Abstract
Exposures to noise and resulting noise-induced hearing loss (NIHL) are not well understood in the dental profession. Previous studies have focused primarily on practicing dental professionals, and have often evaluated hearing loss in the absence of adequate noise exposure assessment. This study was conducted to evaluate exposures among students and staff working in four clinics within a major US university dental school, and to compare these exposures to those among dental professionals in a private general-practice clinic. We measured equivalent continuous average (LEQ) noise exposure levels at 3.75-minute intervals across a variety of procedures in the evaluated clinics, and also had participants complete a brief survey with questions on their experience and perceptions of noise exposure.
We collected 79 partial- or full-shift Time-Weighted Average (TWA) dosimetry measurements on 46 individuals. The mean 3.75-min interval LEQ level was 63.6 ± 13.3 dBA, while the highest 3.75-min interval LEQ was 103.5 dBA. Students from the dental school clinics had the highest variability in average exposure levels, while the pediatric clinic evaluated had the highest average and maximum exposures. Nearly 4% of standardized 8-hr TWA measurements exceeded the 85 dBA Recommended Exposure Limit established by the National Institute for Occupational Safety and Health. Concerns about the potential effects of dental noise on participants’ hearing were significantly correlated with metrics of TWA noise exposure, as well as variability of exposure (as assessed by the SD of the 3.75-min LEQ levels). Our results suggest that dental students and staff may have some risk of developing noise-induced hearing loss, particularly in pediatric clinical settings.
Keywords: Noise, Dentistry, Hearing Loss, Exposure Assessment
INTRODUCTION
Chronic, excessive exposure to hazardous levels of noise is common in many occupations, and, as a result, noise-induced hearing loss (NIHL) is one of the most work-related illnesses in the United States (1). Workers in industries such as manufacturing, mining, construction, and transportation have long been recognized to have excessive exposures to noise (2). However, occupations not historically thought to involve high noise exposures – for example, real estate workers – have recently been identified as having high rates of hearing loss (3). A number of recent studies suggest that dentists, another occupation not typically considered to have excessive exposure to – noise may be at risk of NIHL (4–7). If true, this suggests that a substantial group of dental workers may be at risk; there are an estimated 126,000 general practice dentists, 193,000 dental hygienists, and 6,000 dental specialists in the US alone (8–10). Those who work in dentistry are subjected to noise exposure from their professional tools, including air-turbine and micromotor hand pieces, ultrasonic scalers, sucking tubes, and laboratory equipment. Noise levels associated with clinical handpieces ranged from 76–105 A-weighted decibels (dBA) , and suction ranged from 74–80 dBA, in a 1979 US Army study (11), similar to levels of 70–82 dBA for clinical handpieces and 82–90 dBA for cleaners and scalers reported in a separate study (12). Reports in the contemporary literature suggest that noise levels may not have declined substantially over the intervening 30+ years; mean levels of 70–76 dBA for clinical handpieces and suction were reported in 1998 (13), 66–76 dBA in 2006 (14) 64–97 dBA in 2011 (15) and 75–84 dBA in 2014 (15). It is important to note the majority of these measurements were brief measurements made in close proximity to operating dental instruments, rather than measures of personal exposure, and that noise exposures associated with ultrasonic devices are not completely captured with the A-weighting network used for virtually all occupational exposure assessments, as A-weighting heavily deweights ultrasonic exposures (i.e., exposures to noise frequencies>20 kHz).
Occupational noise exposure regulations typically specify an 8-hour allowable average exposure limit of 85 dBA ((16). Exposures in excess of this level are known to increase the risk of permanent, irreversible NIHL (17), and, more recently, have been recognized as a potential risk factor for the development of non-auditory health effects including hypertension and ischemic heart disease (18). Workers with noise exposures in excess of relevant occupational exposure limits need to be protected through a hearing loss prevention program (HLPP) that includes thorough noise exposure characterization, audiometric testing, noise control, worker training, and routine audiometric testing. In the US, the Occupational Safety and Health Administration (OSHA) requires HLPPs for workers with 8-hour Time-Weighted Average (TWA) noise exposures at or above 85 dBA, and implementation of exposure controls and use of hearing protection devices are required for exposures at or above 90 dBA (19). While many industrial workers are enrolled in HLPPs, professional workers such as dentists are typically not covered by such programs, and as a result little is known about their noise exposures.
The purpose of our study was to assess potential noise exposures among dentists, hygienists and dental students conducting a variety of dental procedures. We did not measure hearing among dental professionals, as has been done in a number of previous studies (4,20). Rather, we set out to better characterize noise exposures during dental work, and to assess possible differences in exposure profiles between dentists, dental hygienists and dental students. A key distinction between this study and previous studies is our use of noise dosimeters to obtain personal average exposures associated with specific dental staff and activities, rather than instantaneous sound pressure measurements made on specific devices, as have been made in a number of previous studies (11,21–23). This approach allows us to evaluate the range of typical personal exposures, rather than emphasizing maximum exposures associated with a single individual dental tool. While such measurements have value in evaluating worst-case exposure scenarios and allowable exposure durations, personal exposure measurements are needed to evaluate the risk of NIHL from chronic exposure to noise.
METHODS
All research procedures were reviewed and approved by the University of Michigan Institutional Review Board prior to data collection. As this was an exploratory study, statistical power was not estimated.
