Abstract
Objectives
The objective of this study was to describe the frequency and nature of antibiotic prescriptions issued by a primary care out-of-hours (OOH) service and compare time trends in prescriptions between OOH and in-hours primary care.
Methods
We performed a retrospective audit of 496 931 patient contacts with the Oxfordshire OOH primary care service. Comparison of time trends in antibiotic prescriptions from OOH primary care and in-hours primary care for the same population was made using multiple linear regression models fitted to the monthly data for OOH prescriptions, OOH contacts and in-hours prescriptions between September 2010 and August 2014.
Results
Compared with the overall population contacting the OOH service, younger age, female sex and patients who were less deprived were independently correlated with an increased chance of a contact resulting in prescription of antibiotics. The majority of antibiotics were prescribed to patients contacting the service at weekends. Despite a reduction in patient contacts with the OOH service [an estimated decrease of 486.5 monthly contacts each year (95% CI −676.3 to −296.8), 5.0% of the average monthly contacts], antibiotic prescriptions from this service rose during the study period [increase of 37.1 monthly prescriptions each year (95% CI 10.6–63.7), 2.5% of the average monthly prescriptions]. A matching increase was not seen for in-hours antibiotic prescriptions; the difference between the year trends was significant (Z test, P = 0.002).
Conclusions
We have demonstrated trends in prescribing that could represent a partial displacement of antibiotic prescribing from in-hours to OOH primary care. The possibility that the trends we describe are evident nationally should be explored.
Introduction
Antimicrobial resistance is associated with both poorer patient outcomes and increased healthcare costs.1,2 Since antimicrobial consumption is a major driver of antimicrobial resistance,3 ensuring that antibiotics are prescribed only where clinically appropriate is key to successful antimicrobial stewardship. Whilst incidence of antimicrobial resistant infection continues to rise, total antibiotic prescribing (measured using daily defined doses) has risen too.4 As the largest contributor to medical antimicrobial prescribing in the UK (74% of antibiotics in 2014),4 general practice has a key role to play in antimicrobial stewardship. Although primary care antibiotic consumption has increased in terms of daily defined doses, the total levels of antibiotic prescription items prescribed per patient have started to decrease in the past 2 years (suggesting that the amount of antibiotic given per course has increased by either duration or dosage).4 What is unclear, however, is the contribution of out-of-hours (OOH) primary care to this problem.
OOH services are an integral part of primary care provision in the UK, providing primary care outside of ‘core’ contracted hours during weekday evenings and nights and on weekends and bank holidays. In 2013–14, OOH primary care in England handled around 5.8 million cases, 3.3 million of which were face-to-face consultations, including 800 000 home visits.5 Patients presenting to OOH primary care are more likely to present with serious illness,6 a context in which antibiotic prescribing may be integral to good patient care. In addition, greater use of telephone consultations may affect antibiotic prescribing practices.7 Over-prescribing of antibiotics according to national guidelines has been reported in the Dutch OOH service,8 but little is known about antibiotic prescribing practices in OOH services in the UK. Concerns exist that governmental drives to decrease antimicrobial prescribing in in-hours primary care may displace antibiotic prescribing to the OOH service, but there is, as yet, little evidence to substantiate these fears.
This descriptive study of an OOH service in Oxfordshire, UK, analyses 4 years of antibiotic prescribing data. We compared antibiotic prescribing data from the Oxfordshire OOH service with in-hours antibiotic prescriptions for the same geographical population. We aimed to describe the demographics of antibiotic prescribing in the OOH service and to explore relationships between in-hours and OOH antibiotic prescribing over time.
Methods
In an Oxford Health NHS Foundation Trust service evaluation, a database of all patients presenting to the Oxfordshire OOH service over the 4 years from June 2010 to August 2014 was created from the electronic medical record used by OOH clinicians (SystmOne). Patients without an NHS number were excluded. All patient identifiers were removed upon entry to the database. Antibiotics were defined as all medications listed for bacterial infections within the Oxfordshire primary care antimicrobial prescribing guidelines.9 Service data included call volume and time period. Days of the week were calculated using calendar days beginning at midnight and timings of contacts were classified as follows: ‘evening’, 19:00–00:00; ‘overnight’, 00:01–08:00; and ‘daytime’, 08:01–18:59 (weekends and bank holidays). The Oxfordshire OOH service reported no significant changes in the population served (∼600 000 patients) over the 4 years of the study.
