Abstract
Objectives
Online weight control technologies could reduce barriers to treatment, including increased ease and convenience of self-monitoring. Self-monitoring consistently predicts outcomes in behavioral weight loss programs; however, little is known about patterns of self-monitoring associated with success.
Methods
The current study examines 161 participants (93% female; 31% African-American; mean BMI=35.7±5.7) randomized to a 6-month online behavioral weight control program which offered weekly group “chat” sessions and online self-monitoring. Self-monitoring log-ins were continuously monitored electronically during treatment and examined in association with weight change and demographics. Weekend and weekday log-ins were examined separately and length of periods of continuous self-monitoring were examined.
Results
We found that 91% of participants logged in to the self-monitoring webpage at least once. Over 6 months, these participants monitored on an average of 28% of weekdays and 17% of weekend days, with most log-ins earlier in the program. Women were less likely to log-in, and there were trends for greater self-monitoring by older participants. Race, education and marital status were not significant predictors of self-monitoring. Both weekday and weekend log-ins were significant independent predictors of weight loss. Patterns of consistent self-monitoring emerged early for participants who went on to achieve greater than a five percent weight loss.
Conclusions
Patterns of online self-monitoring were strongly associated with weight loss outcomes. These results suggest a specific focus on consistent self-monitoring early in a behavioral weight control program might be beneficial for achieving clinically significant weight losses.
Keywords: self-monitoring, temporal patterns, adherence, behavior, weight loss
Self-monitoring involves the systematic observation and recording of eating and exercise behaviors by the individual, and is a crucial component to behavior change according self-regulation theory (Kirschenbaum, 1987). According to this theory, self-regulation involves establishing goals, expectancies, and plans, monitoring one’s behavior, and evaluating one’s performance (Kirschenbaum, 1987). Behavioral weight control programs consistently target all of these elements—goal setting, self-monitoring, and evaluation of progress toward one’s goals—as essential components for weight loss success.
A key, commonly measured outcome of self-regulation—self-monitoring—consistently predicts weight loss outcomes in both in-person (Boutelle & Kirschenbaum, 1998; Burke et al., 2008; Diabetes Prevention Program Research Group, 2004; Helsel, Jakicic, & Otto, 2007; Streit, Stevens, Stevens, & Rossner, 1991; West, Gore, DiLillo, Greene, & Bursac, 2007) and online behavioral weight loss programs (Burke et al., 2011; Cussler et al., 2008; Gold, Burke, Pintauro, Buzzell, & Harvey-Berino, 2007; Tate, Jackvony, & Wing, 2006; Tate, Wing, & Winett, 2001). Online weight control technologies could reduce barriers to behavioral weight control treatment, by providing increased ease and convenience of self-monitoring. Some research suggests that participants in Internet- or technology-based programs may have greater adherence to self-monitoring than participants receiving the program in-person (Burke et al., 2011; Harvey-Berino, Pintauro, Buzzell, & Gold, 2004). For these reasons, greater examination of self-monitoring, a key strategy for weight loss, using the potentially beneficial online modality may be helpful for understanding and enhancing behavioral weight control programs. Currently, little is known about patterns of self-monitoring that are associated with success in a behavioral weight loss program.
Previous research has shown that there may be different patterns of dietary intake and physical activity on weekdays versus weekend days. Specifically, individuals tend to consume more total calories (Jula & Seppanen, 1999), as well as a higher percentage of fat (O'Dwyer, McCarthy, Burke, & Gibney, 2005), on weekends compared to weekdays. In addition, individuals tend to have lower physical activity on the weekends, particularly on Sundays (Clemes, Hamilton, & Lindley, 2008; Tudor-Locke et al., 2004). Weekends have also been shown to be associated with increases in weight (Tuomisto et al., 2006). Taken together, results from these previous studies could be construed to demonstrate that weekends may be particularly challenging times for individuals to remain adherent to effective behavioral weight loss strategies such as self-monitoring. Our clinical experience is that participants in behavioral weight control programs self-monitor less frequently on weekends compared to weekdays; however, we are not aware of any research examining weekend versus weekday self-monitoring behaviors.