Subjects and sampling locations
Individuals training or working in the school of dentistry at a major US research university, as well as a single private dental clinic located near the university, participated in the study on a volunteer basis. Dental students were invited to participate if they were working in any of four clinics: preclinical, endodontics, prosthodontics, and pediatrics. The preclinical area was used by first and second year students learning the basics, and had open benches that allowed one hundred students to work at the same time. The clinic was chosen to assess situations in which multiple dental hand pieces were in operation at the same time. The endodontics, pediatric, and prosthodontics clinics were used by third and fourth year students specializing in particular branches of dentistry. There were at most ten students working simultaneously in each clinic, and they worked in cubicles that were slightly more private than the preclinical area. The endodontics and prosthodontics clinics were chosen for their repeated use of high and low-speed hand pieces and their uniform procedures, while the pediatric clinic was sampled to explore the potential effects of additional noise generated by children during procedures. Other clinics (n=5) within the dental school were not sampled due to a lack of potential high noise sources or logistical/scheduling constraints.
All professional dentists and dental hygienists employed at the small private clinic, which operated independently from the university and conducted a wide range of dental procedures, were invited to participate. The private clinic was included to allow for comparison of the workplace exposures of professionals to those of students.
Potential subjects in all of the sampled clinics regularly used both high and low-speed dental hand pieces and conducted common procedures. Potential subjects were approached in their respective clinical locations by research staff and provided with a brief overview of the study purpose and procedures. Interested volunteers then provided informed consent and were enrolled into the study and assigned a unique study ID number. Participation rates were not formally assessed, but were estimated to be 50–75% in each of the clinics sampled. In clinics with <5 personnel, some subjects were sampled multiple times in order to obtain a sufficient number of samples.
Noise dosimetry
ER-200D datalogging noise dosimeters (Etymotic Research, Inc, Elk Grove Village, IL) were used to measure equivalent continuous average (LEQ) noise levels using the National Institute for Occupational Safety and Health (NIOSH)-Recommended Exposure Limit (REL) as follows: threshold of 80 dBA, below which noise was not accumulated into the measured dose; a criterion level of 85 dBA; a criterion duration of 8 hours; and a time-intensity exchange rate (ER) of 3 dBA (17). This ER assumes that an increase in average exposure level of 3 dB requires a halving of exposure duration to maintain an equivalent risk of NIHL, or, conversely, that a 3 dB reduction in average exposure allows for a doubling of exposure duration. The NIOSH REL was used for this study, rather than 90 dBA Permissible Exposure Limit promulgated by OSHA, since it is more protective (i.e., allows less exposure at higher levels of noise) and more generalizable (most countries in the world uses exposure limits similar or identical to the NIOSH limit).
The dosimeters were operated according to the manufacturer’s specifications. Noise levels were measured continuously, and the dosimeters datalogged the average and maximum sound pressure level (SPL) measured at manufacturer-preset 3.75-min intervals throughout each dosimeter monitoring period; this datalogging interval cannot be modified. Dosimeters were downloaded using the ER-200D Utility Suite Rev 4.04. The dosimeters were factory calibrated by the manufacturer before and after the study; their design does not permit daily field calibration.
For each measurement, the dosimeters were clipped to each subject’s collar or placed in a laboratory coat or scrubs pocket near the collar to allow the microphone to sit within the 2-foot diameter spherical ‘hearing zone’ around the head (24). Dosimeters were placed on the opposite side of their dominant hand because of the subject’s working posture in reference to the hand pieces in use. For example, if the subject was right-handed, the subject’s left side and left ear were closer to the hand pieces, and thus more likely to receive high nose exposure. The subjects wore the dosimeters until they completed their daily schedule of procedures, a period which ranged from several hours to a full workday. Subjects were not observed during monitoring due to patient privacy concerns. Subjects were monitored on more than one day only if they performed the same activities on each monitored day.
Subject surveys
All subjects were all asked to fill out a brief survey defining their job title, experience level and qualifying their perception of noise. The perception questions on the survey all used five-point response scales; all were developed for this study and have not been validated. The first of three noise-related questions was: “People experience noise in different ways. Do you experience noise generally as…”, with response options of “Extremely disturbing”, “Very disturbing”, “Moderately disturbing,” “Not very disturbing”, or “Not at all disturbing.” The second question was: “Over the past 12 months or so, when you are at the clinic, how much are you bothered, disturbed, or annoyed by noise?”, with response options of “Extremely”, “Very”, “Moderately”, “Slightly”, and “Not at all.” The third question was: “How concerned are you that noise from dental procedures or tools might affect your hearing?”, with response options of “Extremely”, “Very”, “Moderately”, “Slightly”, and “Not at all.” Note that the survey did not enquire about perceived risk of noise exposure and hearing loss from non-occupational activities, as the purpose of this study was to evaluate levels and perceptions of dental noise.
The survey also included a blank log that allowed subjects to record the timing and types of procedures they performed over the course of the measurement period. When finished with their sampling period, each subject would record their day’s work in this log attached to their survey, and then submit these materials, along with the noise dosimeter, to research staff.
Data analysis
Microsoft Excel and SPSS were used to analyze the ER-200D data logs, which consisted of measured averages at 3.75-min intervals. The measured LEQ levels were converted to 8-hour TWA values to allow for comparison of exposures measured over varying durations. This was done using Equation 1:
| (Equation 1) |
where N is the number of 3.75-min datalogged intervals collected in a single measurement, T is 128 (the total number of 3.75-min intervals in an 8-hour period), and LEQ is the measured average noise level over measurement period N for measurement i. Note that this equation assumes that non-measured intervals during a subject’s workday contributed nothing to the daily noise exposure.
