Abstract
Background:
This study was done to evaluate remineralizing potential of bioactive glasses (BAGs) and amorphous calcium phosphate-casein phosphopeptide (ACP-CPP) on early enamel lesion.
Materials and Methods:
Twenty freshly extracted mandibular premolars were sectioned sagittally. The buccal half was impregnated in acrylic resin blocks and treated with 37% phosphoric acid in liquid form, to demineralize enamel surface to simulate early enamel lesion. The samples were divided into two groups. The samples in Group I were treated with ACP-CPP (GC Tooth Mousse) and in Group II with BAG (Sensodyne Repair and Protect) and stored in saliva to prevent dehydration. The samples were tested for microhardness. The data obtained was analyzed using ANOVA post hoc multiple comparison and independent sample t- test and presented as a mean and standard deviation.
Results:
All the samples showed a decrease in the microhardness after demineralization. After application of remineralizing agents, Group II showed a highly significant increase in the microhardness (P < 0.05) after 10 days, while Group I showed a significant increase in microhardness after 15 days (P < 0.05).
Conclusion:
Both the remineralizing agents tested in this study can be considered effective in repair and prevention of demineralization. BAG showed better results initially, but eventually both have similar remineralizing potential.
Key Words: Casein phosphopeptide-amorphous calcium phosphate nanocomplex, NovaMin, enamel, remineralization, hardness, number
INTRODUCTION
Tooth enamel is the highest mineralized tissue of the body. It is mainly composed of 96% inorganic material, 4% being organic material and water. A specific population of bacteria which has the capacity to demineralize enamel in the oral cavity under a modified environment results in the early carious lesion. When air dried, this demineralized enamel appears as a white opaque spot.
The oral fluid mainly comprising of saliva and gingival crevicular fluid is rich in calcium, phosphate and fluoride ions. This results in a dynamic equilibrium between the mineral content of tooth and oral fluid in a neutral pH. In conditions when the pH is neutral, there is the minimal dissolution of hydroxyapatite crystals releasing calcium (Ca2+), phosphate (PO43−) and hydroxyl (OH−) ions that are already present in the oral fluid. Increase in Ca2+, and PO43− ions in the oral fluid lead to supersaturation of the solution and precipitation of the minerals back onto the tooth surface that can be termed as remineralization.
In conditions when the pH of the oral fluid is acidic especially at or below 5.5 termed as critical pH, it becomes undersaturated with respect to phosphate ions (PO43−). This results in dissolution of hydroxyapatite crystals from the tooth to resaturate the oral fluid, which is termed as demineralization.[1]
To restore the natural equilibrium, either remineralization must be enhanced, or demineralization must be retarded. Using enhanced remineralizing treatment, the early enamel lesion can be remineralized, with an increase in resistance to further challenge.
Casein phosphopeptide (CPP) is a phsophopeptide obtained from milk protein casein that contains phosphoseryl sequences and stabilizes the calcium phosphate in nanocomplexes. CPP prevents dissolution of calcium and phosphate ions by binding with amorphous calcium phosphate (ACP).[2] The ACP-CCP solution is supersaturated and provides Ca2+ and PO42− ions for remineralization. It has been shown in both in vivo and in vitro studies that ACP-CPP can remineralize the enamel subsurface lesion.[3,4]
To prevent demineralization or to aid in remineralization, calcium sodium phosphatesilicate bioactive glass (BAG) (Novamin) has been introduced. Calcium sodium phosphosilicate disintegrates and gives off sodium that gets exchanged with hydrogen cations (H+ or H3O+) when it comes in contact with saliva results in the release of calcium (Ca2+) and phosphate (PO42−) ions from the particle structure.[5,6,7] There is a transient increase in pH that brings about the precipitation of calcium and phosphate ions from saliva and the particles to form a calcium phosphate layer on the tooth surfaces. Ca-P complexes crystallizes to form hydroxycarbonate apatite that is chemically and structurally similar to biological apatite.[5,8]
This in vitro study was taken up to evaluate the remineralizing potential of BAGs and ACP-CPP on early enamel lesions.
