Abstract
Poor mental health was prevalent among HIV positive men who have sex with men (HIVMSM), and a tremendous burden extents on their families and society. The present study investigated the prevalence of depression and its relationship with social support, HIV self-stigma, positive affect and negative affect among 321 HIVMSM in Chengdu, China. The study was conducted during July 2013 through October 2013. Findings showed that 55.8% of the participants had mild to severe depression. The results of structural equation modeling showed that social support and positive affect were negatively associated with depression, while HIV self-stigma and negative affect were positively associated with depression. Social support, positive affect, and negative affect mediated the association between HIV self-stigma and depression. The hypothesized model had a satisfactory fit. Interventions improving mental health among this population are warranted.
Keywords: men who have sex with men, depression, positive and negative affect, social support, self-stigma
INTRODUCTION
In China, the HIV epidemic among men who have sex with men (MSM) is worsening. A recent meta-analysis which included 84 studies reported that HIV prevalence among Chinese MSM was 6.5% [1]. Some studies have reported HIV prevalence among MSM of about 20% [2]. In addition to life-threatening physical illnesses, HIV positive men who have sex with men (HIVMSM) have to deal with severe stigma and numerous types of stressors, resulting in high prevalence of psychological problems, such as depression and anxiety. The prevalence of depression among HIVMSM ranges from 35% to 49%, which is higher than that of people living with HIV (PLWH) in general and that of HIV negative MSM in the US and India [3–6], while a recent study conducted in China reported prevalence of mild to severe depression of 62% among PLWH [7]. The burden of the mental health problems affects HIVMSM, their families, and the society tremendously. Poor mental health was also significantly associated with a number of HIV-related health outcomes and risk behaviors, such as low service utilization rate, poor adherence to antiretroviral therapy (ART), faster progression to AIDS and shorter survival [8–11], and practice of unsafe sex [12]. These consequences would further facilitate the transmission of HIV. In China, there is however, a lack of psychological support services and interventions targeting PLWH in general and HIVMSM in particular [13–15]. The World Health Organization has also reported the shortage of psychological support services to MSM [16].
HIV-related stigma is one of the strongest determinants of psychological problems (e.g., depression) among MSM [17, 18] and PLWH in China [19]. High levels of stigma and discrimination experienced by PLWH has been well documented [20]. The situation among HIVMSM is likely to be much worse since they encounter multiple and layered sources of social stigma toward homosexuals and PLWH, in addition to their physical health problems. In particular, self-stigma is developed when individuals internalize prejudice, stereotypes, and discrimination toward themselves [21]. HIV-related self-stigma is strongly associated with depression and other health outcomes and behaviors, such as non-adherence to treatment among PLWH [22]. With effective interventions, however, it is possible to reduce self-stigma [23, 24].
Social support refers to the provision of psychological and material resources by people within one’s social network [25]. It reduces depression among PLWH and is associated with a number of positive outcomes such as well-being [26], hope, and optimism [27]. Provision of advice and emotional support helps participants redefine their stressful situations and may lead to better mental health [25, 28]. One recent study suggested that participation in online support groups had positive impact on psychosocial outcomes among PLWH through an empowering processes which fostered social support and positive meanings [29].
To help the designing of effective interventions, it is important to understand the mechanisms, or mediators, that act between risk factors, such as self-stigma, and depression among HIVMSM. As HIV self-stigma is negatively associated with social support among PLWH [30–33], mediation effect may exist. Those who report self-stigma may isolate themselves and therefore, receive limited social support from others [34]. Many published studies supported that higher levels of self-stigma predicted lower levels of social support [31, 35, 36]. A prospective study found that social support mediated the effect of HIV self-stigma onto psychological distress [31]. In this longitudinal study, the authors found that among PLWH, self-stigma directly impacted psychological well-being seven months later; self-stigma also indirectly impacted psychological well-being via dampened perceived social support [31].
Affect may also play a role in mediating the associations between self-stigma and depression as affect regulation is an important determinant of mental health problems [37, 38]. Positive affectivity is a trait that reflects stable individual differences in positive emotional experience [39], while negative affect reflects a general dimension of subjective distress and unpleasant engagement that subsumes a variety of aversive mood states, including anger, contempt, disgust, guilt, fear, and nervousness [40]. A number of studies have investigated associations between positive and negative affects and depression in various populations. The findings support the Tripartite Model which posits that depression is characterized by increased negative affect and reduced positive affect [41]. Positive affect is positively associated with better physical, social, and psychological well-being of PLWH [42–44] and negatively associated with depressive symptoms among undergraduate students [45]. Negative affect is positively associated with depression in general [46]. To our knowledge, there is no study investigating the relationship between positive and negative affects and depression among PLWH and HIVMSM.
It is important to recognize that positive affect and negative affect can be improved via interventions. For instance, the Three Good Things exercise, a positive psychological intervention which requests participants to write down three good things that they experience and feel grateful, was found to be effective in increasing positive affect [47]. Previous studies have shown that increase in positive affect facilitates better coping with stressors related to HIV, while reduction in negative affect facilitates performance of self- care behaviors [48].
Positive affect and negative affect are also positively and negatively associated with social support among PLWH [49]. Social support can increase positive affect through senses of stability, predictability, and control that it provides [50]. Availability of emotional support can help regulate emotion and hence strengthen positive affect and reduce negative affect [48]. Previous findings have suggested that positive affect and negative affect are important pathways through which social support influences illness management strategies among PLWH [48, 49]. However, the hypothesis that positive affect and negative affect mediate the association between social support and depression among PLWH has not been tested in literature.
As HIV self-stigma is associated with social support [31], it is possible that the association between HIV self-stigma and depression among HIVMSM may also be mediated by positive affect and negative affect. Qualitative studies have suggested that self-stigma is associated with various negative emotions such as stress, guilt, and shame [51, 52], which are risk factors of depression. We cannot locate studies reporting associations between HIV self-stigma and positive and negative affects among HIVMSM; the mediation hypothesis has hence not been tested. If such mediating effects exist, psychological interventions improving positive affect and/or negative affect may reduce the risk effect of HIV self-stigma in developing depressive symptoms.
