Abstract
Importance
Although bariatric surgery is the most cost-effective treatment for severe obesity, less than 1% of severely obese patients undergo it. Reasons for low utilization are unclear.
Objectives
To identify patient and referring provider characteristics associated with the likelihood of undergoing bariatric surgery.
Evidence Review
PubMed, PsycINFO, CINAHL, and the Cochrane databases were searched for reports published between January 1, 1998, and December 31, 2014. Reports were eligible if they presented descriptive data regarding facilitators or barriers to bariatric surgery or if they reported statistical associations between patient or provider characteristics and referral to or receipt of bariatric surgery. Frequency effect sizes were calculated as the proportion of studies reporting a finding.
Findings
Of the 7,212 reports identified in the initial search, 53 were included in full-text review. Nine reports met our inclusion criteria and were included in analyses. Of those, four included descriptive findings, six reported statistical associations, and one included both. One report included providers as study participants, whereas eight included patients. Four of nine studies identified an association between female gender and a greater willingness to undergo bariatric surgery. Lack of knowledge about bariatric surgery was a barrier in two studies. Five of nine cited patient concerns about the outcomes and safety of bariatric surgery as a barrier to undergoing it. Patients were more likely to pursue bariatric surgery when it was recommended by referring providers. Providers who believed that obesity treatment should be covered by insurance were more likely to recommend bariatric surgery.
Conclusions and Relevance
Limited patient and referring provider knowledge about the safety and effectiveness of bariatric surgery are important barriers to bariatric surgery utilization. Future efforts focused on improving knowledge and identification of the critical determinants of obesity treatment decision making from both the provider and patient perspectives would have an important public heath impact.
Introduction
Bariatric surgery outcomes have been the focus of more than 30 randomized controlled trials and nearly 150 observational studies over the past decade.1 Compared to medical treatment, bariatric surgery has achieved superior weight loss and comorbidity resolution and significantly improves quality of life.2-9 Most studies suggest that bariatric surgery is a cost-effective intervention.10 Although one concluded that bariatric surgery was not cost-saving after three years in a cohort of mostly male Veterans,11 three others in non-Veterans have found that bariatric surgery may be cost-saving within a decade.12-14 A lead author of one of these economic analyses noted that, “the expectation for any surgical intervention to show a return on investment is unusual, and few effective interventions reach this threshold. Laparoscopic Roux-en-Y gastric bypass, however, may be one of them.”15
Given the strong evidence supporting bariatric surgery, one might expect that a significant percentage of severely obese patients (patients with a body mass index [BMI] ≥ 40 kg/m2 or 35 – 40 kg/m2 in addition to an obesity-related comorbidity) would choose to pursue it. However, of the estimated 18 million severely obese adults in the United States,16 only 125,000 (< 1%) undergo bariatric surgery annually.17,18
Reasons for the low utilization of bariatric surgery are unclear. Lack of access to bariatric surgery due to socioeconomic factors and low education levels have been cited as possible barriers.19 Lack of insurance coverage has been also been reported as a barrier, although utilization rates are even lower in some settings where it is broadly covered (i.e., Veterans Affairs population).20 A comprehensive understanding of facilitators and barriers among patients and referring providers is needed to promote appropriate referrals and provision of bariatric surgery. We performed a systematic review of literature published from 1998 through 2014. Our goal was to identify patient and referring provider characteristics related to demographics, knowledge, and attitudes toward bariatric surgery that are associated with either referral for or receipt of bariatric surgery.
Methods
Search Strategy
We searched Medline, PsycINFO, CINAHL, and the Cochrane Registry for Controlled Trials. Each database was searched from January 1, 1998 through December 1, 2014. 1998 was chosen as the starting point because it represents the beginning of the modern era of bariatric surgery, which incorporates laparoscopy.17 Search terms were used that identified bariatric surgery, including gastric bypass, sleeve gastrectomy, or adjustable gastric band. The complete search-string used for our PubMed search is in the Appendix. Inclusion criteria were 1) observational or interventional study design; 2) descriptive or inferential findings; 3) patient or provider participants, 4) adult human subjects; and 5) English language. Case reports and series, studies examining clinical outcomes, editorials, guidelines, trials comparing surgical or medical therapies, and literature reviews were ineligible. Reports were excluded if they focused on medical or psychiatric comorbidities as predictors of undergoing bariatric surgery because they are part of the clinical decision-making process regarding eligibility. For example, one study included in our initial search found that approximately one in five surgical candidates did not pass initial psychiatric screening.21 Others focused binge eating among bariatric surgery candidates.22,23 We considered these as issues that factored into the bariatric team's decision-making process rather than a patient-level barrier to bariatric surgery.
