Abstract
Hospital readmissions in older adult populations are an emerging quality indicator for acute care hospitals. Recent evidence has linked functional decline during and after hospitalization with an elevated risk of hospital readmission. However, models of care that have been developed to reduce hospital readmission rates do not adequately address functional deficits. Physical therapists, as experts in optimizing physical function, have a strong opportunity to contribute meaningfully to care transition models and demonstrate the value of physical therapy interventions in reducing readmissions. Thus, the purposes of this perspective article are: (1) to describe the need for physical therapist input during care transitions for older adults and (2) to outline strategies for expanding physical therapy participation in care transitions for older adults, with an overall goal of reducing avoidable 30-day hospital readmissions.
Nearly 1 in 5 Medicare beneficiaries are readmitted to the hospital within 30 days after an acute hospitalization.1 Reduction of 30-day hospital readmissions is a major quality improvement goal for many acute care hospitals, partly in response to new Medicare rules that penalize hospitals that demonstrate higher-than-average readmission rates for populations of beneficiaries with certain target conditions.2 Currently, these Medicare target conditions include congestive heart failure, pneumonia, acute myocardial infarction, chronic obstructive pulmonary disease exacerbation, and total knee or hip arthroplasty.3 Thus, there is a strong impetus to develop care models that adequately address known risk factors for hospital readmissions during transitions from hospital to home. These risk factors include medical complexity, age, comorbidities, access to care, hospital length of stay, social support, and—of most relevance to rehabilitation professionals—impaired physical function.4–8
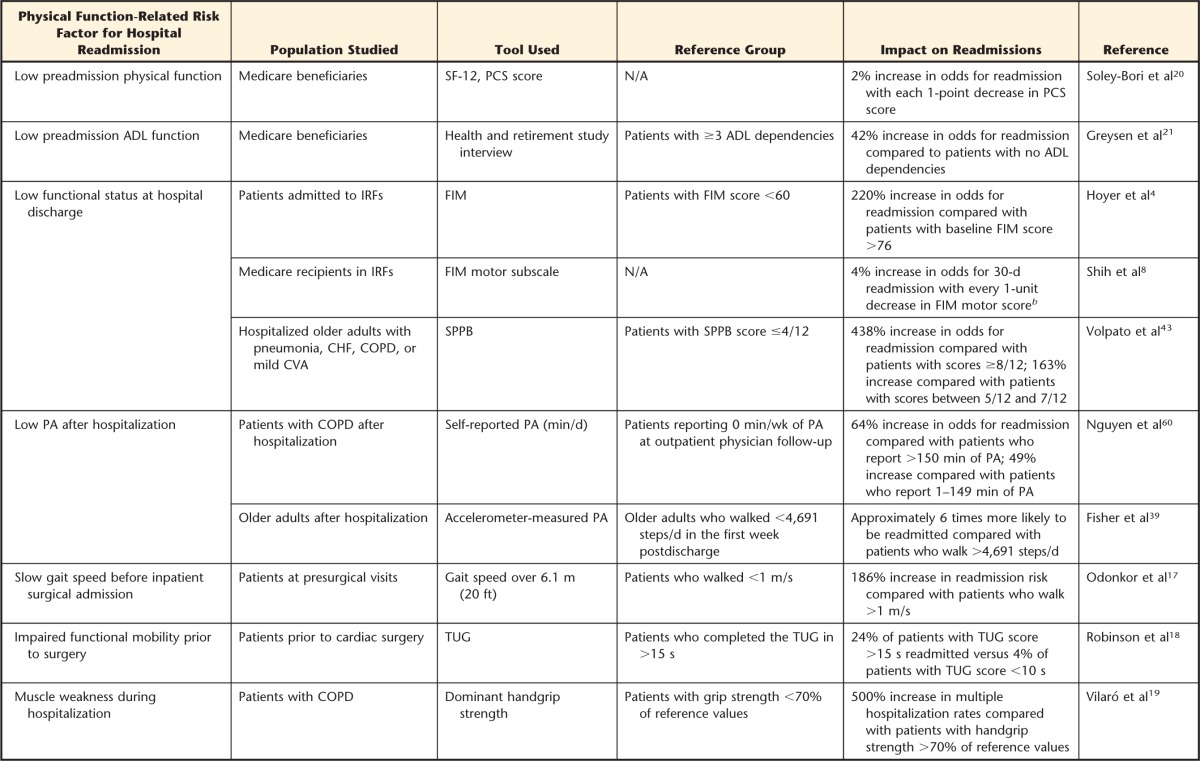
A number of care transition models have emerged to address the growing problem of hospital readmissions. These care models are designed to reduce the fragmentation of health care that occurs during the transfer from acute hospitalization to follow-up with an outpatient primary care provider.9–12 In general, care transition models are predicated on improving provider-to-provider communications, improving coordination of care, and educating patients on how to self-monitor and manage their medical conditions—these activities, when implemented systematically, have been shown to reduce hospital readmissions in controlled trials.13–16 However, to our knowledge, none of these innovative care transition models formally include physical therapist analysis of, or intervention on, known independent functional predictors of hospital readmission, such as gait speed,17,18 strength.19 or activities of daily living (ADL) ability20,21 (Tab. 1).
