Abstract
The study aimed to investigate whether heart-type fatty acid binding protein (H-FABP) measurement provides additional diagnostic value to that of conventional cardiac markers in acute myocardial infarction (AMI) within first 6 h after the onset of symptoms. The study included 120 subjects: 60 AMI cases and 60 age and sex matched controls. The cases and controls were further divided into 2 subgroups depending on the time since onset of chest pain as (1) subjects within 3 h and (2) between 3 and 6 h of onset of chest pain. In all the cases and controls, serum H-FABP concentration was measured by Immunoturbidimetric method, serum Troponin I and myoglobin concentrations by Chemiluminescence immunoassay and serum CK-MB concentration by Immuno-inhibition method. The sensitivity, specificity, positive and negative predictive values of H-FABP were significantly greater than CK-MB and myoglobin but were lesser than Troponin I in patients with suspected AMI in both within 3 h and 3–6 h groups. Receiver operating characteristic curves demonstrated greatest diagnostic ability for Troponin I (AUC = 0.99, p < 0.001) followed by H-FABP (AUC = 0.906, p < 0.001) within 3 h and 3–6 h after the onset of chest pain. In conclusion, the diagnostic value of H-FABP is greater than CK-MB and myoglobin but slightly lesser than troponin I for the early diagnosis of AMI within first 6 h of chest pain. H-FABP can be used as an additional diagnostic tool for the early diagnosis of AMI along with troponin I.
Keywords: Myocardial infarction; Heart-type fatty acid binding protein, human; Troponin-I; Myoglobin; Creatine kinase, MB; Immunoturbidimetric method; ROC analysis
Introduction
Acute coronary syndrome (ACS) is a group of heart conditions caused by insufficient blood supply to the heart. ACS includes acute myocardial infarction (AMI), when blood flow to part of the heart is blocked for long enough that part of the heart muscle is damaged or dies [1]. AMI is one of the leading causes of death in India and worldwide. AMI prevalence rates range from 1.6 to 7.4 % in rural populations and 1 to 13.2 % in urban populations in India [2].
The early diagnosis and treatment is of utmost importance to prevent the mortality and related long term complications. If AMI is diagnosed and treated within 1 h (so called golden hour), mortality can be reduced from 9 to 3 %, and if the treatment is delayed for 3–4 h, mortality could be 5 times higher. Unfortunately, at least one-fifth of the cases of AMI go unrecognized either because of the atypical presentation or atypical ECG changes or delay in the rise of the serum cardiac markers [3].
Currently used biochemical markers such as cardiac troponins, CK-MB or myoglobin are limited by either the lack of specificity or delay in their elevation in the blood by several hours after the onset of symptoms. Therefore their use in the diagnosis of AMI in the early hours (within 6 h) is limited [4]. Among the novel biochemical markers of AMI, heart-type fatty acid binding protein (H-FABP) is of particular interest. H-FABP is a small 15 kDa soluble protein composed of 132 amino acids. It is one of the most abundant proteins in the heart comprising 5–15 % of the total cytosolic protein pool. H-FABP is not totally cardiac specific, occurs in other tissues at much lower concentrations. It is involved in intracellular transportation of fatty acids for oxidation in the mitochondria. Several studies have shown that H-FABP is a sensitive marker for the diagnosis of AMI and might be more sensitive than conventional cardiac markers when measured soon after the onset of symptoms. However, there is still considerable uncertainty regarding the role of H-FABP in the early diagnosis of AMI. Use of H-FABP is restricted to the clinical research because of lack of fast and easy to use method for its measurement. However, a novel automated immuno-turbidimetric H-FABP assay has recently been developed [5].
Aim of this study was to assess whether H-FABP measurement provides additional diagnostic value to that of conventional cardiac markers in AMI. Objective of the study was to compare the sensitivity, specificity, positive predictive value, negative predictive value and diagnostic ability of H-FABP with the conventional cardiac biomarkers (CK-MB, Troponin I and Myoglobin) in patients presenting with chest pain within 3 h and 3–6 h after the onset of chest pain.
