Abstract
Introduction
Following the 2014 expansions of Medicaid and private health insurance through the Affordable Care Act, municipal sexually transmitted disease (STD) clinics— which have historically served predominantly uninsured patients—have been threatened with budget cuts nationwide. This study was conducted to evaluate the impact of the insurance expansions on the demand for STD clinic services.
Methods
The proportion of total incident sexually transmitted infections in Baltimore City that were diagnosed at STD clinics was compared between 2013 and 2014, and a multivariate analysis was conducted to determine factors associated with diagnosis at an STD clinic. Analyses were conducted in July 2015.
Results
There was no change in the overall proportion of sexually transmitted infection diagnoses made at STD clinics from 2013 to 2014 (relative rate, 1.03; 95% CI=0.95, 1.11). Hispanic ethnicity, black race, male sex, and age >24 years were associated with an increased likelihood of STD clinic utilization (p<0.0001).
Conclusions
Despite the Affordable Care Act's insurance expansion measures, the demand for STD clinics remained stable. These safety net clinics serve patients likely to face barriers accessing traditional health care and their preservation should remain a priority.
Introduction
The Affordable Care Act (ACA) improved healthcare access for millions of Americans, putting into question the role of publicly funded sexually transmitted disease (STD) clinics nationwide.1–3 With Medicaid expansion and the Health Benefits Exchanges, policymakers anticipated reduced demands for safety net clinics as newly insured patients increasingly obtained sexually transmitted infection (STI) services directly from primary care providers. However, many other high-income countries have maintained their governmentally supported STD clinics despite universal healthcare access.4 Before policymakers make further cuts to STD clinic budgets, it is critical to evaluate the impact of insurance expansion on STD clinic utilization.
To evaluate changes in the demand for STD clinic services, this study compared the proportion of incident STIs in Baltimore, Maryland, diagnosed at municipal STD clinics before and after implementation of the ACA's insurance expansion measures in January 2014. Baltimore is one of ten U.S. cities with the highest burden of STIs.5
Methods
The Baltimore City Health Department (BCHD) routinely collects surveillance data on new diagnoses of gonorrhea, chlamydia, syphilis, and HIV from all healthcare facilities in Baltimore City. Patient demographics and the healthcare facilities reporting the STIs are recorded for each diagnosis. Among the more than 900 Baltimore City healthcare facilities are two municipal STD clinics overseen by the BCHD, both of which operate primarily on the basis of walk-in visits and do not bill for services or charge copays. STI records of Baltimore residents aged ≥13 years reported to the BCHD between January 1, 2013 and December 31, 2014 were eligible for inclusion in this analysis, which was conducted in July 2015. The main outcome of interest was the relative proportion of incident STIs diagnosed at the STD clinics in 2014 compared with 2013.
Statistical Analysis
Patient demographics for STI diagnoses in 2013 were compared with those in 2014 (Appendix Table 1), and crude proportions of total incident syphilis, HIV, gonorrhea, and chlamydia diagnoses made at STD clinics were compared between the 2 years.
Log binomial regression was used to conduct a multivariate analysis of factors associated with diagnosis at an STD clinic compared with other healthcare facilities. Adjusted variables included diagnosis year, age, sex, race, and ethnicity. Missing values were excluded listwise. Statistical analyses were conducted using Stata, version 13. The study was approved by the Johns Hopkins IRB and the BCHD Public Health Research Review.
Results
A total of 10,061 STI diagnoses were reported to the BCHD in 2013 and 10,047 were reported in 2014. Among these, 98.6% had information on the healthcare facility where the diagnosis was made. Similar proportions of patients with any incident STI were diagnosed at the municipal STD clinics during the 2 years: 11.36% in 2013 versus 11.31% in 2014 (p=0.90).
