Abstract
Background:
The metabolic syndrome and periodontitis coincide with systemic inflammation and glucose tolerance disorder, which indicate the common pathophysiologic pathway of these diseases. The main goal of this study was to determine the effects of the metabolic syndrome on the periodontal indices of hemodialysis (HD) patient.
Materials and Methods:
In this descriptive-analytical study, 75 persons were selected by the simple method, 50 of them were HD patients, and 25 of them were healthy people. They were divided into three groups each of which included 25 persons. The periodontal conditions of the selected persons were determined by radiography, gingival index, probing pocket depth, and bleeding index. Then, the periodontal indices of the patients suffering from metabolic syndrome and the persons not affected by metabolic syndrome were compared. At the end, the data were analyzed by SPSS software (version 20) using Mann–Whitney and Kruskal–Wallis tests at the meaningful level of α = 0.05. Since the condition of the unilateral variance test could not be provided for this study, the Kruskal–Wallis test was used. To complete the test, the Mann–Whitney test was used in the binary form among the groups being studied.
Results:
The obtained results showed a meaningful difference among the groups under study (P < 0.001). The results of the test showed a meaningful difference among the obtained indices of the groups being studied in the binary form (P < 0.001) too.
Conclusion:
The results of the present study revealed when the severity of chronic systemic disease increased the health of the periodontal tissues would decrease.
Key Words: Hemodialysis, patients, metabolic syndrome, periodontal indices
INTRODUCTION
Based on the recent definitions having more than three of the following symptoms confirm the existence of metabolic syndrome in a patient. These symptoms include hypertension, triglyceridemia, dyslipidemia, abdomen obesity, and resistance to insulin, increase of C protein and fibrinogen.[1] The pathogenesis of the metabolic syndrome is unknown yet.[2] Mild systemic inflammation originating from gum infection may relate to the metabolic syndrome.[3] Furthermore, the metabolic syndrome is associated with oxidative syndrome. Oxidative syndrome can be considered as a connective factor for metabolic syndrome and periodontitis.[4,5] Moreover, both metabolic syndrome and periodontitis coincide with systemic inflammation and glucose tolerance disorder, which indicate the common pathophysiologic pathway of these diseases. Nevertheless, there is a little information about the relation of metabolic syndrome and hemodialysis (HD).[5,6] Meanwhile, periodontitis and metabolic syndrome are prevalent in the patients suffering from HD. However, there is a little information about their association.[7]
Although there are no specific signs in the mouth indicating the presence of chronic kidney disease, a whole range of changes occur in the mouth that is associated with chronic kidney disease and HD. This condition has been reported to affect the teeth, oral mucosa, bone, periodontium, salivary glands, tongue, mouth cavity, and temporomandibular joint. These patients suffer from bad taste in their mouth, xerostomia, severe periodontitis, poor dental status, no carious tooth tissue loss, and a 14% prevalence of moderate to severe periodontitis was reported among individuals >20 years of age in the USA population.[7,8]
In their study, Shimazaki et al.[9] and Khader et al.[10] separately showed that the patients suffering from metabolic syndrome show more “pocket depth” and “attachment loss.” They concluded that metabolic syndrome increases the risk of periodontitis and thus, the patients with metabolic syndrome symptoms must be examined to diagnose whether they are affected by periodontitis or not.
Moreover, D'Aiuto et al.[6] and Chen et al.[8] separately showed that severe periodontitis is associated with metabolic syndrome in HD patients. Improvement of mouth care decreases the risk of metabolic syndrome. It was concluded from Nesbitt's study[11] that the volunteers with average to severe bone resorption had a higher chance to be affected by metabolic syndrome.
Since metabolic syndrome is a crucial problem of the society, it is necessary to determine the at-risk individuals to control it and decrease the mortality rate. A more exact and precise understanding of the metabolic syndrome side effects and the involving mechanisms can help to control and overcome it effectively.[12,13] Moreover, the on-time diagnosis of the disease inhibits its progress and increases the patient's lifetime.