Table 1.
Overview of Functional Deficits Associated With Hospital Readmission Riska
SF-12=12-Item Short-Form Health Survey, PCS=Physical Component Summary scale, ADL=activities of daily living, IRF=inpatient rehabilitation facility, FIM=Functional Independence Measure, CHF=congestive heart failure, COPD=chronic obstructive pulmonary disease, CVA=cerebrovascular accident, SPPB=Short Physical Performance Battery, PA=physical activity, TUG=Timed “Up & Go“ Test, N/A=not applicable.
b Quadratic transformation of FIM scores used for modeling.
The paucity of physical therapy involvement in these models is concerning. Functional deficits represent an independent risk factor for hospital readmission and are potentially addressable with physical therapy interventions.22 Older adults with Medicare target conditions who receive physical therapist services during the period between hospital admission and 30 days postdischarge have fewer hospital readmissions23,24 and greater improvements in physical function.25 Thus, increasing physical therapist participation during care transitions may contribute to even better identification and treatment of those older adults at highest risk for a hospital readmission. Physical therapists may be the optimal medical professionals to identify and manage functional decline before, during, and after an acute hospitalization.
How Physical Therapists Could Participate in Care Transitions
The aims of this perspective article are: (1) to describe the need for physical therapist input to monitor and optimize changes in physical function during care transitions for older adults and (2) to outline strategies for expanding physical therapist participation in care transitions for older adults, with an overall goal of reducing avoidable 30-day hospital readmissions. We will use a validated framework that describes the care processes crucial to an ideal transition of care (ITC) developed by Burke and colleagues26,27 (Figure) and outline how physical therapists could contribute within such a model in a meaningful way. This framework provides a comprehensive overview of how medical teams can work collaboratively to bridge the treatment gap between hospital discharge and outpatient follow-up through improved discharge planning, coordination of care, and postdischarge monitoring of vulnerable older adults. We provide evidence-based recommendations for increasing physical therapy involvement in each domain of the ITC framework below, and these recommendations are summarized in Table 2.
Figure.
The ideal transition of care framework. Reprinted with permission of John Wiley & Sons from: Burke RE, Kripalani S, Vasilevskis EF, Schnipper JL. Moving beyond readmission penalties: creating an ideal process to improve transitional care. J Hosp Med. 2013;8:102–109.
Table 2.
Proposed Physical Therapist Contributions to Care Transitions for Older Adultsa

ADL=activities of daily living.
Discharge Planning
The ITC starts with discharge planning. Discharge planning occurs before the patient is discharged from the acute care hospital and ideally throughout the entirety of a hospital stay. Discharge planning includes input from multiple members of the health care team on location and services required for the next level of care. This process is a central role in the care practices of an acute care physical therapist28; hospital readmission rates after acute care discharge are 3 times higher if physical therapist discharge recommendations are replaced with less intensive interventions.29 However, the discharge planning process encompasses more than a recommendation of discharge location and services. For older adults being discharged to community settings, discharge planning also includes collaboration with community health care practitioners (which may include physical therapists) about the discharge and follow-up plan and arranging follow-up visits. Synchronous (eg, by telephone) communication occurs only 3% of the time between hospital physicians and community physicians.30 Likewise, acute care physical therapists are afforded insufficient (if any) time and opportunity to communicate synchronously with community physical therapy providers (home health or outpatient physical therapists) about the discharge and follow-up plan for older adults.
There is a paucity of research evaluating the content or frequency of communications that occur before hospital discharge between acute physical therapy providers and physical therapy providers in community settings, especially in the context of reducing hospital readmissions. Synchronous communications about function between acute care physical therapists and community clinicians prior to discharge should be included for older adults at high risk for readmissions. These communications could help ensure that the community clinician is able to see the patient in a timely manner after hospital discharge, is adequately informed about functional needs, and has the requisite expertise to manage the observed impairments appropriately.
Other key considerations in models of transitional care are ensuring that patients and caregivers are prepared for hospital discharge and empowering patients and caregivers to assert preferences during the discharge planning process. Optimal translation of discharge education into meaningful action in the home setting may occur if physical therapists provide discharge education not only on the day of discharge but throughout the inpatient stay.31 Providing education throughout the length of stay will allow a physical therapist to both solicit feedback from the patient and caregiver about the recommendations and probe for barriers to implementation.