Study Selection
Results of the searches were imported into EndNoteX7, and duplicates were eliminated. Two surgeon members of the study team (Funk, Fischer) manually reviewed record titles and abstracts and excluded reports based on the aforementioned criteria. Reports were subjected to full-text review by two surgeon reviewers (Funk, Fisher) if at least one reviewer marked it for inclusion. If consensus was not reached by both reviewers, a third reviewer (Voils) was included. All three reviewers discussed their reasons for initial inclusion or exclusion. Consensus was reached when all three reviewers subsequently agreed to include or exclude the report.
Data extraction and analysis
Study characteristics were extracted from each report and included dates of data collection, study population (patients or providers), research setting (outpatient, inpatient, ambulatory surgery, integrated health care system, and academic medical center), gender and race/ethnicity of study participants, study design and methodology, and data type (descriptive or inferential).
Relevant findings were extracted by two surgeon members of the research team (Funk, Jolles) and verified by the senior author (Voils). Descriptive and inferential findings were included in this synthesis because they addressed the same research question and were in a format that permits meta-synthesis.24,25 Descriptive findings were included if they were mentioned in a report, regardless of the number of participants mentioning them.26 Descriptive findings were obtained both from qualitative data collection techniques (e.g. interviews, focus groups) and quantitative surveys in which authors reported the percentage of participants endorsing a barrier or facilitator of surgery. Statistical associations between patient or provider characteristics and referral to or receipt of bariatric surgery were included in analyses if p ≤ .05. Following previous research published by the senior author, if only bivariate analyses were reported, then bivariate results were used.24 If results from a multivariable regression analysis were available, then we used those findings rather than the bivariate results because the estimate is likely more accurate after adjusting for confounders. If results from several regression models were presented, results from the model with the largest number of predictors were included. The statistical associations and descriptive findings were grouped by topical similarity, and concise summaries of each finding were created.
For each abstracted finding, a frequency effect size was calculated as the number of reports containing a finding divided by the total number of included reports. Frequency effect sizes reflect the extent to which a particular theme has been studied either because researchers thought the constructs were important to study (in the case of quantitatively-oriented studies in which investigators determine a priori what to measure) or because participants thought the issues were important enough to raise in the context of a discussion (in the case of qualitative data generated by focus groups, interviews, or open-ended survey questions). This strategy follows a data extraction technique that we have described previously for qualitative meta-summaries combining quantitative and qualitative findings.24
Results
Study Selection and Characteristics
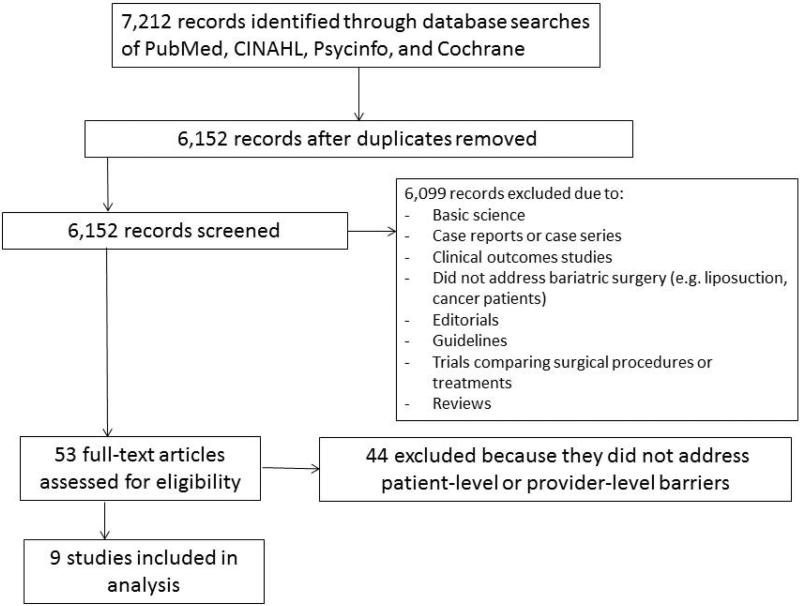
Our literature search identified 7,212 unique records. After removing 1,060 duplicates, 6,152 articles were reviewed at the title and abstract level. Of these, 53 reports were chosen for full-text review. Nine reports representing unique studies were selected for inclusion in the systematic review. The study selection process, as per Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines,27 is shown in the Figure.
Figure.