Figure 1 compares the crude proportions of syphilis, HIV, chlamydia, and gonorrhea diagnoses made at STD clinics pre- and post-Medicaid expansion. Although there were no significant changes in the proportions of syphilis or HIV cases diagnosed at STD clinics, the proportion of chlamydia diagnoses at STD clinics increased from 8.76% in 2013 to 9.77% in 2014 and that for gonorrhea decreased from 18.45% to 14.80% (p<0.05).
Figure 1.
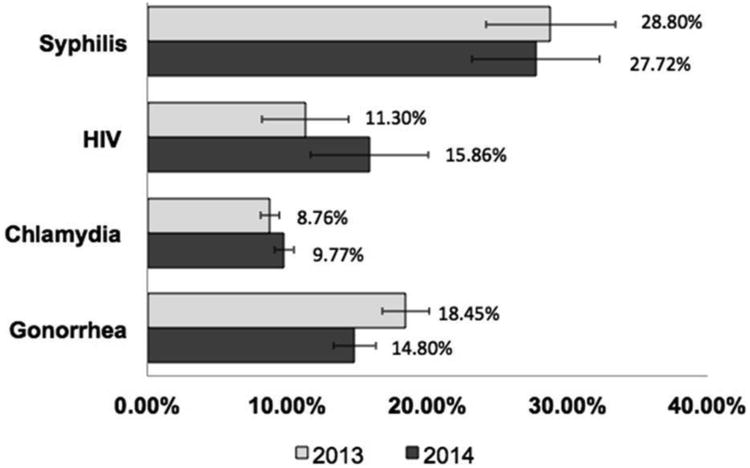
STIs diagnoses made at municipal STD Clinics before and after the ACA's Medicaid and private insurance expansions, Baltimore City, Maryland.
STI, sexually transmitted infection; STD, sexually transmitted disease; ACA, Affordable Care Act
A multivariate analysis demonstrated that, on average, STI patients who were Hispanic, black, male, or aged >24 years were more likely to be diagnosed at an STD clinic than their counterparts (Table 1). Listwise exclusion of missing values in the regression reduced the total number of STI records by 17% (from 20,987 to 17,487).
Table 1. Factors Associated With STI Diagnosis at a Municipal STD Clinic, Baltimore City, MD, 2013-2014.
| Diagnosed at STD clinic | Not diagnosed at STD clinic | Unadjusted relative rate | Adjusted relative rate a | |||||
|---|---|---|---|---|---|---|---|---|
| N= 2,218 | % | N= 15,260 | % | RR | (95% CI) | aRR | (95% CI) | |
| Year | ||||||||
| 2013 | 1,112 | 12.4 | 7,853 | 87.6 | 1.00 | 1.00 | ||
| 2014 | 1,106 | 13.0 | 7,407 | 87.0 | 1.05 | (0.97-1.13) | 1.03 | (0.95–1.11) |
| Age | ||||||||
| <24 yrs. | 1,231 | 10.6 | 10,396 | 89.4 | 0.63 | (0.58-0.68)** | 0.76 | (0.71-0.83)** |
| >24 yrs. | 987 | 16.9 | 4,864 | 83.1 | 1.00 | 1.00 | ||
| Hispanic | ||||||||
| No | 2,150 | 12.6 | 14,910 | 87.4 | 1.00 | 1.00 | ||
| Yes | 68 | 16.3 | 350 | 83.7 | 1.28 | (1.03-1.61)* | 1.52 | (1.20-1.93)** |
| Black race | ||||||||
| No | 201 | 12.0 | 1,469 | 87.96 | 1.00 | 1.00 | ||
| Yes | 2,017 | 12.8 | 13,791 | 87.2 | 1.06 | (0.93-1.21) | 1.34 | (1.15-1.55)** |
| Sex | ||||||||
| Female | 885 | 8.0 | 10,163 | 92.0 | 1.00 | 1.00 | ||
| Male | 1,333 | 20.7 | 5,097 | 79.3 | 2.59 | (2.39-2.80)** | 2.44 | (2.25-2.65)** |
Adjusted for year of diagnosis, age, ethnicity, race, and sex using log binomial regression
Note: Boldface indicates statistical significance
p<0.05;
p<0.001.
