Abstract
The cause of more insulin resistance in female than males are still unknown. To know the cause from early life, normal values of relevant parameters are required. So, aim of this study was to determine the reference levels of glucose and insulin in cord blood of term newborns and to examine their effects on gender, placental and birth weight of term newborns. In cross sectional study 60 consecutive term newborns were included from constituent hospitals. Placental and birth weights were measured and cord blood was collected for estimation of serum insulin and plasma glucose. Plasma glucose estimation was done by auto analyzer (GOD–POD method) and serum insulin analysis was done using Insulin ELISA Kit. After analysis, mean ± 2SD used for estimating cord blood insulin and glucose levels, which were 10.1 ± 7.8 μIU/mL and 67.8 ± 33.8 mg/dL respectively. Correlation of insulin with both birth weight and placental weight were r = 0.359 and 0.41 respectively; p < 0.001. Interestingly we found higher insulin levels in females as compared to male newborns in spite of having lower birth weight in them. In conclusion this study reported the levels of insulin and glucose in cord blood of term newborns. Incidentally, this is the first study as per our knowledge to report significant correlation between cord blood insulin, glucose with birth weight, placental weight and gender in south India. Female newborns had higher insulin levels than males, despite lesser birth weight can be attributed to intrinsic insulin resistance in them.
Keywords: Cord blood, Insulin, Glucose, Birth weight, Placental weight
Introduction
The overall mechanism of the fetal growth and it’s regulation in utero as well as in the postnatal life is still poorly understood. There is interaction between fetal and placental endocrine system which leads to partitioning of nutrients and helps in proliferation and maturation of fetal cells. Among all hormones, insulin is the most important one with a growth promoting function [1]. ‘Fetal insulin hypothesis’ proposed the relationship between inherited insulin resistance and altered growth mediated by insulin. It has been reported that there is gender difference in the insulin levels which show girls are intrinsically more insulin resistant than boys. Hyperinsulinaemia might be seen even without insulin resistance but it is a well-known risk factor for insulin resistance [2, 3].
Birth weight is a valuable measure of fetal growth and to an extent it reflects upon the fetal origin of certain adult diseases. Low as well as high birth weight can lead to development of obesity and diabetes in later part of life [4]. One of the studies in Indian new borns, reported a greater incidence of females being born with lower birth weight as compared to males. It is well-known that birth weight is associated with the placental weight but abnormal birth and placental weight are independent risk factors for different cardiovascular disease development in adult life [5–7]. Placenta is a complex organ having high amount of insulin receptors which has pleiotropic role during fetal growth whereas Insulin has direct and indirect effects on the placenta [8].
The people of Indian origin are found to be more insulin-resistant than European Caucasians. It has been found that newborns of Indian origin have higher insulin levels in cord blood as compared to UK population in spite of having similar birth weight in both the regions. Hyperinsulinemia in the cord blood may be the cause for the genetic predisposition of Indian newborns to insulin resistance [2, 9]. Early alteration in insulin-glucose homeostasis increases the risk of developing insulin resistance and obesity in the later years. As per the ICMR-INDIAB study, new figures for diabetes prevalence indicate that the epidemic is progressing rapidly across the nation, reaching a total of 62.4 million persons with diabetes and 77.5 million persons with pre-diabetes in 2011 [10]. Thus, early detection of such high risk population at an early stage of life is of vital importance and should be considered to decrease the burden of this pandemic disease [11].
To investigate any endocrine or metabolic disorder, normal values of relevant parameters are required. There are no studies in this regard, based on Indian population to date, citing the normal levels of insulin and glucose in cord blood of term newborns. This study is aimed at determining the reference levels of insulin and glucose in cord blood of term newborns. Very few studies have correlated these parameters to placental and birth weight. Hence this study will also emphasize the relationship of cord blood insulin and glucose levels on gender, placental and birth weight of term newborns.