When patients with medically complex conditions are more satisfied with the discharge planning and communication during a hospital stay, there is a decreased risk of 30-day readmissions.32 Descriptions of physical therapist practice in acute care settings suggest that physical therapists routinely include patients and solicit input from caregivers in discussions about the discharge planning process.28 This patient-centered process likely contributes to a reduction in hospital readmissions.33
Complete Communication of Information
At the time of discharge, a complete transfer of information is necessary for an ITC. The ITC framework suggests that the hospital discharge summary should include a complete information set with all relevant information needed for continuing the plan of care.26 However, hospitalists often do not include information about physical function in communications with primary care providers. Functional information is often crucial to coordinating community rehabilitation services34 (eg, certifying that a Medicare beneficiary is homebound). A lack of care coordination surrounding function, therefore, may leave older adults with unresolved biomarkers for further functional disability, hospital readmission, institutionalization, or death.21,35 Across older adults in a large academic medical center, a description of the patient's function compared with baseline is included in only 19% of discharge summaries; similarly, information about discharge physical function is included in only 26% of discharge summaries.36 Specific recommendations from physical therapists, including those regarding the needs for assistive devices or further physical therapist services, are completely missing from 55% of discharge summaries; these omissions are associated with increased risk of hospital readmission.37
Physical therapists can contribute to a complete communication of information by ensuring that documentation about the patient's functional recovery and discharge status is recorded in a timely manner during the hospital stay and is routinely included in any transfer of information to community providers. This process may be accomplished through developing standard information sets that populate automatically into physician discharge summaries or development of separate information sheets that are provided with discharge orders by the discharge planner or case manager. Functional status templates should include measures of the ability to carry out ADLs and measures of different but complementary functional domains38 known to affect readmissions, such as ambulatory ability39 and lower extremity strength.21 In addition, information about trajectory of recovery while in the hospital should be included in any transfer of information, as this information is prognostic for recovery and mortality after hospitalization.40,41 Measures such as gait speed42 or Short Physical Performance Battery score43 are sensitive to change during hospitalization, and data obtained with these measures may help inform discussions with physicians about recovery trajectory, especially for older adults who have not demonstrated an overt decline in ADL function.
Availability, Timeliness, Clarity, and Organization of Information
As older adults are being discharged from acute care hospital stays quicker and sicker,44 the availability, timeliness, clarity, and organization of discharge information are increasingly critical for ideal transitions to community settings. Because the transition from hospital to community settings often occurs without significant lead time, hospital discharge summaries are rarely ready at the time of discharge, and 66% to 88% of the time discharge summaries are still unavailable at the time of the scheduled community follow-up visits.30 This lack of timeliness and availability of discharge information affects care delivery at the physician provider level, and evidence suggests that home health and outpatient physical therapists experience similar concerns regarding availability and timeliness of hospital information.45 The clarity and organization of discharge information is also a concern, with community physicians reporting significantly greater ability to quickly ascertain relevant hospital information when it was presented in a standardized format with clear subheadings.46 Standardizing the presentation of information also has been shown to improve safety and communication regarding mobility impairments within rehabilitation settings.47
In addition to the complete transfer of information described previously, physical therapists can contribute to improving timeliness, availability, clarity, and organization of information by developing clear, standardized templates for reporting functional status to physicians that are included in hospital discharge summaries. Physical therapist participation has not yet been reported in the development of standardized content for hospital discharge summaries, but physical therapist input is likely valuable to develop optimal methods for communicating functional information in discharge summaries to community providers for further follow-up. Thus, it appears that physical therapists can contribute meaningfully to ideal transitions of care and The Joint Commission national patient safety goals48 by ensuring assessments of function with critical importance, such as a gait speed below 0.6 m/s, are communicated to the right person at the right time when older adults are discharged from the hospital.
Medication Safety
Medication safety is a central focus area for care transitions, given that adverse events related to medication management are among the leading causes of hospital readmission.49 Although physicians, nurses, and pharmacists are appropriately the primary drivers of the process of medication management and reconciliation during a hospital stay and at the time of discharge, physical therapists still have a small, albeit important, role in improving this process.
Identification of possible medication side effects that occur during mobility activities is an important insight that physical therapists could contribute during the ITC to reduce the risk of avoidable hospital readmissions. This identification may include communication about the presence of orthostatic hypotension during mobility tasks, fall risk for a patient taking anticoagulant medication, or the balance between function and pain control for a patient taking oral opioid analgesics. Additionally, information about vital sign (eg, heart rate, blood pressure) changes with exercise in the presence of medications (eg, beta-blockers) may be observed primarily by physical therapists in the immediate posthospitalization period. This information is likely valuable for providers in home health or outpatient settings who review medications as part of developing a follow-up plan of care. Increasing physical therapy participation in the medication safety domain of the ITC involves improving communication between community primary care providers and physical therapists when medication changes are implemented so that physical therapists can evaluate for and report any adverse effects on mobility, physical function, or safety.