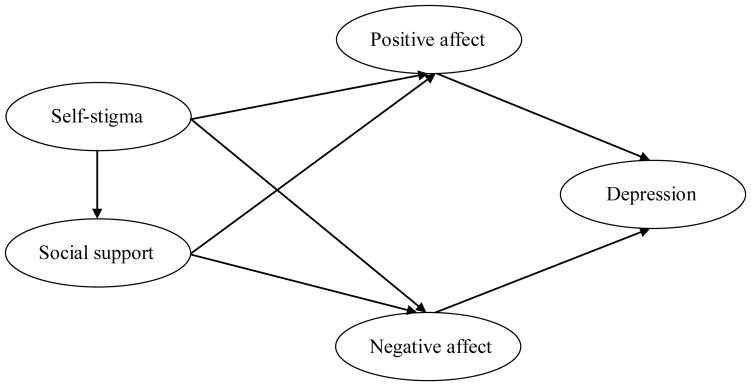
The present study investigated the prevalence of probable depression among HIVMSM in China. We investigated further by using a structural equation modeling approach, the associations between social support, HIV self-stigma, and positive/negative affects onto depressive symptoms. The hypothesized model is shown in Figure 1. It includes the following components: 1) social support and positive affect are negatively associated with, and HIV self-stigma and negative affect are positively associated with, depressive symptoms; 2) HIV self-stigma is negatively associated with social support; 3) social support is positively associated with positive affect and negatively associated with negative affect, while the opposite is true for HIV self-stigma; and 4) HIV self-stigma has an indirect effect onto depression via social support and positive/negative affect. One more model was tested to examine whether the addition of direct path from HIV self-stigma to depression would improve goodness-of-fit. This model investigated the extent to which that the association between self-stigma and depression is mediated by social support, positive affect, and negative affect.
Figure 1.
Hypothesized structural model (model1) in the study relating depression, self-stigma, positive affects, negative affects, and social support.
METHODS
Study population and procedure
Inclusion criteria included: 1) Chinese men who have anal sex with at least one man in the last six months, 2) age 18 years old or above, and 3) having been diagnosed as being HIV positive for at least three months. Similar inclusion criteria has been used in a number of published studies [53, 54].
The cross-sectional study was conducted in Chengdu, China, from July 2013 to October 2013. Participants were recruited by four well-trained peer fieldworkers, who were staff of a local non-governmental organization (NGO). The NGO was one of the largest gay organizations in China. It publicized the study through posters displayed at the public area of the NGO and social media to their service users. The fieldworkers approached prospective participants, briefed them about the study and logistics, and invited them to participate in the study after confirming their eligibility. Interested participants were invited to visit the office of the NGO and met with a research assistant there. It was confirmed that participants’ refusal would not affect their right to use any services and they could quit the interview at any time without being questioned. After obtaining written informed consent, anonymous face-to-face interviews, using a pilot-tested and structured questionnaire, which took about 20 minutes to complete, were conducted in a private room. Upon completion of the interview, a monetary compensation of RMB 50 (about USD 6) was provided to the participants to compensate their time.
There were about 1,000 HIVMSM identified in Chengdu [55, 56]. The NGO served about 600 of them at the time of the study and could potentially contact them by phone call and social media. Of these, 350 were successfully contacted by the peer fieldworkers, of whom 321 (91.7%) completed the interview with written informed consent. Ethics approval was obtained from the Survey and Behavioural Research Ethics Committee of the Chinese University of Hong Kong.
Measures
Participants’ background characteristics
Information was collected about participants’ demographic characteristics including ethnicity (Han vs. other ethnicity), residence, age, education level (primary school or below, junior high school, senior high school, vs. university or above), marital status (i.e., single, married, cohabiting with girlfriend, cohabiting with boyfriend, divorced, widowed, vs. others), job, personal monthly income (in RMB), and sexual orientation (homosexual, heterosexual, bisexual, vs. not sure).
Social support
Two items were constructed in this study to gauge the level of emotional and material social support participants received. Participants were asked: 1) “How much support can you obtain from family/friends/colleagues when you need to talk or to obtain emotional support?” and 2) “How much support can you obtain from family/friends/colleagues when you need material support (e.g., financial help)?” Responses were recorded on scales that ranged from 0 (‘none’) to 10 (‘tremendous’). The Cronbach’s alpha value of the scale formed by adding up the item responses of the two questions, was 0.68 in this study.
Self-stigma
The level of self-stigma was assessed by using the 9-item Self-Stigma Scale-Short Form (SSS-S) [57]. Participants were asked to rate each item on a 4-point Likert scale that ranged from 1 ‘strongly disagree’ to 4 ‘strongly agree’, with higher scores indicating a stronger sense of self-stigma. Example items include “I fear that others would know that I am a PLWH”, “I feel uncomfortable because I am a PLWH”, and “I feel like I cannot do anything about my PLWH status”. The SSS-S has three subscales, with 3 items in each subscale: 1) affective components, 2) cognitive components, and 3) behavioral components. Scores for each subscale range from 3 to 12. The Chinese version has been validated among people with mental illness in Hong Kong (Cronbach’s alpha ranged from 0.84 to 0.91) [57]. In the present study, the Cronbach’s alpha value was 0.90. The Cronbach’s alpha values for the affective, cognitive, and behavioral subscales were 0.68, 0.74, and 0.86, respectively.
Positive affect and negative affect
To assess positive affect and negative affect, the 20-item Positive and Negative Affect Schedule (PANAS) scale [40] was administered. As pointed out by Watson and Clark (1997), positive affect and negative affect are two distinct constructs rather than two extremes of the same dimension [58]. PANAS has been used in the Chinese population (Cronbach’s alpha value was 0.85 for the Positive Affect Subscale and 0.83 for the Negative Affect Subscale) [59]. It consists of 20 items, in which 10 items reflect expectations for positive affect and 10 for negative affect. Participants were asked to rate to what extent they feel this way at the present moment on a 5-point Likert scale (‘very slightly or not at all’ to ‘extremely’). Scores for each subscale range from 10 to 50, with higher scores representing higher levels of positive affect and negative affect. In this study, the Cronbach’s alpha value was 0.86 for the Positive Affect Subscale and 0.93 for the Negative Affect Subscale.
Depression symptoms
The 20-item Center for Epidemiologic Studies Depression Scale (CES-D) [60] was used to assess the presence of depressive symptoms. The Chinese version of the CES-D was validated, showing good internal reliability [60–62]. The Cronbach’s alpha value for CES-D ranged from 0.84 to 0.91 among PLWH [63–66] and from 0.85 to 0.92 among MSM [67–69]. Participants were asked to rate how often they have experienced the symptomatology in the past seven days, on a 4-point Likert scale [‘rarely or none of the time (less than 1 day)’ to ‘almost or all of the time (5–7 days)’]. The total score ranges from 0 to 60, with higher score reflecting greater severity. The CES-D is composed of four dimensions: somatic symptoms (total score ranges from 0 to 21), depressed affect (total score ranges from 0 to 21), (lack of) positive affect (total score ranges from 0 to 12), and interpersonal problems (total score ranges from 0 to 6). Example items include “My sleep was restless”, “I felt depressed”, “I was happy”, and “people were unfriendly”. A score of 16 or more is suggestive of the presence of depressive symptoms (probable depression), and a score of 25 or more is highly associated with major depression. In this study, the Cronbach’s alpha value was 0.92. The Cronbach’s alpha values of the four dimensions were 0.86, 0.89, 0.76, and 0.77, respectively.
