| Brackbill [43] | 40 | CHF, cardiac surgery | 50 µg/kg | Nesiritide bolus 2 µg/kg with infusion 0.01 µg/kg/min for approx. 24 h (30 % received epinephrine; 40 % dopamine) | Primary: mortality (30 days) Secondary: none Other: renal failure, length of ICU and hospital stay Surrogate: haemodynamic parameters |
| 0.375 µg/kg/min for approx. 24 h (20 % received epinephrine; 35 % dopamine) | |||||
| De Hert [45] | 30 | CHF, cardiac surgery | No bolus | Levosimendan 0.1 µg/kg/min maximum 24 h (+dobutamine 5 µg/kg/min) | Primary: mortality (30 days) Secondary: MI, arrhythmias, mechanical ventilation Other: length of ICU and hospital stay Surrogate: biochemical and haemodynamic parameters |
| 0.5 µg/kg/min (+dobutamine 5 µg/kg/min) | |||||
| Jebeli [48] | 70 | CHF, ONCAB | 50 µg/kg | Placebo (>90 % received dopamine) | Primary: mortality (until ICU discharge) Secondary: MI, arrhythmia, mechanical ventilation Other: myocardial ischemia, non-myocardial ischemic events, renal failure, duration of CPB, inotropic support and ICU stay Surrogate: biochemical parameters, need for IABP |
| 0.5 µg/kg/min for 24 h (>90 % received dopamine) | |||||
| Hadadzadeh [47] | 80 | CHF, OPCAB | 50 µg/kg | Placebo (52.5 % received other ‘inotropic support’) | Primary: mortality (until ICU discharge) Secondary: MI, arrhythmia, mechanical ventilation Other: myocardial ischemia, ICU stay, inotropic support duration, renal failure, non-myocardial ischemic events Surrogate: need for IABP, biochemical parameters |
| 0.5 µg/kg/min for 24 h (47.5 % received other ‘inotropic support’) | |||||
| Non-cardiac surgery setting | |||||
| Biddle [42] | 79 | CHF | 50 or 75 µg/kg | Dobutamine 2.5 µg/kg/min, increased to max. 15.0 µg/kg/min | Primary: mortality (48 h) Secondary: arrhythmias Other: adverse reactions Surrogate: haemodynamic parameters |
| 0.5 up to 0.75 or 1.0 µg/kg/min | |||||
| Karlsberg [49] | 30 | AHF post MI | 50 µg/kg | Dobutamine 2.5 µg/kg/min titrated to a max. of 15 µg/kg/min | Primary: mortality (24 h) Secondary: arrhythmias Other: adverse events Surrogate: echocardiographic and haemodynamic parameters |
| First 3 h up titration from 0.5, 0.62 to 0.75 µg/kg/min and then 0.25–0.75 µg/kg/min | |||||
| Siostrzonek [50] | 20 | CHF | No bolus | Conventional (+dobutamine) | Primary: mortality (24 h) Secondary: none Other: length of ICU stay Surrogate: days until complete weaning from catecholamine, haemodynamic and biochemical parameters |
| 0.5 µg/kg/min > 24 h (+dobutamine) | |||||
| Cuffe [44] | 949 | AHF, CHF | No bolus | Placebo (9.3 % received dobutamine) | Primary: mortality (60 days) Secondary: SAE, MI, arrhythmias, hypotension Other: length of stay Surrogate: none |
| 0.5 µg/kg/min, titrated to 0.375–0.75 µg/kg/min and maintained for 48–72 h (11.5 % received dobutamine) | |||||
| Aranda [40] | 36 | CHF, awaiting Htx | No bolus | Dobutamine 2.5 µg/kg/min titrated 2.5 µg/kg/min to a max. 10 µg/kg/min (18 % received dopamine) | Primary: mortality (until hospital discharge) Secondary: arrhythmias Other: Htx, inotrope (bridge to Htx), LVAD (bridge to Htx), IABP (bridge to Htx), length of stay Surrogate: switched to alternate drug, haemodynamic parameters, cost-effectiveness |
| 0.25 µg/kg/min, titrated 0.125 µg/kg/min to max. 0.75 µg/kg/min (32 % received dopamine) | |||||
| Yang [36] | 120 | AHF post MI | No bolus | Control | Primary: mortality (7 days) Secondary: none Other: none Surrogate: echocardiographic, haemodynamic and biochemical parameters |
| 0.5 µg/kg/min for 5 h once a day for 7 days | |||||
| Pang [35] | 50 | AHF post MI | 50 µg/kg | Placebo (+dobutamine) | Primary: mortality (5 days) Secondary: none Other: none Surrogate: gastrointestinal reaction, haemodynamic parameters |
| 0.5 µg/kg/min (+dobutamine) | |||||
| Wang [52]a | 60 | Sepsis | 30 µg/kg | Control | Primary: mortality (28 days) Secondary: none Other: adverse events, ICU/hospital stay Surrogate: haemodynamic and biochemical parameters |
| 0.375–0.5 µg/kg/min | |||||
The maximal length of follow-up for the outcome mortality is reported between quotation marks in the ‘Outcomes’ column
AHF acute heart failure, CHF chronic heart failure, CPB cardiac pulmonary bypass, Htx heart transplant, IABP intra-arterial balloon pump, ICU intensive care unit, LVAD left ventricular assist device, MI myocardial infarction, ONCAB on-pump coronary artery bypass graft, OPCAB off-pump coronary artery bypass graft, SAE serious adverse events
aOnly the comparison between milrinone and control was included
Eight trials evaluated patients after cardiac surgery [38, 41, 43, 45–48, 51], four trials evaluated patients with chronic heart failure [40, 42, 44, 50], three trials evaluated patients with acute heart failure after acute myocardial infarction [35, 36, 49] and one trial evaluated patients with severe sepsis [52].
