Abstract
Cognitive behavioral therapy (CBT) has a rich history of alleviating the suffering associated with mental disorders. Recently, there have been exciting new developments, including multi-component approaches, incorporated alternative therapies (e.g., meditation), targeted and cost-effective technologies, and integrated biological and behavioral frameworks. These field-wide changes have led some to emphasize the differences among variants of CBT. Here, we draw attention to commonalities across cognitive-behavioral therapies, including shared goals, change principles, and therapeutic processes. Specifically, we offer a framework for examining common CBT characteristics that emphasizes behavioral adaptation as a unifying goal and three core change principles, namely (1) context engagement to promote adaptive imagining and enacting of new experiences; (2) attention change to promote adaptive sustaining, shifting, and broadening of attention; and (3) cognitive change to promote adaptive perspective taking on events so as to alter verbal meanings. Further, we argue that specific intervention components including behavioral exposure/activation, attention training, acceptance/tolerance, decentering/defusion, and cognitive reframing may be emphasized to a greater or lesser degree by different treatment packages but are still fundamentally common therapeutic processes that are present across approaches and are best understood by their relationships to these core CBT change principles. We conclude by arguing for shared methodological and design frameworks for investigating unique and common characteristics to advance a unified and strong voice for CBT in a widening, increasingly multimodal and interdisciplinary, intervention science.
Keywords: Cognitive Behavioral Therapy, CBT, Common Principles, Intervention Science, Integration
Cognitive-behavioral therapies (CBTs) constitute a family of clinical interventions designed to produce behavior change. However, CBT approaches are themselves subject to growth and change. Moments of seemingly paradigmatic change within CBT reveal an age-old tension between conserving what is known to work well and pushing to expand the field beyond what is already known to be true. An early instance of this tension emerged during the “cognitive revolution” of the 1970s, during which period cognitive frameworks began to increase in popularity. Radical behavior therapists at the time rightfully criticized this movement for its lack of empirical base and tendency to “speak past the data” (Goldfried, 2010). However, the cognitive perspective eventually became central to the character of CBT, establishing an empirical base in terms of the role of cognitive factors such as attention, memory, and judgment in assessment and intervention (although the role of disputation as a necessary technique remains a point of debate; Jacobson, Martell, & Dimidjian, 2001).
Today we are once again faced with identity issues and challenges as to how best to grow, refine, and possibly redefine what it means to be a cognitive-behavioral theorist, researcher, and therapist. An important voice in the current expansion of CBTs comes from Acceptance and Commitment Therapy (ACT; S. Hayes, Strosahl, & Wilson, 1999; S. Hayes et al., this issue), Dialectical Behavior Therapy (DBT; Linehan, 1993), Mindfulness-Based Cognitive Therapy (MBCT; Segal, Williams, & Teasdale, 2002), Behavioral Activation (BA; Martell, Addis, & Jacobson, 2001), the Unified Protocol (UP; Barlow et al., 2011), Motivational Interviewing (MI; Miller & Rollnick, 1991), and Compassion-Focused Therapy (CFT; Gilbert, 2009), to name just a few of the many promising approaches that are stretching the boundaries of the CBT framework. Other approaches have combined traditional (“tCBTs”) and recent (“rCBTs”) approaches either in additive (Interpersonal Emotional Processing, Newman et al., 2011; MBCT; Segal et al., 2002) or integrative designs (STAIR-PE, Cloitre, Koenen, Cohen, & Han, 2002; Acceptance-Based Behavioral Therapy; ABBT; Roemer & Orsillo, 2009; Exposure-Based Cognitive Therapy; EBCT; A. Hayes et al., 2007; Emotion Regulation Therapy; ERT; Mennin & Fresco, 2009).
Spirited debates about the similarities and differences between tCBTs and rCBTs (Arch & Craske, 2008; Hofmann & Asmundson 2008; Herbert & Forman, this issue) – including the present issue of Behavior Therapy – have focused on whether newer approaches such as ACT have empirical support for their efficacy (“they don’t” vs. “they’re developing it”; Gaudiano, 2009; Öst, 2008); and whether it is novel (“they’re old hat” vs. “they’re something new”; Hofmann & Asmundson, 2008; S. Hayes et al., this issue). In regards to the first issue, as S. Hayes and colleagues (this issue) point out, tCBTs have been around longer and thus have achieved a significant empirical base (e.g., Butler, Chapman, Forman, & Beck, 2006; Tolin, 2010). Despite methodological weaknesses in some studies (Öst, 2008), initial evidence indicates that rCBTs are efficacious (S. Hayes et al., this issue). Given more rigorous investigations, time will likely establish a strong empirical base of efficacy for rCBTs including ACT. The latter issue, concerning whether this movement is novel, is one that concentrates the debate on what is different about these approaches. However, shining the light here may inordinately focus the discourse on the fringes, thereby picking apart smaller differences at the boundaries while ignoring the substantial overlap and synergy of these approaches.
Both S. Hayes and colleagues (this issue) and Hofmann and Asmundson (this issue) accentuate the distinctive philosophical and theoretical foundations of their approaches in their respective target articles. Correspondingly, numerous investigations have examined the comparative utility of rCBTs versus tCBTs. Trials testing these approaches typically involve comparison of the new approach with an established tCBT for that condition (e.g., substance dependence) or contextual problem (e.g., marital difficulties). This comparative efficacy RCT design is the gold standard for determining if a treatment comprised of new components is efficacious. The comparison and demonstrated equivalence or superiority to established treatments is considered a crucial step in determining the empirical basis of a treatment. Indeed, the major systems for determining efficacy of psychosocial interventions (e.g., APA/Division 12 Guidelines: http://www.div12.org/PsychologicalTreatments/index.html; NICE’s Guidelines; http://www.nice.org.uk) utilize this gold standard for determining if a new approach with discernable features can offer a distinctive approach via the ability to provide greater or more pervasive efficacy, encompassing refractory cases that have been difficult to treat with more established interventions.
Drawbacks to this “horse race” approach have been noted throughout numerous articles (Borkovec & Castonguay, 1998; Lohr, 2011). In particular, S. Hayes et al. (this issue) point out that this approach is quite slow. In addition, these studies may be unable to find distinctions that are anything greater than incremental given the inherent similarities in compared CBTs (as opposed to comparing CBT to another approach). Given this heterogeneity within the CBTs, a predominant focus on comparative efficacy may be ill advised given the likelihood of high overlap among these approaches and, hence, any direct comparison is likely to be costly, time consuming, and incremental in the information it provides about matching key components to ameliorating the suffering of the most refractory patients.
We agree that delineating and empirically evaluating core components of different approaches is vital. There clearly are “proprietary” intervention components inherent to each treatment package or approach. However, much of what the CBT models have declared as unique may actually reflect common intervention characteristics including shared goals, principles, and processes. Castonguay (2011) posits that these distinctions often reflect “faux-uniqueness” leading investigators to focus on small distinctions rather than large commonalities. In that spirit, we argue that there is a base of common characteristics that can harmonize tCBT and rCBT. By delineating these common characteristics, a collective language and investigative strategy can be generated that may help increase precision and efficiency in advancing our understanding and treatment of refractory psychopathologies.
Our goal is to emphasize the importance of CBT within a broader intervention science that is increasingly multimodal as well as interdisciplinary. Specifically, interventions have become progressively more heterogeneous as evidenced by a greater variety of multi-componential therapy packages, the integration of alternative therapies (e.g., meditation; Kabat-Zinn, 1994), and the development of targeted lab-based interventions (e.g., attention modification program; [AMP]; Amir, Beard, Burns, & Bomyea, 2009). In addition, psychosocial interventions are more commonly targeting the interplay of both behavioral and biological components (Zinbarg, Mashal, Black, & Flückiger, 2010). Given this wider investigative field, it is crucial that proponents of CBT clearly emphasize the value of their core offerings (i.e., the shared components of CBT) rather than engage in self-destructive internecine wrangling.