Based on the previous research, it seems that no study has been done to compare the healthy people and HD patients suffering from metabolic syndrome in Iran. Hence, the main goal of this research was to determine the effects of the metabolic syndrome on the periodontal indices of HD patients.
MATERIALS AND METHODS
In this descriptive-analytical study, 75 persons were selected by the simple method, 50 of them were HD patients (for 5 years), and 25 of them were healthy people. They were divided into three groups of 25 persons. The inclusion criteria to allow the patients to participate in the research are as follows:
The patient must have more than 10 teeth
The patient must not have the local alterations such as previous surgery or bone transplantation to change the results of the study
The patient must not smoke or take antibiotics from last 2 weeks onward.
The first group included 25 HD patients not suffering from metabolic syndrome; the second group included 25 HD patients suffering from metabolic syndrome and the third group, namely the control group of the study, included 25 healthy persons (not affected by HD and metabolic syndrome). Age, gender, and physical condition were matched between the groups. to minimize the role of the intervening factors. This study was carried out at one of the therapeutic centers of Najaf Abad City. At first, the volunteers signed consent forms to participate in the research. Furthermore, they were coded to keep the information secret. Evaluation of the metabolic syndrome was done considering the five specifications according to the definition of the National Cholesterol Education Program Society of America as follows:
Abdomen obesity: The size of the waist more than 102 cm for men and more than 88 for women
Hypertriglyceridemia: Triglyceride more than 150 mg/dl
High-density lipoprotein cholesterol: Men <40 mg/dl and women <50 mg/dl
Hypertension: Systolic >130 mmHg and diastolic >85 mmHg
High plasma glucose: Glucose >110 mg/dl
At least, three of the above-mentioned specifications must be at the threshold level or higher to confirm the metabolic syndrome in the patient.[11] Then, the periodontal conditions of the selected persons were determined by radiography and the bone resorption was calculated by two periodontitis. To measure the bone resorption, digital panoramic radiography was used. The distance from the crest of the bone to the cement-enamel junction was measured and registered. The distance more than 2 mm was considered as the bone resorption. Considering the enlargement probability of the radiographies, the manufacturer's guidelines were used to analyze the resorption value, and the exact values were obtained
After selecting the patients, the average value of the bone resorption of the groups under study was measured and registered. Then, the gingival index was calculated by the Leo index[14] in four points. To determine the probing pocket depth, the distance from the edge of the gingiva to the depth of the gingival fissure was measured using Williams Probe. The bleeding index in the interproximal areas was measured using the Muhlemann index.[14] Then, the periodontal indices of the patients suffering from metabolic syndrome and the persons not affected by metabolic syndrome were compared. At the end, the data were analyzed by SPSS20 (IBM, Armonk, NY, United States of America) using Mann–Whitney and Kruskal–Wallis tests at the meaningful level of α = 0.05.
RESULTS
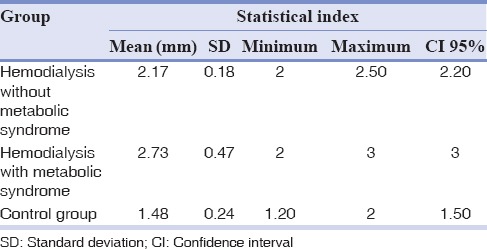
The mean, minimum, maximum, median and standard deviation of the bone resorbtion analysis is shown in Table 1. The mean, minimum, maximum, median, and standard deviation of the probe depth for the groups being studied in terms of mm is shown in Table 2.
Table 1.
The mean, minimum, maximum, median and standard deviation of the bone resorbtion analysis for the studied groups
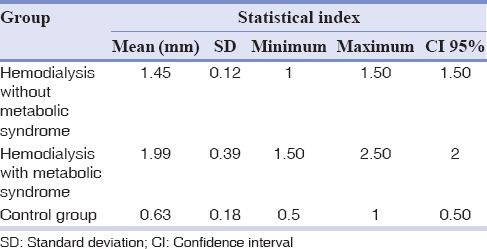
Table 2.
The mean, minimum, maximum, median and standard deviation of the probe depth for the studied groups
In Figure 1, the frequency distribution of the groups under study according to the bleeding index of the gingiva around the teeth is shown.