Educating Older Adults to Promote Self-Management
Teaching older adults and caregivers about their medical condition and required follow-up care is the next essential step in an ITC. Promoting self-management involves education to older adults and caregivers on appropriate postdischarge management of a new surgical or medical diagnosis, written reminders of follow-up appointments, and education on risk factors (“red flags”) that indicate the need for immediate physician follow-up—all of which contribute to a reduction in avoidable hospital readmission. The role of the physical therapist in this process centers on self-management of mobility-related concerns, such as the appropriate device needed for ambulation, equipment needed for safety in the home, or the appropriate amount of assistance needed for ADLs. This process of education ideally should begin in the acute care setting and continue seamlessly through community settings via community physical therapists and physicians.
In addition to addressing older adults' immediate postdischarge needs, physical therapists in acute care and community settings should be involved in ongoing self-management needs, such as progressing older adults through a physical therapy plan of care, which requires identifying and addressing their changing symptoms and mobility needs. For example, physical therapists play a critical role in educating older adults about mobility-related red flags, such as slowing gait speed or new impairments in strength or ADL function that occur during care transitions. Evidence from a small prospective study suggests that older adults who walk <4,691 steps per day over the first week postdischarge are approximately 6 times more likely to be readmitted within 30 days.39 Similarly, a decline in self-reported ADL ability is strongly linked to poor outcomes following hospitalization.50 Thus, physical therapists can participate in improving patient self-management and reducing the risk of hospital readmission during care transitions by emphasizing to both older adults and caregivers the importance of monitoring and reporting declines in physical function. In a small quality improvement study on veterans following total knee arthroplasty, involving physical therapists in the mobility education given to older adults during care transitions resulted in a 36% reduction in hospital readmissions.24
For patients discharged from the hospital without physical therapy or those who did not see a physical therapist during their inpatient stay, education about self-management of physical function is still highly relevant but likely missing in current care transition models. Physical therapists could improve care transitions for these patients by developing general health and wellness educational materials that include strategies for maintaining function, improving physical activity, and reducing fall risk after hospitalization. Other educational materials that may be valuable for older adults include recommendations for group classes or wellness programs to supplement management of medical conditions (eg, a group exercise class for older adults with chronic heart failure). These materials and referrals for self-management activities could be disseminated to older adults by other members of the health care team, such as nurses, when discharge planning occurs without the direct input of a physical therapist.
Enlisting Help of Social and Community Supports
Determining an older adult's need for ongoing assistance in the community after hospital discharge is a shared responsibility between acute care and community practitioners during an ITC. The assessment of functional independence by acute care physical therapists helps guide discharge location. For older adults being discharged home, this assessment also guides recommendations for formal or informal ADL assistance in the community environment.28 Discharge planners then take this information and work to set up the needed resources to be available at the time of discharge and communicate these needs to community practitioners.
When discharge planning is fragmented or incomplete, information about functional or ADL assistance needs is often not appropriately communicated. This breakdown in communication is associated with an elevated risk for hospital readmission; older adults who return home with these unmet needs for ADL assistance have a 66% increase in the odds of hospital readmission compared with older adults discharged home at the same functional level whose needs are adequately addressed after discharge.51 Thus, acute care physical therapists can take a more active role in discharge planning to ensure older adults' ADL disability needs are met during the 30-day posthospitalization period to reduce risk of hospital readmission. Meeting these needs might include training family caregivers on giving appropriate assistance or working with discharge planners to ensure that caregivers can be arranged in a timely manner during the posthospitalization period—especially within the 48 hour window allowed between hospital discharge and initiation of home health care services.
Advance Care Planning
During an ITC, in-hospital advance care planning has been recommended to clarify treatment goals and facilitate referrals, if necessary, to hospice or palliative care services. This process has been shown to reduce avoidable hospital readmissions for symptoms that can be managed in the home or community setting.26 However, physical therapists are rarely involved in the advance care planning process for hospitalized older adults, despite the fact that upward of 50% of older adults utilizing palliative care services experience a fall related to impairments in physical functioning.52
If an older adult receives hospice or palliative care services, the role of the physical therapist in the ITC shifts from that of being a provider of restorative care to being a provider of maintenance services. Acute care physical therapists should recognize that a patient may require physical therapist services to prevent further decline in function or a fall leading to an avoidable hospital readmission. In addition, a physical therapist may explicitly advocate to the palliative care or hospice team for the patient to receive maintenance physical therapy. Many older adults benefit from physical therapist services during palliative care; these services may additionally help reduce avoidable readmissions during transitions from acute hospitalization.