Echoing the calls of others (e.g., David & Montgomery 2011; Hofmann & Asmundson, this issue; Lohr, 2011) we recommend a move away from a stringent focus on comparative efficacy between similar approaches and, rather, emphasize the delineation of common characteristics of all CBTs (encompassing both tCBTs and rCBTs) including common goals, change principles, and therapeutic processes. However, a shift from predominantly a comparative efficacy focus to one that emphasizes characteristics of change means it will be important to clearly define what these characteristics are and how they relate to the current debate about similarities and differences between tCBTs and rCBTs such as ACT. In the remainder of the paper, we argue that CBTs share a common framework for intervention including a common goal of behavioral adaptation and corresponding change principles of context engagement, attention change, and cognitive change that promote this goal. Further, we argue that specific intervention components such as behavioral exposure, behavioral activation, attention training, acceptance/tolerance, decentering/defusion, and cognitive reframing may be emphasized to a greater or lesser degree by different treatment packages but they are still fundamentally common therapeutic processes that are present across approaches and are best understood by their relationships to these core CBT change principles.
A Model of Commonalities Across CBTs
Behavioral Adaptation As The Unifying Goal Of CBT
Reading the target articles of this series, one might think that different CBTs have different goals. For example, ACT emphasizes flexibility as the paramount objective in their hexaflex model of change (S. Hayes et al., this issue); tCBTs privilege the restoration of overall functioning (via symptom reduction). But, both flexibility and functionality reflect an overarching purpose to help individuals optimize their adaptation to circumstances that arise in their lives. By behavioral adaptation, we refer to the process by which organisms become better suited to prospering in their habitats (Dobzhansky, 1970). Humans have learned a variety of behaviors that have enabled us to populate large swathes of our planet, forage far and wide, and provide protection from environmental conditions while gaining advantages over other species that would otherwise compete for nourishment and possibly prey on us.
Making appropriate behavioral responses may be the difference between life and death and between love and loss. Examples of such opportunities for success are being maximally industrious for survival, successfully finding partners for co-habitation, and effectively communicating and building cooperation in group and culture systems (Keltner & Haidt, 1999). Individuals suffering from emotional disorders may demonstrate habitually inflexible and dysfunctional responses in these situations and, subsequently, a primary goal of CBTs is to direct interventions towards cultivating more behaviorally adaptive responses in order to survive and thrive in these important life domains. Whatever their differences, CBTs work to promote behavioral adaptation by assigning meaning to exteroceptive and interoceptive cues and encouraging the use of this information to take effective action.
CBT Principles And Processes That Promote Behavioral Adaptation
In addition to behavioral adaptation, CBTs share common change principles with respect to what needs to be changed for a given treatment goal to be realized (see Goldfried & Davila, 2005; Rosen & Davison, 2003). Specifically, these core change principles represent the roadmap for how to best promote behavioral adaptation. Although there are likely other principles within the family of CBTs, three core CBT principles are: (1) context engagement to promote adaptive imagining and enacting of new experiences to counteract old and well-worn patterns of maladaptive associations and reinforcement; (2) attention change to promote adaptive sustaining, shifting, and broadening of attention to changing contexts; and (3) cognitive change to promote adaptive perspective taking on an event so as to alter verbal meanings and their emotional significance. These change principles represented in a myriad of CBTs (as examples, see Cloitre et al., 2002; Craske & Barlow, 2008) also reflect the basic science of emotion regulation. Gross (2002) has demonstrated that emotional responding can be influenced along a temporal continuum. One can impact an emotional event via early selection or modification of a situation (the primary target of processes that promote context engagement), early stages of emotional processing (the primary target of processes that promote attention change), or at later stages of emotional processing (the primary target of processes that promote cognitive change).
It is important to note that emotional responding, according to Gross’s model, can also be influenced by attempting to impact the quality of a response (i.e., response modulation). Congruently, many tCBTs target a change in the quality of existing emotional responses to achieve symptom reduction and distress relief. For instance, progressive muscle relaxation has traditionally been used to reduce tension associated with apprehensive anxiety. Indeed, these approaches have established considerable efficacy (e.g., Borkovec, Newman, Pincus, & Lytle, 2002) and, for a number of populations such as children and cognitively challenged individuals, they may be a useful tool to help ameliorate suffering in individuals who lack the capacity to fully engage attention or cognitive change. However, approaches such as ACT have noted the difficulties associated with attempts to control a currently experienced emotion and have based a good deal of their approach on the notion that doing this is detrimental to change in the long run for the client (see Hayes et al., this issue). Thus, we have opted not to address response modulation as a change principle as it is not universally encouraged by all CBT approaches and thus, is not considered a common principle.
Numerous therapeutic processes common to the family of CBTs can be seen as differentially promoting these changes principles. Specifically, therapeutic processes of behavioral exposure (i.e., the encouraging of physical or imaginal movement towards threatening contexts) and behavioral activation (i.e., the encouraging of physical or imaginal movement towards rewarding contexts) can be seen as primarily reflecting the principle of context engagement. Further, attention training (i.e., encouraging the direct manipulation of attention in specific directions) and acceptance/tolerance (i.e., encouraging the allowance and unfolding of feeling states) can be seen as primarily reflecting the principle of attention change. Finally, cognitive change is a target of cognitive reframing interventions (i.e., encouraging the changing of one’s evaluation of an event to alter its emotional significance) but can also be seen as a principle that encompasses meta-cognitive distancing processes including decentering/defusion (i.e., encouraging identification, observation, and generation of psychological perspective from inner experiences), as well. Some treatments may be more likely to emphasize attention change principles (e.g., mindfulness-based treatments) and some might be more likely to emphasize cognitive change principles (e.g., cognitive therapy) but no existing approach can claim to focus fully on any one process or principle. More likely, current CBT approaches target multiple entry points in the emotional cascade and are thus likely reflect and align with each of these principles, albeit with varying degrees of engagement of different specific processes.
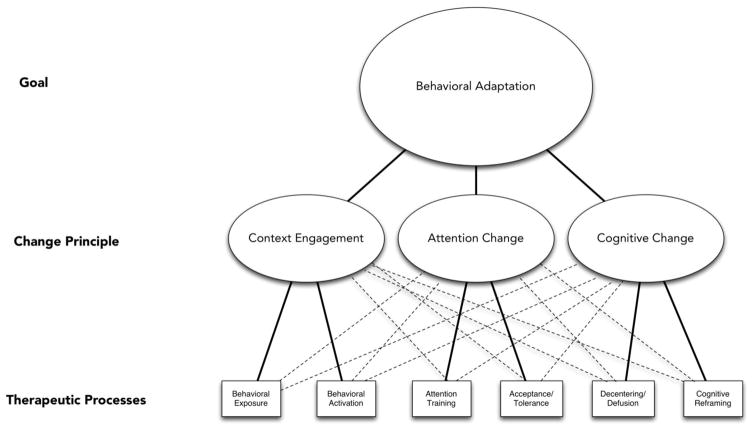
Figure 1 provides a conceptual model of behavioral adaptation reflected in common principles and corresponding therapeutic processes. This list of principles and processes is not exhaustive. Nonetheless, we argue that the therapeutic processes considered in this paper largely target the hypothesized change principles comprised in the broader family of CBTs. This relationship between therapeutic processes and targeted change principles is denoted in Figure 1 by solid lines. However, current therapeutic processes are blunt instruments that may also collaterally impact other principles (e.g., behavioral activation might increase attentional abilities in addition to promoting context engagement). It remains a challenge to the field to focalize interventions such that they are able to increasingly reflect precision in targeting specific change principles of interest. The ability to develop increasingly precise therapeutic processes reflective of clear change principles will be essential for the field to offer what are the key ingredients of CBTs that contribute best to efficacy and then to isolate these ingredients such that our treatments are most parsimonious (Cougle, 2012; see below) yet maximally effective. However, given the current state of heterogeneous relationships between current therapeutic processes and change principles, Figure 1 also displays dotted lines connecting therapeutic processes with non-targeted change principles in recognition that these processes may not solely create change via one corresponding principle. Nonetheless, we argue that each of these processes largely reflects its corresponding target change principle and will be discussed in the following sections, as such. How each change principle encourages the common goal of behavioral adaptation will also be noted. Specifically, in the following three sections, we propose a set of common change principles and corresponding therapeutic processes that may bind disparate CBT approaches together in their goal of behavioral adaptation and, more generally, offer a unified voice within an expanding intervention science.