Statistical analysis
First, zero-order correlations among all variables were examined, and multiple regression analyses were conducted to examine the contribution of demographic characteristics to the studied variables using SPSS 16.0 (SPSS Inc., Chicago, IL). Second, confirmatory factor analysis (CFA) was conducted to assess the goodness of fit of the measurement model [70]. CFA establishes convergent and divergent validity in the proposed model, which is requested by many SEM researchers as a required first step before undertaking structural analysis [70, 71]. Third, structural equation modeling (SEM) was performed by AMOS 17.0 to test the hypothesized model (Model 1). The maximum likelihood method was used. The maximum likelihood method is the most common method of estimating model parameters, which picks estimates with the greatest chance of reproducing covariance in the observed data [71]. The normality was also tested for all indicator variables. To evaluate the overall model fit, we used indices including χ2/df ratio, comparative fit index (CFI), incremental fit index (IFI), and root-mean-square error of approximation (RMSEA). For each index, the following criteria was applied: i) χ2/df ratio values less than 3 indicates a good model fit [70, 72]; ii) CFI and IFI values greater than 0.9 indicates a good model fit [73]; and iii) for RMSEA, a value between 0.05 and 0.08 indicates an acceptable model fit [74]. Fourth, one more model (Model 2) was fitted to test mediations of the associations between HIV self-stigma and depression. In Model 2, a direct path from self-stigma to depression was added to Model 1. Lastly, Model 3 was fitted to test the significance of the direct effect of social support to depression. The total, direct, and indirect effects of the final model were calculated by a bootstrap procedure [75]. As suggested by Shrout and Bolger [76], bias-corrected confidence intervals for each direct and indirect path were reported and calculated in the bootstrap analysis by AMOS 17.0, based on 5,000 bootstrap samples. All statistical tests were two sided, and a p-value<0.05 was considered statistically significant. Since a potential debate on using parcel items exists and the scales on Positive Affect and Negative Affect do not have subscales for parceling the items meaningfully, items were not parceled to avoid arbitrary decisions. We followed the widely used procedure [71] that correlations between the pairs of residuals of some items with the largest Modification Indices (MI) values would be added until the model reaches a satisfactory fit.
RESULTS
Sample characteristics
Among the 321 participants, 58.6% were <30 years old; 10.3% were currently married with a woman or cohabiting with a girlfriend; 59.8% had attended university or above; 10.6% had had monthly personal income of less than 1,000 RMB (160 USD); 85.0% indicated that they were homosexuals; and 33.0% did not have a full-time job (Table 1).
Table 1.
Demographic characteristics of HIVMSM
| Frequency (N=321) | Percentage (%) | |
|---|---|---|
| Demographic Characteristics | ||
| Ethnicity | ||
| Han | 315 | 98.1 |
| Others | 6 | 1.9 |
| Residence (Hukou) | ||
| Chengdu | 174 | 54.2 |
| Others | 147 | 45.8 |
| Age | ||
| <=25 | 88 | 27.4 |
| 26–30 | 100 | 31.2 |
| 31–40 | 96 | 29.9 |
| >40 | 37 | 11.5 |
| Education level | ||
| Junior high school or below | 34 | 10.6 |
| Senior high school | 95 | 29.6 |
| University or above | 192 | 59.8 |
| Marital status | ||
| Single | 203 | 63.2 |
| Married/cohabiting with girlfriend | 33 | 10.3 |
| Cohabiting with boyfriend | 63 | 19.6 |
| Divorced/widow/others | 22 | 6.9 |
| Job | ||
| Full-time | 215 | 67.0 |
| Part-time | 20 | 6.2 |
| Unemployed | 26 | 8.1 |
| Student | 17 | 5.3 |
| Individually owned business | 29 | 9.0 |
| Retired/others | 14 | 4.4 |
| Personal monthly income | ||
| <=1000 | 34 | 10.6 |
| 1001–3000 | 142 | 44.2 |
| 3001–5000 | 97 | 30.2 |
| 5001–7000 | 26 | 8.1 |
| >7000 | 22 | 6.9 |
| Sexual orientation | ||
| Homosexual | 273 | 85.0 |
| Bisexual | 39 | 12.1 |
| Heterosexual/not sure | 9 | 2.8 |
The mean score of the overall self-stigma scale was 24.1 (SD=5.51). The mean score for the three subscales of self-stigma was 8.6 (SD=1.85), 8.2 (SD=2.01), and 7.3 (SD=2.29), respectively. The mean score of Positive Affect subscale and Negative Affect subscale was 27.1 (SD=7.34) and 22.9 (SD=8.68), respectively (Table 2).
Table 2.
Mean, standard deviation of the variable and correlation between variables in the study
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Self-stigma | – | ||||
| 2. Social support | −.25*** | – | |||
| 3. Positive affect | −.19** | .20*** | – | ||
| 4. Negative affect | .56*** | −.32*** | −.15** | – | |
| 5. Depression | .59*** | −.36*** | −.36*** | .80*** | – |
|
| |||||
| Mean (SD) | 24.06 | 12.70 | 27.11 | 22.95 | 19.59 |
| Standard deviation | 5.51 | 4.86 | 7.34 | 8.68 | 11.39 |
p<.01,
p<.001
Prevalence of probable depression
The prevalence of probable mild (16≤CESD<20), moderate (20≤CESD<25) and severe (CESD≥25) depression was 12.8%, 11.2% and 31.8%, respectively (mild to severe: 55.8%). The mean CES-D score was 19.6 (SD=11.39). The mean score for the four subscales of CES-D was 6.4 (SD=4.47), 6.5 (SD=4.75), 5.7 (SD=3.06) and 1.0 (SD=1.37), respectively.
Associations between background characteristics and studied variables
Multiple regression results showed that demographic characteristics (i.e., ethnicity, residence, age, education level, marital status, job, personal monthly income, and sexual orientation) explained a small percentage of variance across the studied variables (probable depression, self-stigma, positive affect, negative affect, and social support). Adjusted R2 only ranged from 0.02 to 0.03 (p value ranged from 0.015 to 0.064). Significant demographic variables (i.e., age, marital status, and sexual orientation) were hence adjusted in subsequent analyses although they had limited contribution to explaining variances of depressive symptom (adjusted R2=0.021, p=0.064), self-stigma (adjusted R2=0.034, p=0.016), social support (adjusted R2=0.028, p=0.031), positive affect (adjusted R =0.034, p=0.015), and negative affect (adjusted R =0.027, p=0.035).
Correlations between variables
Table 2 shows the means, standard deviations, and correlations for all variables in this study. Most variables in the model were correlated with each other in a way that supported the relationships suggested by the SEM model. Specifically, self-stigma showed significant positive correlations (r ranged from 0.56 to 0.59, p<0.001, Table 2) with negative affect and depression, as well as negative correlations (r ranged from −0.19 to −0.25, p<0.01, Table 2) with positive affect and social support. In addition, positive affect showed significant negative correlations (r = −0.36, p<0.001, Table 2), whilst negative affect showed positive correlations (r = 0.80, p<0.001, Table 2) with depression.