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Flowchart Detailing the Selection of Studies for Systematic Review Diagram
All included studies were published from 2007 through 2014. Eight studies included patients as study participants, while one focused on providers. In eight of the nine studies, most participants were female (Table 1). The percentage of non-white participants in the seven reports that included ethnicity/race ranged from 41% to 100%. All study designs were observational and cross-sectional. Study methodologies included surveys or questionnaires (n=7), retrospective chart review (n=1), and focus groups (n=1). Four of the nine studies provided descriptive data. Six reports included inferential statistics, of which four included multivariable analyses.28-31 Three reports focused on receipt of bariatric surgery.30,32,33 The other six targeted referral for bariatric surgery.
Table 1.
Study Characteristics
| Study author (year) | Data collection dates | Design | Data type | Setting | Population | Female (%) | Non-white (%) |
|---|---|---|---|---|---|---|---|
| Afonso35 (2010) | Feb 2007-April 2008 | Observational, cross-sectional | Descriptive and inferential | Outpatient and inpatient | Patients: 77 severely obese patients seen by internal medicine residents as inpatients or outpatients at the Cleveland Clinic Florida for medical problems not related to bariatric surgery | 53 | 51 |
| Arterburn28 (2013) | Not reported | Observational, cross-sectional | Inferential | Integrated health care System | Patients: 295 severely obese participants who were members of Group Health (Washington) who met NIH criteria for bariatric surgery but had not been referred to the Bariatric Surgery Program at Group Health | 68 | 22 |
| Ferrante29 (2009) | March-May 2008 | Observational, cross-sectional | Inferential | Outpatient | Providers: 255 family physicians in New Jersey (members of the NJ Family Medicine Research network and randomly selected family physicians from a Blue Cross Blue Shield provider directory | 41 | 20 |
| Khawali31 (2014) | Jan 2006-Feb 2007 | Observational, cross-sectional | Inferential | Outpatient | Patients: 65 Patients with a BMI >=40 who were registered on the waiting list for bariatric surgery at the Obesity and Bariatric Surgery Outpatient Clinic of the Federal University of Sao Paulo (Brazil) | 62 | Not reported |
| Lynch36 (2007) | Not reported | Observational focus groups | Descriptive | Community | Patients: 41 African-American females with a BMI >30 living in the greater Pittsburgh area; recruited in collaboration with the Black Women and Health Outreach for Longer Life and Empowerment group | 100 | 100 |
| Pitzul32 (2014) | Aug 2009-Feb 2011 | Observational, cross-sectional | Descriptive | Outpatient | Patients: 1,237 patients referred to the Toronto Western Hospital Bariatric Program | 71 | Not reported |
| Sarwer34 (2013) | Not reported | Observational, cross-sectional | Inferential | Integrated health care system | Patients: 130 patients with type 2 diabetes and a BMI of 30-40, ages 18-65, identified from the Pennsylvania Integrated Clinical and Administrative Research Database | 53 | 54 |
| Sivagnanam33 (2008) | Mar 2006-Nov 2007 | Observational, cross-sectional | Descriptive | Outpatient | Patients: 55 patients referred to the Norfolk and Norwich University Hospital (UK) for bariatric surgery | 76 | Not Reported |
| Wee30 (2014) | Not reported | Observational, cross-sectional | Inferential | Two academic medical centers | Patients: 337 patients, ages 18-65, with a BMI>35 who were seen at one of four primary care practices in Greater-Boston | 69 | 65 |
Patient characteristics associated with the likelihood of discussing or considering bariatric surgery referral (Table 2)
Table 2.