Figure 1.
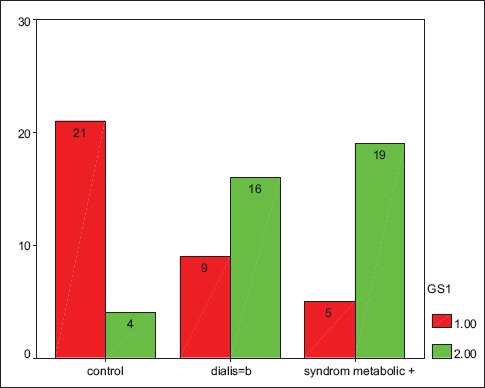
The frequency distribution of the groups under study according to the bleeding index of the gingiva around the teeth.
In Figure 2, the frequency distribution of the gingival index of the groups under study is shown.
Figure 2.
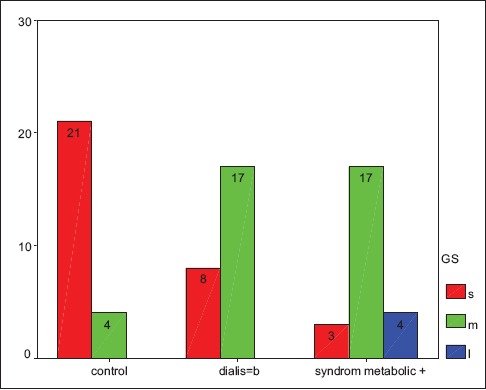
The frequency distribution of the gingival index of the groups under study.
As it can be seen, the mean of the bone resorption, the mean of the probing depth, the value of the gingival index, and the bleeding index of the HD patients with metabolic syndrome show the maximum levels and those of the control group show the minimum values.
Since the condition of the unilateral variance test could not be provided for this study, the Kruskal–Wallis test was used. The obtained results showed a meaningful difference among the groups under study (P < 0.001). To complete the test, the Mann–Whitney test was used in the binary form among the groups being studied. The results of the test showed a significant difference among the obtained indices of the groups being studied in the binary form (P < 0.001) too.
DISCUSSION
Periodontitis is an intensive response to the local pathogens of the gingival areas and periodontal tissues which resultsin bone resorption and tooth loss.[15] Previous studies have shown the high frequency of periodontitis in HD patients.[16,17] In the patients suffering from periodontitis, periodontal pocket can be considered as an important source of systemic inflammation.[5] Oral diseases contribute to the elevated incidence of HD patients. All of the risk factors are interrelated in a vicious circle: Whereas poor oral health may lead to both inflammation and protein-energy wasting in HD patients, numerous pathways associate the accumulation of proinflammatory cytokines with different aspects of protein-energy wasting, including anorexia, muscle loss, low anabolic hormones, increased energy expenditure, and insulin resistance.[7]
Metabolic syndrome is a disorder consisting of several cardiometabolic disorders.[18,19] Metabolic syndrome coincides with the high-risk of cardiovascular diseases and diabetes.[20,21] Periodontitis and metabolic syndrome both coincide with systemic inflammation and glucose tolerance disorder. These findings indicate the common pathophysiologic pathway for both diseases.[6] In this study, the mean of the bone resorption for HD patients suffering from metabolic syndrome was calculated as 1.99 mm, for HD patients not suffering from metabolic syndrome as 1.45 mm and for the control group (not suffering from HD and metabolic syndrome) as 0.63 mm [Table 1].
The difference between the groups understudying the binary form was statistically significant (P < 0.05). Hence, the maximum value of the bone resorption was observed in the group affected by both the metabolic syndrome and HD, and the minimum value was observed in the control group, including the healthy persons. Therefore, the obtained results of this study are in line with the results of Schimazaki's,[9] Nesbitt et al.,[11] Chen et al.,[8] and D'Aiuto et al.[6] Hence, it can be concluded that because of the additive effect of metabolic syndrome and HD, the mean of the bone resorption will increase in such patients. Furthermore, in this study, the means of the probe depth for the HD patients suffering from metabolic syndrome, the HD patients not suffering from metabolic syndrome and the control group including healthy persons were 2.73, 2.17, and 1.48 mm, respectively. The difference among the groups being studied in the binary form was statistically meaningful. Hence, the patients suffering from both metabolic syndrome and HD showed the maximum value for probe depth and the control group, including the healthy persons showed the minimum value for the probe depth. Thus, the results of this study are in agreement with the results of Shimazaki et al.[9] and Khader's.[10] studies. Therefore, it can be concluded that the additive effect of the metabolic syndrome and HD will increase the mean probe depth of the patients.