Measurement model
Table 3 presents the factor loadings of the measurement model. The test of the measurement model resulted in the following statistical values: χ2/df ratio=3.39, CFI=0.85, IFI=0.85, RMSEA=0.086 (90% CI=0.081, 0.092), which were indicative of the need for some modifications. The following modifications were made: i) the item of alert in positive affect was excluded from the final model due to its non-significant and limited contribution to positive affect (Unstandardized and standardized loading (positive affect to alert) is 0.003 and 0.002 respectively, Table 3); and ii) Based on the Modification Indices provided in the CFA results, three correlation paths between some positive affect items residuals (i.e., between strong and determined, between inspired and determined, and between determined and attentive) and five correlation paths between some negative affect items residuals (i.e., between distressed and upset, between guilty and ashamed, between hostile and irritable, between nervous and afraid, and between jittery and afraid) with the largest MI values were added until the model reaches a satisfactory fit. This modification procedure has been widely used [71]. Results of the CFA showed that the overall modified measurement model yielded a satisfactory fit, χ2/df ratio=2.57, CFI=0.91, IFI=0.91, RMSEA=0.07 (90% CI=0.064, 0.076). Standardized factor loading of the modified measurement model ranged from 0.42 to 0.94 and were all statistically significant at the level of p<0.001 (Table 3).
Table 3.
Unstandardized and standardized loading for measurement model
| Parameter estimate | Original measurement model | Modified measurement model | ||
|---|---|---|---|---|
|
| ||||
| Unstandardized loading | Standardized loading | Unstandardized loading | Standardized loading | |
| Positive affect → interested | 1.00 | 0.71 | 1.00 | 0.73 |
| Positive affect → excited | 0.82 (0.072)*** | 0.68 | 0.81 (0.068)*** | 0.70 |
| Positive affect → strong | 0.92 (0.089)*** | 0.62 | 0.85 (0.085)*** | 0.59 |
| Positive affect → enthusiastic | 1.11 (0.091)*** | 0.73 | 1.06 (0.085)*** | 0.73 |
| Positive affect → proud | 1.12 (0.094)*** | 0.72 | 1.10 (0.088)*** | 0.73 |
| Positive affect → alert | 0.00 (0.090) | 0.00 | NA | NA |
| Positive affect → inspired | 1.07 (0.092)*** | 0.69 | 1.01 (0.087)*** | 0.68 |
| Positive affect → determined | 0.90 (0.089)*** | 0.61 | 0.74 (0.084)*** | 0.52 |
| Positive affect → attentive | 1.03 (0.085)*** | 0.72 | 0.95 (0.080)*** | 0.69 |
| Positive affect → active | 1.09 (0.090)*** | 0.73 | 1.06 (0.085)*** | 0.73 |
| Negative affect → distressed | 1.00 | 0.83 | 1.00 | 0.82 |
| Negative affect → upset | 0.79 (0.054)*** | 0.73 | 0.79 (0.045)*** | 0.71 |
| Negative affect → guilty | 0.88 (0.068)*** | 0.66 | 0.87 (0.070)*** | 0.64 |
| Negative affect → scared | 1.04 (0.056)*** | 0.84 | 1.05 (0.058)*** | 0.84 |
| Negative affect → hostile | 0.73 (0.055)*** | 0.67 | 0.74 (0.056)*** | 0.68 |
| Negative affect → irritable | 0.82 (0.068)*** | 0.62 | 0.82 (0.070)*** | 0.61 |
| Negative affect → ashamed | 0.92 (0.066)*** | 0.69 | 0.92 (0.068)*** | 0.68 |
| Negative affect → nervous | 0.95 (0.057)*** | 0.79 | 0.95 (0.059)*** | 0.78 |
| Negative affect → jittery | 1.10 (0.060)*** | 0.84 | 1.10 (0.062)*** | 0.84 |
| Negative affect → afraid | 1.17 (0.063)*** | 0.84 | 1.16 (0.066)*** | 0.83 |
| Self-stigma → affective | 1.00 | 0.86 | 1.00 | 0.86 |
| Self-stigma → cognitive | 1.12 (0.059)*** | 0.89 | 1.12 (0.059)*** | 0.89 |
| Self-stigma → behavioral | 1.10 (0.069)*** | 0.77 | 1.11 (0.069)*** | 0.77 |
| Social support → emotional | 1.00 | 0.69 | 1.00 | 0.68 |
| Social support → material | 1.17 (0.189)*** | 0.76 | 1.17 (0.190)*** | 0.76 |
| Depression → somatic complaints | 1.00 | 0.90 | 1.00 | 0.90 |
| Depression → depressed affect | 1.12 (0.042)*** | 0.94 | 1.12 (0.042)*** | 0.94 |
| Depression → lack of positive affect | 0.32 (0.041)*** | 0.42 | 0.32 (0.041)*** | 0.42 |
| Depression → interpersonal problems | 0.25 (0.015)*** | 0.73 | 0.25 (0.015)*** | 0.73 |
Note: Standard errors are in parentheses
p<0.001.
Structural models
Results of the SEM showed that Model1 (Figure 2) yielded a satisfactory fit [χ2/df ratio=2.46, CFI=0.90, IFI=0.90, RMSEA=0.068 (90% CI=0.062, 0.073)]. In sum, self-stigma exerted its effect onto depression indirectly via social support, positive affect, and negative affect. The overall Model 1 explained 79.8% of the variance in depressive symptoms. The standardized path coefficients of the structural Model 1 are presented in Figure 2.
Figure 2.
Hypothesized structural model (model 1, 2 and 3) relating depression, self-stigma, positive affects, negative affects, and social support.
Note: All path coefficients and factor loadings shown were standardized. *p<0.05, **p<0.01, ***p<0.001
Testing mediation effects of the associations between self-stigma and depression
Model 2 improved significantly as compared to Model 1 (p=0.005, Table 4). The association between self-stigma and depressive symptoms was partially mediated by positive affect, negative affect, and social support (Figure 2). Self-stigma also had significant direct effect on depressive symptoms (Figure 2). Results of the SEM showed that Model 2 yielded a satisfactory fit [χ2/df ratio=2.46, CFI=0.90, IFI=0.90, RMSEA=0.067 (90% CI=0.062, 0.073)]; the overall Model 2 explained 80.0% of the variance in depressive symptoms. The standardized path coefficients of Model 2 are also presented in Figure 2.
Table 4.