Milrinone was administered in different doses. Nine trials used a 50 µg/kg bolus and one trial a 30 µg/kg bolus. Continuous infusion rates ranged from 0.25 to 1.0 µg/kg/min. Eight trials used an inactive comparator and eight trials used a potentially active comparator, including catecholamines, dobutamine, levosimendan, nifedipine or nesirrtide. Many trials applied milrinone as an add-on intervention to standard care including other inotropes.
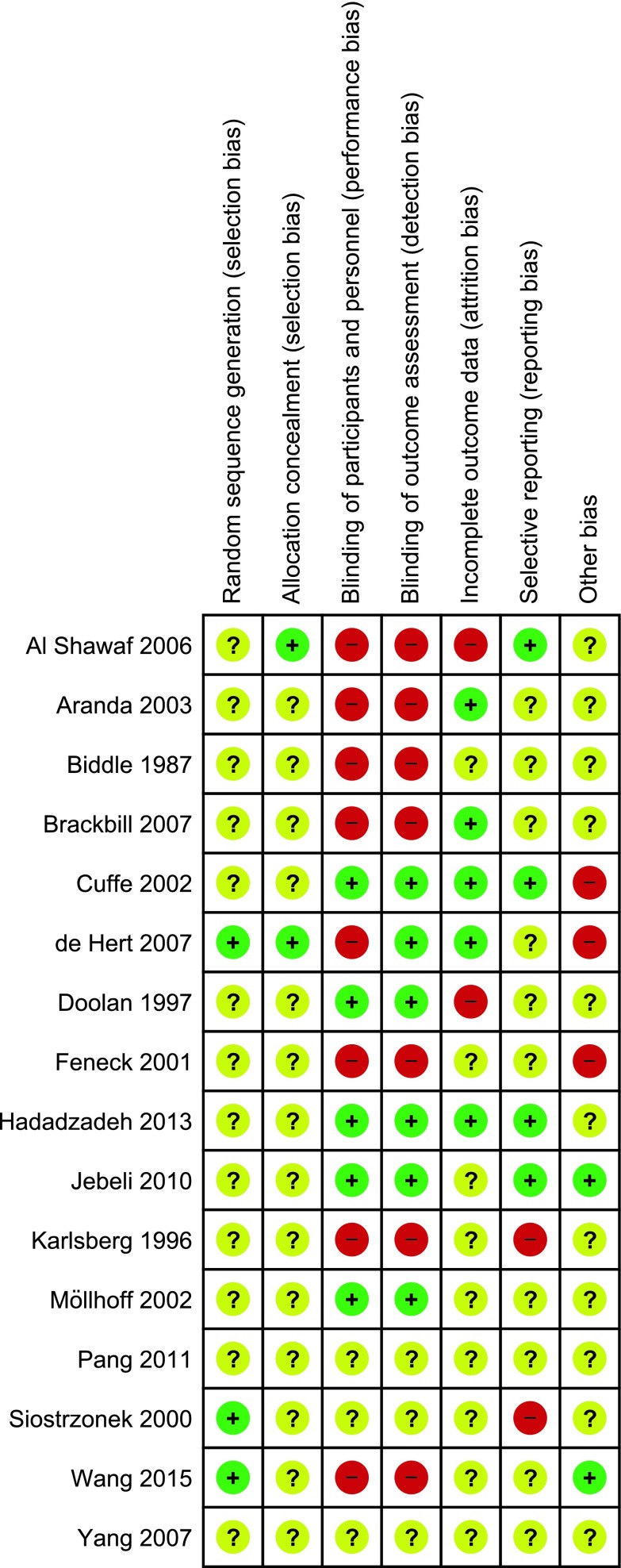
Bias risk assessment
Three trials (19 %) had low risk of bias regarding sequence generation, two trials (13 %) had low risk of bias regarding allocation concealment, five trials (31 %) had low risk of bias regarding blinding of participants, six trials (38 %) had low risk of bias regarding blinding of outcome assessors, five trials (31 %) had low risk of bias regarding incomplete outcome data, four trials (25 %) were without selective outcome reporting and two trials (13 %) were assessed as low risk of bias concerning industry and/or academic bias (Fig. 2). Accordingly, all trials were assessed as high risk of bias.
Fig. 2.
Risk of bias assessment. Review of authors’ judgements about each risk of bias domain for each included study. Red high risk, green low risk, yellow unclear
Outcomes
The pooled intervention effect estimates with the 95 % CI of the outcomes are specified according to control intervention and setting (Table 2 and supplements).
Table 2.