Materials and Methods
The study was carried out on 120 subjects: 60 MI patients and 60 non-cardiac chest pain but otherwise healthy controls. Patients were selected from ICCU, BLDEU’s Shri B M Patil Medical College, Hospital and Research Centre, Vijayapur, during the period from May 2013 to June 2014. The study was approved by the Institutional Ethical Clearance Committee and written informed consent was obtained from all the subjects. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patients presenting with acute chest pain less than 6 h duration suspected of AMI were enrolled consecutively in the study. Full clinical history including personal information, presenting symptoms, past medical history such as diabetes mellitus, hypertension, previous ischemic event etc., and general clinical examination findings, ECG findings, Echocardiography and laboratory investigations were documented using a predefined protocol. Standard diagnosis of either AMI or non-cardiac chest pain was made after critical review of all the above information by a cardiologist. Diagnosis of AMI was done according to the WHO criteria. The cases and controls were further divided into two subgroups depending on the time since the onset of chest pain as the subjects within 3 h of onset of chest pain and those between 3 and 6 h of onset of chest pain. Patients arriving to hospital after 6 h of onset of chest pain, those with chronic muscle disease, renal disease, recent surgery, those receiving direct current shocks and who underwent percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass graft (CABG) procedures within 30 days were excluded from the study.
From all the cases and controls, 5 mL of venous blood sample was drawn using all the aseptic precautions, serum was separated and kept at −20 °C until the analysis was done. Serum H-FABP levels were measured by automated immuno-turbidimetric method [6–8] (Reagent kit from Randox Laboratories Limited, County Antrim, United Kingdom) on Roche cobas c 311 fully automated Biochemistry analyzer (Roche Diagnostic Limited, Rotkreuz, Switzerland). The method is based on the principle that, sample is reacted with a buffer and anti-H-FABP coated latex. The formation of antigen–antibody complex during the reaction results in an increase in turbidity, the extent of which is measured as the amount of light absorbed at 700 nm. By constructing a standard curve from the absorbance of the standards, H-FABP concentration in the sample can be determined. Serum troponin-I [9] and myoglobin [10] levels were measured by chemiluminescence immunoassay on Abbott Architect c4000 analyzer (Abbott Laboratories, Illinois, USA) and serum CK-MB by Immuno-inhibition method [11, 12] using Stat Fax 3300 Biochemistry analyzer (Awareness Technology Inc., Florida, USA).
The cut off levels and coefficients of variation (CV) of H-FABP, troponin-I, myoglobin and CK-MB used for the diagnosis of AMI in this study were >6.32 ng/mL (at 99th percentile, CV = 7.94 %), >0.032 µg/L in males and >0.022 µg/L in females (at 99th percentile, CV = 10 %), >106 ng/mL in males and >155 ng/mL in females (at 99th percentile, CV = 7.94 %) and 24 IU/L respectively. These values are according to the recommendations of the reagent kit manufacturers.
Statistical Analysis
Continuous variables are presented as mean ± standard deviation (SD) values and categorical data are presented as percent frequency of occurrence. Differences between means of two groups were assessed with the unpaired Student t test. Sensitivity, Specificity, positive and negative predictive values (PPV and NPV) were calculated and receiver operating characteristic (ROC) curve analysis was done to assess the diagnostic validity for each marker at each time interval. For all the tests, p value of 0.05 or less was considered for statistical significance. All the statistical procedures were performed using the Statistical Package for the Social Sciences statistical software (SPSS) version 16 for Windows.
Results
A total of 120 patients were included in this study. Of these 60 were AMI cases and 60 were non-cardiac chest pain otherwise healthy controls. Of 60 AMI cases 44 were males and 16 females and of 60 controls 38 were males and 22 females. The average age for the AMI cases was 60.7 years and that in controls was 54.82 years.
The baseline clinical characteristics are depicted in Table 1. Patients diagnosed with AMI tended to be older than non-cardiac chest pain controls. AMI was more common among males when compared to females. The other demographics such as incidence of smoking, alcohol intake, hypertension, diabetes mellitus, hyperlipidemia, H/o previous IHD was more common in AMI cases when compared to controls. Among the ECG changes, ST elevation was seen among 85 % of AMI cases, T wave inversion in 20 % and other changes in 8.3 % of the AMI cases.
Table 1.