Goodness-of-fit of hypothesized structural models (model 1 and 2).
| CFI | IFI | RMSEA | X2/df | Chi-square | df | p-value | |
|---|---|---|---|---|---|---|---|
| Models | |||||||
| Model 1 | 0.90 | 0.90 | 0.068 | 2.46 | 1022.62 | 415 | |
| Model 2 | 0.90 | 0.90 | 0.067 | 2.45 | 1014.78 | 414 | |
| Model 3 | 0.90 | 0.90 | 0.067 | 2.45 | 1012.35 | 413 | |
|
| |||||||
| Comparisons | Changes in χ2 | Changes in df | |||||
|
| |||||||
| Model 2 vs. Model 1 | 7.84 | 1 | 0.005 | ||||
|
| |||||||
| Model 3 vs. Model 2 | 2.43 | 1 | 0.119 | ||||
Model 1: No direct path from self-stigma/social support to depression.
Model 2: A direct path from self-stigma to depression was added to Model 1.
Model 3: A direct path from social support to depression was added to Model 2.
Model 3 did not improve significantly in terms of goodness-of-fit, as compare to Model 2 (p=0.119, Table 4). Social support had no significant direct effect on depressive symptoms (Figure 2). Results of the SEM showed that Model 3 yielded a satisfactory fit [χ2/df ratio=2.45, CFI=0.90, IFI=0.90, RMSEA=0.067 (90% CI=0.062, 0.073)]; the overall Model 3 explained 80.0% of the variance in depressive symptoms. The standardized path coefficients of Model 3 are also presented in Figure 2.
Table 4 compared the goodness-of-fit of Model 1 and 2. Model 2, by adding a direct path from self-stigma to depression, significantly improved goodness-of-fit as compared to Model 1; while Model 3, did not have significant improvement in the goodness-of-fit as compared to Model 2. Thus we chose Model 2 as the final model. Table 5 assessed the sizes of the total, direct, and indirect effects of the final model (Model 2) by bootstrapping procedures. The estimated mediation effect from self-stigma to depression via affects and social support was 0.48 (95%CI: 0.39, 0.58; p<0.001; Table 5). The mediation effect via each specific path is shown in Table 5.
Table 5.
Bootstrap Analyses of total, direct, and indirect effects of the mediation model
| Paths | Effect (95% CI)^ | p-value |
|---|---|---|
| Direct effect | ||
| Self-stigma→Depression | 0.131 (0.031, 0.246) | 0.009 |
| Indirect effect | 0.484 (0.389, 0.582) | <0.001 |
| Self-stigma→Positive affect→Depression | 0.034 (0.005, 0.086) | 0.008 |
| Self-stigma→Negative affect→Depression | 0.382 (0.234, 0.518) | <0.001 |
| Self-stigma→Social support→Positive affect→Depression | 0.011 (0.001, 0.044) | 0.031 |
| Self-stigma→Social support→Negative affect→Depression | 0.056 (0.009, 0.152) | 0.006 |
| Total effect | 0.615 (0.508, 0.704) | <0.001 |
bias-corrected confidence intervals were presented based on 5,000 bootstrap samples.
DISCUSSION
The study examined effects of risk and protective factors (self-stigma and social support) on depressive symptoms among Chinese HIVMSM and tested the mediation roles of positive affect and negative affect regarding such associations. The findings showed that social support was negatively associated with self-stigma. In addition, higher levels of self-stigma were associated with higher levels of depression, and such association was partially mediated by lower social support, lower positive affect, and higher negative affect.
This study confirmed the importance of social support to mental health status of HIVMSM. Our results support existing literature [26, 27] that social support is associated with better health among PLWH. However, many HIVMSM may have inadequate level of social support. This is partially because PLWH often feel isolated and seldom disclose their HIV status to others due to high levels of discrimination and stigmatization [77], contributing to unavailability of social support. In China, over 90% of PLWH did not voluntarily disclose their HIV status to others [77]. Also, 27.2–38.8% of their community members (e.g., neighbors, colleagues, family members, and medical staff) showed negative attitudes after discovering their HIV positive status [77]. Hence the support that they could seek from their family members and friends is very limited [78]. Effective programs enhancing perceived social support are greatly warranted.
We also found significant associations between social support and higher levels of positive affect and lower levels of negative affect. One possible explanation might be that those with higher levels of social support are more likely to receive more love and care, which may lead to higher levels of positive affect and lower levels of negative affect. Such better affect status would in turn result in better mental health.
Many studies reported a high level of self-stigma among PLWH. The present study highlighted the detrimental impact of self-stigma on mental health of PLWH. Such results were consistent with other studies [31, 79]. Findings also suggested that the positive association between self-stigma and depression is partially mediated by lower levels of positive affect, higher levels of negative affect, and lower levels of social support. This finding confirmed previous findings from Mak and her colleagues’ study that self-stigma indirectly impacts psychological well-being via dampened perceived social support [31]. One possible explanation may be that those who report self-stigma may isolate themselves and therefore, receive limited social support from others. Indeed, previous findings have reported that self-stigma is associated with fear of disclosure [80] and social distancing [34].
In the present study, higher level of negative affect and lower level of positive affect were found to be associated with depression, findings corroborating with those of the Tripartite Model [41]. The relatively weak correlation between positive affect and negative affect supported that the two constructs are separate constructs [58]. It is also found that the effect of negative affect is stronger than that of positive affect on depression. It may be due to the fact that the factors in the CESD (somatic complaints, depressed affect, lack of positive affect, interpersonal problems), which was used to measure depressive symptoms in this study, tended to capture better negative affect better compared to positive affect. Indeed, studies have suggested that the items on somatic complaints, depressed affect, and interpersonal problems were found reliable and valid in measuring depressive symptomatology, while items in the positive affect factor were only weakly related to other measures of psychological distress [81].
Findings of the present study have important implications on how to improve mental health among PLWH. First, the study highlights the importance of improving the social support of PLWH in reducing depression symptoms. PLWH tend to seek support from other PLWH, rather than close friends and family members due to the issue of disclosure and social acceptance [34]. Peer support groups were found effective in increasing social support [82]. It is also important to note that online support groups may offer some benefits for PLWH [29]. Therefore it is necessary to encourage PLWH to join peer/online support groups so they can receive support from peers. Secondly, this study also suggests that interventions should aim to reduce self-stigma among PLWH. Empirical data has suggested that self-stigma can be reduced through interventions, e.g. counseling, cognitive behavioral therapy, self-help, or support groups [23, 24]. Third, as we further found that the protective factor of social support is strongly and negatively associated with self-stigma, interventions preventing depression among HIVMSM should integrate components of self-stigma reduction and enhancement of social support. Fourth, the results suggest that self-stigma reduction programs should also integrate affect interventions, given the significant mediation effects of positive affect and negative affect. Positive psychology interventions (PPI) have been developed and tested among general populations, such as undergraduate students, and were found effective in enhancing positive affect [83]. A pilot positive affect intervention that incorporated eight skills (e.g., noticing positive events, gratitude, and personal strengths) has been applied to newly diagnosed PLWH and was found effective in increasing positive affect and reducing negative affect [84]. It has, however, never been applied to the population of HIVMSM. More studies are greatly warranted.