Materials and Methods
Subject Selection Criteria and Sample Collection
Cross sectional study comprising 60 term newborns (37–41 weeks 6/7 days of gestation) from the constituent hospitals of Medical College in and around Mangalore was done from April 2014 to December 2014. The study was approved by the Institutional Research and Ethics Committee and consent were taken from the mothers of all newborns included in this study. Fifth minute Apgar score >9 for all term newborns was included in the study. All preterm newborns or term newborns with fifth minutes Apgar score <9 were excluded from the study. Mothers suffering from any infectious disease or having obstetric complications like gestational diabetes, hypertension, kidney disease, thyroid disease, PCOD etc. were also excluded from the study.
Venous cord blood (VCB) was collected under aseptic conditions from the umbilical cords of 60 newborns born through normal vaginal deliveries. After delivery, but prior to expulsion of placenta, 3 mL blood was drawn from umbilical cord into a plain and a fluoride vacutainer. Plasma glucose was analyzed immediately within 4 h of collection. Serum separated and was stored at −20 °C until further analysis of insulin by ELISA (Enzyme linked immunosorbent assay). All data regarding mother and newborn were collected from mother’s case sheet.
Biochemical Estimations and Analysis
Plasma glucose estimation was done by glucose oxidase–peroxidase (GOD–POD) method (Agappe diagnostic kits, Ernakulam, Kerala) using Roche Hitachi P800 auto-analyser (Roche Diagnostics GmbH, Mannheim). The coefficient of variation (CV) for intra and inter-batch for glucose was <5 %. Insulin levels were assayed based on sandwich principle in ELx 800 by BIO TEK® Instruments, Inc. using insulin ELISA kit manufactured by “DRG, German company”. The CV for intra and inter-batch insulin assay was <3 %. Insulin resistance was calculated by HOMA 2IR/HOMA Calculator ver2.2 (Homeostasis model assessment) [12]. Placenta was weighed with digital scale within 1 h of expulsion. The weights of all newborns were measured with the same instruments in labor room after cord clamping.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics version 17 (SPSS, Chicago, IL, USA). The data were presented as Mean ± SD. The reference values for insulin and glucose was calculated by using Mean ± 2SD. Student independent ‘t’ test and Pearson’s correlation coefficient were used to determine the significance between variables. p value less than 0.05 was considered statistically significant.
Results
Mothers included in the study were between 20 and 38 years of age with mean age of 26.8 years. Data of all 60 newborns with 23 males (38.3 %) and 37 females (67.7 %), their placental weight, birth weight, anthropometry, cord blood glucose, insulin and HOMA 2IR values were reported (Table 1).
Table 1.
Placental weight, birth weight, crown rump length, head circumference, cord blood glucose, insulin and HOMA 2IR
| Categories | Gender | N | Mean | SD (95 % CI) | SE | Range |
|---|---|---|---|---|---|---|
| Placental weight (g) | Male | 23 | 497.3 | 95.9 (455.8–538.8) | 20.0 | 350–680 |