Indications for antibiotic prescription were derived from codes indicating the clinical problem. These are attached to each contact by the consulting physician at the end of the contact and are limited to codes available in the SystmOne operating system. Index of multiple deprivation (IMD) scores were derived from the patient's postcode10 and compared with deciles constructed from the IMD scores of all patient contacts with the OOH service over the same time period in order to compare deprivation levels with the local population. Data analysis was performed using SPSS Version 22.
Comparison of trends in antibiotic prescriptions in-hours and OOH
Data on in-hours dispensed prescriptions by general practitioner (GP) surgeries in Oxfordshire for September 2010–August 2014 were obtained from the Oxfordshire Clinical Commissioning Group, with the total monthly prescriptions summed across all listed general practices.
We aimed to extract information on the underlying prescribing trends over time, in both in-hours and OOH general practice, accounting for seasonal variations and with corrections for weekends and bank holidays and random fluctuations. As such, multiple linear regression models were fitted to the monthly data for OOH prescriptions, OOH contacts and in-hours prescriptions between September 2010 and August 2014 (three different response variables). The models assumed linear trends in year averages (defined as September–August), consistent adjustments away from the year average for each different month of the year and discrete corrections for the number of weekend days and the number of bank holidays (all included as explanatory variables). Model fitting was assessed using goodness-of-fit measures and residual error diagnostics and individual variable significance was judged by coefficient significance. We also determined whether there was a change in the antibiotic prescribing rate before and after the introduction of the ‘111 service’ (which standardized telephone triage and may have altered the case mix of patients subsequently treated in OOH primary care).
For linear regression models with different response scales and ranges, it is not possible to compare the statistical significance of variable coefficients directly between models. For example, the range of OOH prescribing is 1017–2342 items per month, whilst the range of in-hours prescribing is 26 180–42 490. Hence, additional models were fitted for standardized OOH prescriptions and standardized in-hours prescriptions. Standardization consisted of subtracting the variable mean and then dividing by the standard deviation and allows comparison of variable coefficients between independent models on a more appropriate, unit-less scale.11 Linear regression data analysis was performed using R (Version 3.2.2).
Ethics
Ethics approval was not required for this study. Oxford Health NHS Foundation Trust evaluated the protocol and prospectively approved the work as a service evaluation and quality improvement project, conducted by G. N. H., who was part of the direct care team.
Results
Between June 2010 and August 2014 there were 496 931 contacts with the OOH service in Oxfordshire (excluding 14 572 contacts without an NHS number). A total of 77 148 antibiotic prescriptions were issued at 74 739 contacts during this period. The proportion of contacts resulting in a prescription of antibiotics was 15%. There were 2384 patient contacts (0.5%) where two antibiotics were issued and 25 contacts where three antibiotics were issued.
Demographics
The median age of all patient contacts with the OOH service during this period was 35, with an IQR of 13–66. In contrast, the median age of patient contacts resulting in an antibiotic prescription was 30, with an IQR of 9–52. Table 1 compares the ages of the overall patient contacts with the OOH service with the ages of those contacts resulting in antibiotic prescription.
Table 1.
Age comparison between overall patient contacts with the OOH service and the patient contacts resulting in an antibiotic prescription
| Age (years) | Number of OOH contacts (% of all contacts) | Number of contacts resulting in an antibiotic prescription (% of all prescription contacts) | Percentage of all contacts resulting in an antibiotic prescription |
|---|---|---|---|
| 0–4 | 87 315 (17.6) | 14 434 (19.3) | 16.5 |
| 5–17 | 51 039 (10.3) | 10 519 (14.1) | 20.6 |
| 18–59 | 215 585 (43.4) | 36 138 (48.4) | 16.8 |
| 60+ | 142 992 (28.7) | 13 648 (18.3) | 9.5 |
| All ages | 496 931 | 74 739 | 15.0 |
Of the patient contacts where antibiotics were prescribed, 60.8% were for females and 39.2% were for males. This was a higher proportion of females than the overall population contacting the OOH service (58.3% female, 41.7% male).
IMD scores10 for the home address of patients presenting to the OOH service who were prescribed antibiotics were grouped by local deciles of deprivation (lower decile = less deprived) and are shown in Figure 1. In a multivariable logistic regression, younger age, female sex and lower deprivation were independently correlated with an increased likelihood of a contact with the OOH service resulting in prescription of antibiotics (age: OR = 0.990, 95% CI 0.989–0.990, P < 0.001; sex: OR = 0.814, 95% CI 0.800–0.827, P < 0.001; IMD: OR = 0.995, 95% CI 0.994–0.996, P < 0.001).
Figure 1.