Survey analyses were conducted for each monitoring day within subject (for the perception of noise questions, which were time-varying) and at the subject level (for the job title and experience level questions, which were fixed). Descriptive statistics were computed for all evaluated factors from the survey and log, as well as for dosimetry noise levels at the 3.75-min level (i.e., mean and standard deviation [SD] of these levels as a measure of average exposure and variability in exposure) as well as the standardized 8-hr TWA exposure level. We evaluated variability via the SD of the 3.75 min levels because previous studies have demonstrated that individuals may be more annoyed by changing noise than by continuous or steady-state noise (25). Based on measurement period durations, the 8-hr TWA measurements were stratified into “short” and “long” duration exposure groups using a duration cutpoint that created two approximately equally-sized groups, in order to better compare 8-hr TWA levels collected on subjects for which the fraction of time in the 8-hour period that involved dental instrument noise exposure was similar. Scatterplots and bivariate Spearman correlation analyses were run to explore the correlation between the survey answers and the mean 8-hr TWAs (as a measure of overall noise exposure) and 3.75-min LEQ SD (as a measure of variability of noise and potential predictor of annoyance (25)).
RESULTS
A total of 79 partial- or full-shift dosimetry measurements were taken during six weeks of 2015 from 46 subjects (three dentists, six dental hygienists, and 37 students) (Table I). The students had between 3 months and 7 years of dental experience. Subjects from the private clinic were both dentists and dental hygienists with experience that ranged from 12 to 43 years. Eighteen subjects participated more than once, up to a maximum of four times on different days; hygienists had more repeated samples than the other job titles.
Table I.
Experience level of subjects overall and by job title (N=46 subjects)
| Job title | N subjects | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Overall | 46 | 13.7 | 15.5 | <1 | 43 |
| Dentist | 3 | 34.7 | 14.2 | 14 | 43 |
| Hygienist | 5 | 29.9 | 11.0 | 12 | 41 |
| Student | 32 | 4.2 | 3.7 | <1 | 7 |
Noise dosimetry
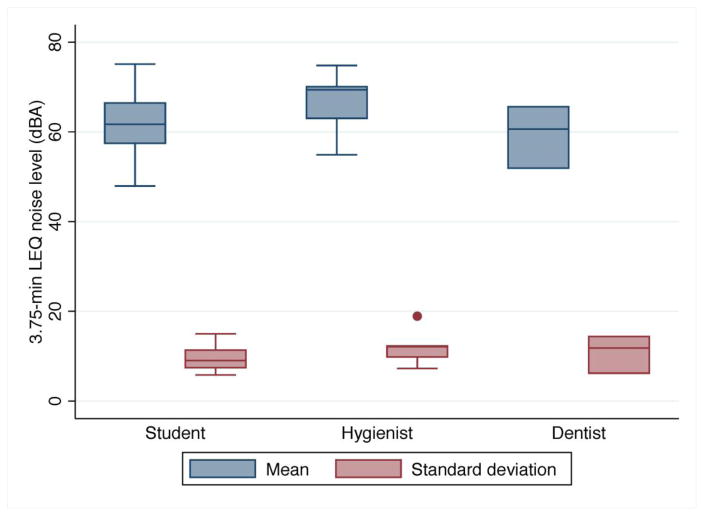
The average dosimetry measurement was 5.5 ± 3.1 hr, with a minimum of 2.2 and a maximum of 8.6 hr (Table II). The arithmetic average 3.75-min interval LEQ was 63.6 ± 13.3 dBA; median 3.75-min interval LEQ levels were highest among hygienists (66.4 dBA), followed by dentists (61.8 dBA) and then students (60.5 dBA, Figure 1) . The highest 3.75-min interval LEQ was 103.5 dBA, and was measured on a student in the pediatric clinic. The median standard deviation across 3.75-min interval LEQ levels within TWA measurement was similar for students (12.7 dBA, dentists (13.6 dBA), and hygienists (14.8 dBA).
Table II.
8-hr TWA noise measurements by job title and clinic (n = 79 measurements)
| 8-hr TWA noise level (dBA)
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Duration (hrs)
|
< 4.5 hrs
|
≥ 4.5 hrs
|
||||||||||||
| Item/category | N subjects | N measure- ments | Mean | SD | Min | Max | N measure- ments | Mean | SD | Max | N measure- ments | Mean | SD | Max |
| Overall | 46 | 79 | 5.5 | 3.1 | 2.2 | 8.6 | 41 | 67.7 | 6.5 | 85.3 | 38 | 74.4 | 6.9 | 92.1 |
| Job title | ||||||||||||||
| Dentist | 3 | 7 | 6.0 | 2.3 | 2.8 | 7.9 | -- | -- | -- | -- | 7 | 74.4 | 1.6 | 77.5 |
| Hygienist | 6 | 19 | 5.5 | 3.4 | 2.2 | 8.2 | 11 | 71.5 | 3.8 | 77.1 | 8 | 75.7 | 2.3 | 78.0 |
| Student | 37 | 53 | 5.1 | 2.4 | 2.9 | 8.1 | 30 | 66.4 | 6.8 | 85.3 | 23 | 74.0 | 8.7 | 92.1 |
| Clinic | ||||||||||||||
| Endodontics | 7 | 11 | 4.5 | 1.9 | 2.7 | 8.4 | 9 | 64.2 | 9.4 | 76.3 | 2 | 73.2 | 3.0 | 75.3 |
| Pediatric | 6 | 17 | 6.9 | 3.0 | 3.9 | 8.6 | 1 | 70.0 | -- | 70.0 | 16 | 76.9 | 7.6 | 92.1 |
| Preclinical | 20 | 20 | 2.5 | 0.4 | 2.4 | 2.7 | 20 | 67.2 | 5.5 | 85.3 | -- | -- | -- | -- |
| Private | 9 | 26 | 5.4 | 2.4 | 2.8 | 8.1 | 11 | 71.5 | 3.8 | 77.1 | 15 | 75.1 | 2.0 | 78.0 |
| Prosthodontics | 4 | 5 | 6.3 | 1.5 | 6.6 | 8.2 | -- | -- | -- | -- | 5 | 64.9 | 7.8 | 72.5 |
|
Duration of measurement (hrs)
|
||||||||||||||
| Ni a | nkb | Mean | SD | Max | nk b | Mean | SD | Max | ||||||
| 46 | 41 | 3.08 | 0.7 | 4.3 | 38 | 7.5 | 1.6 | 9.4 | ||||||
=number of subjects.