Figure 1. Common Cognitive Behavioral Characteristics of Change (Goal, Change Principles, Therapeutic Processes).
Note: Solid lines reflect hypothesized relationships between a sample of therapeutic processes and targeted change principles. Dotted lines demonstrate that therapeutic processes may also impact behavioral adaptation via other change principles that are not primary targets.
Context Engagement
Context Engagement as a Change Principle
A hallmark change principle of CBTs is to assist clients in engaging new external and internal contexts to promote the imagining or enacting of novel responses that counteract old and well-worn patterns of maladaptive associations and reinforcement. Deficits in establishing adaptive and context appropriate contingencies, and the inability to learn new contingencies, represent key difficulties across emotional disorders. Indeed, individuals with psychopathology often exhibit rigid patterns of contextual engagement that reflect poor behavioral adaptation. For instance, individuals with anxiety disorders demonstrate impoverished and inflexible repertoires of behavior that typically function to promote escape, avoidance, or inactivity as a means of attempting to manage the arising of negative emotions (e.g., Lohr et al., 2007). Similarly, depressed individuals are less responsive to contexts for reward (e.g., Bogdan & Pizzagalli, 2006) and fail to distinguish between options yielding large versus small rewards (Forbes, Shaw, & Dahl, 2006). By contrast, bipolar spectrum disorders are characterized by hyperactive behavioral tendencies reflective of reward and goal systems without regard for contextual cues to threat and danger (Alloy et al., 2012). Finally, comorbid anxiety and depression may lead to difficulties resolving approach/avoidance valuation, which may result when an individual is unable to determine the relative value of simultaneous but ambiguous safety and reward contextual cues (Stein & Paulus, 2009).
Adaptive and flexible behavioral responses are dependent upon the ability to increase awareness of cues and contingencies in the environment and emit contextually appropriate responses that promote survival and success. Optimal reward learning requires us to assign value to possibly rewarding stimuli, make predictions about when and where we might encounter these stimuli, and take behavioral actions that are informed by these predictions (O’Doherty, 2004). Equally important is learning to accurately detect safety cues and differentiate these signals from threat cues so that we do not expend valuable resources (e.g., time & energy) in attempts to escape from ‘non-threats.’ Contemporary models of threat and safety learning are predicated on principles of classical conditioning (Bouton, Mineka, & Barlow 2001). One of the most basic directives of an adaptive organism is to bring balance with respect to engaging reward and minimizing loss while seeking safety and avoiding threat (Dollard & Miller, 1950). Normative functioning represents a constant state of engaging and resolving conflicts of reward and threat in service of taking effective behavioral action. CBT may help promote effective selection of appropriate and adaptive behavioral actions via the integration of stored representations, associations, and appraised meanings of the rewarding or aversive properties of a stimulus with contextual information from the internal and external environment. The salient outcomes of this adaptive responding are re-represented and reconsolidated memory stores that exert important influences on future response selection (Nader & Hardt, 2009).
Therapeutic Processes that Target Context Engagement
Behavioral Exposure
Exposure therapy is integral to CBTs for anxiety disorders (Craske et al., 2008). This approach derives from principles of classical conditioning, tracing back to the work of Wolpe (1958), and directly encourages the engagement of threat-perceived contexts. Relatively recent insights into the nature of fear extinction have elucidated the mechanisms underlying behavioral exposure (Craske et al., 2008). Fear extinction reflects the un-pairing of conditional stimulus (CS)-unconditional stimulus (US) associations but does not mean an elimination of the original CS-US association. Rather, the significant mechanism of action in exposure therapy may be inhibitory learning (i.e., CS-no US association), whereby new learning about the CS-US relationship develops that serves to inhibit the expression of previously conditioned responses (Bouton et al., 2001).
In the past 50+ years, exposure therapy has demonstrated considerable efficacy for patients suffering from anxiety disorders and findings continue to extend the acute and enduring treatment effects to a larger proportion of patients (Craske et al., 2008). In vivo exposures for conditions such as social phobia (Blanco et al., 2010), imaginal exposures for conditions such as posttraumatic stress disorder (Cloitre et al., 2002; Foa, 2011), and interoceptive exposures for conditions such as panic disorder (Craske & Barlow, 2008) have demonstrated extensive efficacy. In addition, rCBT approaches have built upon this foundation, and are showing promise in targeting contextual changes in response to perceived threats. For example, one important aspect of ACT is the delineation of values, which reflect construed desired life consequences, and in turn, help individuals clarify behavioral actions and promote motivation and endurance of instances such as facing one’s fears in a variety of contexts, which may be successful through the encouragement of superior inhibitory learning (S. Hayes et al., 1999; Wilson & Murrell, 2004). Similarly, many tCBT and rCBT approaches have been infused with mindfulness meditation practices. Treanor (2011) recently reviewed findings and proposed how mindfulness practices improve exposure therapy via enhanced attention capacity, better discrimination and recall of fear cues, and an increased tolerance to remain in contact with fearful stimuli.
Behavioral Activation
Like exposure therapy, treatment components commonly referred to as behavioral activation (BA) represented foundational behavioral efforts to treat conditions such as MDD that predate cognitive-oriented approaches (e.g., Beck, Rush, Shaw, & Emery, 1979). The BA conceptualization of depression views depressed individuals as no longer able to engage the behavioral repertoires capable of delivering positive reinforcement in their lives—thereby resulting in depression, withdrawal, and an ever-deepening vicious circle of deprivation from positive reinforcement (Lewinsohn, 1974). Ferster (1973) also posited that depression was largely a disorder of emotional withdrawal and that one of the ways that depressed individuals worsened their situation was by inordinately orienting their lives in service of escape and avoidance of aversive situations instead of pursuing opportunities for positive reinforcement. Thus, BA typically consisted of interventions including activity scheduling, contingency management, and skills training as ways of helping individuals gain awareness of the availability of positive reinforcement, emit behaviors capable of contingently obtaining positive reinforcement, and ideally, effecting change in one’s environment to sustain access to positive reinforcers remain available when certain behavioral responses are provided (Ferster, 1973; Kanter et al., 2010; Lewinsohn, 1974).
Encouraging engagement of reward contingencies is also part of tCBTs that emphasize cognitive elements such as the stressing of reward engagement in cognitive rehearsals (Beck et al., 1979) and the identification of triggers, responses, and alternative coping responses to promote engagement (e.g., Martell et al., 2001). Similarly, Kanter and colleagues (2010) note that adding values-based work (a central component of ACT; S. Hayes et al., 2011) can augment BA treatments, possibly by helping to motivate and sustain activation behaviors especially when the reinforcer for that action is not expected to occur immediately. Focusing on values may also provide a stronger compass for meaningful behavioral engagement beyond rewards that may be fleeting, not connected to personal meaning, or detrimental in the long term (e.g., unhealthy desserts, risky behaviors; S. Hayes et al., 2011). Recent findings from an open-label trial of BA highlight the role of reward engagement in the context of recovery from MDD (Dichter et al., 2009). Specifically, 12 MDD patients underwent fMRI assessment before and after treatment with BA. Findings revealed that 9 of 12 patients were classified as treatment responders and evidenced gains in self-report reward sensitivity and associated normalization of neural activity related to reward selection, reward anticipation, and reward feedback.
Attention Change
Attention Change as a Change Principle
Behavioral adaptation requires the ability to flexibly direct attention via constriction or expansion according to situational demands. A principle of attentional change can be seen as improving one’s ability to focus attention on a target stimulus, sustain attention on the chosen stimulus, or flexibly move attention to different stimuli. The ability to focus attention involves actively choosing the stimulus to which one will attend (Kabat-Zinn, 2005). The ability to sustain attention refers to maintaining this focus on the target stimuli (see Posner & Rothbart, 1992) as well as actively re-directing attention back to the target stimuli when attention has wandered (e.g., Smallwood & Schooler, 2006). The ability to flexibly move attention entails leading attention to various different aspects of an experience (Szymura, Smigasiewicz, & Corr, 2007).