Patient characteristics associated with the likelihood of discussing or considering bariatric surgery referral
| Favoring discussion or consideration of bariatric surgery referral | Effect Size | NOT favoring discussion or consideration of bariatric surgery referral | Effect Size |
|---|---|---|---|
| Patient Demographics | |||
| Female gender (Arterburn, Sarwer) | 2/9 | Older age (Afonso) | 1/9 |
| Higher body mass index (Arterburn, Khawali) | 2/9 | White ethnicity (Afonso) | 1/9 |
| Higher socioeconomic status (Khawali) | 1/9 | Employed in a professional occupation (Afonso) | 1/9 |
| Higher number of comorbidities (Arterburn) | 1/9 | ||
| Obstructive sleep apnea as a comorbidity (Khawali) | 1/9 | ||
| Patient level of knowledge | |||
| Not aware of being a candidate for bariatric surgery (Afonso) | 1/9 | ||
| Not aware of bariatric surgery as a treatment option (Afonso) | 1/9 | ||
| Patient attitudes and behavior | |||
| Feeling that other obesity treatment options have been exhausted (Lynch) | 1/9 | Concerns about surgical complications or death (Afonso, Lynch, Sarwer) | 3/9 |
| Higher role-emotional score on SF-36 (Khawali) | 1/9 | Concern about the financial burden of bariatric surgery (Afonso) | 1/9 |
| Concerns about having no control over the amount of weight lost (Lynch) | 1/9 | ||
| Not receiving a recommendation from primary care physician to consider undergoing bariatric surgery (Alfonso) | 1/9 | ||
| Physical and lifestyle restrictions after bariatric surgery (Lynch) | 1/9 | ||
| Concerns about weight regain following surgery (Lynch) | 1/9 | ||
| Perception that bariatric surgery is an option of last resort (Lynch) | 1/9 | ||
| Not interested in surgery as a strategy to treat morbid obesity (Afonso) | 1/9 | ||
| Insurance Coverage | |||
| Having insurance coverage for bariatric surgery (favored discussion with PCP but barrier to considering it) (Arterburn) | 1/9 | Not having insurance coverage for bariatric surgery (Afonso) | 1/9 |
ES=effect size
Patient demographics
Two studies found that females were more likely to consider referral for bariatric surgery,20,34 while two also found that higher BMI was associated with a higher likelihood of considering referral.20,31 The presence of a higher number of obesity-related comorbidities28 - specifically obstructive sleep apnea31 - was associated with a higher likelihood of bariatric surgery consideration while older age was associated with a lower likelihood of considering bariatric surgery.35 White ethnicity was associated with a lower likelihood of considering bariatric surgery referral in one report,35 while another found that patients who were in higher socioeconomic status groups were more likely to consider bariatric surgery.31
Patient level of knowledge
Afonso and colleagues assessed the association between patient knowledge and the likelihood of considering bariatric surgery.35 Lack of knowledge regarding bariatric surgery as a treatment option for severe obesity was associated with a lower likelihood that a severely obese patient would consider bariatric surgery. 13% of patients were not aware that they qualified as a candidate for bariatric surgery, and 8% had never heard of bariatric surgery.
Patient attitudes and behavior
Patient concerns about surgical complications or death were associated with a lower likelihood of considering bariatric surgery referral in three studies.34-36 Concerns regarding the financial burden of bariatric surgery were reported in one.35 In their focus group study of obese African-American women, Lynch and colleagues reported that patients were concerned about the loss of control over the amount of weight loss, lifestyle restrictions, and possible weight re-gain after bariatric surgery.36 Patients who felt their other treatment options had been exhausted were more likely to consider bariatric surgery.
Insurance coverage
Arterburn and colleagues concluded that having insurance coverage for bariatric surgery was associated with a higher likelihood that patients had discussed bariatric surgery with a primary care provider (PCP) but a lower likelihood that they would consider pursuing it.28 In the aforementioned Afonso study, not having insurance coverage for bariatric surgery was associated with a lower likelihood that the patient would consider it.35
Patient characteristics associated with the likelihood of receiving of bariatric surgery (Table 3)
Table 3.
Patient characteristics associated with the likelihood of receiving of bariatric surgery
| Favoring receipt of bariatric surgery | Effect Size | NOT favoring receipt of bariatric surgery | Effect Size |
|---|---|---|---|
| Patient Demographics | |||
| Female gender (Pitzul, Wee) | 2/9 | Older age (Wee) | 1/9 |
| Higher body mass index (Sivagnanam) | 1/9 | ||
| African Americans and Hispanics were more likely than Whites to consider bariatric surgery if their doctor advised it (Wee) | 1/9 | ||
| Having some college education (Wee) | 1/9 | ||
| Hypertension as a comorbidity (Wee) | 1/9 | ||
| Patient attitudes and behavior | |||
| Having a lower ideal body weight (Wee) | 1/9 | Concerns about surgical complications or death (Sivagnanam, Wee) | 2/9 |
| Receiving a recommendation from primary care physician to consider undergoing bariatric surgery (Wee) | 1/9 | Concern about the financial burden of bariatric surgery (Pitzul, Sivagnanam) | 2/9 |
| Higher obesity-specific quality of life (Wee) | 1/9 | ||
| Physically incapable of commuting (Sivagnanam) | 1/9 | ||
| Unable to arrange childcare for clinic appointments (Sivagnanam) | 1/9 | ||
| Concern about financial burden associated with commuting to clinic appointments (Sivagnanam) | 1/9 | ||
| Lack of choice regarding surgeon, type of operation and/or hospital (Sivagnanam) | 1/9 | ||