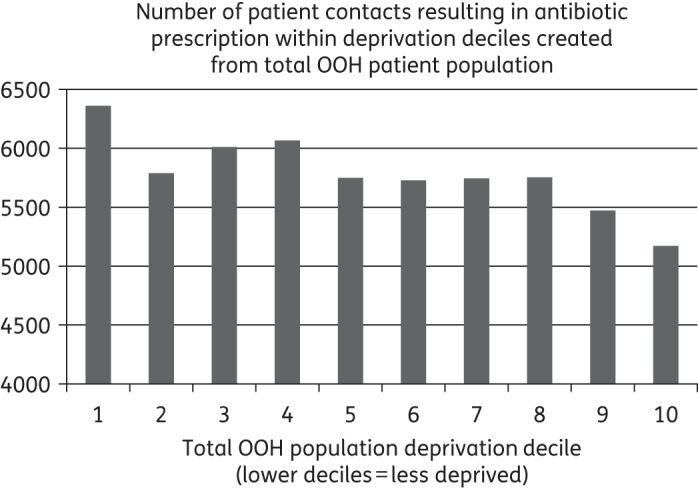
IMD scores of patients prescribed antibiotics by the OOH service.
Repeat antibiotic prescriptions
The majority of patients receiving antibiotics OOH had only 1 contact resulting in a prescription in the 4 years of the study (61 260, 82%); 9708 (13%) had 2 contacts resulting in antibiotic prescriptions and 3770 (5%) had ≥3 separate antibiotic prescriptions from the service (range 3–17).
Timing of antibiotic prescriptions
Antibiotics were prescribed at 19.9% of all daytime contacts (including weekends and bank holidays), 8.2% of all evening contacts and 8.7% of all overnight contacts. Thus, the majority (76.4%) of antibiotic prescriptions were issued during daytime hours (16.5% in the evenings and 7.1% overnight). Most antibiotics (44%) were issued on Saturday; 31.2% were issued on Sundays. The monthly OOH prescriptions and contacts and in-hours prescriptions data are shown in Figure 2. OOH antibiotic prescriptions and contact rates appeared to follow similar seasonal trends over the period of the study with a primary peak in December and one or two secondary peaks in the spring (between March and June). In comparison, the seasonal trend for in-hours prescriptions more closely matched a single yearly cycle with a peak in winter and an approximate trough in summer.
Figure 2.

Monthly data for OOH prescriptions and contacts and in-hours prescriptions in Oxfordshire.
What is being prescribed
The most commonly prescribed antibiotics were penicillins, with amoxicillin accounting for 28.2% of total antibiotic prescriptions, and flucloxacillin and phenoxymethylpenicillin accounting for 13.7% and 11.9% of total antibiotic prescriptions, respectively.
Amoxicillin was the most frequently prescribed antibiotic in all age groups, with 8.5% of contacts resulting in a prescription in children aged 0–4 years. However, the top five most frequent prescriptions differed between age groups. Chloramphenicol and erythromycin only featured in the top five for young children. Antibiotics targeting urinary infection were in the top five for adults and older adults. Penicillin V, which is only used first line for acute tonsillitis, was in the top five for all age groups except older adults. Table 2 shows the distribution of antibiotic prescriptions by age group and antibiotic.
Table 2.