MATERIALS AND METHODS
The present study was conducted in the Department of Conservative Dentistry and Endodontics, Army College of Dental Sciences, Secunderabad in collaboration with Defence Metallurgical Research Laboratory, Hyderabad and Department of Health Research, National Institute of Nutrition.
The materials used in the study
ACP-CPP (GC Tooth Mousse, Recaldent; GC Corp.; Japan)
BAG (Novamin, Sensodyne Repair and Protect; GlaxoSmithKline; UK)
37% phosphoric acid; Ivoclar Vivadent
Natural saliva
Deionized water.
Equipment used for testing
Vickers microhardness tester (Leica VMHT Auto; Germany).
PREPARATION OF SPECIMENS
Twenty freshly extracted noncarious mandibular premolars were selected. The teeth were cut sagittally using diamond disc (Horico-Horico; New Jersey, USA) and the buccal surfaceswere mounted in cold cure acrylic resin facing upwards. Using wax molds the resins blocks were made (10 × 10 × 10). A total of twenty specimens were made, which were then kept in natural saliva to prevent dehydration.[9] The samples were rinsed in water and dabbed dry with absorbent paper before subjecting them for baseline hardness test.
PROCEDURE FOR MICROHARDNESS TEST
For microhardness testing the “Leica VMHT Auto; Germany” was used for measuring Vickers hardness test. The tests were carried out according to the manufacturer's instructions.[10] The test specimens were placed on the stage of the tester and stabilized. Then area to indent was selected by focusing with 10x objective lens. After this, the test was carried out where the indentations were made with a rate of l00 g load for 30 s.[11] The indentation formed was viewed and measured on the display monitor with 10x objective lens [Figure 1]. The average microhardness of the specimen was determined from two indentations to avoid any discrepancy, since the enamel surface has a curvature. The procedure was repeated for all the twenty specimens.
Figure 1.
Microhardness indentation.
PREPARATION FOR ARTIFICIAL ENAMEL LESION
Thirty-seven percent phosphoric acid liquid was applied with an applicator and left for 20 min to demineralize the enamel surface sufficiently to simulate early enamel lesions that can be differentiated from the baseline enamel surface in its microhardness.[12] The specimens were rinsed with water and dried.
AMORPHOUS CALCIUM PHOSPHATE-CASEIN PHOSPHOPEPTIDE AND BIOACTIVE GLASS APPLICATION
ACP-CPP and BAG were applied with cotton applicator tips on demineralized tooth surface ten samples each, every day for 10 days with a minimum application time of 3 min for ACP-CPP[10] and 1 min for BAG.[13] The samples were then washed under deionized water, stored in artificial saliva for 10 days ( first cycle of remineralization) after which the samples were tested for microhardness and the values were recorded. Following this, ACP-CPP and BAG were applied for another 5 days and at the end of 15 days (second cycle of remineralization), the samples were subjected for microhardness testing using the same procedure as described earlier. Figure 1.
The data obtained from the following test were subjected for statistical analysis and were presented as a mean and standard deviation. “P” value of 0.05 or less was considered for statistical significance. The change in microhardness at different times of assessment was analyzed using ANNOVA post hoc multiple comparison test and independent sample t-test using SPSS Statistics Version 17.0. (Chicago: SPSS Inc.).
RESULTS
Table 1 shows the mean and P value change for ACP-CPP and BAG from the baseline, post demineralization cycle and 1st cycle of remineralization.
Table 1.