Conventional risk ratios with 95 % confidence intervals (CI) for the evaluated outcome measures including all patients stratified by intervention
| Number of trials | Number of patients | Conventional meta-analysis | ||
|---|---|---|---|---|
| RR with 95 % CI | Test of interaction | |||
| Mortality | ||||
| Inactive control | 5 | 1267 | 0.99 (0.77–1.27) | |
| Potentially active control | 9 | 344 | 0.76 (0.31–1.89) | |
| Any control | 14 | 1611 | 0.96 (0.76–1.21) | P = 0.59 |
| MI | ||||
| Inactive control | 3 | 1060 | 0.54 (0.11–2.69) | |
| Potentially active control | 2 | 60 | 1.09 (0.36–3.29) | |
| Any control | 5 | 1120 | 0.73 (0.25–2.09) | P = 0.48 |
| VT/VF | ||||
| Inactive control | 4 | 1087 | 0.80 (0.40–1.61) | |
| Potentially active control | 3 | 139 | 1.11 (0.58–2.15) | |
| Any control | 7 | 1226 | 0.96 (0.65–1.41) | P = 0.50 |
| SVT | ||||
| Inactive control | 2 | 988 | 1.43 (0.80–2.54) | |
| Potentially active control | 2 | 150 | 0.60 (0.13–2.70) | |
| Any control | 4 | 1138 | 0.89 (0.43–1.87) | P = 0.29 |
| MV durationa | ||||
| Inactive control | 2 | 150 | −2.85 (−5.00 to −0.69) | |
| Potentially active control | 2 | 60 | 12.66 (−3.48 to 28.80) | |
| Any control | 4 | 210 | 1.03 (−4.87 to 6.93) | P = 0.06 |
All pooled estimates are reported using risk ratio and calculated using a random-effects model unless stated otherwise. TSA adjusted risk ratios with the predefined α = 0.05 (two sided), β = 0.10 (power 90 %) and an anticipated relative risk increase of 10 % could not be calculated in any outcome with <5 % of the DARIS accrued
DARIS diversity adjusted required information size, MI myocardial infarction, SVT supraventricular tachyarrhythmia, VT/VF ventricular tachyarrhythmia, MV mechanical ventilation
aMV duration is reported in mean difference with 95 % CI
In the absence of trials that reported the primary composite outcome SAE including mortality, we have chosen to report all-cause mortality at maximum follow-up as the most important outcome. There were insufficient data for time-specific analyses of mortality. Meta-regression was not performed because of insufficient data.
Subgroup analyses according to risk of bias were not performed as no trial was assessed as having low risk of bias.
All analyses were conducted with stratification by control intervention, unless stated otherwise.
Comparison 1: all critically ill patients with cardiac dysfunction
All-cause mortality
Fourteen trials with 1611 randomised patients reported mortality. Pooled data showed that mortality at maximal follow-up was 11 % in both groups (RR 0.96; 95 % CI 0.76–1.21; I2 0 %; Fig. 3).
Fig. 3.
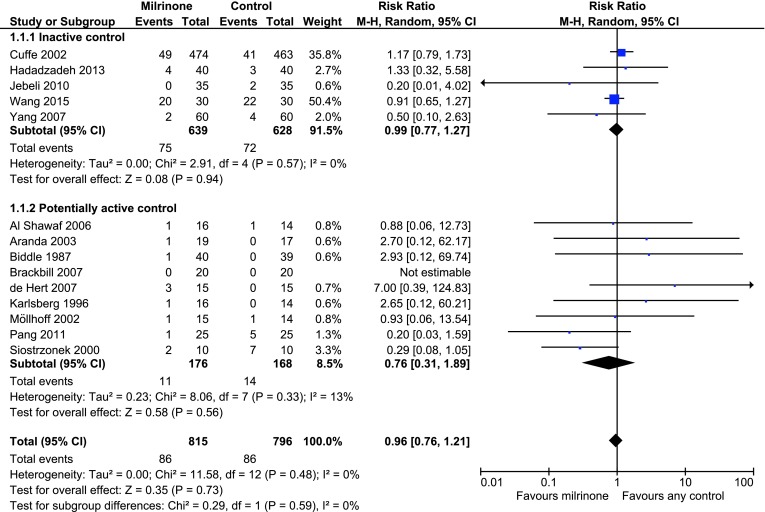
Forest plot of all-cause mortality in trials stratified by intervention. Size of squares for risk ratio (RR) reflects the weight of the trial in the pooled analyses. Horizontal bars 95 % confidence intervals (CI)
Subgroup analyses on type of control intervention and clinical setting showed differences in mortality event proportions in the control groups (inactive control group 0–70 %; potentially active control group 9–73 %; cardiac surgery setting control group 0–7 %; non-cardiac surgery setting control group 0–73 %), but tests of interaction showed no statistically significant differences between the groups (P = 0.59 and P = 0.83, respectively; Table 2 and supplements). No comparison could be analysed with TSA using the prespecified type I error of 5 % and type II error of 10 % because less than 5 % of DARIS was accrued.
As a sensitivity analysis, we conducted TSA with an RRR of 20 % and power of 80 % which showed that 20 % of the data was accrued and thousands of additional randomised patients are needed before futility or the required information size will be reached (RR 0.96; TSA adjusted CI 0.60–1.53; see supplements).
Myocardial infarction
Five trials with 1120 patients reported myocardial infarction (MI). MI at maximal follow-up occurred in 3 % in the inactive control group versus 15 % in the potentially active control group. Two small trials [41, 45] had a potentially active control group. There were no statistically significant differences in MI between milrinone and any control group (RR 0.73; 95 % CI 0.25–2.09; I2 61 %, P = 0.48; Table 2). No comparison could be analysed with TSA using the prespecified type I error of 5 % and type II error of 10 % because less than 5 % of DARIS was accrued.