| Prefer to lose weight on their own (Pitzul) | 1/9 | ||
| Unable to complete participation in bariatric surgery preoperative program indicated by multiple missing appointments or dropping out of the program (Pitzul) | 1/9 | ||
| Unable to complete participation in bariatric surgery preoperative program due to inability to stop smoking cigarettes or marijuana, both preoperative requirements (Pitzul) | 1/9 | ||
| Prefer to lose weight on their own (Pitzul) | 1/9 | ||
ES=effect size
Patient demographics
Two reports found that female gender was associated with a higher likelihood of considering receipt of bariatric surgery.30,32 In a telephone survey of 325 severely obese patients seen at four primary care practices in the Boston area, Wee and colleagues found that African American and Hispanic ethnicities were more likely to consider undergoing bariatric surgery if they received a physician recommendation for surgery but were less likely to consider it if they were older.37
Patient attitudes and behavior
In multivariable analyses, Wee reported that patients who received a recommendation from a PCP to consider bariatric surgery were five times more likely to consider it. Physician recommendation was a stronger predictor than patient race, gender, age, BMI, or comorbidities.30 In their chart review and subsequent telephone follow-up with 55 patients who were referred but did not undergo bariatric surgery in the U.K., Sivagnanam and colleagues reported that patients were concerned about bariatric surgery complications, its financial burden, and logistical challenges related to attending clinic visits, such as arranging for childcare.33 Difficulty with participation in the bariatric surgery preoperative program was cited by Pitzul as a reason that patients did not undergo bariatric surgery despite referral.32
Provider characteristics associated with the likelihood of referring a patient for bariatric surgery (Table 4)
Table 4.
Provider characteristics associated with the likelihood of recommending bariatric surgery
| Favoring recommendation of bariatric surgery | Effect Size | Not favoring recommendation of bariatric surgery | Effect Size |
|---|---|---|---|
| Provider level of knowledge | |||
| Greater knowledge about bariatric surgery (Ferrante) | 1/9 | ||
| Provider attitudes and behavior | |||
| N/A | |||
| Type of practice | |||
| Higher percentage of severely obese patients in a primary care physician's practice (Ferrante) | 1/9 | ||
One study investigated the association between provider characteristics bariatric surgery referral.29 Family physicians with a self-reported greater knowledge about bariatric surgery were more likely to recommend bariatric surgery in bivariate analysis. Having higher self-reported knowledge regarding the care of extremely obese patients was associated with a more positive attitude toward bariatric surgery in bivariate analyses. The relationship between physician attitude and actual discussion or referral for bariatric surgery was not assessed. In multivariable analyses, PCPs with a higher percentage of severely obese patients in their practice (>7%) were more likely to refer severely obese patients for bariatric surgery.
Discussion
Our findings suggest that patient concerns regarding complications or death following bariatric surgery are a notable barrier to pursuing bariatric surgery. Only two studies in our literature review examined the association between patient or referring provider knowledge of bariatric surgery and the likelihood of patients undergoing or being referred for bariatric surgery. Primary care physicians who were more knowledgeable about bariatric surgery were more likely to refer patients for bariatric surgery. This is a critical observation because a recommendation from a PCP increases the likelihood that a patient will consider bariatric surgery more than any other patient characteristic that has been studied, including patient race, gender, socioeconomic status, weight, or comorbidity status.
Despite the concerns about complications or death that patients reported in several studies included in this review, the published literature suggests that bariatric surgery is very safe.38,39 In 2008, national registry data from the U.S. indicated that the 30-day mortality rate was 0.16% for bariatric surgery.38 Subsequent analysis of over 400,000 bariatric operations from 2007 to 2012 found that 30-day mortality had declined to 0.1%.39 By comparison, data from the National Surgical Quality Improvement Program (NSQIP) indicate that the 30-day mortality rate following cholecystectomy is 0.27%.40 For laparoscopic anti-reflux surgery, typically considered an advanced laparoscopic procedure, NSQIP data indicated that the 30-day mortality rate was 0.19%.41 Yet, in contrast to bariatric surgery, patient and provider concerns about the risk of death following cholecystectomy or laparoscopic anti-reflux surgery are not described in the literature as a barrier to undergoing surgery.
Reasons for the discordance between the actual and perceived risks of bariatric surgery are unknown. This is especially confusing when one considers that severely obese patients in one study were willing to accept a 13% mortality rate – a more than a 10-fold increase in the actual risk – to achieve their desired health state.42 One possible explanation is that, as with other health risks, patients may rely on vivid examples, such as experiences of friends or cases in the lay press, rather than actual risks to guide their impressions.43 Ongoing education is needed to assure that patients have an accurate understanding of the expected, often very favorable, outcomes following bariatric surgery.