Baseline characteristics of study participants
| Clinical characteristic | AMI cases (n = 60) | Controls (n = 60) |
|---|---|---|
| Age (years) (mean ± SD) | 60.7 ± 12.2 | 54.82 ± 14.4 |
| Males | 44 (73.3 %) | 38 (63.3 %) |
| Females | 16 (26.7 %) | 22 (36.7 %) |
| Smoking | 18 (30 %) | 16 (26.7 %) |
| Alcohol intake | 16 (26.7 %) | 16 (26.7 %) |
| Hypertension | 25 (41.7 %) | 15 (25 %) |
| Diabetes mellitus | 19 (31.7 %) | 15 (25 %) |
| Hyperlipidemia | 09 (15 %) | 05 (8.3 %) |
| H/o previous IHD | 03 (5 %) | 00 |
| ECG changes | ||
| ST elevation | 51 (85 %) | – |
| T-wave inversion | 12 (20 %) | 05 (8.3 %) |
| Other changes (ST depression/tall T waves/Q wave) | 05 (8.3 %) | 03 (5 %) |
Values are given as ‘n’ (%), unless otherwise specified
IHD ischemic heart disease
Table 2 shows the mean ± SD values of four cardiac biomarkers in AMI cases and non-AMI controls. The mean levels of CK-MB, troponin I, myoglobin and H-FABP were significantly higher in AMI cases when compared to that of controls in both 0–3 and 3–6 h groups. The difference between cases and controls was statistically significant in both the time intervals (p < 0.01).
Table 2.
Mean levels of four cardiac biomarkers in AMI cases and controls
| AMI cases (n = 60) (Mean ± SD) |
Controls (n = 60) (Mean ± SD) |
P 1 value | P 2 value | |||
|---|---|---|---|---|---|---|
| 0–3 h (n = 26) |
3–6 h (n = 34) |
0–3 h (n = 26) |
3–6 h (n = 34) |
|||
| CK-MB (IU/L) |
26.2 ± 19.2 | 36.9 ± 48.9 | 18.6 ± 9.5 | 25 ± 10.1 | <0.01 | <0.01 |
| Troponin I (µg/L) |
5.9 ± 16.2 | 8.5 ± 16.9 | 0.0048 ± 0.0077 | 0.0087 ± 0.0079 | <0.01 | <0.01 |
| Myoglobin (ng/mL) |
364.9 ± 363.9 | 584.5 ± 393.9 | 55.7 ± 53.4 | 90.8 ± 74.2 | <0.01 | <0.01 |
| H-FABP (ng/mL) |
40.4 ± 56.3 | 76.3 ± 56.1 | 4.7 ± 7.3 | 6.7 ± 8.6 | <0.01 | <0.01 |