| Female | 37 | 556.7 | 74.6 (531.8–581.6) | 12.26 | 420–680 | |
| Total | 60 | 534 | 87.6 (511.3–566.6) | 11.31 | 350–680 | |
| Birth weight (kg) | Male | 23 | 3.0 | 0.37 (2.9–3.2) | 0.07 | 2.5–3.5 |
| Female | 37 | 2.8 | 0.23 (2.7–2.9) | 0.03 | 2.5–3.4 | |
| Total | 60 | 2.9 | 0.31 (2.8–3) | 0.04 | 2.5–3.5 | |
| Crown-rump length (cm) | Male | 23 | 50.0 | 2.22 (49–51) | 0.46 | 46–54 |
| Female | 37 | 48.1 | 1.73 (47.5–48.7) | 0.28 | 44–51 | |
| Total | 60 | 48.8 | 2.13 (48.3–49.4) | 0.27 | 44–54 | |
| Head circumference (cm) | Male | 23 | 33.3 | 0.98 (32.9–33.7) | 0.20 | 32–35 |
| Female | 37 | 33.0 | 1.50 (32.5–33.5) | 0.24 | 30–38 | |
| Total | 60 | 33.1 | 1.32 (32.8–33.5) | 0.17 | 30–38 | |
| Insulin (μIU/mL) | Male | 23 | 8.5 | 3.63 (6.9–10.1) | 0.75 | 3.3–16 |
| Female | 37 | 11.0 | 3.83 (9.8–12.3) | 0.63 | 3–18 | |
| Total | 60 | 10.1 | 3.93 (9–11.1) | 0.50 | 3–18 | |
| Glucose (mg/dL) | Male | 23 | 74.0 | 17.48 (66.4–81.6) | 3.64 | 40–114 |
| Female | 37 | 63.9 | 15.56 (58.7–69) | 2.55 | 39–124 | |
| Total | 60 | 67.8 | 16.91 (63.4–72.2) | 2.18 | 39–124 | |
| HOMA 2IR | Male | 23 | 1.02 | 0.44 | 0.092 | 0.4–2 |
| Female | 37 | 1.26 | 0.45 | 0.074 | 0.3–2.3 | |
| Total | 60 | 1.17 | 0.46 | 0.059 | 0.3–2.3 |
HOMA 2IR homeostasis model assessment-insulin resistance, CI confidence interval (lower value–higher value), N number of subjects
Normal range of cord blood insulin and glucose levels in all subjects was calculated by taking Mean ± 2SD which were 2.31–17.9 μIU/mL and 34–101.6 mg/dL respectively. Independent sample ‘t’ test was done to compare the different parameters between male and female term newborns (Table 2). Male and female term newborns differed significantly in terms of insulin levels and placental weight. Female newborns were having higher insulin (11 ± 3.8 μIU/mL, p = 0.01) and placental weight (556.7 ± 74.6 g, p = 0.01) than males in whom mean insulin and placental weight was 8.5 ± 3.6 μIU/mL and 497.3 ± 95.9 g respectively. On the other hand, male babies had higher birth weight (3.08 ± 0.3 kg, p = 0.02) and glucose levels (74 ± 17.4 mg/dL, p = 0.03) as compared to female babies in whom birth weight and glucose levels were 2.87 ± 0.2 kg and 63.9 ± 15.5 mg/dL respectively.
Table 2.
Comparison of cord blood insulin, glucose, placental and birth weight in Male and female of term newborns
| Males (23) | Females (37) | p value | |
|---|---|---|---|
| Insulin (μIU/mL) | 8.5 ± 3.6 | 11 ± 3.8 | 0.01* |
| Glucose (mg/dL) | 74 ± 17.4 | 63.9 ± 5.5 | 0.03* |
| Placental weight (g) | 497.3 ± 95.9 | 556.7 ± 74.6 | 0.01* |
| Birth weight (kg) | 3.08 ± 0.3 | 2.87 ± 0.2 | 0.02* |
Values are presented as mean ± SD and significance was calculated between male and female (* indicates p < 0.05; statically significant)
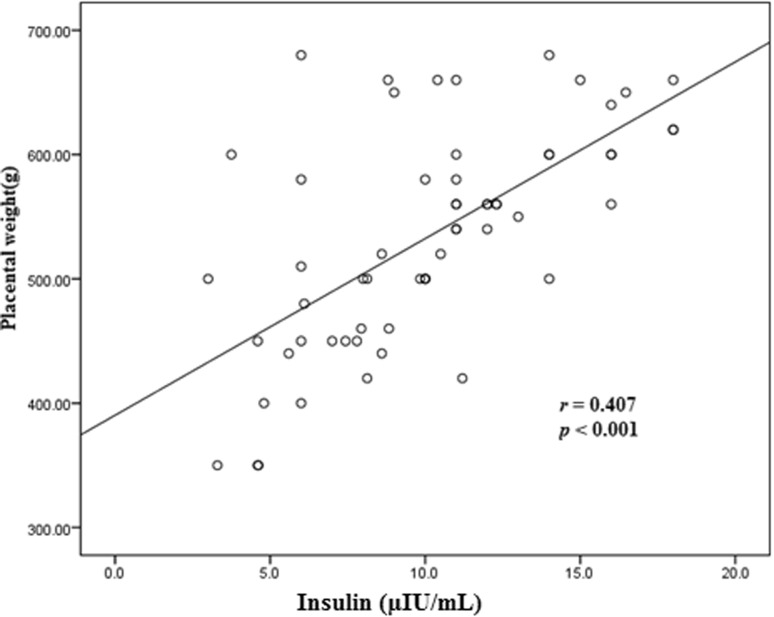
Scatter plot and Pearson’s correlation coefficient was used to describe the linear relationship between birth weight and insulin in term newborns (Fig. 1). There was a statistically significant correlation between them (r = 0.359 and p < 0.001) and also a significant linear relation between placental weight and insulin (r = 0.407 and p < 0.001) (Fig. 2).