In this study, the frequency of the gingival bleeding index showed the maximum value in the HD patient suffering from metabolic syndrome. The control group, however, showed the minimum value. Furthermore, the results of this study revealed that the patients suffering severely from systemic inflammation showed a higher percentage of the gingival index frequency so that the patients suffering from both HD and metabolic syndrome showed the maximum value and the control group showed the minimum value of the gingival index.
The difference between the groups being studied in the binary form was statistically significant (P < 0.05). Therefore, the additive effect of the metabolic syndrome and HD increased the gingival index. In regard, based on the results obtained in a study on the 4 considered specifications of the periodontal indices, it can be concluded that the more the severity of the systemic disease increases, the more the health of the periodontal tissues will decrease. So that, in this study all the periodontal indices of the HD patients suffering from metabolic syndrome were at the lowest level in comparison with other groups and the patient not suffering from metabolic syndrome as well as the control group were in the second and third positions, respectively. The causes can be attributed to the hemodialysis role to disable the patient to care for his mouth and tooth health, the same risk factors of the metabolic syndrome and periodontal disease which intensify the periodontal disease and the suppression of the immune system resulting from chronic diseases.
This study was limited by some factors, including a low number of the samples and the impossibility of the prevalence calculation of metabolic syndrome in the patients suffering from periodontal disease. A cross-sectional study with a limited case number, it has a little clinical impact, so the confounding effect of glucose intolerance or overt diabetes mellitus cannot be clearly excluded in a small-scale study also panoramic is not a suitable radiographic for bone loss evaluation due to distortions and superimpositions, so a better radiographic is recommended.
CONCLUSION
The results of this study revealed when the severity of chronic systemic disease increased the health of the periodontal tissues would decrease in such a manner that the HD patients suffering from metabolic syndrome showed the lowest level of health for the periodontal tissues, and the HD patients not suffering from metabolic syndrome and the control group showed the highest level of health, respectively.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
REFERENCES
- 1.Scott CL. Diagnosis, prevention, and intervention for the metabolic syndrome. Am J Cardiol. 2003;92:35i–42i. doi: 10.1016/s0002-9149(03)00507-1. [DOI] [PubMed] [Google Scholar]
- 2.Bharti V, Khurana P. Metabolic syndrome and periodontal disease. J Indian Soc Periodontol. 2009;13:172–4. doi: 10.4103/0972-124X.60234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson LW, Weinstock RS, editors. The Metabolic Syndrome: Concepts and Controversy. Elsevier: Mayo Clinic Proceedings; 2006. [DOI] [PubMed] [Google Scholar]
- 4.Bensley L, VanEenwyk J, Ossiander EM. Associations of self-reported periodontal disease with metabolic syndrome and number of self-reported chronic conditions. Prev Chronic Dis. 2011;8:A50. [PMC free article] [PubMed] [Google Scholar]
- 5.Hujoel PP, White BA, García RI, Listgarten MA. The dentogingival epithelial surface area revisited. J Periodontal Res. 2001;36:48–55. doi: 10.1034/j.1600-0765.2001.00011.x. [DOI] [PubMed] [Google Scholar]