Mean and P value change for amorphous calcium phosphate-casein phosphopeptide and bioactive glass from the baseline, postdemineralization cycle and first cycle of remineralization
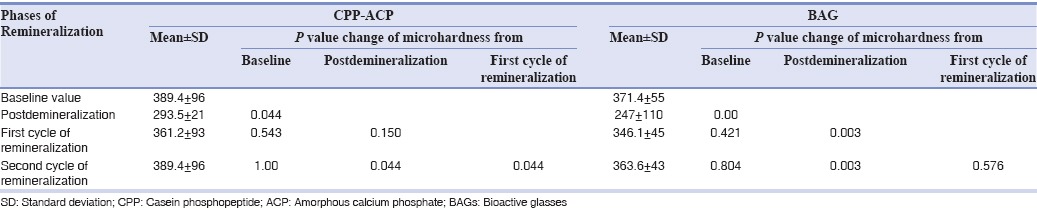
P value changes of microhardness from the baseline, when compared to postdemineralization, shows the significant result (P < 0.05) for both BAG and ACP-CPP, which shows that significant demineralization of enamel has taken place when demineralized with 37% phosphoric acid. In the same table for both the products when P value of 1st and 2nd cycle of remineralization was compared with baseline values, it was not significant representing that BAG and ACP-CPP have equated the lost mineralization equivalent to the baseline value in 10–15 days.
The P value changes of microhardness from postdemineralization cycle compared to 1st cycle of remineralization showing highly significant (P < 0.003) change for BAG comparing it to ACP-CPP shows no significant change in remineralization after 10 days of remineralization cycle. However, 2nd remineralization cycle is highly significant for BAG and showing significant value for ACP-CPP compared to postdemineralization after 15 days.
Mean, P value changes of microhardness between 1st and 2nd cycle of remineralization for BAG and ACP-CPP shows no significant change between the two cycles for each product.
Using independent sample t-test comparing BAG and ACP-CPP independently 1st and 2nd cycle of remineralization of BAG and ACP-CPP did not show any statistically significant difference (P > 0.05).
After 10 days
Average remineralization of BAG 346.15 ± 45
Average remineralization of ACP-CPP 361.20 ± 93.
After 15 days
Average remineralization of BAG 363.65 ± 65
Average remineralization of ACP-CPP 389.45 ± 45 showing P > 0.453 (NS).
DISCUSSION
As the normal translucency of the enamel is lost, the early enamel lesion appears white clinically. The surface is susceptible to damage on probing and becomes fragile. Even though initial enamel lesions have intact surfaces, they have a low mineral content at the surface layer when compared to sound enamel; thus showing a lower hardness value at the surface than for sound enamel tissue.[10,14]
Microorganisms, through their metabolic activity, produce organic acid in bacterial plaque. These acids diffuse into the surface of enamel through the pellicle and attack the vulnerable lattice points with carbonate ions in the apatite crystals.
This leads to the removal of Ca2+, OH−, PO42−, F−, CO3−, Na+ and Mg2+ from the crystal lattice and gets diffused into the solution phase in between the crystals. From the various calcium phosphate salts, calcium ions and phosphate ions dissolved and either diffuse to the exterior or provide an environment that facilitate remineralization of the faulty crystallites beneath the enamel surface.[15] As long as sufficient acid is available, demineralization or mineral loss proceeds. The concentration of the Ca+ ion and Po42− ion increases as more enamel dissolves.
As there is outward diffusion of calcium and phosphate ions, it is more likely for remineralization at the surface. This leads to the formation of about 20–40 microns intact enamel surface layer where the mineral content is greater than the body of the lesion.
In this study, 37% phosphoric acid was used for 20 min to demineralize the enamel surface simulating an early enamel lesion though the principal use of 37% phosphoric acid in dentistry is for etching the tooth surface prior to bonding for a maximum of 15–20 s.[16] Using 37% phosphoric acid for 20 min was established such that we get sufficient microhardness variation with respect to baseline value so that the subsequent remineralization could be well differentiated and compared.