There were several limitations in the current study. First, we cannot derive any conclusive causal relationships as this study used a cross-sectional design. Although this study provided evidence that higher levels of self-stigma are associated with lower social support, lower positive affect and higher negative affect, which in turn increases depressive symptoms, longitudinal studies are warranted to further explicate the causalities between these variables. Second, the results may not be generalized to other cultures and populations. Third, reporting bias may exist due to the nature of self-reported data. Fourth, selection bias may exist as this study had a convenient sample which did not include all HIVMSM in Chengdu and there were non-contacts. Fifth, the measurement on social support was self-constructed for this study and has not been validated. It only included two items measuring emotional support and material support (a part of instrumental support), which may be less ideal to form a latent variable in SEM. The Cronbach’s alpha for this self-constructed measurement was moderate. However, it is important to point out that the use of self-constructed items for social support was very commonly in the literature [85, 86]. Sixth, the sample size of 321 may not be enough for this study. Seventh, the values of the model fit indices were close to the lower boundary of the recommended range [73]. Eighth, depression was measured using self-reported instrument. Therefore misclassification errors might exist.
In sum, this study is among the first to examine the importance of positive and negative affects and social support as mechanisms though which self-stigma related to depressive symptoms among HIVMSM. Results suggested that there is a need to reduce HIV self-stigma and increase social support in improving mental health among PLWH. Affect interventions (e.g., positive psychological interventions) should be integrated in programs that aim to reduce self-stigma.
Acknowledgments
The study was supported by a 2013 international developmental grant from the Lifespan/Tufts/Brown Center for AIDS Research (P30AI042853) and the National Natural Science Foundation of China (81302479). We thank the local NGO, Chengdu Tongle Health Counseling Service Center for its support. Our thanks also extend to all participants who have taken part in this study and all research assistances for their support on data collection. We thank Professor Winnie W.S. MAK and Ms. Sherry Xue YANG for assistance with statistical analysis.
Footnotes
Conflict of interests: There is no conflict of interests of all authors.
References
- 1.Zhou Y, Li D, Lu D, Ruan Y, Qi X, Gao G. Prevalence of HIV and syphilis infection among men who have sex with men in China: a meta-analysis. Biomed Res Int. 2014;2014:620431. doi: 10.1155/2014/620431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y, Chen P, Lu R, et al. Prevalence of HIV among men who have sex with men in Chongqing, China, 2006–2009: cross-sectional biological and behavioural surveys. Sex Transm Infect. 2012;88:444–450. doi: 10.1136/sextrans-2011-050295. [DOI] [PubMed] [Google Scholar]
- 3.Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among Black men with HIV. Cultur Divers Ethnic Minor Psychol. 2011;17:295–302. doi: 10.1037/a0024056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comulada WS, Rotheram-Borus MJ, Pequegnat W, et al. Relationships over time between mental health symptoms and transmission risk among persons living with HIV. Psychol Addict Behav. 2010;24:109–118. doi: 10.1037/a0018190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mills TC, Paul J, Stall R, et al. Distress and depression in men who have sex with men: the Urban Men's Health Study. Am J Psychiatry. 2004;161:278–285. doi: 10.1176/appi.ajp.161.2.278. [DOI] [PubMed] [Google Scholar]
- 6.Sivasubramanian M, Mimiaga MJ, Mayer KH, et al. Suicidality, clinical depression, and anxiety disorders are highly prevalent in men who have sex with men in Mumbai, India: findings from a community-recruited sample. Psychol Health Med. 2011;16:450–462. doi: 10.1080/13548506.2011.554645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H, Zhang C, Ruan Y, Li X, Fennie K, Williams AB. Depressive Symptoms and Social Support among People Living With HIV in Hunan, China. J Assoc Nurses AIDS Care. 2014 doi: 10.1016/j.jana.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Cook JA, Cohen MH, Burke J, et al. Effects of depressive symptoms and mental health quality of life on use of highly active antiretroviral therapy among HIV- seropositive women. J Acquir Immune Defic Syndr. 2002;30:401–409. doi: 10.1097/00042560-200208010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Lyketsos CG, Hoover DR, Guccione M, et al. Changes in depressive symptoms as AIDS develops. The Multicenter AIDS Cohort Study. Am J Psychiatry. 1996;153:1430–1437. doi: 10.1176/ajp.153.11.1430. [DOI] [PubMed] [Google Scholar]
- 10.Perry S, Fishman B. Depression and HIV. How does one affect the other? JAMA. 1993;270:2609–2610. [PubMed] [Google Scholar]
- 11.Schuster R, Bornovalova M, Hunt E. The influence of depression on the progression of HIV: direct and indirect effects. Behav Modif. 2012;36:123–145. doi: 10.1177/0145445511425231. [DOI] [PubMed] [Google Scholar]
- 12.Parsons JT, Halkitis PN, Wolitski RJ, Gomez CA. Correlates of sexual risk behaviors among HIV-positive men who have sex with men. AIDS Educ Prev. 2003;15:383–400. doi: 10.1521/aeap.15.6.383.24043. [DOI] [PubMed] [Google Scholar]
- 13.Sun YH, Sun L, Wu HY, et al. Loneliness, social support and family function of people living with HIV/AIDS in Anhui rural area, China. Int J STD AIDS. 2009;20:255–258. doi: 10.1258/ijsa.2008.008348. [DOI] [PubMed] [Google Scholar]
- 14.Tao X, Gai R, Zhang N, et al. HIV infection and mental health of "money boys": a pilot study in Shandong Province, China. Southeast Asian. J Trop Med Public Health. 2010;41:358–368. [PubMed] [Google Scholar]
- 15.Zhao Q, Li X, Kaljee LM, Fang X, Stanton B, Zhang L. AIDS orphanages in China: reality and challenges. AIDS Patient Care STDS. 2009;23:297–303. doi: 10.1089/apc.2008.0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Prevention and treatment of HIV and other sexually transmitted infections among men who have sex with men and transgender people: recommendations for a public health approach. 2011 [PubMed] [Google Scholar]