- 6.D’Aiuto F, Sabbah W, Netuveli G, Donos N, Hingorani AD, Deanfield J, et al. Association of the metabolic syndrome with severe periodontitis in a large U.S. population-based survey. J Clin Endocrinol Metab. 2008;93:3889–94. doi: 10.1210/jc.2007-2522. [DOI] [PubMed] [Google Scholar]
- 7.Akar H, Akar GC, Carrero JJ, Stenvinkel P, Lindholm B. Systemic consequences of poor oral health in chronic kidney disease patients. Clin J Am Soc Nephrol. 2011;6:218–26. doi: 10.2215/CJN.05470610. [DOI] [PubMed] [Google Scholar]
- 8.Chen LP, Hsu SP, Peng YS, Chiang CK, Hung KY. Periodontal disease is associated with metabolic syndrome in hemodialysis patients. Nephrol Dial Transplant. 2011;26:4068–73. doi: 10.1093/ndt/gfr209. [DOI] [PubMed] [Google Scholar]
- 9.Shimazaki Y, Saito T, Yonemoto K, Kiyohara Y, Iida M, Yamashita Y. Relationship of metabolic syndrome to periodontal disease in Japanese women: The Hisayama Study. J Dent Res. 2007;86:271–5. doi: 10.1177/154405910708600314. [DOI] [PubMed] [Google Scholar]
- 10.Khader Y, Khassawneh B, Obeidat B, Hammad M, El-Salem K, Bawadi H, et al. Periodontal status of patients with metabolic syndrome compared to those without metabolic syndrome. J Periodontol. 2008;79:2048–53. doi: 10.1902/jop.2008.080022. [DOI] [PubMed] [Google Scholar]
- 11.Nesbitt MJ, Reynolds MA, Shiau H, Choe K, Simonsick EM, Ferrucci L. Association of periodontitis and etabolic syndrome in the Baltimore Longitudinal Study of Aging. Aging Clin Exp Res. 2010;22:238–42. doi: 10.1007/bf03324802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eckel R.H. Obesity: Mechanisms and Clinical Management. Philadelphia, pa, USA: Lippincott Williams and wilkins; 2003. [Google Scholar]
- 13.Friedlander AH, Weinreb J, Friedlander I, Yagiela JA. Metabolic syndrome: Pathogenesis, medical care and dental implications. J Am Dent Assoc. 2007;138:179–87. doi: 10.14219/jada.archive.2007.0134. [DOI] [PubMed] [Google Scholar]
- 14.Misch CE, editor. Contemporary Implant Dentistry. 3rd ed. 2008. Rationale for dental implants; pp. 555–543. Ch. 25. [Google Scholar]
- 15.Kornman KS. Mapping the pathogenesis of periodontitis: A new look. J Periodontol. 2008;79(8 Suppl):1560–8. doi: 10.1902/jop.2008.080213. [DOI] [PubMed] [Google Scholar]
- 16.Chen LP, Chiang CK, Chan CP, Hung KY, Huang CS. Does periodontitis reflect inflammation and malnutrition status in hemodialysis patients? Am J Kidney Dis. 2006;47:815–22. doi: 10.1053/j.ajkd.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 17.Chen LP, Chiang CK, Peng YS, Hsu SP, Lin CY, Lai CF, et al. Relationship between periodontal disease and mortality in patients treated with maintenance hemodialysis. Am J Kidney Dis. 2011;57:276–82. doi: 10.1053/j.ajkd.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 18.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement: Executive Summary. Crit Pathw Cardiol. 2005;4:198–203. doi: 10.1097/00132577-200512000-00018. [DOI] [PubMed] [Google Scholar]
- 20.de Vinuesa SG, Goicoechea M, Kanter J, Puerta M, Cachofeiro V, Lahera V, et al. Insulin resistance, inflammatory biomarkers, and adipokines in patients with chronic kidney disease: Effects of angiotensin II blockade. J Am Soc Nephrol. 2006;17(12 Suppl 3):S206–12. doi: 10.1681/ASN.2006080916. [DOI] [PubMed] [Google Scholar]
- 21.Mauras N, Delgiorno C, Kollman C, Bird K, Morgan M, Sweeten S, et al. Obesity without established comorbidities of the metabolic syndrome is associated with a proinflammatory and prothrombotic state, even before the onset of puberty in children. J Clin Endocrinol Metab. 2010;95:1060–8. doi: 10.1210/jc.2009-1887. [DOI] [PubMed] [Google Scholar]