Number of antibiotic prescriptions issued by OOH primary care by age group and antibiotic name
| 0–4 years |
5–17 years |
18–59 years |
60+ years |
N (total) | Per 1000 contacts across all age groups | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | per 1000 contacts | N | per 1000 contacts | N | per 1000 contacts | N | per 1000 contacts | |||
| Amoxicillin | 7434 | 85.14 | 3451 | 67.61 | 8103 | 37.59 | 2793 | 19.53 | 21 781 | 43.83 |
| Azithromycin | 0 | 0 | 9 | 0.18 | 101 | 0.47 | 32 | 0.22 | 142 | 0.29 |
| Benzylpenicillin | 0 | 0 | 2 | 0.04 | 5 | 0.02 | 0 | 0 | 7 | 0.01 |
| Cefalexin | 232 | 2.66 | 296 | 5.80 | 1353 | 6.28 | 634 | 4.43 | 2515 | 5.06 |
| Cefuroxime | 1 | 0.01 | 3 | 0.06 | 0 | 0 | 0 | 0 | 4 | 0.01 |
| Chloramphenicol | 1651 | 18.91 | 475 | 9.31 | 1282 | 5.95 | 425 | 2.97 | 3833 | 7.71 |
| Ciprofloxacin | 0 | 0 | 21 | 0.41 | 373 | 1.73 | 251 | 1.76 | 645 | 1.29 |
| Clarithromycin | 182 | 2.08 | 154 | 3.02 | 898 | 4.17 | 389 | 2.72 | 1623 | 3.27 |
| Clindamycin | 0 | 0 | 4 | 0.08 | 95 | 0.44 | 39 | 0.27 | 138 | 0.28 |
| Co-amoxiclav | 745 | 8.53 | 917 | 17.97 | 4811 | 22.31 | 1880 | 13.15 | 8353 | 16.81 |
| Doxycycline | 0 | 0 | 25 | 0.49 | 628 | 2.91 | 186 | 1.3 | 839 | 1.68 |
| Erythromycin | 1340 | 15.35 | 763 | 14.95 | 1592 | 7.38 | 458 | 3.2 | 4153 | 8.36 |
| Flucloxacillin | 925 | 10.59 | 1394 | 27.31 | 6380 | 29.59 | 1875 | 13.11 | 10 574 | 21.28 |
| Lymecycline | 0 | 0 | 1 | 0.02 | 8 | 0.04 | 1 | 0.01 | 10 | 0.02 |
| Metronidazole | 8 | 0.09 | 44 | 0.86 | 1010 | 4.68 | 230 | 1.61 | 1292 | 2.59 |
| Nitrofurantoin | 10 | 0.11 | 202 | 3.96 | 3050 | 14.15 | 1611 | 11.27 | 4873 | 9.81 |
| Ofloxacin | 0 | 0 | 1 | 0.02 | 32 | 0.15 | 0 | 0 | 33 | 0.07 |
| Phenoxymethylpenicillin | 1934 | 22.15 | 2339 | 45.83 | 4656 | 21.60 | 236 | 1.65 | 9165 | 18.44 |
| Rifampicin | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0.02 | 3 | 0.01 |
| Trimethoprim | 370 | 4.24 | 656 | 12.85 | 3626 | 16.82 | 2505 | 17.51 | 7157 | 14.40 |
| Vancomycin | 0 | 0 | 0 | 0 | 3 | 0.01 | 5 | 0.03 | 8 | 0.02 |
| Totals | 14 832 | 10 757 | 38 006 | 13 553 | 77 148 | |||||
Bold text indicates the top five most frequently prescribed antibiotics for each age group and overall.
Organ systems clinically coded as associated with antibiotic prescriptions
Primary codes relating to four different organ systems accounted for >80% of the contacts that resulted in antibiotic prescription. These were: ‘Ophthalmic or ENT’ (17 247 contacts, 23%), ‘Genito-Urinary’ (15 835 contacts, 21%), ‘Respiratory’ (15 018, 20%) and ‘Dermatology or Local Infection’ (13 020 contacts, 17%).
Trends in antibiotic prescribing: comparison of in-hours and OOH
The fitting of linear regression models to the data for Oxfordshire OOH antibiotic prescriptions and patient contacts and in-hours antibiotic prescriptions is shown in Figure 3, with the details given in Table 3 and Table S1 (available as Supplementary data at JAC Online). Overall goodness of fit was satisfactory for all models, with 85%–90% of variation in the data explained by the models. Patient contacts with the OOH service reduced over the 4 year period; a statistically significant year trend was fitted with an estimated decrease of 486.5 monthly contacts each year (95% CI −676.3 to −296.8). This corresponds to 5.0% of the average number of monthly OOH contacts. Despite this decrease in contacts, antibiotic prescriptions from the OOH service rose during the study period; a statistically significant year trend was fitted, with an estimated increase of 37.1 monthly prescriptions each year (95% CI 10.6–63.7), 2.5% of the average number of monthly OOH prescriptions. Over the 3 years from 2010–11 to 2013–14, this would correspond to a 7.7% (95% CI 2.2–13.2) increase in antibiotic prescribing. A matching increase was not seen for in-hours antibiotic prescriptions; the year trend was non-significant, with an estimated decrease of 294.0 antibiotic prescriptions per month (95% CI −701.1 to 113.0).
Figure 3.