As the surface layer in the carious lesion is considered important, changes in this region should be evaluated. A suitable technique for this is surface microhardness measurement. Microhardness measurement is appropriate for enamel, which has a fine nonhomogenous microstructure and is prone to cracking. Surface microhardness indentation is a rapid, simple and nondestructive and rapid method that can be used in demineralization and remineralization studies.[10] In this study, the microhardness values for specimen were measured as the baseline microhardness, after induction of carious lesion/demineralization and after remineralization.
Microhardness measurement of tooth material can be done either by Knoop's hardness number (KHN) or Vickers's hardness number (VHN). According to Chow et al.[17] both KHN and VHN have reported approximately the same value. The average hardness value for enamel is in the range of 270–350 KHN or 250 to 360 VHN.[11] In this study, the average values for enamel microhardness were in the range of 257–440 VHN with a slight variation from the standard range that could be attributed to fluoride belt in the state. A large indentation and thus a small VHN may result from any tilt on a surface which is not flat. Therefore producing a flat surface in the specimens was crucial in this study, but the cut enamel surface tested for microhardness did not have a flat surface. The convex surface gave variations in the VHN.[18] Hence, two indentations were made to avoid any operation bias, and then average of two indentations was taken for statistical analysis.
The samples were stored in natural saliva because in many studies[17,19] saliva was used for storing the specimens and it is believed that saliva contributed to a slight increase in the microhardness, after demineralization, In present study, we have tried to use natural saliva, changing it after every cycle of remineralization to simulate the oral cavity with varying pH, ions and enzymes.
The values obtained after the application of remineralizing solution for 10 days ( first cycle of remineralization) showed highly significant recovery in the microhardness (P < 0.003) for BAG while the mineral recovery was not significant for ACP-CPP (P > 0.15). After 15 days of remineralization, the mineral recovery was again highly significant for BAG (P < 0.001) and ACP-CPP has also shown significant remineralization (P < 0.044). There was no significant gain in mineralization between 1st and 2nd cycle of remineralization for BAG and ACP-CPP, respectively.
Using independent sample t- test when 1st and 2nd cycle of demineralization of BAG and ACP-CPP were compared with each other they did not show any statistically significant difference (P > 0.05).
In summary, 37% phosphoric acid decreases the enamel microhardness when it was compared with the baseline values. Both BAG and ACP-CPP were able to remineralize the tooth in 15 days almost equal to the baseline value. Although early mineral recovery postdemineralization was seen with BAG in 10 days evaluation.
CONCLUSION
Within the limits of this study BAG and ACP-CPP both act as novel agents to repair and prevent demineralization, while BAG being more effective for early remineralization; but eventually, both have similar remineralizing potential.
This study was conducted with a small number of samples utilizing in vitro conditions. Application to general population requires further research and analysis.
Furthermore, remineralization in vitro may be quite different when compared to a dynamic biological system that usually occurs in the oral cavity in vivo. Thus, direct extrapolations to clinical conditions must be exercised with caution because of obvious limitations of in vitro studies.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
REFERENCES
- 1.Usha C, Satyanarayanan R. Dental caries – A complete changeover (Part I) J Conserv Dent. 2009;12:46–54. doi: 10.4103/0972-0707.55617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reynolds EC. Additional aids to rernineralization of the tooth structure. In: Mount GJ, Hume WR, editors. Preservation and Restoration of Tooth Structure. 2nd ed. Brisbane, Australia: Knowledge Books and Software; 2005. pp. 111–8. [Google Scholar]