STI, sexually transmitted infection; STD, sexually transmitted disease
Discussion
The results of this study demonstrate a continued demand for municipal STD clinics during the year following implementation of the ACA, as the overall proportion of STI diagnoses made at these safety net clinics did not change. In addition, ethnic and racial minorities and men were more likely to be diagnosed at STD clinics. These populations are at increased risk of STIs and less likely to have established sources of primary care.6–9
Many factors likely contributed to the steady utilization of STD clinics in 2014. STD clinics offer walk-in services free of charge, improving access to uninsured populations. A recent study predicted that, despite the ACA, more than 10% of Americans are expected to remain uninsured over the next 8 years and, by 2023, 4.7 million uninsured people will be in need of STI services.10
Even pre-ACA, approximately a third of patients visiting the San Francisco and Denver municipal STD clinics were insured, suggesting that patients use STD clinics for reasons other than a lack of insurance.6,9,11 In 2015, approximately 50% of patients receiving services at the Baltimore City STD clinic were insured, primarily through Medicaid. STD clinics are preferred because of convenience, confidentiality, and cultural competence in treating vulnerable populations.4,7,9,11,12
Hispanic ethnicity, black race, male sex, and age >24 years were associated with increased risk of diagnosis at STD clinics compared with other healthcare settings. Hispanic immigrants in Baltimore may rely on STD clinics, as many are ineligible for insurance coverage owing to their immigration status. Similarly, black patients who reside within the vicinity of the STD clinics face stressors associated with lack of insurance, including poverty, lack of trust in the traditional healthcare system, substance abuse, and urban violence. The finding that men were more likely to be diagnosed at STD clinics than women was not surprising because men have lower utilization of traditional healthcare resources than women of childbearing age.8,12
Given the current fiscal environment, budget cuts may be inevitable, and STD clinics must seek alternative methods to maximize efficiency. Express testing or STD testing without a full clinical exam on asymptomatic patients can significantly reduce patient waiting time.13–15 Likewise, third-party billing, including Medicaid billing, could diversify revenue streams.2
Limitations
Only 1 year of surveillance data after the 2014 ACA insurance expansion measures was available, so these findings may be premature. However, the number of patient visits to the BCHD STD clinics remained stable in 2015 compared to 2014, more than 1 year after the ACA's implementation. Of note, budget cuts made to the BCHD STD clinics in October 2013 reduced operating hours by nearly 50% and an express testing pathway was implemented. These changes would have been expected to cause a decrease in the proportion of diagnoses made at STD clinics in 2014 compared with 2013, but this was not the case, demonstrating steady demand.
The multivariate analysis excluded a greater proportion of STI cases occurring at non– STD clinic locations owing to increased propensity of missing demographic data by these providers. However, bias and a Type II error are unlikely, as the excluded proportions were similar in 2013 and 2014. Finally, this study represents one urban center, and STI data from other cities must be analyzed to fully understand the ACA's effects on STD clinic utilization on a national scale.
Conclusions
Utilization of STD clinic services—particularly among high-risk individuals—has remained steady after the implementation of the ACA, substantiating their need for continued funding. Although the ACA has made important strides in expanding health insurance coverage, gaps persist and barriers to timely access to STD-related healthcare services are common.
Supplementary Material
Acknowledgments
This publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by Grant Number TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS), a component of NIH. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS, or NIH. NM conducted the analyses and prepared the article. CS, KGG, LJ, and JJ provided extensive input on the design of the study and aided in the article's editing process. JK and CPC provided additional comments and suggestions and approved the final article. KRP conceptualized and designed the study and provided extensive editing for the article.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cramer R, Leichliter JC, Gift TL. Are safety net sexually transmitted disease clinical and preventive services still needed in a changing health care system? Sex Transm Dis. 2014;41(10):628–630. doi: 10.1097/OLQ.0000000000000187. http://dx.doi.org/10.1097/OLQ.0000000000000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Coalition of STD Directors (NCSD) Fact Sheet: Shifting to Third-Party Billing for Public Health STD Services: Policy Context and Case Studies. [Accessed June 26, 2015]; www.ncsddc.org/sites/default/files/media/finalbillingguide.pdf.