=number of partial- or full-shift TWA measurements.
Figure 1.
Distribution of mean and standard deviation 3.75-min LEQ noise levels within TWA measurement (N=79 TWA measurements)
Based on measured exposure durations, a cutpoint of 4.5 hours was used to create “short” and “long” duration exposure groups. The average measurement length for partial-shift TWA measurements <4.5 hours was about 185 minutes, and the average length for the partial- to full-shift TWA measurements ≥4.5 hours was roughly 448 minutes (Table II). On average, the mean 8-hr TWA was below the NIOSH REL of 85 dBA, but 3.8 percent of all 8-hr TWA measurements exceeded the REL. The pediatric clinic had both the highest maximum (92.1 dBA) and average 8-hr TWA exposure (76.9 dBA) of any location for 8-hr TWAs < 4.5 hours and ≥4.5 hours. Among 8-hr TWAs ≥4.5 hours, the pediatric clinic had the highest noise levels, and the prosthodontics clinic the lowest, while among 8-hr TWAs <4.5 hours, the private clinic had the highest noise levels, and the endodontics clinic the lowest.
Students showed greater variability (i.e. SDs that were 2–3 times larger) across 8-hr TWA levels compared to the private clinic dentist and hygienists for measurements < and ≥4.5 hours. The endodontics and pediatrics clinics had the greatest variability for TWA durations <4.5 hours, while the pediatric and prosthodontics clinics had the greatest variability of the clinical groups ≥4.5 hours. Also, the pediatric clinic was the noisiest of all the clinics, with individual 3.75-min interval LEQ levels as high as 103.5 dBA. The private clinic had the smallest variability for 8-hr TWA measurements of all durations.
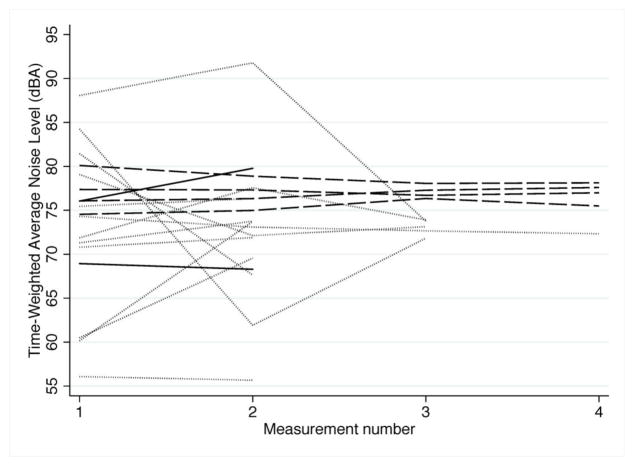
When analyses were restricted to the subset of 19 (41.3%) subjects on whom repeated measurements were available, within-subject patterns of exposure variability became evident (Figure 2). Exposures within student but across day showed the largest variability, as indicated by the dotted lines in Figure 2, while variability within hygienist but across day (dashed line) was quite small. Variability within dentist (solid line) was difficult to assess due to the fact that only two of the dentists assessed were evaluated on multiple days.
Figure 2.
Time-weighted average noise exposure levels among subjects with repeated measurements (N=19 subjects; 2 dentists, 4 hygienists, 13 students). Dotted line = student, dashed line = hygienist, solid line = dentist.
Subject surveys
Table III shows the distribution of subject responses to the three primary survey questions, along with the distribution of job titles at each location evaluated in the study. There were three dentists and six hygienists that worked within the private clinic. All (n=37) of the students worked in the student clinics: endodontics (19%), pediatrics (16%), preclinical (54%), and prosthodontics (11%). Most subjects described general noise in their lives to be “moderately,” “slightly” or “not very” disturbing. None of the dentists or hygienists found dental-related noise “extremely” or “very” disturbing, nor did they express concern for dental-related noise. However, 40% of the hygienists surveyed showed concern over noise in general. The students had a variety of opinions, but most students seemed to be “moderately,” “slightly” or “not very” disturbed by general noise or dental-related noise.
Table III.