Both studies in our review that investigated the relationship between knowledge and referral or receipt of bariatric surgery found that lower knowledge was associated with lower referral and receipt rates. Poor knowledge regarding the effectiveness of bariatric surgery has been reported by other investigators. Sikorski and colleagues found that the general public felt that dietary changes and psychological changes were both more effective treatments than bariatric surgery.44 While these are important components of any multi-disciplinary weight management program, there is no evidence that lifestyle change is more effective than bariatric surgery. Further, fewer than half of general practitioners consider themselves capable of managing obesity effectively.45 This lack of confidence is a significant concern.
The impact of insurance coverage on bariatric surgery utilization remains unclear. In the hypothetical scenario posed by Arterburn and colleagues,28 having bariatric surgery coverage was associated with an increase in the likelihood of having a discussion with the primary care physician, but a decrease in the likelihood of considering it. The authors stated that this finding was likely the result of unmeasured confounding. Yet, in an environment where less than one in three patients had coverage for bariatric surgery – a rate common for commercial insurers in the U.S. – they urged more research in this area. Other investigators have found that among patients referred for bariatric surgery, lack of insurance coverage was the most common reason that patients were rejected from participation in a bariatric surgery program.46
Our findings point to an excellent opportunity for ongoing research and quality improvement efforts to have a major public health impact. More qualitative studies examining perspectives and attitudes toward obesity care and bariatric surgery would help us understand why 99% of patients do not pursue the most effective treatment.5,6,8 Studies addressing why females are much more likely to undergo bariatric surgery are also needed as it seems likely that males are being undertreated. A better understanding of referring provider practices is also needed given that referral is the first step in the path to bariatric surgery. In one study, nearly 90% of PCPs indicated that an educational program would increase the likelihood that appropriate patients would be referred for bariatric surgery; more than 80% wanted handouts to give to patients regarding obesity treatment options.47
This study has several limitations. We did not assess the extent to which reports included data on methodological rigor, as is commonly done in systematic reviews. Our stance is that all data can inform the evidence base and that sensitivity analyses can be performed based on quality of reporting. Our small sample size precluded meaningful analyses by quality of reporting. Second, although our search strategy was comprehensive and generated more than 7,000 records to review, we may have missed relevant studies. We were not able to perform a meta-analysis to assess the effect size associated with predictors of bariatric surgery referral and uptake. We would have needed a larger, more homogeneous sample of studies that included a single outcome and inferential statistics. Our mixed synthesis approach, which included descriptive and inferential findings and allowed for a larger range of outcomes by patients and providers, meets the imperative of using more available types of data in meta-syntheses.
In summary, limited patient and provider knowledge about the safety and effectiveness of bariatric surgery are barriers to bariatric surgery utilization. Advances are needed in this field, including improved design and availability of qualitative studies and rigorous investigation of the factors that impact decision-making for referring providers. An increase in the appropriate utilization of bariatric surgery may result from these efforts which would be welcomed given that few of the nearly 20 million severely obese patients in the U.S. are pursuing the most effective treatment.
Acknowledgement
The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. This award provided assistance with interpretation of the data as well as preparation and review of the manuscript. The design and conduct of the study, data collection, management, analysis, approval of the manuscript and decision to submit were made solely by the research team.
Appendix
Search strategy
PubMed
Search (“Bariatric Surgery”[Mesh] OR (bariatric AND (care OR surgery)) OR “weight loss surgery” OR “gastric bypass” OR “sleeve gastrectomy” OR laparoscopic adjustable gastric banding) AND (Clinical Trial OR Comparative Study OR Controlled Clinical Trial OR Evaluation Studies OR Meta-Analysis OR Multicenter Study OR Observational Study OR Randomized Controlled Trial OR systematic[sb] OR Validation Studies OR prospective OR retrospective OR epidemiologic OR cohort OR case-control OR longitudinal OR cross-sectional) Filters: Publication date from 1998/01/01 to 2014/12/31; Humans; English; Adult: 19+ years
Footnotes
Conflicts of interest: Drs. Funk, Fischer, and Voils declare no conflicts of interest. Ms. Jolles declares no conflicts of interest.