- 3.Stephens SC, Cohen SE, Philip SS, Bernstein KT. Insurance among patients seeking care at a municipal sexually transmitted disease clinic: implications for health care reform in the United States. Sex Transm Dis. 2014;41(4):227–232. doi: 10.1097/OLQ.0000000000000109. http://dx.doi.org/10.1097/OLQ.0000000000000109. [DOI] [PubMed] [Google Scholar]
- 4.Golden MR, Kerndt PR. Improving clinical operations: can we and should we save our STD clinics? Sex Transm Dis. 2010;37(4):264–265. doi: 10.1097/OLQ.0b013e3181d5e01e. http://dx.doi.org/10.1097/olq.0b013e3181d5e01e. [DOI] [PubMed] [Google Scholar]
- 5.CDC. Sexually Transmitted Disease Surveillance 2014. Atlanta: U.S. DHHS; 2015. [Google Scholar]
- 6.Celum CL, Bolan G, Krone M, et al. Patients attending STD clinics in an evolving health care environment. Demographics, insurance coverage, preferences for STD services, and STD morbidity. Sex Transm Dis. 1997;24(10):599–605. doi: 10.1097/00007435-199711000-00009. http://dx.doi.org/10.1097/00007435-199711000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Pathela P, Klingler EJ, Guerry SL, et al. Sexually transmitted infection clinics as safety net providers: exploring the role of categorical sexually transmitted infection clinics in an era of health care reform. Sex Transm Dis. 2015;42(5):286–293. doi: 10.1097/OLQ.0000000000000255. http://dx.doi.org/10.1097/OLQ.0000000000000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.James C, Alina S, Usha R, Andrew G, Philethea D. Putting men's health care disparities on the map: Examining racial and ethnic disparities at the state level. [Accessed June 26, 2015];2012 http://www.edfoxphd.com/men_shealth.pdf.
- 9.Hoover KW, Parsell KW, Leichliter JS, et al. Continuing need for Sexually Transmitted Disease Clinics after the Affordable Care Act. Am J Public Health. 2015;105(S5):S690–S695. doi: 10.2105/AJPH.2015.302839. http://dx.doi.org/10.2105/AJPH.2015.302839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gift TL, Haderxhanaj LT, Torrone EA, Behl AS, Romaguera RA, Leichliter JS. Estimating the Size and Cost of the STD Prevention Services Safety Net. Public Health Rep. 2014;130(6):602–609. doi: 10.1177/003335491513000608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thrun M, Shlay JC. Sexually Transmitted Disease Clinics in the Era of the Affordable Care Act: Is It Time to Tear Down the Walls? Sex Transm Dis. 2014;41(7):461–462. doi: 10.1097/OLQ.0000000000000148. http://dx.doi.org/10.1097/OLQ.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 12.Rietmeijer CA, Mettenbrink C. Why we should save our STD clinics. Sex Transm Dis. 2010;37(9):591. doi: 10.1097/OLQ.0b013e3181ed2e01. http://dx.doi.org/10.1097/OLQ.0b013e3181ed2e01. [DOI] [PubMed] [Google Scholar]
- 13.Rietmeijer CA. The pros and cons of the express visit option. Sex Transm Dis. 2013;40(1):62–63. doi: 10.1097/OLQ.0b013e31827e16ac. http://dx.doi.org/10.1097/OLQ.0b013e31827e16ac. [DOI] [PubMed] [Google Scholar]
- 14.Wong W, Johnson T, Rutledge T, Quinn L, Broad J. Developing and improving a fast track STD services program in Chicago STD clinics. 2008 National STD Prevention Conference. 2008 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