Subject job title and location distribution and survey results (N=46 subjects)
| Job title
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Overall
|
Dentist
|
Student
|
Hygienist
|
|||||
| Item/category | N subjects | % | N subjects | % | N subjects | % | N subjects | % |
| Location | ||||||||
| Endodontics | 7 | 15.2 | 0 | 0.0 | 7 | 18.9 | 0 | 0.0 |
| Pediatric | 6 | 13.0 | 0 | 0.0 | 6 | 16.2 | 0 | 0.0 |
| Preclinical | 20 | 43.5 | 0 | 0.0 | 20 | 54.1 | 0 | 0.0 |
| Private practice | 9 | 19.6 | 3 | 100.0 | 0 | 0.0 | 6 | 100.0 |
| Prosthodontics | 4 | 8.7 | 0 | 0.0 | 4 | 10.8 | 0 | 0.0 |
| Disturbed by general noise | ||||||||
| Extremely | 1 | 2.2 | 0 | 0.0 | 1 | 2.7 | 0 | 0.0 |
| Very | 7 | 15.6 | 0 | 0.0 | 5 | 13.6 | 2 | 40.0 |
| Moderately | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Not very | 33 | 73.3 | 2 | 66.6 | 28 | 75.7 | 3 | 60.0 |
| Not at all | 4 | 8.9 | 1 | 33.3 | 3 | 8.1 | 0 | 0.0 |
| Disturbed by dental noise | ||||||||
| Extremely | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Very | 2 | 4.4 | 0 | 0.0 | 2 | 5.4 | 0 | 0.0 |
| Moderately | 14 | 31.1 | 0 | 0.0 | 13 | 35.1 | 1 | 20.0 |
| Slightly | 20 | 44.4 | 3 | 100.0 | 14 | 37.8 | 3 | 60.0 |
| Not at all | 9 | 20.0 | 0 | 0.0 | 8 | 21.6 | 1 | 20.0 |
| Concerned about noise | ||||||||
| Extremely | 2 | 4.4 | 0 | 0.0 | 2 | 5.4 | 0 | 0.0 |
| Very | 7 | 15.6 | 0 | 0.0 | 6 | 16.2 | 1 | 20.0 |
| Moderately | 13 | 28.9 | 2 | 66.6 | 11 | 29.7 | 0 | 0.0 |
| Slightly | 13 | 28.9 | 1 | 33.3 | 10 | 27.0 | 2 | 40.0 |
| Not at all | 10 | 22.2 | 0 | 0.0 | 8 | 21.6 | 2 | 40.0 |
Noise dosimetry vs. subject surveys
Two of the three survey questions (whether the participant found general noise disturbing and whether the participant found noise at the dental clinics disturbing) showed insignificant correlations with measured 8-hr TWA levels (Table IV). However, subjects’ responses to the question addressing their concern about dental noise affecting their hearing were significantly correlated with their measured 8-hr TWAs. The items regarding disturbance by general noise or dental noise were not highly correlated with the variability in 3.75-min interval LEQ levels, but responses to the item regarding concern about noise did show a significant correlation with the SD of the 3.75-min LEQ levels.
Table IV.
Correlations between two metrics of measured noise exposure (8–hr TWA and 3.75 min LEQ) vs perceived noise exposure items
| Correlation
|
||
|---|---|---|
| Noise metric/perceived exposure item | Spearman ρ | p-value |
| 8-hr TWA | ||
| Disturbed by general noise | 0.28 | 0.24 |
| Disturbed by dental noise | 0.65 | 0.04 |
| Concerned about noise | 0.21 | 0.33 |
| SD of 3.75-min LEQ | ||
| Disturbed by general noise | 0.32 | 0.41 |
| Disturbed by dental noise | 0.25 | 0.37 |
| Concerned about noise | 0.59 | 0.04 |
DISCUSSION
The results of our pilot study suggest that dental professionals and students may have a small risk of NIHL. The mean 8-hr TWA noise level was 70.9 dBA, which is well below the NIOSH REL of 85 dBA designed to prevent against NIHL. However, 3.8% of the 79 partial- or full-shift TWA measurements were above the NIOSH REL, indicating that overexposures to noise are possible under some conditions. The pediatric clinic was the environment with the highest average and maximum noise levels, and the greatest variability in levels; this finding was likely driven, at least in part, by child-created noise during procedures. The monitored students showed greater variability in TWA noise exposure levels than did dentists or dental hygienists, probably due to the variety of activities they participate in on a given day of training in the clinic. However, within-shift variability (as measured by the SD of 3.75-min LEQ levels) was similar across students, dentists, and hygienists, suggesting that over the course of a workday each group experiences a variety of activities and subsequently variable noise levels. The endodontics and prosthodontics clinics had the lowest exposures. Survey results, combined with noise dosimetry, suggested that individuals with the highest noise exposure levels were the most disturbed by dental noise, and that individuals with the most variability across their daily noise levels had the most concerns about dental noise. Collectively, these results suggest that concerns about NIHL among dentists and dental students are not unfounded, and present a potential opportunity for education of dental professionals and students regarding the risks of noise and NIHL, with the important caveat that we did not assess perceptions of non-occupational noise, which, for many subjects, may be the more important source of potentially hazardous noise exposure, given the dental noise levels observed in this study.