References
- 1.Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The Effectiveness and Risks of Bariatric Surgery: An Updated Systematic Review and Meta-analysis, 2003-2012. JAMA surgery. 2013 doi: 10.1001/jamasurg.2013.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. The New England journal of medicine. 2004;351:2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 3.Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. The New England journal of medicine. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 4.Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Annals of surgery. 2004;240:416–23. doi: 10.1097/01.sla.0000137343.63376.19. discussion 23-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA : the journal of the American Medical Association. 2013;309:2240–9. doi: 10.1001/jama.2013.5835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. The New England journal of medicine. 2012;366:1577–85. doi: 10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- 7.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. The New England journal of medicine. 2012;366:1567–76. doi: 10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 3-Year Outcomes. The New England journal of medicine. 2014 doi: 10.1056/NEJMoa1401329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA : the journal of the American Medical Association. 2003;289:1792–8. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 10.Wang BC, Furnback W. Modelling the long-term outcomes of bariatric surgery: A review of cost-effectiveness studies. Best practice & research Clinical gastroenterology. 2013;27:987–95. doi: 10.1016/j.bpg.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Maciejewski ML, Livingston EH, Smith VA, Kahwati LC, Henderson WG, Arterburn DE. Health expenditures among high-risk patients after gastric bypass and matched controls. Archives of surgery. 2012;147:633–40. doi: 10.1001/archsurg.2012.818. [DOI] [PubMed] [Google Scholar]
- 12.Cremieux PY, Ledoux S, Clerici C, Cremieux F, Buessing M. The impact of bariatric surgery on comorbidities and medication use among obese patients. Obesity surgery. 2010;20:861–70. doi: 10.1007/s11695-010-0163-6. [DOI] [PubMed] [Google Scholar]
- 13.Finkelstein EA, Allaire BT, Globe D, Dixon JB. The business case for bariatric surgery revisited: a non-randomized case-control study. PloS one. 2013;8:e75498. doi: 10.1371/journal.pone.0075498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myers VH, McVay MA, Adams CE, et al. Actual medical and pharmacy costs for bariatric surgery: 6-year follow-up. Southern medical journal. 2012;105:530–7. doi: 10.1097/SMJ.0b013e318268c76d. [DOI] [PubMed] [Google Scholar]
- 15.Finkelstein EA, DiBonaventura M, Burgess SM, Hale BC. The costs of obesity in the workplace. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2010;52:971–6. doi: 10.1097/JOM.0b013e3181f274d2. [DOI] [PubMed] [Google Scholar]
- 16.Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. International journal of obesity. 2013;37:889–91. doi: 10.1038/ijo.2012.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003-2008. Journal of the American College of Surgeons. 2011;213:261–6. doi: 10.1016/j.jamcollsurg.2011.04.030. [DOI] [PubMed] [Google Scholar]
- 18.MBSAQIP Semiannual Report. American College of Surgeons, American Society for Metabolic and Bariatric Surgery; Jun, 2014. [Google Scholar]
- 19.Jackson TD, Zhang R, Glockler D, et al. Health inequity in access to bariatric surgery: a protocol for a systematic review. Systematic reviews. 2014;3:15. doi: 10.1186/2046-4053-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arterburn DE, Olsen MK, Smith VA, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313:62–70. doi: 10.1001/jama.2014.16968. [DOI] [PubMed] [Google Scholar]
- 21.Zimmerman M, Francione-Witt C, Chelminski I, et al. Presurgical psychiatric evaluations of candidates for bariatric surgery, part 1: Reliability and reasons for and frequency of exclusion. J Clin Psychiatry. 2007;68:1557–62. doi: 10.4088/jcp.v68n1014. [DOI] [PubMed] [Google Scholar]
- 22.Mazzeo SE, Saunders R, Mitchell KS. Binge eating among African American and Caucasian bariatric surgery candidates. Eating Behaviors. 2005;6:189–96. doi: 10.1016/j.eatbeh.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Mazzeo SE, Saunders R, Mitchell KS. Gender and binge eating among bariatric surgery candidates. Eating Behaviors. 2006;7:47–52. doi: 10.1016/j.eatbeh.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Sandelowski M, Barroso J, Voils C. Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Res Nurs Health. 2007;39:99–111. doi: 10.1002/nur.20176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sandelowski M, Voils C, Barroso J. Comparability work and the management of difference in research synthesis studies. Social Science & Medicine. 2007;64:236–47. doi: 10.1016/j.socscimed.2006.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Voils CI, Sandelowski M, Barroso J, Hasselblad V. Making Sense of Qualitative and Quantitative Findings in Mixed Research Synthesis Studies. Field methods. 2008;20:3–25. doi: 10.1177/1525822X07307463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arterburn D, Westbrook EO, Terrell A. Weight control practices of severely obese patients who are not seeking bariatric surgery. Obesity. 2013;21:1509–13. doi: 10.1002/oby.20488. [DOI] [PubMed] [Google Scholar]