P 1 = AMI cases (0–3 h group) versus controls (0–3 h group)
P 2 = AMI cases (3–6 h group) versus controls (3–6 h group)
Table 3 shows the sensitivity, specificity, PPV and NPV of all the four cardiac biomarkers. As it is evident from the table that, the sensitivity, specificity, PPV and NPV of H-FABP were significantly higher than that of CK-MB and myoglobin and slightly lesser than that of troponin I in both 0–3 h and 3–6 h groups.
Table 3.
Diagnostic performances of four cardiac biomarkers for the early diagnosis of AMI within 3 h and 3–6 h after the onset of chest pain
| Sensitivity | Specificity | PPV | NPV | |||||
|---|---|---|---|---|---|---|---|---|
| 0–3 h | 3–6 h | 0–3 h | 3–6 h | 0–3 h | 3–6 h | 0–3 h | 3–6 h | |
| CK-MB (IU/L) |
23.1 | 52.9 | 61.5 | 58.8 | 37.5 | 56.3 | 44.5 | 55.6 |
| Troponin I (µg/L) |
96.2 | 100 | 100 | 100 | 100 | 100 | 96.3 | 100 |
| Myoglobin (ng/mL) |
73.1 | 88.2 | 76.9 | 70.6 | 76.0 | 75.0 | 74.1 | 85.7 |
| H-FABP (ng/mL) |
92.3 | 94.1 | 88.5 | 79.4 | 88.9 | 82.1 | 92.0 | 93.1 |
PPV positive predictive value, NPV negative predictive value
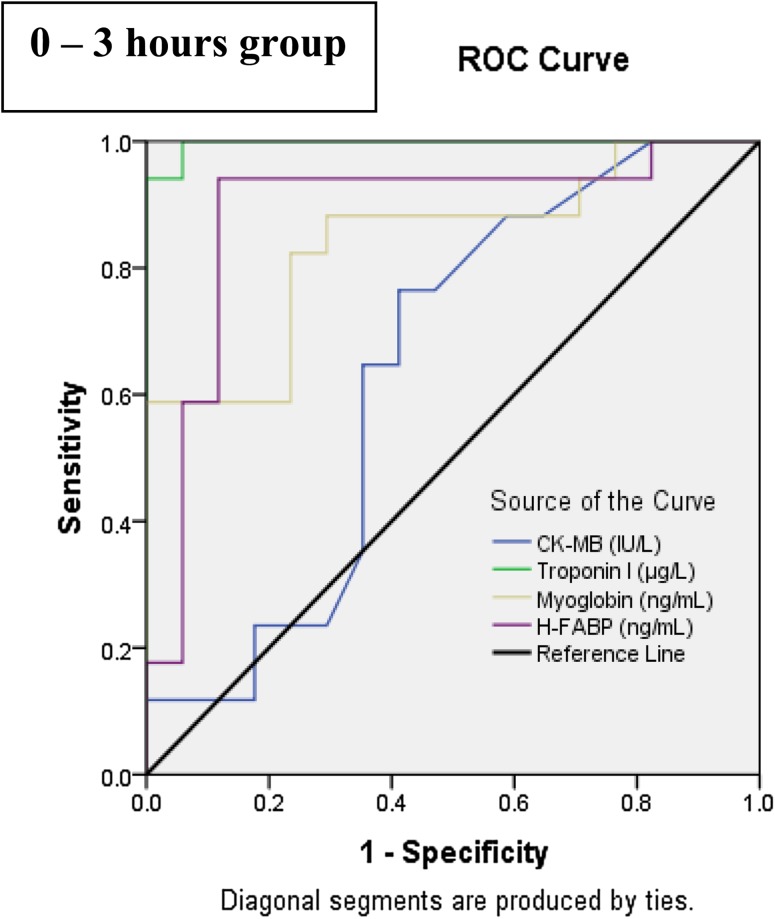
Within 3 h after the onset of chest pain, ROC curve analysis of CK-MB, Troponin I, Myoglobin and H-FABP shows that, troponin I has highest diagnostic accuracy (AUC = 0.997) followed by H-FABP (AUC = 0.886), myoglobin (AUC = 0.841) and CK-MB (AUC = 0.64) (Fig. 1).
Fig. 1.
ROC curve analysis of CK-MB, Troponin I, Myoglobin and H-FABP in 0–3 h group
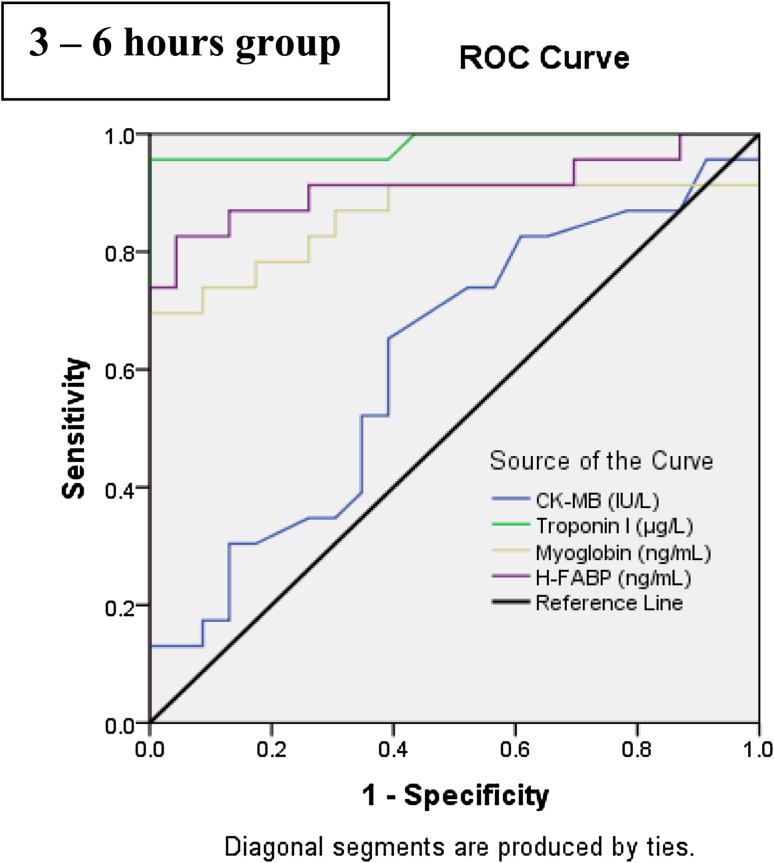
Between 3 and 6 h after the onset of chest pain, ROC curve analysis of CK-MB, Troponin I, Myoglobin and H-FABP shows that, troponin I has highest diagnostic accuracy (AUC = 0.982) followed by H-FABP (AUC = 0.911), myoglobin (AUC = 0.86) and CK-MB (AUC = 0.616) (Fig. 2).