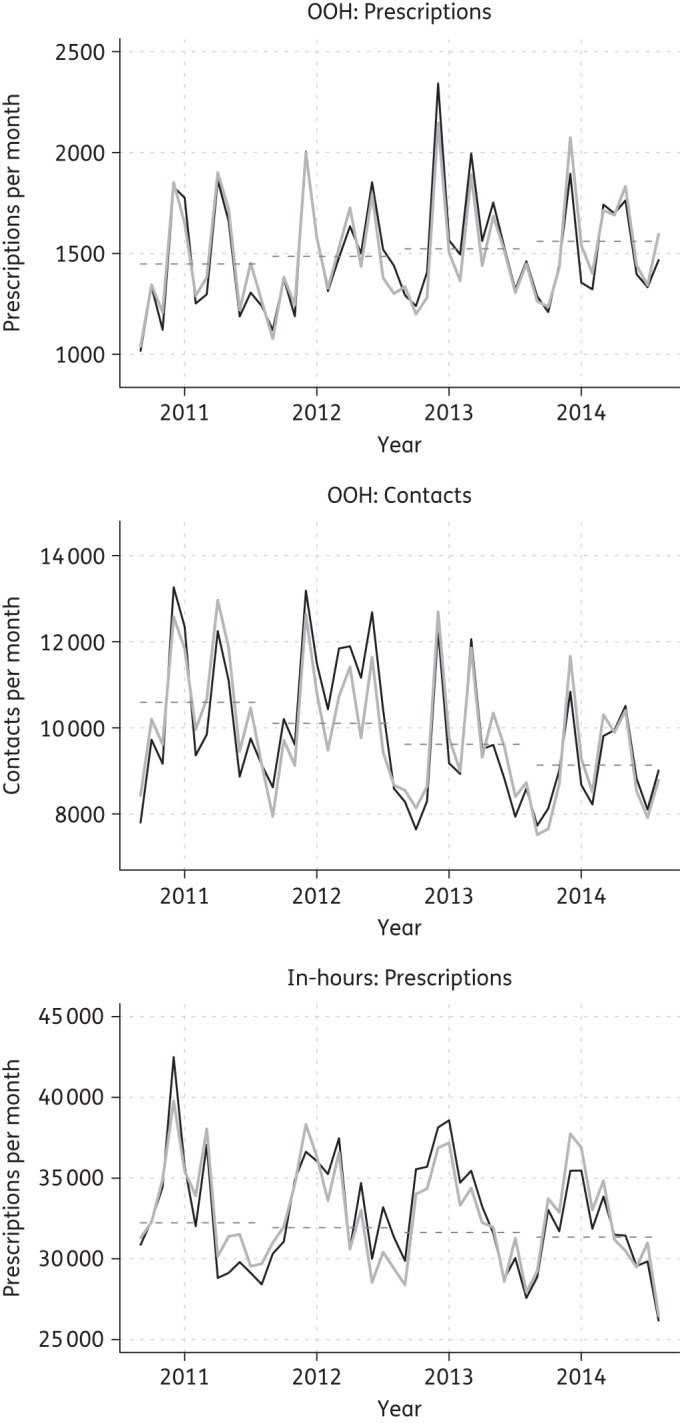
OOH monthly prescriptions and contacts and in-hours monthly prescriptions for Oxfordshire between September 2010 and August 2014. Black continuous lines correspond to the observed data. Grey continuous lines correspond to the fitted regression models. Grey broken lines represent the modelled change in the yearly averages.
Table 3.
Linear regression model details
| Response variable | Explanatory variables | Coefficient (standard error) | 95% CI | P |
|---|---|---|---|---|
| OOH prescriptions (R2 = 0.90) | year | 37.1 (13.1) | 10.6 to 63.7 | 0.008 |
| weekend days | 110.3 (20.7) | 68.3 to 152.3 | <0.001 | |
| bank holidays | 212.5 (40.2) | 130.6 to 294.4 | <0.001 | |
| (intercept, months†) | — | — | — | |
| OOH contacts (R2 = 0.85) | year | −486.5 (93.3) | −676.3 to −296.8 | <0.001 |
| weekend days | 545.5 (147.6) | 245.2 to 845.7 | <0.001 | |
| bank holidays | 1062.6 (287.6) | 477.5 to 1647.7 | <0.001 | |
| (intercept, months†) | — | — | — | |
| In-hours prescriptions (R2 = 0.85) | year | −294.0 (200.1) | −701.1 to 113 | 0.151 |
| weekend days | −1162.8 (316.5) | −1806.8 to −518.8 | <0.001 | |
| bank holidays | −758.5 (616.9) | −2013.5 to 496.6 | 0.228 | |
| (intercept, months†) | — | — | — | |
| Standardized OOH prescriptions (R2 = 0.90) | year | 0.137 (0.048) | 0.039 to 0.234 | 0.008 |
| (intercept, months, weekend days, bank holidays†) | — | — | — | |
| Standardized in-hours prescriptions (R2 = 0.85) | year | −0.087 (0.059) | −0.208 to 0.034 | 0.151 |
| (intercept, months, weekend days, bank holidays†) | — | — | — |
Coefficients correspond to changes in monthly prescription/contact numbers.