Several converging lines of research suggest that reduced attentional flexibility and rigid attentional biases towards negative or threatening information, as well as difficulty disengaging from negative stimuli differentiate individuals with numerous psychopathologies from healthy controls and reflect key characteristics of emotional disorders (e.g., Joormann & Gotlib, 2007; Mathews & MacLeod, 2005). As such, numerous CBTs directly and indirectly target changes in attentional processing. Increasing attentional flexibility involves adapting attentional responding to varying contexts. Constricted, narrowly focused attention is adaptive during times of potential threat (i.e., concentrating resources on the threat and facilitating the selection and mobilization of appropriate responses; Friedman & Forster, 2010) but when no threat is present, broadened attention is more adaptive (facilitating exploratory behavior and allowing for the detection of new information and novel incentives; Friedman & Forster, 2010). Hyper-responsivity towards threatening information and attentional bias occur within milliseconds, and appear to influence further processing almost immediately (Mathews & MacLeod, 2005). As such, early processing biases towards threat are followed by reduced processing of threat or increased avoidant responding (see Hofmann, Ellard, & Siegle, 2011, for review). Disruptions in the earliest perceptual processing of stimuli set in motion regulatory control attempts and behavioral attempts to dampen responding (e.g., gaze aversion; Garner, Mogg, & Bradley, 2006).
Improving directed attention to external stimuli might aid in freeing an individual from passively attending (i.e., “mind wandering”; Smallwood & Schooler, 2006) to assumptions, predictions, evaluations, and other elaborative responding triggered by a given environmental context. Indeed, greater awareness of one’s environment may facilitate action that is more flexible and adaptive for the current situation. Targeting directed attention to internal, non-verbal stimuli might improve one’s awareness of personal experiences as they unfold. For instance, when attending to an emotion such as sadness, individuals can develop the capacity to attend to one’s body and notice the sensory qualities rather than cognitively appraising the emotion and engaging in rumination in response to the emotion (Farb et al., 2007).
Therapeutic Processes that Promote Attention Change
Attention Training
Although many tCBTs and rCBTs reduce attentional biases (Mathews & MacLeod, 2005), recent CBT interventions specifically work to increase attentional flexibility. Recent attentional bias modification (ABM) studies find an increased ability to improve directed attention away from a hypervigilant threat focus and subsequent improvement in symptoms and impairment, particularly for anxiety disorders (e.g., Amir et al., 2009; however, numerous meta-analyses have recently challenged whether this approach establishes durable efficacy; see Hallion & Ruscio, 2011, for one such meta-analytic example). In ABM, participants who were trained to attend away from threatening cues using a modified dot-probe paradigm showed an increased ability to disengage from threat-related cues, changes in attention bias, and a decrease in distress as indicated by self-report and interviewer measures.
Therapeutic processes that utilize mindfulness training also promote attentional flexibility. Mindful awareness training has been increasingly incorporated into psychological treatments as a method of promoting a level of open awareness that is intended to increase the objective, present-moment perception of internal and external cues (Baer, 2003). Exercises that target attention change include mindfulness of emotions, in which the client brings to mind an emotionally-provocative situation and observes, allows, and directs attention towards his or her internal, emotional experience (see Mennin & Fresco, 2009; Orsillo & Roemer, 2011; Segal et al., 2002) and mindfulness of senses and the body, which involve the client visualizing what the emotion would look like and feel like if it could be tangibly encountered through the senses; see S. Hayes et al., 1999; Segal et al., 2002). Engaging in formal mindfulness training reduces depressive symptoms and rumination while improving sustained attention (e.g., Chambers, Lo, & Allen, 2008) and perceptual sensitivity (e.g., MacLean et al., 2010).
Acceptance/Tolerance
In addition to processes that centrally train directed attention, interventions that promote emotional acceptance and tolerance primarily target attention change by encouraging sustained contact with feeling states without being dissuaded by elaborative thought processes that promote disengagement and avoidance (e.g., maintaining attendance to visceral aspects of emotions within the body without labeling or judging; see S. Hayes et al., 1999; Linehan, 1993; Segal et al., 2002). Although treatment research isolating emotional acceptance and tolerance processes is limited, increases in self-reported acceptance of difficult inner experiences (including emotional experiences) is associated with positive treatment outcomes (e.g., Forman, Herbert, Moitra, Yeomans, & Geller, 2007; McCracken, Vowles, & Eccleston, 2005). Similarly, lab based measures of distress tolerance predict early dropout in residential substance abuse treatment (Daughters, Lejuez, Bornovalova, Kahler, Strong, & Brown, 2005) whereas improvements in clinical outcome and distress tolerance occur when targeted by treatments designed to improve distress tolerance skills (Bornovalova, Gratz, Daughters, Hunta, & Lejuez, 2012).
Promoting acceptance and tolerance of emotions is a core component of rCBTs such as ACT and DBT. In ACT, clients are encouraged to notice the function of their thoughts and actions in terms of how they may promote distraction, attentional constriction, and overall “experiential avoidance” (see S. Hayes et al., 1999). ACT therapists then help clients work towards broadening their focus to allow all aspects of experience regardless of whether these feel difficult or aversive. Clients are encouraged to notice, describe, and maintain contact with an aversive internal experience (i.e., bodily sensation, feeling, thought, memory) as well as notice any efforts to constrict, disengage, or avoid these experiences. In DBT, distress tolerance skills promote an allowance of distressing emotions by encouraging a “wise mind” attendance of internal experience that is not wholly engaged and consumed (i.e., “emotional mind”) nor fully disengaged (i.e., “reasonable mind”) but rather is characterized by the simultaneous noticing of both urges to engage and disengage. Clients are then encouraged to utilize a series of tolerance skills to allow their difficult emotional experience while broadening attention to other aspects of their experience that are less negatively emotionally laden (see Linehan, 1993).
Cognitive Change
Cognitive Change as a Change Principle
Cognitive change refers to the ability to change one’s perspective on an event so as to alter verbal meanings and their emotional significance (Gross, 2002). Two types of cognitive processing are particularly important, namely cognitive distancing and cognitive reinterpretation. Cognitive distancing can be defined as a metacognitive ability to observe items that arise in the mind (e.g., thoughts, feelings, memories, etc.) with healthy psychological distance, greater self-awareness and perspective-taking, and the recognition that one’s thoughts, feelings, and urges are subjective, transient internal events rather than inherent, permanent aspects of the self or accurate representations of reality (Fresco, Moore et al., 2007; Fresco, Segal et al., 2007; Segal et al., 2002). Cognitive distancing helps individuals disengage from an intense emotion, its corresponding motivational impetus, and associated maladaptive self-referential processing in favor of a more experiential perspective with respect to personally relevant emotionally laden information (Farb et al., 2007).
Promoting distance from the self in time (e.g., viewing inner experiences as temporary; Watkins, Teasdale, & Williams, 2000), distance from the self in space (e.g., viewing inner experiences as physical objects that are separate from oneself; e.g., Kalisch et al., 2005), or distance from the self in personal perspective (e.g., viewing inner experiences as not inherent to one’s self-concept; Farb et al., 2007; Kross & Ayduk, 2009) is associated with psychological benefits. Further, a distanced perspective from aversive stimuli can decrease psychological distress (e.g., Davis, Gross, & Ochsner, 2011) and the believability of negative, self-relevant thoughts (Masuda et al., 2010). Fresco, Moore, and colleagues (2007) found cognitive distancing to be negatively related to self-report measures of depressive symptoms, anxiety symptoms, depressive rumination, experiential avoidance, and expressive suppression. Conversely, studies on individuals with psychopathology have found distress-reducing benefits from experimental techniques designed to promote an observational distance from the self (Farb et al., 2007; Kross & Ayduk, 2009). Further, distancing manipulations have also been shown to reduce depressotypic thought accessibility, diminished emotional recounting, and increase accuracy of reconstruals of past events in individuals who are depressed (Kross, Gard, Deldin, Clifton, & Ayduk, 2012).