Fig. 1.
Correlation between birth weight and cord blood insulin levels
Fig. 2.
Correlation between placental weight and cord blood insulin levels
Distribution of insulin, glucose and HOMA 2IR at birth (Table 3); the 90th percentile of distribution for insulin levels was 16 μIU/mL, glucose 87.9 mg/dL and fourth quartile of HOMA 2IR index was found 1.5. In the absence of established reference cut-off points for insulin, glucose and HOMA 2IR in cord blood of term newborns, the above values have been considered as the cut-off points for this study.
Table 3.
Distribution of VCB insulin, glucose and HOMA 2IR index in term newborns
| Categories | Mean ± SD | Percentile | ||||
|---|---|---|---|---|---|---|
| 5 | 25 | 50 | 75 | 90 | ||
| Insulin (µIU/mL) | 10.1 ± 3.9 | 3.8 | 7.1 | 10 | 12.3 | 16 |
| Glucose (mg/dL) | 67.83 ± 16.9 | 40.2 | 58.2 | 64 | 77.7 | 87.9 |
| HOMA 2IR | 1.17 ± 0.46 | 0.6 | 0.8 | 1.1 | 1.5 | 1.89 |
HOMA 2IR homeostasis model assessment-insulin resistance
Discussion
Cord blood is a substantial source of information of the body status of the newborns. For reliable estimation and interpretation of cord blood parameters, it is essential to have an established reference range to support any clinical diagnosis. The values given in the text books are with reference to very old studies conducted elsewhere. Therefore, current study evaluation of VCB estimate of insulin and glucose levels in 60 consecutive healthy term newborns is an add-on to the information pool.
The normal range of cord blood insulin (3–18 μIU/mL) reported in our study results is in agreement with that reported by Kirmi et al. (0.5–18 μIU/mL) and also matches the value quoted in text books (3–20 µIU/mL). We have calculated the reference levels of insulin by Mean ± 2SD 10.1 ± 7.8 µIU/mL and obtained the reference range of 2.31–17.9 which shows range of insulin is almost same i.e. 0.5–18 µIU/mL, but the mean is higher 6.01 ± 7.3 µIU/mL than the other study. There are studies which claimed that levels of VCB insulin levels can be different among different races [13]. Mean ± 2SD of glucose was 67 ± 33.8 mg/dL and reference range we calculated was 34–101.6 mg/dL, which differs from other studies.
This study also highlights the significant difference in values of cord blood insulin, glucose, placental weight and birth weight with respect to gender. Female newborns were having significantly higher insulin levels and placental weight than male newborns. The action of insulin as a growth factor helps in the development of placenta owing to the presence of higher amount of insulin receptors as compared to other tissues. This shows female newborns are more intrinsically prone to insulin resistance than the male newborns owing to high insulin levels. They are also more prone to risk of developing diabetes mellitus than males as claimed by other studies [2, 3]. This can be further justified by the current literature stating that average weight, length, and the head circumference of girls are lower than that of boys, but girls are having more adipose tissue because of higher circulating insulin levels at term may be due to some intrinsic genetic cause [14].