Fig. 2.
ROC curve analysis of CK-MB, Troponin I, Myoglobin and H-FABP in 3–6 h group
Discussion
In our study, serum concentrations of HFABP, troponin-I, myoglobin and CK-MB were significantly higher in AMI cases when compared to controls both in 0–3 h and 3–6 h groups. These findings are in full agreement with the study conducted by Elmadbouh et al. [3]. Pasaoglu et al. [13] showed that, in blood samples collected at 1–2 and 3 h, H-FABP and myoglobin in the AMI group were significantly higher (p = 0.00) than in non-AMI and control groups. Troponin-I and CK-MB in the AMI group were not yet significantly higher than in non-AMI and control groups at 1–2 h. Troponin-I in the AMI group was higher than in the non-AMI and control groups at 3 h. CK-MB in the AMI group was higher than in the control group, but not in the non-AMI group at 3 h. All parameters in the AMI group were significantly higher than in the non-AMI and control groups at 6 h [13]. Orak et al. [14] found that, there was a significant difference in the mean levels of H-FABP and CK-MB in ACS cases when compared to the controls (p = 0.000), whereas no difference was observed for troponin-I (p = 0.013) within 6 h [14].
In our study, H-FABP demonstrated greater sensitivity, specificity, PPV and NPV than CK-MB and myoglobin in patients with suspected AMI both within 3 h and 3–6 h after the onset of chest pain. The diagnostic validity of H-FABP was comparable to troponin-I but never superior both within 3 h and 3–6 h after the onset of chest pain.
Several studies have compared the diagnostic value of H-FABP with CK-MB, myoglobin and troponin-I in patients with chest pain and arrived at conflicting conclusions. In their study, Elmadbouh et al. [3] found that within 3 h, H-FABP had diagnostic sensitivity (81.8 %) equal to that of CK-MB and troponin-I but superior to that of myoglobin (72.7 %). However, H-FABP had higher specificity (88.2 %) equal to that of myoglobin but superior to that of CK-MB and troponin-I. This trend extends to within 6 h as well [3]. Pasaoglu et al. [13] demonstrated that for AMI detection, serum H-FABP shows significantly higher diagnostic sensitivity and specificity than troponin-I and CK-MB, similar to myoglobin, especially soon after (within 1–2 and 3 h) the onset of symptoms [13]. In another study, Orak et al. [14] showed that, for patients admitted with chest pain, H-FABP is more sensitive and specific than troponin-I and CK-MB in the early diagnosis of ACS. In patients with ACS who were admitted within 0–3 h, the H-FABP sensitivity was 100 % and specificity was 75 %; for CK-MB, the sensitivity was 81 % and the specificity was 16 %; and for troponin-I, the sensitivity was 100 % and the specificity was 20 %. In patients with ACS who were admitted within 3–6 h, the H-FABP sensitivity was 97 % and specificity was 68 %; for CK-MB, the sensitivity was 90 % and specificity was 80 %; and for troponin-I, the sensitivity was 75 % and specificity was 21 % [14]. Alhadi et al. [5] conducted a study in 100 consecutive patients admitted with acute chest pain suggestive of ACS and found that, H-FABP peak concentration occurred at 8 h after symptoms onset and was the most sensitive early marker with 79.9 and 98 % sensitivity at presentation and 2 h after presentation respectively. The sensitivity of all other markers namely CK-MB, troponin-I and myoglobin at presentation was less than 62 % [15]. McMahon et al. [4] concluded that, of the four biomarkers measured in this study, H-FABP demonstrated highest sensitivity at the early time points (64.3 % at 0–3 h and 85.3 % at 3–6 h) [4].
In contrast, Alansari and Croal [16] suggested that H-FABP and myoglobin provide little clinical value compared to troponin-I, when measured at presentation in patients presenting with chest pain (3–12 h) [16]. In a multicentre study conducted by Freund et al. [17], H-FABP had no additional value over cardiac troponin-I for the diagnosis of myocardial necrosis (STEMI and NSTEMI) in ED patients with chest pain of less than 6 h duration [17].