Another form of cognitive change is cognitive reinterpretation of situations or circumstances in one’s life. Three common forms of cognitive reinterpretation include realistic reappraisal (e.g., re-evaluating an event in a more accurate, objective, factual manner while remaining sensitive to contextual factors; Ray, Wilhelm, & Gross, 2008), positive reappraisal (e.g., re-evaluating an event in a manner that orients towards possible desired, rewarding, or beneficial aspects of the event or consequences of the event that may have been overlooked in the original appraisal; Ray et al., 2008), and compassionate reappraisal (e.g., re-evaluating an event in a manner that appreciates that either oneself or another is in emotional pain, validates the pain, desires to alleviate the pain, and identifies the pain as a natural aspect of the human experience; Leary, Tate, Adams, Batts, & Hancock, 2007).
Laboratory based studies of cognitive change report psychological benefits from instructing participants to reappraise emotional stimuli or tasks in a manner designed to diminish personal identification and increase objectivity before the individuals encounter the stimuli or task (e.g., Gross, 2002; Hofmann et al., 2007). Studies have found distress-reducing benefits from inducing realistic/objective reappraisal (e.g., Ray et al., 2008), positive reappraisal (e.g., Ray et al., 2008), other-focused compassionate reappraisal (e.g., Witvliet, DeYoung, Hofelich, & DeYoung, 2011), and self-focused compassionate reappraisal (e.g., Leary et al., 2007) of personally emotionally provocative events. For instance, a substantial literature has shown that viewing a video of oneself is only useful in changing self-evaluation of performance and/or anxiety in those with social anxiety if one does so from the reappraising perspective of a third party (e.g., Rodebaugh, Heimberg, Schultz, & Blackmore, 2010). Difficulties implementing cognitive change appear to characterize various forms of psychopathology (Aldao, Nolen-Hoeksema, & Schweizer, 2011). A capacity to change cognitions and relinquish one’s original interpretation may undermine passive, repetitive elaborative processes central to transdiagnostic psychopathology (e.g., rumination; Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008) and promote flexibility that allows for more effective, rather than habitual, behavioral reactions. Indeed, reappraisal has been found to be positively associated with a number of indices of well being including effective interpersonal functioning (Gross & John, 2003).
Therapeutic Processes that Promote Cognitive Change
Decentering/Defusion
Many therapeutic processes of tCBTs and rCBTs (e.g., Beck, 1979; S. Hayes et al., 1999; Safran & Segal, 1990; Segal et al., 2002) promote cognitive distancing, albeit by different means. For example, the common CBT practice of instructing clients to self-monitor distressing thoughts and emotions and write down these experiences likely encourages observing, distancing, and labeling of emotional meanings. More directly, mindfulness and acceptance based perspectives (e.g., S. Hayes et al., 1999; Roemer & Orsillo, 2009; Segal et al., 2002) target cognitive distancing through various exercises such as mindfully noticing inner experiences or visualizing inner experiences as objects. Promoting temporal distance can be accomplished with “decentering” practices such as the mountain meditation (Kabat-Zinn, 1994), a mindfulness practice to help clients gain temporal perspective on a difficult emotional state by imagining themselves as a sturdy mountain that is continually awash in the effects of changing climates and seasons yet essentially still, consistent, and grounded. Thus, clients are able to decenter when they recognize that emotional storms, like real ones, are experiences rather than defining entities. Promoting a sense of spatial distance can be encouraged by practices such as the Observer exercise or “carrying your keys” in ACT (S. Hayes et al., 1999). In these practices, clients learn to notice internal emotional processes (i.e., emotional sensations, thoughts, memories) as a component or part of experience rather than defining characteristics.
Teasdale and colleagues (2002) found that MBCT resulted in larger increases in decentering as compared to treatment-as-usual. Further, self-reported decentering predicts acute treatment response in MDD following cognitive therapy but not medication (Fresco, Segal et al., 2007), durability of treatment gains (Fresco, Segal et al., 2007) and in the prevention of MDD relapse following MBCT (Bieling et al., 2012). Findings from an fMRI study on a subset of patients from the Bieling et al. trial revealed that hyperactivation of medial prefrontal regions implicated in self-referential processing predicted earlier relapse whereas increased activation in visual processing regions, interpreted as a capacity to observe emotionally evocative percepts, predicted treatment durability (Farb, Anderson, Bloch, & Segal, 2011).
As S. Hayes and colleagues (this issue) explain, clients can be encouraged to practice a similar form of cognitive distancing called defusion, which involves perspective taking on the impact of language-reinforcing associations. For example, clients might be encouraged to say “I am having anxiety right now” instead of “I am anxious”. Zettle, Rains, and Hayes (2011) compared group ACT versus group cognitive therapy in the treatment of MDD found that the differential impact of treatment condition on depressive symptoms at follow-up was mediated by self-reported decreases in the believability of depressogenic thoughts at post-treatment, which was used as an indication of increases in cognitive defusion. It is unclear, however, if cognitive distancing as opposed to reframing (see below) was the active process of change given the limits of self-report.
Cognitive Reframing
Reappraisal is a central focus of reframing interventions in tCBTs. One way that CBT therapists promote reframing is to encourage clients to monitor and interpret emotionally provocative events. When interpretations are found to be unrealistic or unhelpful, the therapist helps clients challenge the ascribed meaning through logical questioning, identification of cognitive “distortions” (i.e., interpretations that are not based on logic), and encourage clients to generate new possible meanings that are more rational and realistic (i.e., “restructuring”; e.g., Beck et al., 1979). Behavioral experiments can also elucidate how unhelpful or unrealistic meanings ascribed to events are not in line with what objectively occurs (e.g., Beck et al., 1979). Also, cognitive change is accomplished by providing psychoeducation to assist clients in identifying “thinking traps” in their appraisals, and generating alternative appraisals (e.g., Barlow et al., 2011). Although treatment research isolating reframing interventions is limited, Goldin et al. (2012) found that increases in cognitive reappraisal self-efficacy mediated CBT treatment efficacy. In a recent meta-analysis testing the role of threat reappraisal in symptom change from cognitive behavioral treatment of anxiety disorders, Smits and colleagues (2012) found that a small majority of these studies had established statistical mediation but only a few studies had established threat reappraisal preceded anxiety reduction and even fewer demonstrated specificity in this effect.
CBT therapists can also generate meaning change by helping clients to reframe via self-compassionate reappraisal. Techniques designed to enhance self-compassion include clients imagining telling a very caring, interested, compassionate individual about their difficult thoughts and feelings, clients asking themselves factual questions about the reality of their situation in a caring, nonjudgmental, and understanding manner, clients reminding themselves of their strengths and coping ability, clients empathically reflecting on the perspective of others involved in the situation, and clients offering soothing, helpful alternative thoughts while talking to themselves in the mirror (see Gilbert, 2009). CBT therapists have also incorporated loving-kindness meditation, in which clients imagine extending kindness to loved ones, to themselves, to neutral people or strangers, to individuals who have caused them harm, and to all living beings (e.g., Salzberg, 1995). Other exercises include the observation of self-critical thoughts and subsequent application of a statement of self-validation and self-compassion (see Mennin & Fresco, 2009, adapted from Segal et al., 2002).
Although ACT does not encourage challenging of thought content, it does emphasize the use of descriptive metaphors or analogies that encourage changing of perspectives on difficult emotional experiences from one of requiring avoidance and escape to one of viewing them as natural responses that are best allowed and not overly controlled (e.g., visualizing “dropping the rope” in a tug of war with an “anxiety monster”; “chess metaphor”; see S. Hayes et al., 1999). In other words, although ACT focuses on the concept of acceptance in their more metaphorically focused interventions, what might best account for change in these particular techniques is the implicit reframing of cognitions about the averseness of emotional experience and the need for it to be controlled. However, it is important to emphasize that cognitions are not reframed according to direct analysis but rather through an invitation to consider an alternative viewpoint about the struggle to reduce suffering.
The Broader Context
The past fifty years have seen considerable advances in the treatment of mental disorders. CBT has been particularly instrumental in developing treatments that alleviate the suffering associated with many of these conditions. Despite these advances, disorders characterized by high levels of comorbidity, unyielding course, and poor life satisfaction, remain refractory to existing treatments. To meet these challenges, we have witnessed exciting new developments in multi-componential behavioral approaches (e.g., ACT), alternative therapies (e.g., meditation), briefer, more targeted and cost-effective, technologies, and the integration of biological and behavioral frameworks of change. These changes reflect a widening, increasingly multi-disciplinary, intervention science. Although competition and disunity are natural responses to a diversifying field, a lack of cohesion limits opportunities for the CBT field to align in a shared vision and a common language to offer these CBTs to the larger community.