There are few previous studies of dental noise with which our results can be compared. In 1979, the US Army evaluated exposure to noise from micromotor hand pieces. This study concluded that the average daily use of hand pieces was approximately 14.5 minutes, and noise levels of the devices ranged from 76 to 105 dBA (11). More recent studies have found that despite the changes in technology, including the transition from micromotor hand-pieces to air-turbine hand-pieces, produce similar ranges of noise levels (4,6,12,13,21–23,26–31), and these levels are consistent with our results, as well. Several previous studies have noted high variability in dental noise levels. For example, one study using personal noise dosimetry found that a resident in a pediatric dental clinic had a range of exposures from 94–112.9 dBA (22). The same study found an average exposure of 106 dBA, substantially higher than the mean pediatric clinic 8-hr TWA level measured here of 76.2 dBA. This may be due to structural differences in clinic architecture, or perhaps to an increased frequency of contact with pediatric patients by the resident compared to our own study subjects. Nevertheless, this finding, combined with our own results, suggest that noise exposures are likely to be highest for dental professionals and students in pediatric clinical settings; Jahid et al observed children screaming in a pediatric clinic at a maximum level of 112.9 dBA (measured via personal noise dosimeter, distance from child unknown), and noted that this far exceeded the noise levels observed for dental instruments (22).
In another study, TWA noise measurements made on twelve dentists in a teaching hospital indicated levels of 60.2±8.5 dBA (28), substantially lower than those measured here. However, these levels were measured according to the less conservative OSHA criteria (90 dBA criterion level and 5 dB time-intensity exchange rate), which is well-known to underestimate variable noise exposures compared to the NIOSH criteria used here (32,33). This same study surveyed perceptions of noise among 31 dentists using a previously-evaluated communications difficulty scale, as well as an un-validated item asking dentists to rate their annoyance associated with 10 different dental and non-dental noise sources on a 10-point scale (28). The mean annoyance score in this latter item was >5 for all three sources; seniority was not associated with annoyance scores for dental sources. The authors did not attempt to relate their measured noise exposures to annoyance, as we have done here, so a comparison of the results of the two studies is not possible. Other authors have surveyed perception of dental noise and annoyance from a patient perspective (28), but those evaluations are of little use in the current study of occupational exposures.
There is some evidence that, despite the low average noise exposures found in our study, and the relatively infrequent exposure to high noise during specific procedures, dentists and dental professionals suffer from NIHL. A study of audiometric hearing threshold levels among 53 dentists and 55 other academic professional controls found that dentists had a statistically significant impairment compared to the control subjects at both 3 kHz and 4 kHz (20). More studies found that dentists who regularly used high-speed hand pieces had a significantly higher hearing threshold than dentists who did not regularly use high-speed hand pieces as well as dental students (4,6). In addition to decreased hearing acuity overall, some studies have identified differences in hearing thresholds between ears, which can be a sign of directional noise exposure. For example, one study showed that right-handed dentists had greater hearing loss in their left ears than their right, likely due to the position of the dentists’ bodies relative to the patient and the hand pieces. By comparison, such differences were not noted among other medical professionals (7,34). Our study was not designed to address the directionality of dental noise exposures, but this is a factor that should receive additional attention in future research.
Limitations
Our study had several limitations. The primary limitation is the small sample size characteristic of any pilot study (79 measurements on 46 subjects). The number of dental professionals in particular was small (three dentists and six hygienists). The small sample size may limit the generalizability of the study results to the broader dental professional and student population, but even if the results are representative of only clinical training settings, they are still valuable, as over 40,000 dentists graduate from US dental schools every decade, and all have exposure to noise during their several years of training time (35). A second limitation relates to measurement duration. Some of our measurements were short due to the nature of procedure-based work activities, and may not accurately represent the noise levels that an individual would experience across a full 8-hour workday. Nevertheless, we feel that presenting results in terms of a 8-hr TWA is useful, as it allows for assessment of which work activities have the potential to result in exposure to noise in excess of the NIOSH REL. The long 3.75-min LEQ datalogging intervals inherent to the noise dosimeters used in this study – and not modifiable by the end user - are a third limitation. While the noise dosimeters integrate noise continuously, and the 3.75-min LEQ accurately reflects the mean noise level during that period, the average time a student or professional uses a dental hand pieces is short and often lasts <3.75 min. This limited our ability to conduct tool-specific analysis of noise levels among the subjects assessed; use of instruments with finer temporal resolution appears necessary to identify tasks and equipment that make the largest contribution to exposures among dentists, given the high variability in their exposures. Lack of a mechanism to conduct daily field calibrations of the dosimeters limited our ability to assess the performance of the dosimeters over the course of the study; however, all instruments passed the manufacturer’s calibration process pre- and post-study. In order to protect patient privacy we were unable to observe our subjects continuously over the duration of their exposure measurement. It is possible that some subjects removed the noise dosimeters or wore them incorrectly for some of their measurement, which could have influenced the measured noise levels. However, as the dosimeters were small and unobtrusive, and all subjects were volunteers, this situation is unlikely. Finally, the survey items used in this study have not been validated, and the lack of questions on our survey concerning perceptions of non-occupational noise exposure limits our ability to evaluate the potential importance of, and perceived risk and annoyance associated with, noise from non-dental sources. Given the low exposures noted for most measured dental exposures, non-occupational noise may well represent a larger risk of NIHL than dental activities; however, this possibility cannot be evaluated without additional exposure measurement data.