Coordinating Care Among Team Members
A successful transition of care from hospital to home also includes strong coordination of care among all health care providers. Care coordination efforts during care transitions ensure that all home and community providers have access to pertinent information and are communicating cohesively about the continued treatment plan. Coordination during an ITC should involve as much continuity in care providers as possible. Maintaining continuity of physical therapy providers reduces hospitalization risk and improves functional outcomes for older adults receiving home health care.53 Additionally, when coordination is strong among physicians, nurses, and physical therapists during a care transition, older adults perceive their quality of care to be better and self-report less pain and better postoperative physical function.54
A 2008 American Physical Therapy Association position statement (HOD P06-08-16-16) encourages physical therapists to implement standardized handoff communications to ensure appropriate care coordination.55 Although this position statement emphasizes care handoffs between 2 therapists treating a common patient at the same facility, these communications may be even more critical to implement across care settings, especially when managing older adults during the period of high vulnerability after acute hospitalization. Medicare data suggest that 39% of older adults transfer between different care settings 2 or more times in the 30 days after hospital discharge.56
Physical therapists can contribute to improving continuity of care in 2 ways. First, physical therapists can adopt and utilize templates such as the Situation-Background-Assessment-Recommendation (SBAR) to streamline communications about and coordinating care for older adults with functional impairments with other physical therapists, care transition nurses, and community physicians.47 Development of a standardized template could reduce the communication breakdowns among rehabilitation providers that have been reported when older adults with mobility impairments transition to the home setting45,57 and subsequently may help reduce hospital readmissions. Second, physical therapists can develop standards for provider continuity during the 30-day transitional period after acute hospitalization, especially for those older adults at high risk for hospital readmission.
Monitoring and Managing Symptoms After Discharge
Monitoring and managing symptoms after discharge is a cardinal feature in most current care transitions models, especially for older adults with Medicare target conditions such as congestive heart failure.13 Noting the presence of any medical complications early during the care transition process is thought to be a key way to reduce avoidable hospital readmissions.9 However, neither physical therapy consultation nor postdischarge monitoring of the trajectory of physical function recovery is explicitly mentioned in the 3 major care transition models.14–16
Physical therapists can increase participation in the monitoring and management of physical function and related symptoms after hospital discharge in a variety of ways. First, physical therapists can establish use of common tools to assess function in older adults after hospital discharge and monitor for recovery commiserate with environmental needs (ie, adequate mobility to perform ADLs and instrumental activities of daily living [IADLs] needed for community independence). Second, physical therapists can educate community physicians and nursing staff on key self-reported functional deficits representing increased risk of hospitalization, such as patient reports of declining ADL ability21 or increasing lower extremity weakness.58 Additionally, physical therapists can assess and communicate a range of symptoms with medical etiology that may occur during and limit these tasks, such as dizziness, light-headedness, pain, fear, anxiety, or excessive fatigue.
Outpatient Follow-up
The final step in an ITC for an older adult is attendance at an outpatient follow-up visit with his or her primary care provider or other provider familiar with the patient. However, recommendations about the content of hospital follow-up visits do not routinely include any formal assessment of, or interventions for, impaired functional status.59 Older adults who report low physical activity levels during posthospitalization follow-up visits with physicians have a 64% increase in the odds of hospital readmission.60 Thus, the lack of a routine functional assessment during outpatient physician follow-ups is an especially concerning omission for those older adults who are discharged home without a referral for or access to physical therapist services (eg, those who are not homebound and thus do not qualify for Medicare home health services but are still functionally impaired and unable to access outpatient physical therapy).
Declining physical function can occur in isolation of increasing disease severity61 and thus should be monitored separately as an independent risk factor for hospital readmission by all members of the medical team. Physical therapists, therefore, have a tremendous opportunity to improve the final stages of a care transition by helping develop functional assessment batteries that can be carried out by community physicians or nurses as part of the posthospital follow-up visit for older adults. These assessments could use tools with established functional cutoffs for adverse outcomes related to hospitalization, such as gait speed (below 1.0 m/s17,62) or inability to rise from a chair without use of hands.63 A framework for this approach is provided by the Centers for Disease Control and Prevention's Stopping Elderly Accidents, Deaths, and Injuries (STEADI) fall-risk assessment tool.64 The STEADI tool is a standardized algorithm implemented by physicians during office visits that identifies older adults who are at risk for falls and offers suggested management strategies; physical therapists could contribute or lead development of a similar algorithm for assessment and management of functional decline after hospitalization in primary care settings. Optimal physical therapist treatment of older adults with functional decline after hospitalization has previously been described by Falvey et al.22
Integration of physical therapists into patient-centered medical home (PCMH) models of primary care may be another highly translatable implementation strategy for improving the quality of functional assessment during posthospitalization follow-up visits. The PCMH models utilize team-based health care delivery strategies to provide a comprehensive, patient-centered primary care service.65 The PCMH models that include physical therapist input have been shown to improve quality of life and reduce emergency department utilization in a population of vulnerable older adults.66,67 This finding suggests that inclusion of physical therapists in a PCMH model may have value in optimizing outcomes for older adults transitioning from hospital settings to the community. How physical therapists are best integrated into these models, however, has yet to be determined.