To promote this shared vision and common language, we have suggested that CBTs are characterized by (1) a common goal of behavioral adaptation; (2) common change principles of context engagement, attention change, and cognitive change to realize this behavioral adaptation goal; and (3) common therapeutic processes that can be seen as differentially reflecting each of these principles. Specifically, we have argued that to achieve a common goal of behavioral adaptation, CBTs share change principles that target responding at different points along an emotional trajectory (Gross, 2002), including context engagement which can be seen as encompassing therapeutic processes of behavioral exposure and behavioral activation; attention change, which can be seen as encompassing therapeutic processes of attention training and acceptance/tolerance; and cognitive change, which can be seeing as encompassing therapeutic processes of decentering/defusion and cognitive reframing.
Advancing core characteristics of CBT within an intervention science framework will require changes in research design and practice. One important change is in how we determine how our interventions produce change what is often termed mechanisms. Throughout the history of CBT, different approaches have focused on mechanisms defined by their intervention philosophy. However, we argue that efforts to demonstrate how a treatment produces clinical improvement should reflect common target mechanisms such as those that might underlie behavioral adaptation (e.g., inhibitory learning, Craske, 2008). Further, it will be important to examine target mechanisms with rich biobehavioral marker assessments (e.g., behavioral tasks, functional magnetic resonance imaging, psychophysiology) that have established reliability and validity in lab and analogue studies. This approach aligns CBT mechanism research with the growing multidisciplinary field of intervention science as well as with NIMH priorities such as the Research Domain Criteria initiative (i.e, “RDoC”; Sanislow et al., 2010) since it is agnostic to treatment theory and can help elucidate biobehavioral markers that are reliably dissociable in patient subgroups as compared to healthy controls. Also, assessing common target mechanisms in various approaches may help us better understand patient characteristics that predict treatment success and failure (e.g., treatment matching, treatment optimization/augmentation; NIMH Council’s treatment personalization initiative; Kraemer et al., 2002).
It will also be important to test the role of common change characteristics in differing intervention contexts. Traditional methods such as Rounsaville, Carroll, and Onken’s (2001) stage model provide established frameworks for determining how a treatment produces change and what are the most important core components. Typically, this involves successive tests of the efficacy of a treatment and later determination of core processes through dismantling designs. However, CBT also has a rich history of undertaking laboratory and analogue studies that inform treatment development. As S. Hayes and colleagues (this issue) have argued, laboratory studies can test whether a specific intervention process produces meaningful change in a given targeted mechanism via a more controlled environment. This approach is ultimately more cost effective than waiting to establish efficacy before testing how and why a treatment works. Laboratory paradigms that show promise in delineating common processes and mechanisms could be utilized within trial research to determine how these factors produce and mediate behavioral adaptation as a result of a given intervention.
One concern is that existing treatments are quite heterogeneous and, thus, it might be difficult to isolate the role of common characteristics. As Dobson (this issue) notes, CBT packages are technically eclectic (i.e., comprised of heterogeneous components) thereby complicating the identification of key principles and processes that lead to successful outcome, let alone differentiate how this is achieved in a given treatment versus another. In response to this issue, briefer, more homogeneous interventions have emerged (e.g., ABM; Amir et al., 2009). However, questions remain whether briefer means better in terms of improved efficacy or, more importantly, the ability to target the full spectrum of psychopathology in many conditions (e.g., see Hallion & Ruscio, 2011, for one meta-analytic example that calls into question the ability of ABM to provide durable efficacy for complex conditions). Indeed, conditions with dysfunction in multiple mechanisms may require longer, multi-process, approaches given greater complexity and refractory intervention response (e.g., anxious depression; Fava et al., 2008).
Thus, it will be important to have a shared language for assessing common principles and processes in approaches and modalities that differ in focus and scope. Adherence has typically reflected the measuring or coding of behaviors or actions on the part of the therapist related to the delivery of specific techniques in a treatment package. However, we may better serve the field by examining adherence and integrity at the level of common change principles and therapeutic processes (Rosen & Davison, 2003). This endeavor would involve developing a core battery of items related to principles and processes. For instance, adherence to context engagement could include items related to whether the intervention directly encouraged engagement of new behaviors and whether these were towards threatening or rewarding internal or external environments. However, given variability of treatments in their levels of heterogeneity, it will also be important to also index parsimony. Cougle (2012) has pointed out that more parsimonious treatments require less formal training in order to implement, lead to greater integrity and adherence, and are, thus, able to have superior outcomes. Ideally, therapies, according to Cougle, will be feasible for different settings, least aversive, as brief as possible, and cost effective. Thus, heterogeneous treatments may be necessary for some conditions but in addition to measuring how they reflect common characteristics, it will also be important to determine their parsimony, ease, and efficiency (Cougle, 2012).
The model of common change characteristics that we have provided is by no means exhaustive. Instead, it represents an initial attempt to provide scaffolding for seemingly diverse CBT approaches to find common ground in the purposes and targets of their interventions. Of course, philosophical differences underlying these therapeutic processes can be honored and modeled when examining common characteristics. For instance, the role of response modulation was not addressed given our view that it is not a common principle of change. However, given the efficacy o therapeutic process that target response modulation, especially in child and cognitively challenged populations where therapeutic processes reflective of other change principles (e.g., attention change, cognitive change) may be more difficult, it may be important to determine the role of response modulation-based change principles and whether these can be targeted from a common CBT perspective. Indeed, a recent extension of applied relaxation from an acceptance perspective supports this possibility (e.g., Hayes-Skelton, Usmani, Lee, Roemer, & Orsillo, 2012). Further, there are likely other common change principles and processes that CBT approaches encompass. Those offered in this article and other possible characteristics of change will be important to further examine both empirically and theoretically. As this special issue has demonstrated, there are exciting new developments in both tCBTs and rCBTs. We hope that by developing a common framework, we can honor these developments but also CBT as an integrated whole and step forward in a new age of intervention science with a strong and unified voice.
Highlights.