Subgroup analyses based on clinical setting revealed discrepancy between fixed- and random-effects models driven by different weighting of one trial with 94 % relative risk reduction (random-effects model RR 0.53; 95 % CI 0.24–1.17, and fixed-effect model RR 0.45; 95 % CI 0.25–0.81; I2 34 %; see supplements) [48].
Other outcomes
Ventricular tachyarrhythmias [i.e. ventricular tachycardia (VT)/ventricular fibrillation (VF)] were reported in seven randomised trials (1226 patients) with equal event rate percentages (7 %) in both groups (RR 0.96; 95 % CI 0.65–1.41; I2 0 %). No comparison could be analysed with TSA using the prespecified type I error of 5 % and type II error of 10 % because less than 5 % of DARIS was accrued.
The pooled results and the subgroup analyses showed no associations between milrinone and ventricular tachyarrhythmia (see supplements).
Supraventricular tachyarrhythmia’s (SVT) were reported in four trials (1138 patients). There was a statistically significant heterogeneity between the trials in both subgroup analyses (both I2 55 %; P = 0.08). SVT varied from 5 to 18 % in the different subgroups (inactive versus potentially active and cardiac surgery versus non-cardiac surgery). Analyses of the pooled data (RR 0.89; 95 % CI 0.43–1.87) and the subgroups showed no significant associations (see supplements). No comparison could be analysed with TSA using the prespecified type I error of 5 % and type II error of 10 % since less than 5 % of DARIS was accrued.
Mechanical ventilation duration was reported in four trials (210 patients) in a cardiac surgery setting; duration ranged from 11 to 34 h in the control group and 10–65 h in the milrinone group. There was statistically significant heterogeneity (I2 80 %; P = 0.002). No significant differences were found. Test of interaction was not significant (P = 0.06).
Comparison 2: patients with cardiac dysfunction after cardiac surgery
All-cause mortality
Six trials with 279 randomised patients reported mortality data. Mortality at maximal follow-up was 4 % in both groups (RR 1.04; 95 % CI 0.30–3.63; I2 0 %). No comparison could be analysed with TSA using the prespecified type I and type II error because less than 5 % of DARIS was accrued.
Two trials used an inactive comparator and four trials used a potentially active comparator. No significant associations between milrinone and mortality were found (see supplements).
Myocardial infarction
MI was reported in four trials including 210 patients. There was significant statistical heterogeneity between the trials (I2 58 %; P = 0.09). There was discrepancy between the fixed- and the random-effects models driven by different weighting of one trial [48] (fixed-effect model RR 0.42; 95 % CI 0.21–0.86; random-effects model RR 0.47; 95 % CI 0.13–1.72; see supplements). No comparison could be analysed with TSA using the prespecified type I and type II error because less than 5 % of DARIS was accrued.
Other outcomes
Five trials with 240 patients documented ventricular tachyarrhythmia and no significant associations were found (see supplements).
SVTs were reported in three trials with 230 randomised patients and no significant associations were found between milrinone and SVTs (see supplements).
Comparison 3: patients with cardiac dysfunction not having cardiac surgery
All-cause mortality
Eight trials with 1332 randomised patients reported mortality. Mortality at maximal follow-up was 11 % in the milrinone group versus 12 % in the control group (RR 0.91; 95 % CI 0.64–1.28; I2 0 %). No comparison could be analysed with TSA using the prespecified type I error of 5 % and type II error of 10 % because less than 5 % of DARIS was accrued.
Three trials used an inactive control and five trials used a potentially active control. Subgroup analyses on type of control intervention showed no significant difference (test of interaction P = 0.34). No significant associations between milrinone and mortality were found (see supplements).
Other outcomes
Ventricular tachyarrhythmia’s (VT/VF) were reported in two trials (986 patients). No significant associations between milrinone and VT/VF were found (RR 1.19 95 % CI 0.68–2.06).
There was insufficient data on other secondary outcomes.
Error matrix approach
The Manhattan error matrix plots of milrinone showed that there is a similar amount of evidence regarding the benefits and harms of milrinone. All trials had high risks of systematic errors (bias) and the large majority of the trials also had high risks of random errors (see supplements).
Small trial bias
Funnel plots showed no clear arguments for small trial bias including publication bias (see supplements).
GRADE approach
The quality of the evidence was assessed as very low for all outcomes based on risk of bias limitations, indirectness, inconsistency, imprecision and other considerations. Table 3 shows the GRADEpro summary of findings table with stratification by control intervention.
Table 3.