Future Directions
Care transitions are a major part of emerging care bundling efforts currently being tested by the Centers for Medicare & Medicaid Services (CMS),68 such as the community-based care transitions model and the care bundling initiatives for specific acute care diagnosis groups. A common quality of care indicator within these care bundling models is a reduction in avoidable hospital readmissions—a reduction that feasibly could be facilitated through improvements in posthospitalization management of physical function. Thus, there are 3 main future directions to further physical therapist involvement in care transitions: (1) develop standardized tools for communicating functional deficits to multiple disciplines across care settings, (2) develop research and quality improvement initiatives that test the impact of different models of physical therapist service delivery on hospital readmissions, and (3) expand interprofessional education to further expose physicians, pharmacists, and nurses to the role of physical therapists in the treatment of older adults after acute hospitalization. These initiatives will help physical therapists be more responsive to current goals surrounding communication and coordination of care during care transitions set forth by The Joint Commission, demonstrate how physical therapy affects patient outcomes after hospitalization, and improve recognition of how physical therapists can meaningfully improve outcomes for older adults emerging interdisciplinary models of care.
Conclusions
Considering the strong evidence that links functional abilities in the immediate posthospitalization period to readmission risk, physical therapists need to assume a stronger role in the treatment of older adults within care transition models. Physical therapists can contribute meaningfully to existing care transition models and work collaboratively with other health care disciplines in reducing avoidable hospital readmissions. They also are uniquely qualified to assess physical function, which represents a strong independent risk factor for hospital readmission. Yet, physical therapists have not routinely been included in care transition efforts beyond recommendations of discharge location—an important, but limited, utilization of our skills as health care professionals for older adults. This omission should start a conversation about how we shift the rehabilitation paradigm in acute care settings away from a distinct “silo” of care that ends when the patient leaves the hospital toward a model where acute care physical therapists extend their plan of care to include the 30-day transitional care period during which hospitals remain accountable for patient outcomes. Opportunities exist for physical therapists to increase their involvement in care transitions, especially when new Medicare penalties for excessive readmissions from other health care facilities (eg, inpatient rehabilitation) begin to be enforced.
For many older adults transitioning from the hospital to home settings, physical therapists are the right provider at the right time to assess and address posthospitalization physical and functional deficits. Developing tools and models of care that encompass this period not only shifts physical therapist practices to being more responsive to patient needs during care transitions but may improve functional outcomes for older adults after hospitalization. Such approaches may plausibly contribute to reducing hospital readmissions, improving overall medical outcomes, and subsequently decreasing health care costs—thereby objectively demonstrating the value of physical therapy in both this emerging care delivery model and future care bundling efforts for older adults.
Footnotes
Dr Falvey, Dr Burke, Dr Ridgeway, and Dr Stevens-Lapsley provided concept/idea/project design. Dr Falvey, Dr Burke, and Dr Ridgeway provided writing. Dr Falvey provided data analysis. Dr Stevens-Lapsley provided fund procurement and institutional liaisons. Dr Burke, Dr Malone, Dr Ridgeway, Dr McManus, and Dr Stevens-Lapsley provided consultation (including review of manuscript before submission).
Dr Falvey's work on the manuscript was supported, in part, by a Promotion of Doctoral Studies I Award from the Foundation for Physical Therapy and a research grant from the Health Policy and Administration Section of the American Physical Therapy Association. Dr McManus was supported, in part, by a Comprehensive Opportunities in Rehabilitation Research Training (CORRT) K12 award (K12 HD055931) through the National Institutes of Health. Dr Burke was supported, in part, by a Veterans Administration Health Services Research and Development Career Development Award.
The contents of this article do not necessarily represent the views of the US Department of Veterans Affairs or the US government.
References
- 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 2. Voss R, Gardner R, Baier R, et al. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171:1232–1237. [DOI] [PubMed] [Google Scholar]
- 3. Kortebein P, Bopp MM, Granger CV, Sullivan DH. Outcomes of inpatient rehabilitation for older adults with debility. Am J Phys Med Rehabil. 2008;87:118–125. [DOI] [PubMed] [Google Scholar]
- 4. Hoyer EH, Needham DM, Atanelov L, et al. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9:277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bohannon RW, Maljanian RD. Hospital readmissions of elderly patients hospitalized with pneumonia. Conn Med. 2002;67:599–603. [PubMed] [Google Scholar]