CBTs have a rich history of established efficacy for treating a myriad of pathological populations
New developments in the expanding field of intervention science suggest the importance of delineating core CBT components beyond establishing relative efficacy
Common characteristics of CBT may include a goal of behavioral adaptation and three associated core principles of context engagement, attention change, and cognitive change, which may help elucidate the core contributions of CBT research and treatments
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2009;118:28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arch JJ, Craske MG. Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology Science and Practice. 2008;15:263–279. doi: 10.1111/j.1468-2850.2008.00137.x. [DOI] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. doi: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J. The unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York, NY: Oxford University Press; 2011. [Google Scholar]
- Beck AT, Rush J, Shaw BF, Emery G. Cognitive therapy of depression. A treatment manual. New York, NY: Guilford Press; 1979. [Google Scholar]
- Bieling PJ, Hawley LL, Bloch RT, Corcoran KM, Levitan RD, Young LT, MacQueen GM, Segal ZV. Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse. Journal of Consulting and Clinical Psychology. 2012;80:365–372. doi: 10.1037/a0027483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Heimberg RG, Schneier FR, Fresco DM, Chen H, Turk CL, Vermes D, … Liebowitz MR. A placebo-controlled trial of phenelzine, cognitive behavioral group therapy, and their combination for social anxiety disorder. Archives of General Psychiatry. 2010;67:286–295. doi: 10.1001/archgenpsychiatry.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdan R, Pizzagalli DA. Acute stress reduces reward responsiveness: Implications for depression. Biological Psychiatry. 2006;60:1147–1154. doi: 10.1016/j.biopsych.2006.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, Castonguay LG. What is the scientific meaning of empirically supported therapy? Journal of Consulting and Clinical Psychology. 1998;66:136–142. doi: 10.1037//0022-006X.66.1.136. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70(2):288–298. doi: 10.1037//0022-006X.70.2.288. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug and Alcohol Dependence. 2012;122:70–76. doi: 10.1016/j.drugalcdep.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychological Review. 2001;108:4–32. doi: 10.1037/0033-295X.108.1.4. [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Castonguay LG. Psychotherapy, psychopathology, research and practice: Pathways of connections and integration. Psychotherapy Research. 2011;21:125–140. doi: 10.1080/10503307.2011.563250. [DOI] [PubMed] [Google Scholar]
- Chambers R, Lo BCY, Allen NB. The impact of intensive mindfulness training on attentional control, cognitive style, and affect. Cognitive Therapy and Research. 2008;32:303–322. doi: 10.1007/s10608-007-9119-0. [DOI] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology. 2002;70:1067–1074. doi: 10.1037//0022-006X.70.5.1067. [DOI] [PubMed] [Google Scholar]
- Cougle JR. What makes a quality therapy? A consideration of parsimony, ease, and efficiency. Behavior Therapy. 2012;43:468–481. doi: 10.1016/j.beth.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Craske MG, Barlow DH. Panic disorder and agoraphobia. In: Barlow DH, editor. Clinical handbook of psychological disorders. 4. New York, NY: Guilford Press; 2008. pp. 1–64. [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy. 2008;46:5–27. doi: 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, Kahler CW, Strong DR, Brown RA. Distress Tolerance as a Predictor of Early Treatment Dropout in a Residential Substance Abuse Treatment Facility. Journal of Abnormal Psychology. 2005;114:729–734. doi: 10.1037/0021-843X.114.4.729. [DOI] [PubMed] [Google Scholar]
- David D, Montgomery GH. The scientific status of psychotherapies: A new evaluative framework for evidence-based psychosocial interventions. Clinical Psychology Science and Practice. 2011;18:89–99. doi: 10.1111/j.1468-2850.2011.01239.x. [DOI] [Google Scholar]
- Davis JI, Gross JJ, Ochsner KN. Psychological distance and emotional experience: What you see is what you get. Emotion. 2011;11:438–444. doi: 10.1037/a0021783. [DOI] [PubMed] [Google Scholar]
- Dichter GS, Felder JN, Petty C, Bizzell J, Ernst M, Smoski MJ. The effects of psychotherapy on neural responses to rewards in major depression. Biological Psychiatry. 2009;66:886–897. doi: 10.1016/j.biopsych.2009.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobzhansky T. Genetics of the evolutionary process. New York, NY: Columbia University Press; 1970. [Google Scholar]
- Farb NAS, Anderson AK, Bloch RT, Segal ZV. Mood-linked responses in medial prefrontal cortex predict relapse in patients with recurrent unipolar depression. Biological Psychiatry. 2011;70:366–372. doi: 10.1016/j.biopsych.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, Anderson AK. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Social Cognitive and Affective Neuroscience. 2007;2:313–322. doi: 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Alpert JE, Balasubramani GK, Carmin CN, Biggs MM, Zisook S, Leuchter A, Howland R, Warden D, Trivedi M. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: A STAR*D report. American Journal of Psychiatry. 2008;165:342–351. doi: 10.1176/appi.ajp.2007.06111868. [DOI] [PubMed] [Google Scholar]
- Ferster CB. A functional analysis of depression. American Psychologist. 1973;28:857–870. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- Foa EB. Prolonged exposure therapy: past, present, and future. Depression and Anxiety. 2011;28:1043–1047. doi: 10.1002/da.20907. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Shaw DS, Dahl RE. Alterations in reward-related decisions in boys with depressive and anxiety disorders. Biological Psychiatry. 2006;59:126S–126S. doi: 10.1016/j.biopsych.2006.05.026. [DOI] [PubMed] [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31:772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Moore M, van Dulmen M, Segal Z, Ma S, Teasdale J, Williams J. Initial psychometric properties of the Experiences Questionnaire: Validation of a self-report measure of decentering. Behavior Therapy. 2007;38:234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology. 2007;75:447–455. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Friedman RS, Forster J. Implicit affective cues and attentional tuning: An integrative review. Psychological Bulletin. 2010;136:875–893. doi: 10.1037/a0020495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner M, Mogg K, Bradley BP. Orienting and maintenance of gaze to facial expressions in social anxiety. Journal of Abnormal Psychology. 2006;115:760–770. doi: 10.1037/0021-843X.115.4.760. [DOI] [PubMed] [Google Scholar]
- Gaudiano BA. Öst’s (2008) methodological comparison of clinical trials of acceptance and commitment therapy versus cognitive behavior therapy: Matching apples with oranges? Behaviour Research and Therapy. 2009;47:1066–1070. doi: 10.1016/j.brat.2009.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P. The compassionate mind: A new approach to life’s challenges. Oakland, CA: New Harbinger; 2009. [Google Scholar]
- Goldfried MR. Mindfulness and acceptance in cognitive behavior therapy: What’s new? In: Herbert JD, Forman EM, editors. Acceptance and mindfulness in cognitive behavior therapy: Understanding and applying the new therapies. Hoboken, NJ: John Wiley & Sons, Inc; 2010. pp. 317–336. [Google Scholar]
- Goldfried MR, Davila J. The role of relationship and technique in therapeutic change. Psychotherapy. 2005;42:421–430. doi: 10.1037/0033-3204.42.4.421. [DOI] [Google Scholar]
- Goldin PR, Ziv M, Jazaieri H, Werner K, Kraemer H, Heimberg RG, Gross JJ. Cognitive reappraisal self-efficacy mediates the effects of individual cognitive-behavioral therapy for social anxiety disorder. Journal of Consulting and Clinical Psychology. 2012;80:1034–1040. doi: 10.1037/a0028555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology. 2002;39:281–291. doi: 10.1017/s0048577201393198. doi:10.1017.S0048577201393198. [DOI] [PubMed] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychological Bulletin. 2011;137:940–958. doi: 10.1037/a0024355. [DOI] [PubMed] [Google Scholar]
- Hayes AM, Feldman GC, Beevers CG, Laurenceau JP, Cardaciotto L, Lewis-Smith J. Discontinuities and cognitive changes in an exposure-based cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 2007;75:409–421. doi: 10.1037/0022-006X.75.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Hayes-Skelton SA, Usmani A, Lee JK, Roemer L, Orsillo SM. A fresh look at potential mechanisms of change in applied relaxation for generalized anxiety disorder: A case series. Cognitive and Behavioral Practice. doi: 10.1016/j.cbpra.2011.12.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Asmundson GJG. Acceptance and mindfulness-based therapy: New wave or old hat? Clinical Psychology Review. 2008;28:1–16. doi: 10.1016/j.cpr.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Ellard KK, Siegle GJ. Neurobiological correlates of cognitions in fear and anxiety: A cognitive- neurobiological information processing model. Cognition & Emotion. 2011;26:282–299. doi: 10.1080/02699931.2011.579414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Meuret AE, Rosenfield D, Suvak MK, Barlow DH, Gorman J, Woods SW. Preliminary evidence for cognitive mediation during cognitive behavioral therapy for panic disorder. Journal of Consulting and Clinical Psychology. 2007;75:374–379. doi: 10.1037/0022-006X.75.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology Science and Practice. 2001;8:255–270. doi: 10.1093/clipsy.8.3.255. [DOI] [Google Scholar]