- 29.Ferrante JM, Piasecki AK, Ohman-Strickland PA, Crabtree BF. Family physicians' practices and attitudes regarding care of extremely obese patients. Obesity. 2009;17:1710–6. doi: 10.1038/oby.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wee CC, Davis RB, Chiodi S, Huskey KW, Hamel MB. Sex, Race, and the Adverse Effects of Social Stigma vs. Other Quality of Life Factors Among Primary Care Patients with Moderate to Severe Obesity. J Gen Intern Med. 2014 doi: 10.1007/s11606-014-3041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khawali C, Ferraz MB, Zanella MT, Ferreira SR. Willingness to pay as patient preference to bariatric surgery. Health expectations : an international journal of public participation in health care and health policy. 2014;17:73–81. doi: 10.1111/j.1369-7625.2011.00738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pitzul KB, Jackson T, Crawford S, et al. Understanding disposition after referral for bariatric surgery: when and why patients referred do not undergo surgery. Obes Surg. 2014;24:134–40. doi: 10.1007/s11695-013-1083-z. [DOI] [PubMed] [Google Scholar]
- 33.Sivagnaman P, Rhodes M. Provision of bariatric surgery in Norfolk. British Journal of Healthcare Management. 2008;14:186–90. [Google Scholar]
- 34.Sarwer DB, Ritter S, Wadden TA, Spitzer JC, Vetter ML, Moore RH. Attitudes about the safety and efficacy of bariatric surgery among patients with type 2 diabetes and a body mass index of 30-40 kg/m2. Surg Obes Relat Dis. 2013;9:630–5. doi: 10.1016/j.soard.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Afonso BB, Rosenthal R, Li KM, Zapatier J, Szomstein S. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obes Relat Dis. 2010;6:16–21. doi: 10.1016/j.soard.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 36.Lynch CS, Chang JC, Ford AF, Ibrahim SA. Obese African-American women's perspectives on weight loss and bariatric surgery. J Gen Intern Med. 2007;22:908–14. doi: 10.1007/s11606-007-0218-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Birkmeyer NJ, Gu N. Race, socioeconomic status, and the use of bariatric surgery in Michigan. Obes Surg. 2012;22:259–65. doi: 10.1007/s11695-010-0210-3. [DOI] [PubMed] [Google Scholar]
- 38.Pratt GM, Learn CA, Hughes GD, Clark BL, Warthen M, Pories W. Demographics and outcomes at American Society for Metabolic and Bariatric Surgery Centers of Excellence. Surgical endoscopy. 2009;23:795–9. doi: 10.1007/s00464-008-0077-8. [DOI] [PubMed] [Google Scholar]
- 39.Sudan R, Nguyen NT, Hutter MM, Brethauer SA, Ponce J, Morton JM. Morbidity, mortality, and weight loss outcomes after reoperative bariatric surgery in the USA. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2015;19:171–9. doi: 10.1007/s11605-014-2639-5. [DOI] [PubMed] [Google Scholar]
- 40.Ingraham AM, Cohen ME, Ko CY, Hall BL. A current profile and assessment of north american cholecystectomy: results from the american college of surgeons national surgical quality improvement program. Journal of the American College of Surgeons. 2010;211:176–86. doi: 10.1016/j.jamcollsurg.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 41.Niebisch S, Fleming FJ, Galey KM, et al. Perioperative risk of laparoscopic fundoplication: safer than previously reported-analysis of the American College of Surgeons National Surgical Quality Improvement Program 2005 to 2009. Journal of the American College of Surgeons. 2012;215:61–8. doi: 10.1016/j.jamcollsurg.2012.03.022. discussion 8-9. [DOI] [PubMed] [Google Scholar]
- 42.Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the importance of obesity-related social stigma and functional status. J Gen Intern Med. 2013;28:231–8. doi: 10.1007/s11606-012-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.D. K, A. T. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47:263–91. [Google Scholar]
- 44.Sikorski C, Luppa M, Dame K, et al. Attitudes towards bariatric surgery in the general public. Obes Surg. 2013;23:338–45. doi: 10.1007/s11695-012-0767-0. [DOI] [PubMed] [Google Scholar]
- 45.Thuan JF, Avignon A. Obesity management: Attitudes and practices of French general practitioners in a region of France. Int J Obes. 2005;29:1100–6. doi: 10.1038/sj.ijo.0803016. [DOI] [PubMed] [Google Scholar]
- 46.Tsuda S, Barrios L, Schneider B, Jones DB. Factors affecting rejection of bariatric patients from an academic weight loss program. Surg Obes Relat Dis. 2009;5:199–202. doi: 10.1016/j.soard.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 47.Sansone RA, McDonald S, Wiederman MW, Ferreira K. Gastric bypass surgery: A survey of primary care physicians. Eating Disorders: The Journal of Treatment & Prevention. 2007;15:145–52. doi: 10.1080/10640260701190667. [DOI] [PubMed] [Google Scholar]