- 7. Bohannon RW, Lee N. Hospital readmissions and deaths during the first year after hospitalization for stroke. Conn Med. 2003;67:535–539. [PubMed] [Google Scholar]
- 8. Shih SL, Gerrard P, Goldstein R, et al. Functional status outperforms comorbidities in predicting acute care readmissions in medically complex patients. J Gen Intern Med. 2015;30:1688–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52:1817–1825. [DOI] [PubMed] [Google Scholar]
- 10. Naylor MD, Aiken LH, Kurtzman ET, et al. The importance of transitional care in achieving health reform. Health Aff (Millwood). 2011;30:746–754. [DOI] [PubMed] [Google Scholar]
- 11. Naylor MD. A decade of transitional care research with vulnerable elders. J Cardiovasc Nurs. 2000;14:1–14. [DOI] [PubMed] [Google Scholar]
- 12. Parry C, Coleman EA, Smith JD, et al. The care transitions intervention: a patient-centered approach to ensuring effective transfers between sites of geriatric care. Home Health Care Serv Q. 2003;22:1–17. [DOI] [PubMed] [Google Scholar]
- 13. Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–684. [DOI] [PubMed] [Google Scholar]
- 14. Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. [DOI] [PubMed] [Google Scholar]
- 15. Naylor M, Brooten D, Jones R, et al. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120:999–1006. [DOI] [PubMed] [Google Scholar]
- 16. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Odonkor CA, Schonberger RB, Dai F, et al. New utility for an old tool: can a simple gait speed test predict ambulatory surgical discharge outcomes? Am J Phys Med Rehabil. 2013;92:849–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Robinson TN, Wu DS, Sauaia A, et al. Slower walking speed forecasts increased postoperative morbidity and one-year mortality across surgical specialties. Ann Surg. 2013;258:582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vilaró J, Ramirez-Sarmiento A, Martínez-Llorens JM, et al. Global muscle dysfunction as a risk factor of readmission to hospital due to COPD exacerbations. Respir Med. 2010;104:1896–1902. [DOI] [PubMed] [Google Scholar]
- 20. Soley-Bori M, Soria-Saucedo R, Ryan CM, et al. Functional status and hospital readmissions using the Medical Expenditure Panel Survey. J Gen Intern Med. 2015;30:965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Greysen SR, Cenzer IS, Auerbach AD, Covinsky KE. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015;175:559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Falvey JR, Mangione KK, Stevens-Lapsley JE. Rethinking hospital-associated deconditioning: proposed paradigm shift. Phys Ther. 2015;95:1307–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim SJ, Lee JH, Han B, et al. Effects of Hospital-based physical therapy on hospital discharge outcomes among hospitalized older adults with community-acquired pneumonia and declining physical function. Aging Dis. 2015;6:174–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Green UR, Dearmon V, Taggart H. Improving transition of care for veterans after total joint replacement. Orthop Nurs. 2015;34:79–86. [DOI] [PubMed] [Google Scholar]
- 25. Madigan EA, Gordon N, Fortinsky RH, et al. Predictors of functional capacity changes in a US population of Medicare home health care (HHC) patients with heart failure (HF). Arch Gerontol Geriatr. 2012;54:e300–e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Burke RE, Kripalani S, Vasilevskis EE, Schnipper JL. Moving beyond readmission penalties: creating an ideal process to improve transitional care. J Hosp Med. 2013;8:102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Burke RE, Guo R, Prochazka AV, Misky GJ. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res. 2014;14:423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jette DU, Grover L, Keck CP. A qualitative study of clinical decision making in recommending discharge placement from the acute care setting. Phys Ther. 2003;83:224–236. [PubMed] [Google Scholar]
- 29. Smith BA, Fields CJ, Fernandez N. Physical therapists make accurate and appropriate discharge recommendations for patients who are acutely ill. Phys Ther. 2010;90:693–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care. JAMA. 2007;297:831–841. [DOI] [PubMed] [Google Scholar]
- 31. Cain CH, Neuwirth E, Bellows J, et al. Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;7:382–387. [DOI] [PubMed] [Google Scholar]
- 32. Boulding W, Glickman SW, Manary MP, et al. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17:41–48. [PubMed] [Google Scholar]
- 33. Burke RE, Jones J, Ho PM, Bekelman DB. Caregivers' perceived roles in caring for patients with heart failure: what do clinicians need to know? J Card Fail. 2014;20:731–738. [DOI] [PubMed] [Google Scholar]
- 34. Jones CD, Vu MB, O'Donnell CM, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Internl Med. 2015;30:417–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. [DOI] [PubMed] [Google Scholar]
- 36. Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8:436–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Polnaszek B, Mirr J, Roiland R, et al. Omission of physical therapy recommendations for high-risk patients transitioning from the hospital to sub-acute care facilities. Arch Phys Med Rehabil. 2015;96:1966–1972.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Silva AG, Queirós A, Sa-Couto P, Rocha NP. Self-reported disability: association with lower extremity performance and other determinates in older adults attending primary care. Phys Ther. 2015;95:1628–1637. [DOI] [PubMed] [Google Scholar]