GRADE pro summary of findings table of the outcomes of interest stratified by control intervention
| Quality assessment | No. of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Milrinone | Any control | Relative (95 % CI) | Absolute (95 % CI) | ||
| Serious adverse events—not reported | ||||||||||||
| – | – | – | – | – | – | – | – | – | – | – | – | Critical |
| Milrinone mortality at max FU comparator | ||||||||||||
| 14 | Randomised trials | Seriousa | Not seriousb | Seriousb,c,d | Very seriouse | Nonef | 86/815 (10.6 %) | 86/796 (10.8 %) | RR 0.96 (0.76 to 1.21) |
4 fewer per 1000 (from 23 more to 26 fewer) |
⨁◯◯◯ Very low |
Critical |
| 6.9 % | 3 fewer per 1000 (from 14 more to 17 fewer) |
|||||||||||
| Myocardial infarction | ||||||||||||
| 5 | Randomised trials | Seriousa | Seriousg | Seriousc,d | Very serious5 | None | 19/568 (3.3 %) | 26/552 (4.7 %) | RR 0.73 (0.25 to 2.09) |
13 fewer per 1000 (from 35 fewer to 51 more) |
⨁◯◯◯ Very low |
Important |
| 22.5 % | 61 fewer per 1000 (from 169 fewer to 245 more) |
|||||||||||
| Ventricular arrhythmias | ||||||||||||
| 7 | Randomised trials | Seriousa | Not serioush | Seriousc,d | Very seriouse | None | 41/622 (6.6 %) | 42/604 (7.0 %) | RR 0.96 (0.65 to 1.41) |
3 fewer per 1000 (from 24 fewer to 29 more) |
⨁◯◯◯ Very low |
Important |
| 5.1 % | 2 fewer per 1000 (from 18 fewer to 21 more) |
|||||||||||
| Supraventricular arrhythmias | ||||||||||||
| 4 | Randomised trials | Seriousa | Seriousg | Seriousc,d | Very seriouse | None | 38/577 (6.6 %) | 36/561 (6.4 %) | RR 0.89 (0.43 to 1.87) |
7 fewer per 1000 (from 37 fewer to 56 more) |
⨁◯◯◯ Very low |
Not important |
| 12.9 % | 14 fewer per 1000 (from 74 fewer to 112 more) |
|||||||||||
| Mechanical ventilation duration | ||||||||||||
| 4 | Randomised trials | Seriousa | Seriousg | Very seriousc,d | Seriouse | None | – | MD 1.03 higher (4.87 lower to 6.93 higher) |
⨁◯◯◯ Very low |
Not important | ||
CI confidence interval, RR risk ratio, MD mean difference
aNo trial with low risk of bias in all domains; many bias assessment items are not reported in the trials
bThere was considerable clinical heterogeneity in setting (reflected by >5 % difference in control event rate between populations) and comparator. All in all not enough to downgrade the evidence for inconsistency concerning the outcome mortality
cThere was considerable difference in dosing, titration and duration of milrinone; furthermore trials evaluated milrinone in a minority of trials against the most valuable inactive comparator (placebo); and even then different conventional inotropes were used between the trials
dMost trials used surrogate outcomes instead of patient-important outcomes
eMany trials with few patients and few events; less than 5 % of DARIS accrued
fFunnel plots showed no clear asymmetry
gThere was considerable clinical and statistical heterogeneity
hDespite different clinical settings and interventions the CI were overlapping and statistical heterogeneity was low
Discussion
Our systematic review evaluating the effects of milrinone for critically ill adult patients with cardiac dysfunction found few data on outcomes critical for decision making. Thirty-one randomised clinical trials fulfilled our inclusion criteria. All included trials had high risk of bias, most as a result of not reporting bias protection, and nearly all trials had large risks of random errors. Fifteen trials only reported surrogate outcomes. No trial reported the primary outcome, SAE (including mortality). All-cause mortality was reported in 14 trials with 1611 patients. No significant effect on any patient-centred outcome was found.
A general issue is that systematic reviews depend on the strengths of the included randomised trials. Trials with unclear or high risks of bias are associated with overestimation of benefits and underestimation of harms [15, 16, 18, 19]. The unknown true intervention effect may be beneficial, neutral or harmful. Previous meta-analyses on milrinone differ in design from our systematic review and they come to different conclusions [3–5]. One study focussed only on patients with myocardial infarction [3] and two only on cardiac surgery patients, in which the latter was an update [4, 5]. The meta-analysis on patients with myocardial infarction observed no significant effect on mortality, but stated that milrinone increased left ventricular ejection fraction and cardiac output [3]. The first meta-analysis evaluating patients having cardiac surgery suggested an increase in mortality using milrinone, which disappeared in the updated meta-analysis [4, 5]. Our prepublished protocol, a sensitive search strategy and thorough evaluations of the risks of systematic errors and random errors may explain differences with these previous publications [3–5]. First, previous meta-analyses ignored exploring associations of bias risk with intervention effect estimates. Final conclusions ought to be derived from trials with low risk of bias, of which there were none [6]. Second, despite including more patients (n = 1611) as compared to previous meta-analyses (n = 303 [3], n = 518 [4], n = 1037 [5]) the number of included patients is still far too small to draw any firm conclusions. We think that any significance needs the perspective of sample size considerations, in individual trials and also in meta-analyses [27, 31, 53–55]. Third, previous meta-analyses combined patients with normal cardiac functions [4, 5] and children [5] with patients with cardiac dysfunction into one pooled estimate. We included trials that randomised adult patients who had cardiac dysfunction. It is unlikely that patients benefit from milrinone when their cardiac function is unaffected, i.e. when the pathophysiological basis for cardiac stimulation is lacking.
Co-interventions with medications with an efficacy profile similar to milrinone might also have obscured results. Trials that evaluated milrinone versus placebo could also be considered add-on trials since co-interventions were allowed. The largest trial that evaluated milrinone versus placebo allowed at least co-interventions with dobutamine in their randomised patients; other inotropes were not reported [44]. The results of this trial suggest that milrinone may be harmful in patients with heart failure (LVEF <40 %) compared with standard treatment (ACE inhibitor and diuretics). Furthermore, the sickest patients were excluded in this trial [44]. For daily practice it is of utmost interest to know which vasopressor, inotrope, vasodilator or any combination is indicated for which patient and at what target [56, 57]. We found that for milrinone and levosimendan for critically ill adult patients with cardiac dysfunction evidence from trials with low risk of bias and low risk of random error is lacking to support its use [58]. Other interventions are currently being evaluated in systematic reviews which might feed future evidence-based guidance for clinicians or substantiate new trials.