To the best of our knowledge, this is the first study of its kind in India in term newborns conducted to correlate cord blood insulin levels with birth and placental weight. Moderate linear correlation was found between insulin levels and birth weight (r = 0.359, p = 0.001) and placental weight (r = 0.407, p = 0.001). This implies that as insulin level increases, birth and placental weight also increases. This finding confirms the growth promoting effect of insulin in early stage of life [13]. Mean birth weight (2.9 ± 0.31 kg) in our study was lower than that reported by Wolf et al. (3.3 ± 0.5 kg) whereas mean insulin levels (10.1 ± 3.9 µIU/mL) were higher than the levels reported by others studies (7.1 ± 4.3 µIU/mL). This difference can be attributed to genetic predisposition of insulin to certain races [15].
In this study we also calculated the distribution of hyperinsulinemia and insulin resistance in term newborns by using 90th percentile for insulin and fourth quartile for HOMA 2IR index. Cutoff values of 16 µIU/mL for insulin and 1.5 for HOMA2IR have been found in our study population. So hyperinsulinemia in cord blood is defined by serum insulin levels >16 µIU/mL and insulin resistance by HOMA 2IR by >1.5. In our study cut off value for insulin was higher than that reported by Simental-Mendia et al. (13 µIU/mL), however they stated higher IR values i.e. 2.6 [4]. This may be attributed to racial variation, even though none of the newborns were seen to cross these cut-off values in our study population.
The reference range established from a smaller sample size cannot be generalized to a larger population is the limitation of this study. Hence, further studies in this regard can be taken up in a larger population. Our study population consisted of more number of females which might be a bias in the study. Ideally Receiver Operating Curve should be plotted to establish the optimum cut-off for cord blood insulin and HOMA 2IR. Larger prospective cohort studies are needed in future to measure the levels of these parameters in cord blood and compare the same levels in blood.
Impact of current study is the reference values of cord blood insulin and glucose established in term newborns of Southern India residing in and around Mangalore considering normal distribution of data. This is a first study in India to the best of our knowledge which reports the gender difference of insulin, glucose, birth weight and placental weight in term newborns. This study also indicates a linear correlation between cord blood insulin and birth and placental weight. An additional implication of this study is the evaluation of percentile distribution to estimate the cut off levels for insulin and HOMA 2IR index in order to predict insulin resistance in term newborns.
Conclusion
This study suggests the reference levels for cord blood insulin and glucose in term newborns. Placental weight is an important determinant of both birthweight and fetal growth. It modifies the effect of determinants insulin and glucose on both birthweight and fetal growth parameters. The important finding of the present study was the presence of lower birth weight in female newborns when compared to males in spite of high cord blood insulin levels, low glucose and smaller size. Thus, less fat content and high insulin level at birth may influence the body composition of Indian female newborns to develop intrinsic insulin resistance in them since birth and their susceptibility to future metabolic disorders.
Acknowledgments
The authors are grateful to the Department of OBG and all the mothers of newborns recruited in this study for their kind cooperation. The authors thank Dr. Vinay Kumar Saili for aiding with the statistics.
Compliance with Ethical Standards
Conflict of interest
The authors have no conflict of interest.
Source of Funding
(i) Part of PG Dissertation granted by Indian Council of Medical Research (ICMR), MOH&FW, New Delhi and (ii) Manipal University Research Grant for MD dissertation.