We examined the diagnostic ability of each cardiac marker for 0–3 and 3–6 h groups by ROC curve analysis. In both 0–3 and 3–6 h groups, troponin I had the highest area under curve value followed by H-FABP, myoglobin and CK-MB. The AUC values of these markers were statistically significant except for CK-MB. This finding is in full agreement with the studies conducted by Freund et al. [17] and Kim et al. [18]. However McMahon et al. and Orak et al. showed that, AUC for H-FABP was highest of all markers at 0–6 h after chest pain followed by CK-MB, troponin I and myoglobin [4] (Tables 4, 5).
Table 4.
Area under ROC curve for cardiac markers in 0–3 h group
| AUC | p value | CI | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| CK-MB | 0.640 | 0.163 | 0.446 | 0.834 |
| Troponin I | 0.997 | 0.000 | 0.985 | 1.008 |
| Myoglobin | 0.841 | 0.001 | 0.705 | 0.977 |
| H-FABP | 0.886 | 0.000 | 0.756 | 1.015 |
AUC area under curve
Table 5.
Area under ROC curve for cardiac markers in 3–6 h group
| AUC | p value | CI | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| CK-MB | 0.616 | 0.177 | 0.452 | 0.781 |
| Troponin I | 0.982 | 0.000 | 0.946 | 1.019 |
| Myoglobin | 0.86 | 0.000 | 0.738 | 0.983 |
| H-FABP | 0.911 | 0.000 | 0.816 | 1.007 |
AUC area under curve
Superior performance of the H-FABP over CK-MB and myoglobin may be because of the following reasons: (1) H-FABP has small molecular weight (15 kDa) when compared to CK-MB (80 kDa) and myoglobin (18 kDa). (2) Relative specificity of the H-FABP for the cardiac tissue. Its concentration within the myocardial tissue is 10 times higher when compared to that of skeletal muscle. However, CK-MB and myoglobin are less specific for cardiac tissue; concentration of myoglobin is approximately twofold lower in cardiac than skeletal muscle. (3) H-FABP appears in the plasma early (within 2 h) with a peak at 6 h after the cardiac damage. However CK-MB begins to increase in the blood between 3 and 6 h after the onset of infarction and peaking at 16–20 h [5].
Several studies [3, 4, 13–15] found that the diagnostic value of H-FABP was greater than troponin-I particularly within 3 h after the onset of symptoms of AMI. Some other studies [16–18] showed H-FABP does not provide additional useful information to troponin-I. Reasons for the conflicting results can be the duration of MI at the time of sampling, different study settings (cardiology units, Emergency department or pre-hospital etc.), different methods and cut off values for the H-FABP used.
Limitations
We are aware that our study presents few limitations. First, sample size is small. Second, we could not do the serial measurements of the cardiac markers for the assessment of their kinetics.
Conclusion
Diagnostic value of H-FABP is much better than CK-MB and myoglobin but lesser than troponin I for the early diagnosis of myocardial infarction within 6 h of chest pain. When used as a lone marker H-FABP has no additional diagnostic value than the troponin I which is considered as the single best cardiac marker currently. H-FABP deserves further investigation as it may have a role along with troponin I in multimarker approach for the early diagnosis of AMI.
Acknowledgments
We would like to thank BLDE University, Vijayapur, Karnataka for the research grant towards this study. We thank the staff of the Department of Medicine and Department of Biochemistry, BLDEU’s Shri B M Patil Medical College, Hospital and Research Centre, Vijayapur for Their constant support and motivation for the collection of cases and carrying out investigations. Special thanks to Dr Kusal K Das, Professor, Department of Physiology, BLDEU’s Shri B M Patil Medical College, for valuable suggestions and inspiration. We also thank all the study subjects who took part in this study.
Funding
This study was funded by BLDE University, Vijayapur, 586103, Karnataka, India.