Limitations
During the process of the systematic review we were non-adherent to our prepublished protocol for several reasons. We rephrased the title and terminology for an improved description of the cardiac state of the patients at interest (i.e. cardiac dysfunction instead of cardiac support or myocardial dysfunction). We divided subgroup comparisons into inactive versus (potentially) active control interventions. Since no data was found on the predefined subgroup comparison milrinone versus vasopressors we were unable to report this comparison. There were also no data on the composite outcome SAE (mortality included) and, therefore, all-cause mortality became the most important outcome. The outcome hypotension was regarded as a surrogate outcome and therefore omitted.
We frequently found significant statistical heterogeneity, but even when absent, there was still considerable clinical heterogeneity in patients, interventions, comparators, outcomes or settings. Pooling the data was frequently considered disputable, even in the absence of statistically significant tests of interactions. One example is the pooled intervention effect estimate of mortality (comparison 1), which has low statistical heterogeneity (I2 0 %; P = 0.50) and no subgroup differences, but the clinical heterogeneity is obvious, also reflected by control event rates for all-cause mortality varying from 3.6 to 12.0 %. The large variety in types of control interventions further increases clinical heterogeneity.
Milrinone dose and duration varied among the included trials. Also, there were differences in definitions of outcomes. Further, 15 trials evaluated surrogate outcomes, such as haemodynamic and biochemical parameters. Finally, most trials had short follow-up; only one trial evaluated 1-year follow-up [51], so that mortality analyses reflect rather short follow-up.
Conclusions
The quantity and quality of evidence for benefit or harm of milrinone in critically ill adult patients with cardiac dysfunction are very low because of high risks of systematic and random errors. Future randomised clinical trials need to be large and well designed by following SPIRIT guidelines and reported according to CONSORT guidelines. The widespread use of milrinone in critical care cannot be advocated or refuted on the basis of the current evidence.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We thank Sarah Louise Klingenberg, the Trial Search Coordinator of The Cochrane Hepato-Biliary Group at the Copenhagen Trial Unit, for her assistance with the search strategy. We thank Lu Yeh for her assistance with the Chinese translations.
Abbreviations
- AHF
Acute heart failure
- CHF
Chronic heart failure
- CPB
Cardiopulmonary bypass
- DARIS
Diversity adjusted required information size
- GRADE
Grade of Recommendations Assessment, Development and Evaluation
- ICU
Intensive care unit
- LVEF
Left ventricular ejection fraction
- MI
Myocardial infarction
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- RCT
Randomised controlled trial
- SAE
Serious adverse events
- SE
Standard error
- SVT
Supraventricular tachyarrhythmia
- TSA
Trial sequential analysis
- VF
Ventricular fibrillation
- VT
Ventricular tachycardia
Compliance with ethical standards
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
G. Koster and H. J. Bekema contributed equally to this work.
References
- 1.McMurray JJV, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–1847. doi: 10.1093/eurheartj/ehs104. [DOI] [PubMed] [Google Scholar]
- 2.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary. J Am Coll Cardiol. 2013;62:1495–1539. doi: 10.1016/j.jacc.2013.05.020. [DOI] [Google Scholar]
- 3.Tang X, Liu P, Li R, et al. Milrinone for the treatment of acute heart failure after acute myocardial infarction: a systematic review and meta-analysis. Basic Clin Pharmacol Toxicol. 2015;117:186–194. doi: 10.1111/bcpt.12385. [DOI] [PubMed] [Google Scholar]
- 4.Zangrillo A, Biondi-Zoccai G, Ponschab M, et al. Milrinone and mortality in adult cardiac surgery: a meta-analysis. J Cardiothorac Vasc Anesth. 2012;26:70–77. doi: 10.1053/j.jvca.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Majure DT, Greco T, Greco M, et al. Meta-analysis of randomized trials of effect of milrinone on mortality in cardiac surgery: an update. J Cardiothorac Vasc Anesth. 2013;27:220–229. doi: 10.1053/j.jvca.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 6.The Cochrane Collaboration (2011). In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1.0. http://www.handbook.cochrane.org. Accessed 14 June 2016
- 7.Gluud C, Nikolova D, Klingenber SL et al (2015) Cochrane Hepato-Biliary Group. About The Cochrane Collaboration (Cochrane Review Groups (CRGs)) 2015, issue 4. Art. No.:LIVER
- 8.Brok J, Thorlund K, Wetterslev J, Gluud C. Apparently conclusive meta-analyses may be inconclusive—trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta-analyses. Int J Epidemiol. 2009;38:287–298. doi: 10.1093/ije/dyn188. [DOI] [PubMed] [Google Scholar]