Model goodness of fit is given by R2 values.
All models had at least one significant month coefficient (P < 0.05).
†Details for these variables are given in Table S1.
Using the year coefficients and standard errors from the models fitted to the standardized prescription data (given in Table 3), the difference between the year trend for OOH and in-hours prescriptions was significant (Z test,12 P = 0.002).
The trend in OOH prescription proportion (antibiotic prescriptions per contact) was explored, specifically to assess any impact of the introduction of the 111 service, which began in July 2012. This suggested an increase in the number of prescriptions per OOH contact from the first 2 years of the data (0.138 prescriptions per contact for September 2010 to August 2012) to the last 2 years of the data (0.168 prescriptions per contact for September 2012 to August 2014) (Figure 4 and Table 4).
Figure 4.
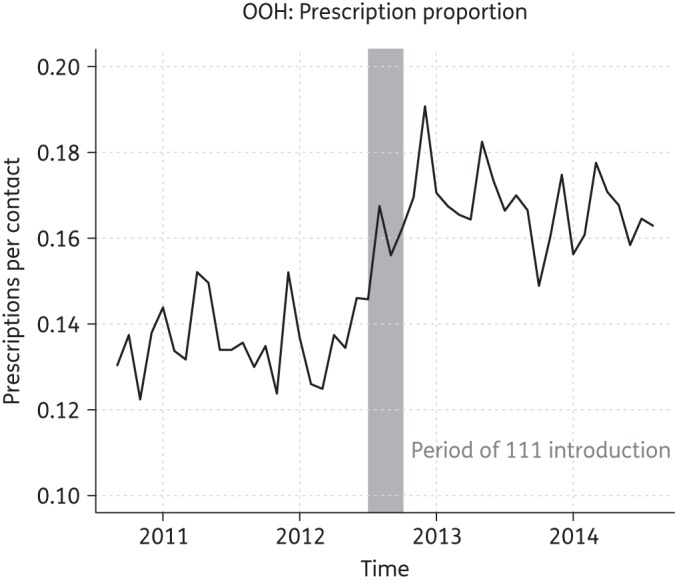
Changes in the OOH prescription proportion. The grey region corresponds to the introduction of the NHS 111 service in Oxfordshire.
Table 4.
Changes in the OOH prescription proportion over the time span of the data
| Prescription proportion | 95% CI | |
|---|---|---|
| September 2010–August 2011 | 13.8% | 13.6%–14.0% |
| September 2011–August 2012 | 13.8% | 13.6%–14.0% |
| September 2012–August 2013 | 17.0% | 16.8%–17.3% |
| September 2013–August 2014 | 16.4% | 16.2%–16.7% |
CIs were calculated assuming a binomial distribution.
Discussion
We did not observe a significant change in the total number of antibiotic prescriptions dispensed in Oxfordshire over the last 4 years. However, over the same time period we found an increase in issued antibiotic prescriptions in the OOH service, despite a slight reduction in OOH patient contacts, a trend that was significantly different from the in-hours data. The fitted increase in annual OOH antibiotic prescribing corresponds to 446 (95% CI 127–764) additional prescriptions each year.
Antibiotics were prescribed in 15% of all contacts with OOH primary care. Younger age, female sex and lower deprivation score were all independently correlated with an increased chance of a contact with the OOH service resulting in prescription of antibiotics. Amoxicillin was the most frequently prescribed antibiotic across all age groups. Almost 75% of antibiotic prescriptions issued by the OOH service were dispensed at weekends.
Strengths and limitations
To the best of our knowledge this is the first UK-based evaluation of antibiotic prescribing in OOH primary care and the first to compare trends over time with in-hours primary care antibiotic prescribing. Our study benefits from the robustness of the dataset used. However, limitations of the electronic record constrained our ability to analyse the type of consultation in which antibiotics were prescribed. Furthermore, our data on antibiotic prescribing from the OOH service consist of issued prescriptions, whereas our in-hours prescribing data are based on dispensed prescriptions, which may have resulted in additional ‘delayed’ antibiotic prescriptions counting towards the total in OOH, but not in-hours, time trends. However, this is unlikely to affect the overall trends observed. Finally, limitations of both in-hours and OOH data meant that we could not formulate prescribing as daily defined doses or compare the proportion of broad-spectrum antibiotics prescribed in each group. Recent evidence4 suggests that these measures are increasing in primary care despite a reduction in overall number of prescriptions issued.