- 39. Fisher SR, Kuo YF, Sharma G, et al. Mobility after hospital discharge as a marker for 30-day readmission. J Gerontol A Biol Sci Med Sci. 2013;68:805–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sleiman I, Rozzini R, Barbisoni P, et al. Functional trajectories during hospitalization: a prognostic sign for elderly patients. J Gerontol A Biol Sci Med Sci. 2009;64:659–663. [DOI] [PubMed] [Google Scholar]
- 41. Fortinsky RH, Covinsky KE, Palmer RM, Landefeld CS. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M521–M526. [DOI] [PubMed] [Google Scholar]
- 42. Ostir GV, Berges I, Kuo Y, et al. Assessing gait speed in acutely ill older patients admitted to an acute care for elders hospital unit. Arch Intern Med. 2012;172:353–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Volpato S, Cavalieri M, Sioulis F, et al. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66:89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Qian X, Russell LB, Valiyeva E, Miller JE. “Quicker and sicker” under Medicare's prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 2011;63:1–27. [DOI] [PubMed] [Google Scholar]
- 45. Dossa A, Bokhour B, Hoenig H. Care transitions from the hospital to home for patients with mobility impairments: patient and family caregiver experiences. Rehabil Nurs. 2012;37:277–285. [DOI] [PubMed] [Google Scholar]
- 46. van Walraven C, Duke SM, Weinberg AL, Wells PS. Standardized or narrative discharge summaries: Which do family physicians prefer? Can Fam Physician. 1998;44:62–69. [PMC free article] [PubMed] [Google Scholar]
- 47. Boaro N, Fancott C, Baker R, et al. Using SBAR to improve communication in interprofessional rehabilitation teams. J Interprof Care. 2010;24:111–114. [DOI] [PubMed] [Google Scholar]
- 48. Wolff JL, Meadow A, Weiss CO, et al. Medicare home health patients' transitions through acute and post-acute care settings. Med Care. 2008;46:1188–1193. [DOI] [PubMed] [Google Scholar]
- 49. Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. [DOI] [PubMed] [Google Scholar]
- 50. Portegijs E, Buurman BM, Essink-Bot ML, et al. Failure to regain function at 3 months after acute hospital admission predicts institutionalization within 12 months in older patients. J Am Med Dir Assoc. 2012;13:569.e1–7. [DOI] [PubMed] [Google Scholar]
- 51. DePalma G, Xu H, Covinsky KE, et al. Hospital readmission among older adults who return home with unmet need for ADL disability. Gerontologist. 2013;53:454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Stone CA, Lawlor PG, Savva GM, et al. Prospective study of falls and risk factors for falls in adults with advanced cancer. J Clin Oncol. 2012;30:2128–2133. [DOI] [PubMed] [Google Scholar]
- 53. Russell D, Rosati RJ, Andreopoulos E. Continuity in the provider of home-based physical therapy services and its implications for outcomes of patients. Phys Ther. 2012;92:227–235. [DOI] [PubMed] [Google Scholar]
- 54. Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care. 2000;38:807–819. [DOI] [PubMed] [Google Scholar]
- 55. American Physical Theraphy Association. Physical therapist of record and “hand off” communication (HOD P06–08-16-16). Available at: http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Practice/RecordHandOffCommunication.pdf Accessed September 15, 2015.
- 56. Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39:1449–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Greysen SR, Hoi-Cheung D, Garcia V, et al. “Missing pieces”—functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. J Am Geriatr Soc. 2014;62:1556–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women's Health Initiative Observational Study. J Am Geriatr Soc. 2005;53:1321–1330. [DOI] [PubMed] [Google Scholar]
- 59. Zuliani G, Soavi C, Maggio M, et al. Counteracting inflammation and insulin resistance with diet and exercise: a strategy for frailty prevention? Eur Geriatr Med. 2015;6:220–231. [Google Scholar]
- 60. Nguyen HQ, Chu L, Amy Liu IL, et al. Associations between physical activity and 30-day readmission risk in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11:695–705. [DOI] [PubMed] [Google Scholar]
- 61. Piepoli MF, Conraads V, Corrà U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13:347–357. [DOI] [PubMed] [Google Scholar]
- 62. Montero-Odasso M, Schapira M, Soriano ER, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60:1304–1309. [DOI] [PubMed] [Google Scholar]
- 63. Fisher SR, Ottenbacher KJ, Goodwin JS, Ostir GV. Chair rise ability and length of stay in hospitalized older adults. J Am Geriatr Soc. 2009;57:1938–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Centers for Disease Control and Prevention. STEADI–Older Adult Fall Prevention. Available at: http://www.cdc.gov/steadi Accessed December 18, 2015.
- 65. Agency for Healthcare Research and Quality, Patient Centered Medical Home Resource Center. Available at https://pcmh.ahrq.gov Accessed December 18, 2015.
- 66. Counsell SR, Callahan CM, Clark DO, et al. Geriatric care management for low-income seniors: a randomized controlled trial. JAMA. 2007;298:2623–2633. [DOI] [PubMed] [Google Scholar]
- 67. Counsell SR, Callahan CM, Buttar AB, et al. Geriatric Resources for Assessment and Care of Elders (GRACE): a new model of primary care for low-income seniors. J Am Geriatr Soc. 2006;54:1136–1141. [DOI] [PubMed] [Google Scholar]
- 68. Marengoni A, Von Strauss E, Rizzuto D, et al. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons: a community based, longitudinal study. J Intern Med. 2009;265:288–295. [DOI] [PubMed] [Google Scholar]