- 9.Thorlund K, Devereaux PJ, Wetterslev J, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int J Epidemiol. 2009;38:276–286. doi: 10.1093/ije/dyn179. [DOI] [PubMed] [Google Scholar]
- 10.Guyatt GH, Oxman AD, Kunz R, et al. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, For the PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 [PMC free article] [PubMed] [Google Scholar]
- 12.Bekema HJ, Koster G, Wetterslev J et al (2014) Milrinone for cardiac support: a systematic review of randomised clinical trials with meta-analyses and trial sequential analyses. In: PROSPERO 2014:CRD42014009061. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014009061. Accessed 30 May 2016 [DOI] [PMC free article] [PubMed]
- 13.Rao V, Ivanov J, Weisel RD, et al. Predictors of low cardiac output syndrome after coronary artery bypass. J Thorac Cardiovasc Surg. 1996;112:38–51. doi: 10.1016/S0022-5223(96)70176-9. [DOI] [PubMed] [Google Scholar]
- 14.ICH Harmonised Tripartite Guideline Clinical safety data management: definitions and standards for expedited reporting. Fed Regist. 1995;60:11284–11287. [Google Scholar]
- 15.Wood L, Egger M, Gluud LL, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336:601–605. doi: 10.1136/bmj.39465.451748.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.1995.03520290060030. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Jadad AR, Tugwell P. Assessing the quality of randomized controlled trials. Current issues and future directions. Int J Technol Assess Health Care. 1996;12:195–208. doi: 10.1017/S0266462300009570. [DOI] [PubMed] [Google Scholar]
- 18.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135:982–989. doi: 10.7326/0003-4819-135-11-200112040-00010. [DOI] [PubMed] [Google Scholar]
- 19.Savović J, Jones HE, Altman DG, et al. Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Ann Intern Med. 2012;157:429–438. doi: 10.7326/0003-4819-157-6-201209180-00537. [DOI] [PubMed] [Google Scholar]
- 20.Lundh A, Gøtzsche PC. Recommendations by Cochrane review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. 2008;8:22. doi: 10.1186/1471-2288-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keus F, Wetterslev J, Gluud C, van Laarhoven CJHM. Evidence at a glance: error matrix approach for overviewing available evidence. BMC Med Res Methodol. 2010;10:90. doi: 10.1186/1471-2288-10-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Cochrane Collaboration (2014) Review Manager (RevMan) [Computer Program] Version 5.3 Copenhagen. The Nordic Cochrane Centre
- 23.Thorlund K, Engstrøm J, Wetterslev J, Brok J, Imberger G, Gluud C (2011) User manual for trial sequential analysis (TSA). http://ctu.dk/tsa/files/tsa_manual.pdf. Accessed 1 Jan 2016
- 24.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 25.Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med. 1987;6:341–350. doi: 10.1002/sim.4780060325. [DOI] [PubMed] [Google Scholar]
- 26.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 27.Jakobsen JC, Wetterslev J, Winkel P, et al. Thresholds for statistical and clinical significance in systematic reviews with meta-analytic methods. BMC Med Res Methodol. 2014;14:120. doi: 10.1186/1471-2288-14-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 29.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001;20:641–654. doi: 10.1002/sim.698. [DOI] [PubMed] [Google Scholar]
- 31.Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol. 2008;61:64–75. doi: 10.1016/j.jclinepi.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 32.Wetterslev J, Engstrøm J, Gluud C, Thorlund K (2012) Trial sequential analysis: methods and software for cumulative meta-analyses. In: Chandl J, Clarke M, Higgins J (eds) Cochrane methods, Cochrane DB Syst Rev Suppl 1, pp 1–56
- 33.Pogue JM, Yusuf S. Cumulating evidence from randomized trials: utilizing sequential monitoring boundaries for cumulative meta-analysis. Control Clin Trials. 1997;18:580–593. doi: 10.1016/S0197-2456(97)00051-2. [DOI] [PubMed] [Google Scholar]
- 34.Wetterslev J, Thorlund K, Brok J, Gluud C. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol. 2009;9:86. doi: 10.1186/1471-2288-9-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pang Z, Zhao W. Milrinone in treatment of patients with cardiac shock following acute myocardial infarction. J Clin Med Pr. 2011;15:82–83. [Google Scholar]
- 36.Yang G, Han Y, Tong M, Deng J. Milrinone in treatment of patients with acute myocardial infarction and acute left heart failure. Chin Heart J. 2007;19:454–456. [Google Scholar]
- 37.Tang X, Li R, Jing Q, et al. Observation on the clinical efficacy of milrinone in the treatment of heart failure patients with acute myocardial infarction. J Clin Med Pr. 2012;16:163–165. [Google Scholar]
- 38.Feneck RO, Sherry KM, Withington PS, Oduro-Dominah A. Comparison of the hemodynamic effects of milrinone with dobutamine in patients after cardiac surgery. J Cardiothorac Vasc Anesth. 2001;15:306–315. doi: 10.1053/jcan.2001.23274. [DOI] [PubMed] [Google Scholar]