Our modelling of time trends in antibiotic prescribing assumed that the monthly prescription data were independent observations and that their variation could be adequately described by the linear regression models outlined in the Methods section. Most notably, linear year trends were included in the models for interpretation purposes—assuming a constant change in the prescription numbers each year. However, not unexpectedly, the data exhibited some deviation away from this ideal behaviour. For example, the fitted values (grey continuous lines in Figure 3) for OOH contacts were consistently below the observed figures (black continuous lines) for the second year of the data. Whilst model fitting could be improved slightly by allowing non-linear year trends, the overall fit of the models was sufficient to retain the linear year trends as this facilitated interpretation and does not alter the overall conclusions of the analysis.
Comparison with other literature
A retrospective Danish study describing antibiotic prescribing practices in their OOH primary care service reported an identical 15% of contacts resulting in antibiotic prescription.7 Increased frequency of antibiotic prescribing amongst the young and women is consistent with previously observed trends in in-hours antibiotic prescribing.13 A recent European evaluation of paediatric outpatient antibiotic prescribing confirmed our finding that rates of antibiotic prescribing were highest in children aged under 414 and showed that rates were similar in Denmark and the UK.
Our finding that patients receiving antibiotics from OOH were relatively less deprived than the overall population contacting the service is in contrast with a recent suggestion that in-hours GPs in the UK prescribe more antibiotics in more deprived areas,15 but in line with research from the USA suggesting that children from low-income homes are less likely to use antibiotics.16 The reasons for this trend are unclear and could relate to issues of access17 or to patient expectations when attending an urgent care service.
We noted a decrease in overall contacts with the OOH service during the study period and an increase in the proportion of contacts resulting in an antibiotic prescription. Since this proportion increased most markedly after the summer of 2012, it is plausible that this is related to the introduction of the ‘NHS 111’ service, a central telephone triage service for healthcare needs outside office hours, which began in Oxfordshire in a limited form in July 2012 and was fully introduced in October 2012. This is consistent with an overall national trend for a reduction in the number of OOH contacts since the introduction of the NHS 111 service.5 It is possible that pre-triaging patients could have resulted in lower overall contacts, but increased morbidity, in the population assessed. To our knowledge there have been no evaluations of the impact of introducing the 111 service on the severity of illness in patients contacting OOH care.
Implications
‘Antimicrobial stewardship’ encourages a focus not just on absolute reduction in number of antibiotic prescriptions issued, but also on ensuring that when an antibiotic is needed, an appropriate one is prescribed, for an appropriate duration. This study was not designed to test compliance of GP prescribers with local antibiotic guidelines, though we note that almost 4000 prescriptions for topical chloramphenicol were issued (4.97% of all antibiotic prescriptions). As acute conjunctivitis can usually be considered a self-limiting condition18 this may provide a targeted opportunity for reducing antibiotic prescribing within the service. More than 2% of all patient contacts resulted in a prescription of co-amoxiclav. The use of broad-spectrum antibiotics is a concern as it is thought to result in greater levels of resistance.19 These levels might suggest that patients are contacting OOH when they feel their initial antibiotic prescription has failed, as guidelines would suggest this is usually a second-line prescription.
We have demonstrated trends in prescribing that could represent a partial displacement of antibiotic prescribing from in-hours to OOH, e.g. due to patients' antibiotic-seeking behaviour after refusal by the in-hours GP. The significant increase in prescriptions in Oxfordshire—a fitted absolute increase of 446 (95% CI 127–764) prescriptions each year—would be equivalent to 43 600 (95% CI 12 400–74 800) annually if we assume this is a national trend. However, there are a number of alternative explanations for higher prescribing, including the increased prevalence of serious pathology in the population attending OOH,6 lower thresholds for prescribing by OOH clinicians who do not have access to previous history or the ability to follow up the patient and a lack of targets or incentives for reducing antimicrobials imposed by the government or local commissioners. If antibiotic prescribing is being displaced, this may be appropriate: in a system that restricts antibiotic prescribing in-hours, the OOH service could act as a safety net offering antibiotics to the smaller percentage where they would be of benefit. However, if this is the case then it is important to consider the implications in terms of access to the service by more-deprived patient groups.
Future directions
National antimicrobial prescribing data for OOH services are not available, but our analysis suggests there would be merit in examining this more closely across a range of OOH service providers to see whether the trends we describe are generalized across the UK. A detailed assessment of the diagnoses and the severity of presenting illness in those patients prescribed antibiotics OOH would help to contextualize any potential difference in prescribing rates. In the absence of data from other services we are unable to set our figure of antibiotic prescription in 15% of contacts with the OOH service within any broader context. We do suggest, however, that this context is needed. Effective strategies to tackle antimicrobial resistance require targeting—and that would best be achieved by a nuanced understanding of prescribing behaviour across sectors.