- 17.Chen G, Li Y, Zhang B, Yu Z, Li X, Wang L. Psychological characteristics in high-risk MSM in China. BMC Public Health. 2012;12:58. doi: 10.1186/1471-2458-12-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feng Y, Wu Z, Detels R. Evolution of men who have sex with men community and experienced stigma among men who have sex with men in Chengdu, China. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S98–103. doi: 10.1097/QAI.0b013e3181c7df71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao G, Li X, Zhao J, Zhang L, Stanton B. Relative importance of various measures of HIV-related stigma in predicting psychological outcomes among children affected by HIV. Community Ment Health J. 2012;48:275–283. doi: 10.1007/s10597-011-9424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology: Science & Practice. 2002;9:35–53. [Google Scholar]
- 22.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17:1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11:353–363. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- 24.Kaleeba N, Kalibala S, Kaseje M, et al. Participatory evaluation of counselling, medical and social services of The AIDS Support Organization (TASO) in Uganda. AIDS Care. 1997;9:13–26. doi: 10.1080/09540129750125307. [DOI] [PubMed] [Google Scholar]
- 25.Cohen S, Mckay G. Social support, stress, and the buffering hypothesis: A theoretical analysis. In: Baum A, Singer JE, Taylor SE, editors. Handbook of Psychology and Health. Hillsdale: Erlbaum; 1984. pp. 253–267. [Google Scholar]
- 26.Arriola KJ, Spaulding AC, Booker CA, et al. Understanding the Relationship between Social Support and Physical and Mental Well-Being among Jail Detainees Living with HIV. J Health Psychol. 2013 doi: 10.1177/1359105313496447. [DOI] [PubMed] [Google Scholar]
- 27.Liu L, Pang R, Sun W, et al. Functional social support, psychological capital, and depressive and anxiety symptoms among people living with HIV/AIDS employed full-time. BMC Psychiatry. 2013;13:324. doi: 10.1186/1471-244X-13-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 29.Mo PK, Coulson NS. Developing a model for online support group use, empowering processes and psychosocial outcomes for individuals living with HIV/AIDS. Psychol Health. 2012;27:445–459. doi: 10.1080/08870446.2011.592981. [DOI] [PubMed] [Google Scholar]
- 30.Galvan FH, Davis EM, Banks D, Bing EG. HIV stigma and social support among African Americans. AIDS Patient Care STDS. 2008;22:423–436. doi: 10.1089/apc.2007.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mak WW, Cheung RY, Law RW, Woo J, Li PC, Chung RW. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc Sci Med. 2007;64:1549–1559. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 32.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64:1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one's HIV-positive status, stigma and social support. AIDS Care. 2008;20:1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 34.Davison KP, Pennebaker JW, Dickerson SS. Who talks? The social psychology of illness support groups. Am Psychol. 2000;55:205–217. [PubMed] [Google Scholar]
- 35.Liu H, Feng T, Ha T, et al. Chinese Culture, Homosexuality Stigma, Social Support and Condom Use: A Path Analytic Model. Stigma Res Action. 2011;1:27–35. doi: 10.5463/sra.v1i1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zang C, Guida J, Sun Y, Liu H. Collectivism culture, HIV stigma and social network support in Anhui, China: a path analytic model. AIDS Patient Care STDS. 2014;28:452–458. doi: 10.1089/apc.2014.0015. [DOI] [PubMed] [Google Scholar]
- 37.Romens SE, Pollak SD. Emotion regulation predicts attention bias in maltreated children at-risk for depression. J Child Psychol Psychiatry. 2012;53:120–127. doi: 10.1111/j.1469-7610.2011.02474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soenke M, Hahn KS, Tull MT, Gratz KL. Exploring the relationship between childhood abuse and analogue generalized anxiety disorder: the mediating role of emotion dysregulation. Development and Psychopathology. 2010;34:401–412. [Google Scholar]
- 39.Watson D. Positive affectivity: the disposition to experience pleasurable emotional states. In: Snyder CR, Lopez SJ, editors. Handbook of positive psychology. New York, NY: Oxford university press; 2002. pp. 106–119. [Google Scholar]
- 40.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 41.Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 42.Ironson G, Balbin E, Stuetzle R, et al. Dispositional optimism and the mechanisms by which it predicts slower disease progression in HIV: proactive behavior, avoidant coping, and depression. Int J Behav Med. 2005;12:86–97. doi: 10.1207/s15327558ijbm1202_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ironson G, Hayward H. Do positive psychosocial factors predict disease progression in HIV-1? A review of the evidence. Psychosom Med. 2008;70:546–554. doi: 10.1097/PSY.0b013e318177216c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moskowitz JT. Positive affect predicts lower risk of AIDS mortality. Psychosom Med. 2003;65:620–626. doi: 10.1097/01.psy.0000073873.74829.23. [DOI] [PubMed] [Google Scholar]
- 45.Harding KA, Hudson MR, Mezulis A. Cognitive mechanisms linking low trait positive affect to depressive symptoms: A prospective diary study. Cogn Emot. 2014 doi: 10.1080/02699931.2014.889661. [DOI] [PubMed] [Google Scholar]
- 46.Nima AA, Rosenberg P, Archer T, Garcia D. Anxiety, affect, self-esteem, and stress: mediation and moderation effects on depression. PLoS One. 2013;8:e73265. doi: 10.1371/journal.pone.0073265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Emmons RA, McCullough ME. Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology. 2003;84:377–389. doi: 10.1037//0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- 48.Deichert NT, Fekete EM, Boarts JM, Druley JA, Delahanty DL. Emotional support and affect: associations with health behaviors and active coping efforts in men living with HIV. AIDS Behav. 2008;12:139–145. doi: 10.1007/s10461-007-9214-y. [DOI] [PubMed] [Google Scholar]
- 49.Gonzalez JS, Penedo FJ, Antoni MH, et al. Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychol. 2004;23:413–418. doi: 10.1037/0278-6133.23.4.413. [DOI] [PubMed] [Google Scholar]
- 50.Cohen S, Syme SL. Issues in the study and application of social support. In: Cohen S, Syme SL, editors. Social support and health. Orlando, FL: Academic Press; 1985. pp. 3–22. [Google Scholar]
- 51.Burgess D, Widome R, Ryan Mv, Phelan S, Fu S. Self-stigma, stress, and smoking among african american and american indian female smokers: an exploratory qualitative Study. Journal of Health Disparities Research and Practice. 2011;5:20–31. [Google Scholar]
- 52.Henderson M, Brooks SK, Del Busso L, et al. Shame! Self-stigmatisation as an obstacle to sick doctors returning to work: a qualitative study. BMJ Open. 2012:2. doi: 10.1136/bmjopen-2012-001776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu YL, Yang HY, Wang J, et al. Prevalence of suicidal ideation and associated factors among HIV-positive MSM in Anhui, China. Int J STD AIDS. 2014 doi: 10.1177/0956462414544722. [DOI] [PubMed] [Google Scholar]