- 39.Heringlake M, Wernerus M, Grünefeld J, et al. The metabolic and renal effects of adrenaline and milrinone in patients with myocardial dysfunction after coronary artery bypass grafting. Crit Care. 2007;11:R51. doi: 10.1186/cc5904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aranda JM, Schofield RS, Pauly DF, et al. Comparison of dobutamine versus milrinone therapy in hospitalized patients awaiting cardiac transplantation: a prospective, randomized trial. Am Heart J. 2003;145:324–329. doi: 10.1067/mhj.2003.50. [DOI] [PubMed] [Google Scholar]
- 41.Al-Shawaf E, Ayed A, Vislocky I, et al. Levosimendan or milrinone in the type 2 diabetic patient with low ejection fraction undergoing elective coronary artery surgery. J Cardiothorac Vasc Anesth. 2006;20:353–357. doi: 10.1053/j.jvca.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 42.Biddle TL, Benotti JR, Creager Ma, et al. Comparison of intravenous milrinone and dobutamine for congestive heart failure secondary to either ischemic or dilated cardiomyopathy. Am J Cardiol. 1987;59:1345–1350. doi: 10.1016/0002-9149(87)90917-9. [DOI] [PubMed] [Google Scholar]
- 43.Brackbill ML, Stam MD, Schuller-Williams RV, Dhavle AA. Perioperative nesiritide versus milrinone in high-risk coronary artery bypass graft patients. Ann Pharmacother. 2007;41:427–432. doi: 10.1345/aph.1H500. [DOI] [PubMed] [Google Scholar]
- 44.Cuffe MS, Califf RM, Adams KF, et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure. JAMA. 2002;287:1541–1547. doi: 10.1001/jama.287.12.1541. [DOI] [PubMed] [Google Scholar]
- 45.De Hert SG, Lorsomradee S, Cromheecke S, Van der Linden PJ. The effects of levosimendan in cardiac surgery patients with poor left ventricular function. Anesth Analg. 2007;104:766–773. doi: 10.1213/01.ane.0000256863.92050.d3. [DOI] [PubMed] [Google Scholar]
- 46.Doolan LA, Jones EF, Kalman J, et al. A placebo-controlled trial verifying the efficacy of milrinone in weaning high-risk patients from cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 1997;11:37–41. doi: 10.1016/S1053-0770(97)90250-0. [DOI] [PubMed] [Google Scholar]
- 47.Hadadzadeh M, Hosseini SH, Mostafavi Pour Manshadi SM et al (2013) Effect of Milrinone on short term outcome of patients with myocardial dysfunction undergoing off-pump coronary artery bypass graft: a randomized clinical trial. Acta Med Iran 51(10):681–686 [PubMed]
- 48.Jebeli M, Ghazinoor M, Mandegar MH, et al. Effect of milrinone on short-term outcome of patients with myocardial dysfunction undergoing coronary artery bypass graft: a randomized controlled trial. Cardiol J. 2010;17:73–78. [PubMed] [Google Scholar]
- 49.Karlsberg RP, DeWood MA, DeMaria AN, et al. Comparative efficacy of short-term intravenous infusions of milrinone and dobutamine in acute congestive heart failure following acute myocardial infarction. Milrinone–Dobutamine Study Group. Clin Cardiol. 1996;19:21–30. doi: 10.1002/clc.4960190106. [DOI] [PubMed] [Google Scholar]
- 50.Siostrzonek P, Koreny M, Delle-Karth G, et al. Milrinone therapy in catecholamine-dependent critically ill patients with heart failure. Acta Anaesthesiol Scand. 2000;44:403–409. doi: 10.1034/j.1399-6576.2000.440408.x. [DOI] [PubMed] [Google Scholar]
- 51.Möllhoff T, Schmidt C, Van Aken H, et al. Myocardial ischaemia in patients with impaired left ventricular function undergoing coronary artery bypass grafting—milrinone versus nifedipin. Eur J Anaesthesiol. 2002;19:796–802. doi: 10.1017/s026502150200128x. [DOI] [PubMed] [Google Scholar]
- 52.Wang Z, Wu Q, Nie X, et al. Combination therapy with milrinone and esmolol for heart protection in patients with severe sepsis: a prospective, randomized trial. Clin Drug Investig. 2015;35:707–716. doi: 10.1007/s40261-015-0325-3. [DOI] [PubMed] [Google Scholar]
- 53.Pogue J, Yusuf S. Overcoming the limitations of current meta-analysis of randomised controlled trials. Lancet. 1998;351:47–52. doi: 10.1016/S0140-6736(97)08461-4. [DOI] [PubMed] [Google Scholar]
- 54.Imberger G, Gluud C, Boylan J, Wetterslev J. Systematic reviews of anesthesiologic interventions reported as statistically significant: problems with power, precision, and type 1 error protection. Anesth Analg. 2015;121:1611–1622. doi: 10.1213/ANE.0000000000000892. [DOI] [PubMed] [Google Scholar]
- 55.Roberts I, Ker K, Edwards P, et al. The knowledge system underpinning healthcare is not fit for purpose and must change. BMJ. 2015;350:h2463. doi: 10.1136/bmj.h2463. [DOI] [PubMed] [Google Scholar]
- 56.Lamontagne F, Meade MO, Hébert PC, et al. Canadian critical care trials group. Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Med. 2016;42:542–550. doi: 10.1007/s00134-016-4237-3. [DOI] [PubMed] [Google Scholar]
- 57.Mebazaa A, Tolppanen H, Mueller C, et al. Acute heart failure and cardiogenic shock: a multidisciplinary practical guidance. Intensive Care Med. 2016;42:147–163. doi: 10.1007/s00134-015-4041-5. [DOI] [PubMed] [Google Scholar]
- 58.Koster G, Wetterslev J, Gluud C, et al. Effects of levosimendan for low cardiac output syndrome in critically ill patients: systematic review with meta-analysis and trial sequential analysis. Intensive Care Med. 2015;41(2):203–221. doi: 10.1007/s00134-014-3604-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.