CONCLUSIONS
Our study suggests that a small proportion of dental professionals and students may be at risk of developing NIHL, depending on the duration of their exposure and their clinical environment. In particular, we found that work in a pediatric dental clinic could result in dental students and professionals being exposed to high levels of noise, likely from the children receiving dental procedures. Note that while the fraction of dental professionals and students with possible overexposures to noise is small, the large number of individuals exposed in these professions may mean that thousands of individuals are at risk of NIHL.
Our study adds to the growing evidence that dentist professionals, and potentially dental students, have some risk of work-related hearing loss from noise exposure. More research is required in order to more accurately assess and quantify the risk of NIHL among dental students and professionals. Ideally, such research will involve inception prospective cohort studies of dentists that assess exposure and hearing ability longitudinally to evaluate the potential causal relationship between dental noise and NIHL. In particular, our finding that within-subject variability across work days varied between students and hygienists suggests that a greater focus on within-subject variability is warranted in future research. Development and validation of additional survey items addressing specific dental and nonoccupational noise exposures, and the relative intensity of these exposures, appears warranted, and would ideally be accompanied by long-term, high-resolution noise dosimetry measurements that would permit quantification of the relative contribution of each of these activities to total noise exposure.
In the meantime, while the risk of NIHL appears to be small, exploration of noise reduction methods may be warranted, both to reduce NIHL risk and negative perceptions of noise among dental professionals and students and to increase patient comfort, and implementation of noise control measures in pediatric clinics for example, better isolation between dental rooms or cubicles – may help reduce patient-related noise exposures. Educational programs on hearing conservation for dentists that include information on likely noise exposures and risk of NIHL may also help reduce fears of NIHL among dental professionals and students. Such programs could be introduced as part of the education of dental students to better ensure awareness of noise and NIHL.
Acknowledgments
This study was supported by funds and equipment from Etymotic Research, Inc, as well as by resources from the University of Michigan Risk Science Center and by grant R21OH010482 from the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. The authors wish to thank the participating subjects and dental clinics, as well as the University of Michigan Dental School, without whose support this research would not have been possible, and Kan Sun for her assistance with data collection.
Footnotes
Conflicts of interest
The study was funded in part by Etymotic Research, a corporation that manufactures hearing protection devices and personal noise dosimeters. The authors have no further conflicts of interest to declare.
Contributor Information
Allison Burk, University of Michigan Department of Environmental Health Sciences, Ann Arbor, MI USA.
Richard L Neitzel, University of Michigan Department of Environmental Health Sciences, Ann Arbor, MI USA.
References
- 1.Sataloff RT, Sataloff J. Occupational Hearing Loss. 3. New York: Taylor & Francis; 1996. [Google Scholar]
- 2.Franks J. Number of workers exposed to occupational noise. Semin Hear. 1988;9(4):287–97. [Google Scholar]
- 3.Masterson EA, Tak S, Themann CL, Wall DK, Groenewold MR, Deddens JA, et al. Prevalence of hearing loss in the United States by industry. Am J Ind Med. 2013;56:670–81. doi: 10.1002/ajim.22082. [DOI] [PubMed] [Google Scholar]
- 4.Theodoroff S, Folmer R. Hearing loss associated with long-term exposure to high-speed dental handpieces. Gen Dent. 2015 Jun;63(3):71–6. [PubMed] [Google Scholar]
- 5.Messano GA, Petti S. General dental practitioners and hearing impairment. J Dent. 2012 doi: 10.1016/j.jdent.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Daud M, Noh N, Sidek D, Abd Rahman N, Abd Rahi N, Zakaria M. Screening of dental staff nurses for noise induced hearing loss. B-ENT. 2011;7(4):245–9. [PubMed] [Google Scholar]
- 7.Khaimook W, Suksamae P, Choosong T, Chayarpham S, Tantisarasart R. The prevalence of noise-induced occupational hearing loss in dentistry personnel. Work Heal Saf. 2014;62(9):357–60. doi: 10.3928/21650799-20140815-02. [DOI] [PubMed] [Google Scholar]
- 8.O*Net Online. Summary Report for: 29-1021.00 - Dentists, General [Internet] O*Net Online; 2015. [cited 2015 Aug 15]. Available from: http://www.onetonline.org/link/summary/29-1021.00. [Google Scholar]
- 9.O*Net Online. Summary Report for: 29-2021.00 - Dental Hygienists [Internet] O*Net Online; 2015. [cited 2015 Aug 15]. Available from: http://www.onetonline.org/link/summary/29-2021.00. [Google Scholar]
- 10.O*Net Online. Summary Report for: 29-1029.00 - Dentists, All Other Specialists [Internet] O*Net Online; 2015. [cited 2015 Aug 15]. Available from: http://www.onetonline.org/link/summary/29-1029.00. [Google Scholar]