Compliance with Ethical Standards
Conflict of interest
Dr Anand K. Pyati, Dr Basavaraj B. Devaranavadagi, Dr Sanjeev L. Sajjannar, Dr Shashikant V. Nikam, Dr Mohd Shannawaz and Dr Satish Patil declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Dienstag JL. Ischemic heart disease. In: Fauci AS, Kasper DL, Longo DL, Braunwald E, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison’s principles of internal medicine. 17. New York: McGraw Hill Medical; 2008. pp. 1955–1969. [Google Scholar]
- 2.Gupta R, Joshi P, Mohan V, Reddy KS, Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94(1):16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 3.Elmadbouh I, Mahfouz R, Bayomy N, Faried W, Ghanayem N. The value of human heart-type fatty acid binding protein in diagnosis of patients with acute chest pain. Egypt Heart J. 2012;64:179–184. doi: 10.1016/j.ehj.2012.06.004. [DOI] [Google Scholar]
- 4.McMahon CG, Lamont JV, Curtin E, McConnell RI, Crockard M, Kurth MJ, et al. Diagnostic accuracy of heart-type fatty-acid binding protein for the early diagnosis of acute myocardial infarction. Am J Emerg Med. 2012;30:267–274. doi: 10.1016/j.ajem.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 5.Alhadi HA, Fox KAA. Do we need additional markers of myocyte necrosis: the potential value of heart type fatty acid binding protein. Q J Med. 2004;97:187–198. doi: 10.1093/qjmed/hch037. [DOI] [PubMed] [Google Scholar]
- 6.Wild D, editor. The immunoassay handbook. 2. London: Nature Publishing Group; 2001. [Google Scholar]
- 7.Bhatia DP, Carless DR, Viswanathan K, Hall AS, Barth JH. Serum 99th centile values for two heart type fatty acid binding protein assays. Ann Clin Biochem. 2009;46(6):464–467. doi: 10.1258/acb.2009.009055. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y, Kim H, Kim SY, Lee HK, Kwon HJ, Kim YG, et al. Automated heart-type fatty acid binding protein assay for the early diagnosis of acute myocardial infarction. Am J Clin Pathol. 2010;134:157–162. doi: 10.1309/AJCP0F6AXRCJMQQG. [DOI] [PubMed] [Google Scholar]
- 9.ARCHITECT Stat Troponin: I [Package Insert]. Abbott Park, IL 60064 USA: Abbott Laboratories; 2010.
- 10.ARCHITECT Stat Myoglobin [Package Insert]. Abbott Park, IL 60064 USA: Abbott Laboratories; 2010.
- 11.Recommendations of the German Society for Clinical Chemistry Standardization of methods for the estimation of enzyme activities in biological fluids. Standard method for the determination of creatine kinase activity (1976) J Clin Chem Clin Biochem. 1977;15:255. [Google Scholar]
- 12.Witt I, Trendelenburg C. Joint study to establish reference values for clinical chemical parameters in childhood. J Clin Chem Clin Biochem. 1982;20(4):235–242. [PubMed] [Google Scholar]
- 13.Pasaoglu H, Ofluoglu E, Ilhan MN, Cengel A, Ozdemir M, Durakoglugil E, et al. The role of heart-type fatty acid binding protein (H-FABP) in acute myocardial infarction compared to cardiac biochemical markers. Turk J Med Sci. 2007;37(2):61–67. [Google Scholar]
- 14.Orak M, Üstündag M, Güloglu C, Özhasenekler A, Alyan O, Kale E. The role of the heart-type fatty acid binding protein in the early diagnosis of acute coronary syndrome and its comparison with troponin I and creatine kinase-MB isoform. Am J Emerg Med. 2010;28:891–896. doi: 10.1016/j.ajem.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Alhadi HA, Fox KAA. Heart-type fatty acid-binding protein in the early diagnosis of acute myocardial infarction: the potential for influencing patient management. Sultan Qaboos Univ Med J. 2010;10(1):41–49. [PMC free article] [PubMed] [Google Scholar]
- 16.Alansari SE, Croal BL. Diagnostic value of heart fatty acid binding protein and myoglobin in patients admitted with chest pain. Ann Clin Biochem. 2004;41:391–396. doi: 10.1258/0004563041731565. [DOI] [PubMed] [Google Scholar]
- 17.Freund Y, Chenevier-Gobeaux C, Leumani F, Claessens Y, Allo J, Doumenc B, et al. Heart-type fatty acid binding protein and the diagnosis of acute coronary syndrome in ED. Am J Emerg Med. 2012;30:1378–1384. doi: 10.1016/j.ajem.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Kim KS, Lee HJ, Kim K, Jo YH, Kim TY, Lee JH, et al. Heart-type fatty acid binding protein as an adjunct to cardiac troponin-i for the diagnosis of myocardial infarction. Korean Med Sci. 2011;26:47–52. doi: 10.3346/jkms.2011.26.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]