- 3.Reynolds EC. Remineralization of enamel subsurface lesions by casein phosphopeptide-stabilized calcium phosphate solutions. J Dent Res. 1997;76:1587–95. doi: 10.1177/00220345970760091101. [DOI] [PubMed] [Google Scholar]
- 4.Cai F, Shen P, Morgan MV, Reynolds EC. Remineralization of enamel subsurface lesions in situ by sugar-free lozenges containing casein phosphopeptide-amorphous calcium phosphate. Aust Dent J. 2003;48:240–3. doi: 10.1111/j.1834-7819.2003.tb00037.x. [DOI] [PubMed] [Google Scholar]
- 5.Andersson OH, Kangasniemi I. Calcium phosphate formation at the surface of bioactive glass in vitro. J Biomed Mater Res. 1991;25:1019–30. doi: 10.1002/jbm.820250808. [DOI] [PubMed] [Google Scholar]
- 6.Hench LL, Andersson OH. An introduction to bioceramics. In: Hench LL, Wilson J, editors. Advanced Series in Ceramics. Vol. 1. Singapore: Scientific Publishing Co. Ltd.; 1993. pp. 41–6. [Google Scholar]
- 7.Cerruti MG, Greenspan D, Powers K. An analytical model for the dissolution of different particle size samples of Bioglass in TRIS-buffered solution. Biomaterials. 2005;26:4903–11. doi: 10.1016/j.biomaterials.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 8.Burwell AK, Litkowski LJ, Greenspan DC. Calcium sodium phosphosilicate (NovaMin): Remineralization potential. Adv Dent Res. 2009;21:35–9. doi: 10.1177/0895937409335621. [DOI] [PubMed] [Google Scholar]
- 9.White DJ, Faller RV, Bowman WD. Demineralization and remineralization evaluation techniques – Added considerations. J Dent Res. 1992;71:929–33. doi: 10.1177/002203459207100S28. [DOI] [PubMed] [Google Scholar]
- 10.Lata S, Varghese NO, Varughese JM. Remineralization potential of fluoride and amorphous calcium phosphate-casein phospho peptide on enamel lesions: An in vitro comparative evaluation. J Conserv Dent. 2010;13:42–6. doi: 10.4103/0972-0707.62634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Darshan HE, Shashikiran ND. The effect of McInnes solution on enamel and the effect of Tooth mousse on bleached enamel: An in vitro study. J Conserv Dent. 2008;11:86–91. doi: 10.4103/0972-0707.44058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vashisht R, Kumar A, Indira R, Srinivasan MR, Ramachandran S. Remineralization of early enamel lesions using casein phosphopeptide amorphous calcium phosphate: An ex-vivo study. Contemp Clin Dent. 2010;1:210–3. doi: 10.4103/0976-237X.76385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta AB, Kumari V, Jose R, Izadikhah V. Remineralization potential of bioactive glass and casein phosphopeptide-amorphous calcium phosphate on initial carious lesion: An in-vitro pH-cycling study. J Conserv Dent. 2014;17:3–7. doi: 10.4103/0972-0707.124085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arend J, Ten Cate JM. Tooth enamel remineralization. J Cryst Growth. 1981;53:135–47. [Google Scholar]
- 15.Featherstone JD, ten Cate JM, Shariati M, Arends J. Comparison of artificial caries-like lesions by quantitative microradiography and microhardness profiles. Caries Res. 1983;17:385–91. doi: 10.1159/000260692. [DOI] [PubMed] [Google Scholar]
- 16.Perdigão J, Geraldeli S, Hodges JS. Total-etch versus self-etch adhesive: Effect on postoperative sensitivity. J Am Dent Assoc. 2003;134:1621–9. doi: 10.14219/jada.archive.2003.0109. [DOI] [PubMed] [Google Scholar]
- 17.Chow LC, Takagi S, Carey CM, Sieck BA. Remineralization effects of a two-solution fluoride mouthrinse: An in situ study. J Dent Res. 2000;79:991–5. doi: 10.1177/00220345000790041601. [DOI] [PubMed] [Google Scholar]
- 18.Guangming Z, Stanley JN, Le DT, Young D. To evaluate and compare the microhardness of enamel at different loading conditions. Dent Mater. 1973;12:102–6. [Google Scholar]
- 19.Iijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. Caries Res. 2004;38:551–6. doi: 10.1159/000080585. [DOI] [PubMed] [Google Scholar]