- 54.Kahler CW, Wray TB, Pantalone DW, et al. Daily Associations Between Alcohol Use and Unprotected Anal Sex Among Heavy Drinking HIV-Positive Men Who Have Sex with Men. AIDS Behav. 2014 doi: 10.1007/s10461-014-0896-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chengdu Tongle Health Counseling Service Center. Study of MSM Population Size in Chengdu,Global Fund HIV/AIDS Project, China. 4. 2007. [Google Scholar]
- 56.Feng Y, Wu Z, Detels R, et al. HIV/STD prevalence among men who have sex with men in Chengdu, China and associated risk factors for HIV infection. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S74–80. doi: 10.1097/QAI.0b013e3181c7dd16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mak WW, Cheung RY. Self-stigma among concealable minorities in Hong Kong: conceptualization and unified measurement. Am J Orthopsychiatry. 2010;80:267–281. doi: 10.1111/j.1939-0025.2010.01030.x. [DOI] [PubMed] [Google Scholar]
- 58.Watson D, Clark LA. Measurement and mismeasurement of mood: recurrent and emergent issues. J Pers Assess. 1997;68:267–296. doi: 10.1207/s15327752jpa6802_4. [DOI] [PubMed] [Google Scholar]
- 59.Huang L, Yang T, Ji Z. Applicability of the Positive and Negative Affect Scale in Chinese. Chinese Mental Health Journal. 2003;17:54–56. [Google Scholar]
- 60.Cheung C-K, Bagley C. Validating an American Scale in Hong Kong: The Center for Epidemiological Studies Depression Scale (CES-D) The Journal of Psychology. 1998;132:169–186. doi: 10.1080/00223989809599157. [DOI] [PubMed] [Google Scholar]
- 61.Chi I, Boey KW. Hong Kong Validation of Measuring Instruments of Mental Health Status of the Elderly. Clinical Gerontologist: The Journal of Aging and Mental Health. 1993;13:35–51. [Google Scholar]
- 62.Song Y, Huang Y, Liu D, et al. Depression in college: depressive symptoms and personality factors in Beijing and Hong Kong college freshmen. Comprehensive Psychiatry. 2008;49:496–502. doi: 10.1016/j.comppsych.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 63.Chishinga N, Kinyanda E, Weiss HA, Patel V, Ayles H, Seedat S. Validation of brief screening tools for depressive and alcohol use disorders among TB and HIV patients in primary care in Zambia. BMC Psychiatry. 2011;11:75. doi: 10.1186/1471-244X-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farley J, Miller E, Zamani A, et al. Screening for hazardous alcohol use and depressive symptomatology among HIV-infected patients in Nigeria: prevalence, predictors, and association with adherence. J Int Assoc Physicians AIDS Care (Chic) 2010;9:218–226. doi: 10.1177/1545109710371133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hudson A, Kirksey K, Holzemer W. The influence of symptoms on quality of life among HIV-infected women. West J Nurs Res. 2004;26:9–23. doi: 10.1177/0193945903259221. discussion 24–30. [DOI] [PubMed] [Google Scholar]
- 66.Richardson J, Barkan S, Cohen M, et al. Experience and covariates of depressive symptoms among a cohort of HIV infected women. Soc Work Health Care. 2001;32:93–111. doi: 10.1300/J010v32n04_05. [DOI] [PubMed] [Google Scholar]
- 67.Alvy LM, McKirnan DJ, Mansergh G, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2011;15:1171–1179. doi: 10.1007/s10461-010-9678-z. [DOI] [PubMed] [Google Scholar]
- 68.Berg CJ, Nehl EJ, Wong FY, et al. Prevalence and correlates of tobacco use among a sample of MSM in Shanghai, China. Nicotine Tob Res. 2011;13:22–28. doi: 10.1093/ntr/ntq193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tucker A, Liht J, de Swardt G, et al. Homophobic stigma, depression, self-efficacy and unprotected anal intercourse for peri-urban township men who have sex with men in Cape Town, South Africa: a cross-sectional association model. AIDS Care. 2014;26:882–889. doi: 10.1080/09540121.2013.859652. [DOI] [PubMed] [Google Scholar]
- 70.Kline RB. Principles and practice of structural equation modeling. New York: Guilford; 2005. [Google Scholar]
- 71.Garson GD. Structural Equation Modeling: 2015 Edition (Statistical Associates "Blue Book" Series Book 14) Statistical Associates Publishers; 2015. [Google Scholar]
- 72.Carmines EG, McIver JP. Analyzing models with unobserved variables. In: Bohrnstedt GM, Borgatta EF, editors. Social measurement: Current issues. Beverly Hills: Sage; 1981. pp. 63–115. [Google Scholar]
- 73.Hoyle RH, Panter AT. Writing about structural equation models. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks, CA: Sage; 1995. pp. 158–176. [Google Scholar]
- 74.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- 75.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- 77.Jin C, Zhao G, Zhang F, Feng L, Wu N. The psychological status of HIV-positive people and their psychosocial experiences in eastern China. HIV Med. 2010;11:253–259. doi: 10.1111/j.1468-1293.2009.00770.x. [DOI] [PubMed] [Google Scholar]
- 78.Herek GM. AIDS and stigma. American Behavioral Scientist. 1999;42:1106–1116. [Google Scholar]
- 79.Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. J Assoc Nurses AIDS Care. 2010;21:144–152. doi: 10.1016/j.jana.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gielen AC, O'Campo P, Faden RR, Eke A. Women's disclosure of HIV status: experiences of mistreatment and violence in an urban setting. Women Health. 1997;25:19–31. doi: 10.1300/J013v25n03_02. [DOI] [PubMed] [Google Scholar]
- 81.Schroevers M, Sanderman R, van Sonderen E, Ranchor A. The evaluation of the Center for Epidemiologic Studies Depression (CES-D) scale: Depressed and Positive Affect in cancer patients and healthy reference subjects. Quality of Life Research. 2000;9:1015–1029. doi: 10.1023/a:1016673003237. [DOI] [PubMed] [Google Scholar]
- 82.Cully JA, Mignogna J, Stanley MA, et al. Development and pilot testing of a standardized training program for a patient-mentoring intervention to increase adherence to outpatient HIV care. AIDS Patient Care STDS. 2012;26:165–172. doi: 10.1089/apc.2011.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65:467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 84.Moskowitz JT, Hult JR, Duncan LG, et al. A positive affect intervention for people experiencing health-related stress: development and non-randomized pilot test. J Health Psychol. 2012;17:676–692. doi: 10.1177/1359105311425275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gu J, Lau JT, Chen H, Chen X, Liu C, Liu J. Mental health and interpersonal factors associated with HIV-related risk behaviors among non-institutionalized female injection drug users who are also sex workers in China. Women Health. 2010;50:20–36. doi: 10.1080/03630241003601137. [DOI] [PubMed] [Google Scholar]
- 86.Li J, Gu J, Lau JT, Chen H, Mo PK, Tang M. Prevalence of depressive symptoms and associated factors among people who inject drugs in China. Drug Alcohol Depend. 2015;151:228–235. doi: 10.1016/j.drugalcdep.2015.03.028. [DOI] [PubMed] [Google Scholar]