Funding
This study was conducted as part of our routine work. G. N. H. was funded by a National Institute of Health Research (NIHR) Academic Clinical Fellowship and Academic Clinical Lectureship whilst working on this study. D. S. L. is funded by the NIHR Oxford Biomedical Research Centre and NIHR Oxford Collaboration for Leadership in Applied Health Research and Care (CLAHRC). R. F. R. F. is funded by an NIHR Academic Clinical Fellowship. G. T. S. is funded by the NIHR Trainees Coordinating Centre (Research Methods Fellowship).
No additional funding was sought for this study. This paper represents independent research and the views expressed here are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Transparency declarations
None to declare.
Supplementary data
Table S1 is available as Supplementary data at JAC Online (http://jac.oxfordjournals.org/).
Acknowledgements
We would like to acknowledge the input and assistance of Ms Helen Hunt, Urgent and Ambulatory Care Service Clinical Lead for Oxford Health NHS Foundation Trust, in this project.
References
- 1.Cosgrove SE. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin Infect Dis 2006; 42 Suppl 2: S82–9. [DOI] [PubMed] [Google Scholar]
- 2.Butler CC, Hillier S, Roberts Z et al. . Antibiotic-resistant infections in primary care are symptomatic for longer and increase workload: outcomes for patients with E. coli UTIs. Br J Gen Pract 2006; 56: 686–92. [PMC free article] [PubMed] [Google Scholar]
- 3.Costelloe C, Metcalfe C, Lovering A et al. . Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 2010; 340: 2096. [DOI] [PubMed] [Google Scholar]
- 4.PHE. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/477962/ESPAUR_Report_2015.pdf.
- 5.National Audit Office. Out-of-Hours GP Services in England. London: Department of Health and NHS England, 2014. [Google Scholar]
- 6.Huibers LA, Moth G, Bondevik GT et al. . Diagnostic scope in out-of-hours primary care services in eight European countries: an observational study. BMC Fam Pract 2011; 12: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huibers L, Moth G, Christensen MB et al. . Antibiotic prescribing patterns in out-of-hours primary care: a population-based descriptive study. Scand J Prim Health Care 2014; 32: 200–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willekens M, Giesen P, Plat E et al. . Quality of after-hours primary care in The Netherlands: adherence to national guidelines. BMJ Qual Saf 2011; 20: 223–7. [DOI] [PubMed] [Google Scholar]
- 9.Oxfordshire Clinical Commissioning Group. Oxfordshire Adult Antimicrobial Prescribing Guidelines for Primary Care. 2012. http://www.oxfordshireccg.nhs.uk/wp-content/uploads/2013/08/Oxfordshire-ADULT-Antimicrobial-Prescribing-Guidelines-for-Primary-Care.pdf.
- 10.Department for Communities and Local Government. English Indices of Deprivation 2015. London, 2015. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015. [Google Scholar]
- 11.Bring J. How to standardize regression coefficients. Am Stat 1994; 48: 209–13. [Google Scholar]
- 12.Paternoster R, Brame R, Mazerolle P et al. . Using the correct statistical test for the equality of regression coefficients. Criminology 1998; 36: 859–66. [Google Scholar]
- 13.Majeed A, Moser K. Age-and sex-specific antibiotic prescribing patterns in general practice in England and Wales in 1996. Br J Gen Pract 1999; 49: 735–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Holstiege J, Schink T, Molokhia M et al. . Systemic antibiotic prescribing to paediatric outpatients in 5 European countries: a population-based cohort study. BMC Pediatr 2014; 14: 174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wise J. Antibiotic prescribing is higher in deprived areas of England. BMJ 2015; 351: h6117. [DOI] [PubMed] [Google Scholar]
- 16.Sarpong EM, Miller GE. Narrow- and broad-spectrum antibiotic use among U.S. children. Health Serv Res 2015; 50: 830–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marmot M, Allen J, Goldblatt P et al. . Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010. http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot-review.
- 18.Jefferis J, Perera R, Everitt H et al. . Acute infective conjunctivitis in primary care: who needs antibiotics? An individual patient data meta-analysis. Br J Gen Pract 2011; 61: e542–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rao GG. Risk factors for the spread of antibiotic-resistant bacteria. Drugs 1998; 55: 323–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