References
- 1.Buongiorno AM, Morelli S, Sagratella E, Sensi M, Maroccia E, Caiola S, et al. Influence of family history of type 2 diabetes on leptin concentration in cord blood of male offspring with high birth weight. Ann Ist Super Sanita. 2007;43(1):77–82. [PubMed] [Google Scholar]
- 2.Shields BM, Knight B, Hopper H, Hill A, Powell RJ, Hattersley AT, et al. Measurement of cord insulin and insulin-related peptides suggests that girls are more insulin resistant than boys at birth. Diabetes Care. 2007;30:2661–2666. doi: 10.2337/dc06-1501. [DOI] [PubMed] [Google Scholar]
- 3.Brunner S, Schmid D, Huttinger K, Much D, Heimberg E, Sedlmeier EM, et al. Maternal insulin resistance, triglycerides and cord blood insulin in relation to post-natal weight trajectories and body composition in the offspring up to 2 years. Diabet Med. 2013;30(12):1500–1507. doi: 10.1111/dme.12298. [DOI] [PubMed] [Google Scholar]
- 4.Simental-Mendia LE, Castaneda-Chacon A, Rodriguez-Moran M, Guerrero-Romero F. Birth-weight, insulin levels, and HOMA-IR in newborns at term. BMC Pediatr. 2012;7(12):94. doi: 10.1186/1471-2431-12-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nayak AU, Sundari N. Placental weight and its ratio to birth weight in normal pregnancy. Indian J Prev Soc Med. 2009;40(3–4):147–150. [Google Scholar]
- 6.Agarwal N, Reddaiah VP. Factors affecting birth weight in a sub-urban community: a study in a secondary level hospital in Delhi. Health Popul Perspect. 2005;28(4):189–196. [Google Scholar]
- 7.Madkar C, Musale J, Deshpande H, Shitole R. A study of Placental weight and birth weight ratio (PW/BW) and it’s effects on perinatal outcome. IJOGR. 2015;2(1):1–6. [Google Scholar]
- 8.Desoye G, Hauguel-de mouzon S. The human placenta in gestational diabetes mellitus. Diabetes Care. 2007;30:120–126. doi: 10.2337/dc07-s203. [DOI] [PubMed] [Google Scholar]
- 9.Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA, Deshpande SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metab. 2002;87(12):5575–5580. doi: 10.1210/jc.2002-020434. [DOI] [PubMed] [Google Scholar]
- 10.Anjana RM, Pradeepa R, Deepa M, Dutta M, Sudha V, Unnikrishna R, et al. Prevalence of diabetes and prediabetes in urban and rural India: phase I results of Indian Council of Medical Research-(ICMR-INDIAB) study. Diabetologia. 2011;54:3022–3027. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 11.Gesteiro E, Bastida S, Sanchez-Muniz FJ. Cord-blood lipoproteins, homocysteine, insulin sensitivity/resistance marker profile, and concurrence of dysglycaemia and dyslipaemia in full-term neonates of the merida study. Eur J Pediatr. 2013;172(7):883–894. doi: 10.1007/s00431-013-1959-x. [DOI] [PubMed] [Google Scholar]
- 12.Geloneze B, Vasques AC, Stabes CF, Pareja JC, Rosado PL, Queiroz EC, et al. HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian metabolic syndrome study. Arq Bras Endocrinol Metabol. 2009;53(2):281–287. doi: 10.1590/S0004-27302009000200020. [DOI] [PubMed] [Google Scholar]
- 13.Kirimi E, Cesur Y, Gul A. Normal levels of insulin, growth hormone and cortisol levels in venous cord blood of healthy full term infants: correlation with birth weight and placental weight. East J Med. 2000;6(1):14–17. [Google Scholar]
- 14.Mitra S, Nayak PK, Sahoo J, Misra S, Kamalanathan S. Gender-based differences in anthropometry and cord blood insulin levels in term neonates. Iran J Pediatr. 2014;24(1):118–119. [PMC free article] [PubMed] [Google Scholar]
- 15.Wolf HJ, Ebenbichler CF, Huter O, Bodner J, Lechleitner M, Foger B, et al. Fetal leptin and insulin levels only correlate inlarge-for-gestational age infants. Eur J Endocrinol. 2000;142(6):623–629. doi: 10.1530/eje.0.1420623. [DOI] [PubMed] [Google Scholar]