- Joormann J, Gotlib IH. Selective attention to emotional faces following recovery from depression. Journal of Abnormal Psychology. 2007;116:80–85. doi: 10.1037/0021-843X.116.1.80. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are. New York, NY: Hyperion Press; 1994. [Google Scholar]
- Kabat-Zinn J. Coming to our senses: Healing ourselves and the world through mindfulness. New York, NY: Hyperion Press; 2005. [Google Scholar]
- Kalisch R, Wiech K, Critchley HD, Seymour B, O’Doherty JP, Oakley DA, … Dolan RJ. Anxiety reduction through detachment: Subjective, physiological, and neural effects. Journal of Cognitive Neuroscience. 2005;17:874–883. doi: 10.1162/0898929054021184. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC. What is behavioral activation? A review of the empirical literature. Clinical Psychology Review. 2010;30:608–620. doi: 10.1016/j.cpr.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Keltner D, Haidt J. Social function of emotions at four levels of analysis. Cognition and Emotion. 1998;13:505–521. [Google Scholar]
- Kraemer H, Wilson G, Fairburn C, Agras W. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Kross E, Ayduk Z. Boundary conditions and buffering effects: Does depressive symptomology moderate the effectiveness of self–distancing for facilitating adaptive emotional analysis? Journal of Research in Personality. 2009;43:923–927. doi: 10.1016/j.jrp.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kross E, Gard D, Deldin P, Clifton J, Ayduk Ö. “Asking why” from a distance: Its cognitive and emotional consequences for people with major depressive disorder. Journal of Abnormal Psychology. 2012;121:559–563. doi: 10.1037/a0028808. [DOI] [PubMed] [Google Scholar]
- Leary MR, Tate EB, Adams CE, Batts Allen A, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. Journal of Personality and Social Psychology. 2007;92:887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM. A behavioral approach to depression. In: Friedman RM, Katz MM, editors. The psychology of depression: Contemporary theory and research. Washington, DC: Winston-Wiley; 1974. pp. 157–185. [Google Scholar]
- Linehan M. Skills training manual for treating borderline personality disorder. New York, NY: The Guilford Press; 1993. [Google Scholar]
- Lohr JM. What is (and what is not) the meaning of evidence-based psychosocial intervention? Clinical Psychology: Science and Practice. 2011;18:100–104. doi: 10.1111/j.1468-2850.2011.01240.x. [DOI] [Google Scholar]
- Lohr JM, Olatunji B, Sawchuk C. A functional analysis of danger and safety signals in anxiety disorders. Clinical Psychology Review. 2007;27:114–126. doi: 10.1016/j.cpr.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Martell CR, Addis ME, Jacobson NS. Depression in context: Strategies for guided action. New York, NY: Norton; 2001. [Google Scholar]
- Masuda A, Twohig MP, Stormo AR, Feinstein AB, Chou YY, Wendell JW. The effects of cognitive defusion and thought distraction on emotional discomfort and believability of negative self-referential thoughts. Journal of Behavior Therapy and Experimental Psychiatry. 2010;41:11–17. doi: 10.1016/j.jbtep.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annual Review of Clinical Psychology. 2005;1:167–195. doi: 10.1146/annurev.clinpsy.1.102803.143916. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long standing chronic pain: A preliminary analysis of treatment outcome in comparison to a waiting phase. Behaviour Research and Therapy. 2005;43:1335–1346. doi: 10.1016/j.brat.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM. Emotion regulation as an integrative framework for understanding and treating psychopathology. In: Kring AM, Sloan DM, editors. Emotion regulation in psychopathology: A transdiagnostic approach to etiology and treatment. New York: Guilford; 2009. pp. 356–379. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press; 1991. [DOI] [Google Scholar]
- Mineka S, Öhman A. Born to fear: non-associative vs associative factors in the etiology of phobias. Behaviour Research and Therapy. 2002;40:173–184. doi: 10.1016/S0005-7967(01)00050-X. [DOI] [PubMed] [Google Scholar]
- Nader K, Hardt O. A single standard for memory: the case for reconsolidation. Nature Reviews Neuroscience. 2009;10:224–234. doi: 10.1038/nrn2590. [DOI] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell JF, Szkodny LE, Nordberg SS. A randomized controlled trial of cognitive-behavioral therapy for generalized anxiety disorder with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology. 2011;79:171–181. doi: 10.1037/a0022489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- O’Doherty JP. Reward representations and reward-related learning in the human brain: insights from neuroimaging. Current Opinion in Neurobiology. 2004;14:769–776. doi: 10.1016/j.conb.2004.10.016. [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Roemer L. The mindful way through anxiety: Break free from chronic worry and reclaim your life. New York, NY: Guilford Press; 2011. [Google Scholar]
- Öst LG. Efficacy of the third wave of behavioral therapies: A systematic review and meta-analysis. Behaviour Research and Therapy. 2008;46:296–321. doi: 10.1016/j.brat.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Posner MI, Rothbart MK. Attentional regulation - from mechanism to culture. International Journal of Psychology. 1992;27:41–57. [Google Scholar]
- Ray RD, Wilhelm FH, Gross JJ. All in the mind’s eye? Anger rumination and reappraisal. Journal of Personality and Social Psychology. 2008;94:133–145. doi: 10.1037/0022-3514.94.1.133. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Heimberg RG, Schultz LT, Blackmore M. The Moderated Effects of Video Feedback for Social Anxiety Disorder. Journal of Anxiety Disorders. 2010;24:663–671. doi: 10.1016/j.janxdis.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM. Mindfulness- and acceptance-based behavioral therapies in practice. New York, NY: Guilford Press; 2009. [Google Scholar]
- Rosen G, Davison G. Psychology should list empirically supported principles of change (ESPs) and not credential trademarked therapies or other treatment packages. Behavior Modification. 2003;27:1–13. doi: 10.1177/0145445503253829. [DOI] [PubMed] [Google Scholar]
- Rounsaville B, Carroll K, Onken L. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology Science and Practice. 2001;8:133–142. doi: 10.1093/clipsy.8.2.133. [DOI] [Google Scholar]
- Safran JD, Segal ZV. Interpersonal process in cognitive therapy. New York, NY: Basic Books; 1990. [Google Scholar]
- Salzberg S. Loving-kindness: The revolutionary art of happiness. Boston: Shambhala; 1995. [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, … Cuthbert BN. Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: Guilford; 2002. [Google Scholar]
- Smits JAJ, Julian K, Rosenfield D, Powers MB. Threat reappraisal as a mediator of symptom change in cognitive-behavioral treatment of anxiety disorders: A systematic review. Journal of Consulting and Clinical Psychology. 2012;80:624–635. doi: 10.1037/a0028957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straube T, Glauer M, Dilger S, Mentzel HJ, Miltner WHR. Effects of cognitive-behavioral therapy on brain activation in specific phobia. Neuroimage. 2006;29:125–135. doi: 10.1016/j.neuroimage.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Szymura B, Smigasiewicz K, Corr P. Psychoticism and attentional flexibility. Personality and Individual Differences. 2007;43:2033–2046. doi: 10.1016/j.paid.2007.06.023. [DOI] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006X.70.2.275. [DOI] [PubMed] [Google Scholar]
- Tolin DF. Is cognitive–behavioral therapy more effective than other therapies? Clinical Psychology Review. 2010;30:710–720. doi: 10.1016/j.cpr.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Treanor M. The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clinical Psychology Review. 2011;31:617–625. doi: 10.1016/j.cpr.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Watkins E, Teasdale JD, Williams RM. Decentering and distraction reduce overgeneral autobiographical memory in depression. Psychological Medicine. 2000;30:911–920. doi: 10.1017/S0033291799002263. [DOI] [PubMed] [Google Scholar]
- Wilson KG, Murrell AR. Values work in acceptance and commitment therapy. In: Hayes SC, Follette VM, Linehan M, editors. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York, NY: Guilford Press; 2004. [Google Scholar]
- Witvliet CVO, DeYoung NJ, Hofelich AJ, DeYoung PA. Compassionate reappraisal and emotion suppression as alternatives to offense-focused rumination: Implications for forgiveness and psychophysiological well-being. The Journal of Positive Psychology. 2011;6:286–299. doi: 10.1080/17439760.2011.577091. [DOI] [Google Scholar]
- Wolpe J. Psychotherapy by reciprocal inhibition. Stanford, CA: Stanford University Press; 1958. [Google Scholar]
- Zettle RD, Rains JC, Hayes SSC. Processes of change in acceptance and commitment therapy and cognitive therapy for depression: A mediation reanalysis of Zettle and Rains. Behavior Modification. 2011;35:265–283. doi: 10.1177/0145445511398344. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Mashal NM, Black DA, Flückiger C. The future and promise of cognitive behavioral therapy: a commentary. Psychiatric Clinics of North America. 2010;33:711–727. doi: 10.1016/j.psc.2010.04.003. [DOI] [PubMed] [Google Scholar]