- 11.Shields W. Noise Hazards in the Practice of Dentistry. Washington DC: 1979. Report No. AD-A078-221. [Google Scholar]
- 12.Kilpatrick HC. Decibel ratings of dental office sounds. J Prosthet Dent. 1981 Feb;45(2):175–8. doi: 10.1016/0022-3913(81)90336-x. [DOI] [PubMed] [Google Scholar]
- 13.Setcos JC, Mahyuddin a. Noise levels encountered in dental clinical and laboratory practice. Int J Prosthodont. 1998;11(2):150–7. [PubMed] [Google Scholar]
- 14.Sampaio Fernandes JC, Carvalho aPO, Gallas M, Vaz P, Matos Pa. Noise levels in dental schools. Eur J Dent Educ. 2006;10(1):32–7. doi: 10.1111/j.1600-0579.2006.00393.x. [DOI] [PubMed] [Google Scholar]
- 15.Kadanakuppe S, Jyothi C, Bhat P, Ramegowda C. Assessment of noise levels of the equipments used in the dental teaching institution, Bangalore. Indian Journal of Dental Research. 2011:424. doi: 10.4103/0970-9290.87065. [DOI] [PubMed] [Google Scholar]
- 16.Arenas JP, Suter AH. Comparison of occupational noise legislation in the Americas: an overview and analysis. Noise Health. 2014 Jan;16(72):306–19. doi: 10.4103/1463-1741.140511. [DOI] [PubMed] [Google Scholar]
- 17.NIOSH. Criteria for a Recommended Standard: Occupational Noise Exposure, Revised Criteria 1998. Cincinnati, OH: US Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1998. p. 105. [Google Scholar]
- 18.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. The Lancet. 2014:1325–32. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed]
- 19.OSHA. Fed Reg. Washington, D.C: US Department of Labor; 1983. Occupational Noise Exposure: Hearing Conservation Amendment; Final Rule; pp. 9738–85. [Google Scholar]
- 20.Willershausen B, Callaway A, Wolf TG, Ehlers V, Scholz L, Wolf D, et al. Hearing assessment in dental practitioners and other academic professionals from an urban setting. Head Face Med. 2014;10(1) doi: 10.1186/1746-160X-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dutta A, Mala K, Acharya SR. Sound levels in conservative dentistry and endodontics clinic. J Conserv Dent. 2015 doi: 10.4103/0972-0707.108188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jadid K, Klein U, Meinke D. Assessment of noise exposures in a pediatric dentistry residency clinic. Pediatr Dent. 2011;33(4):343–8. [PubMed] [Google Scholar]
- 23.Sampaio Fernandes JC, Carvalho APO, Gallas M, Vaz P, Matos PA. Noise levels in dental schools. Eur J Dent Educ. 2006 doi: 10.1111/j.1600-0579.2006.00393.x. [DOI] [PubMed] [Google Scholar]
- 24.Earshen J. Chapter 3: Sound measurement: Instrumentation and noise descriptors. In: Berger EH, Royster LH, Royster JD, Driscoll DP, Layne ML, editors. The Noise Manual. 5. US: American Industrial Hygiene Association; 2000. pp. 41–100. [Google Scholar]
- 25.Laszlo HE, McRobie ES, Stansfeld SA, Hansell AL. Annoyance and other reaction measures to changes in noise exposure - A review. Science of the Total Environment. 2012:551–62. doi: 10.1016/j.scitotenv.2012.06.112. [DOI] [PubMed] [Google Scholar]
- 26.Al-Dujaili M, Thomson W, Meldrum R, Al-Ani A. Noise levels in dental school clinics. N Z Dent J. 2014 Sep;110(3):105–8. [PubMed] [Google Scholar]
- 27.Choosong T, Kaimook W, Tantisarasart R, Sooksamear P, Chayaphum S, Kongkamol C, et al. Noise Exposure Assessment in a Dental School. Safety and Health at Work. 2011 doi: 10.5491/SHAW.2011.2.4.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yousuf A, Ganta S, Nagaraj A, Pareek S, Atri M, Singh K, et al. Acoustic noise levels of dental equipments and its association with fear and annoyance levels among patients attending different dental clinic setups in Jaipur, India. J Clin Diagnostic Res. 2014;8(4) doi: 10.7860/JCDR/2014/7678.4245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choosong T, Kaimook W, Tantisarasart R, Sooksamear P, Chayaphum S, Kongkamol C, et al. Noise Exposure Assessment in a Dental School. Saf Health Work. 2011;2(4):348. doi: 10.5491/SHAW.2011.2.4.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bahannan S, El-Hamid AA, Bahnassy A. Noise level of dental handpieces and laboratory engines. J Prosthet Dent. 1993 Oct;70(4):356–60. doi: 10.1016/0022-3913(93)90222-a. [DOI] [PubMed] [Google Scholar]
- 31.Chen W-L, Chen C-J, Yeh C-Y, Lin C-T, Cheng H-C, Chen R-Y. Workplace Noise Exposure and Its Consequent Annoyance to Dentists. J Exp Clin Med. 2013 Oct;5(5):177–80. [Google Scholar]
- 32.Neitzel R, Seixas NS, Camp J, Yost M. An assessment of occupational noise exposure in four construction trades. Am Ind Hyg Assoc J. 1999;60:807–17. doi: 10.1080/00028899908984506. [DOI] [PubMed] [Google Scholar]
- 33.Sriwattanatamma P, Breysse P. Comparison of NIOSH noise criteria and OSHA hearing conservation criteria. Am J Ind Med. 2000;37(4):334–8. doi: 10.1002/(sici)1097-0274(200004)37:4<334::aid-ajim2>3.0.co;2-z. 2000/03/08 ed. [DOI] [PubMed] [Google Scholar]
- 34.Sorainen E, Rytkönen E. High-frequency noise in dentistry. AIHA J (Fairfax, Va) 2002;63(2):231–3. doi: 10.1080/15428110208984709. [DOI] [PubMed] [Google Scholar]
- 35.Byck G, Kaste L, Cooksey J, Chou C-F. Dental Student Enrollment and Graduation: A Report by State, Census Division, and Region. J Dent Educ. 2006;70(10):1023–37. [PubMed] [Google Scholar]