Despite the strong and consistent findings that greater self-monitoring is associated with greater weight loss, rates of self-monitoring consistently decline over the course of behavioral weight control programs (Burke et al., 2011; Sevick et al., 2010; Tate et al., 2006; Wadden et al., 2005). Furthermore, there is some recent research that indicates that participant performance in the early weeks of a behavioral weight loss program may differentiate those who will go on to be successful and those who will be less successful (West, Harvey-Berino, Krukowski, & Skelly, e-published before publication). However, available data on the frequency and patterns of how self monitoring declines over time are few, and there is little to inform which patterns of declining self monitoring are more detrimental to outcomes and which preserve benefit and contribute to long-term success. Such information would be critical in shaping recommendations for duration and frequency of self-monitoring.
Therefore, the primary purpose of the study was to examine patterns of self-monitoring associated with greater weight loss at 6-months. We hypothesize that participants will be less likely to self-monitor on the weekends compared to weekdays, because previous research and clinical experience suggests that there may be more challenges in adherence to health behaviors on weekends, and that greater weekend self-monitoring will be associated with greater weight loss at 6-months (Aim 1). Furthermore, we expect that self-monitoring frequency will decrease over the course of the program; thus, we will examine the self-monitoring patterns over the course of the program, with a specific focus on early periods of the program, to determine whether there are critical periods associated with weight loss success (Aim 2).
Methods
Study Design
The current report examines individuals randomized to online treatment modalities as part of a larger randomized controlled trial comparing in-person and online modalities for delivering group-based behavioral weight control, which has previously been described in detail (Harvey-Berino et al., 2010). In short, participants were randomized to one of three intervention delivery arms (i.e., in-person, online, and combination) which offered group sessions weekly for six months. Participants were accrued over the course of five trial waves stratified within each of two sites, Vermont and Arkansas. Each trial wave consisted of three intact groups of participants recruited at each site who were able to attend predetermined meeting times. Each group within each wave was stratified by their baseline BMI percentile values (25th, 50th, 75th) prior to randomization and then groups were randomized. Groups were randomized using a biased coin approach. The current report focuses on the 161 participants who were randomized to the online condition.
Participants
Initial eligibility was assessed via a study recruitment website from February 2003 to March 2005. Interested participants then were phone screened and attended a study orientation. Informed consent was obtained at the first of two in-person screening and baseline data collection visits. Eligibility criteria included: being overweight or obese with a body mass index [BMI; calculated as weight (kg)/ height (m2)] between 25 and 50, age 18 years or older, and access to a computer with an Internet connection. Exclusion criteria included a history of major medical or psychiatric conditions; recent changes in medication known to affect weight; current, planned or recent pregnancy; medical conditions that would prohibit exercise; and a schedule that would prohibit or restrict attendance at a designated time for weekly group meetings. The study was approved by the Committee on Human Research in the Behavioral Sciences at the University of Vermont and the Institutional Review Board at the University of Arkansas for Medical Sciences.
Online Behavioral Weight Control Intervention
The six-month manualized comprehensive behavioral weight loss intervention was delivered over 24 group sessions. Groups of 12–18 participants met weekly for one hour in a secure online format via a synchronous chat. Group counselors used a written protocol that outlined standard lessons with counselor guides to ensure treatment fidelity. Counselors included behaviorally trained public health practitioners, clinical psychologists, and registered dieticians with extensive weight management experience.
The behavioral weight loss program focused on the modification of eating and exercise habits through the use of behavioral strategies and self-management skills. Participants were prescribed a calorie restricted diet and given a dietary fat goal corresponding to ≤25% of calories from fat. Graded exercise goals were provided which progressed to 200 min/week of moderate to vigorous exercise like walking, and pedometers were provided. Behavioral strategies included self-monitoring, stimulus control, problem solving, goal setting, relapse prevention, and assertiveness training (Boutelle & Kirschenbaum, 1998; D'Zurilla & Goldfried, 1971; Perri et al., 2001; Perry, Baranowski, & Parcel, 1990). Online homework assignments corresponding to these strategies were provided weekly. Participants were instructed to record their dietary intake, minutes of physical activity and weight daily in an online journal. Participants had access to an online database to help monitor calorie intake based on the United States Department of Agriculture’s National Nutrient Database for Standard Reference. Participants received weekly individualized counselor feedback on self-monitoring (or lack thereof) and progress toward meeting exercise and dietary intake goals. The Web site also included educational resources, a bulletin board for group communication, weekly tips and recipes, a BMI calculator, and local physical activity events.
Measures
Body weight
Weight change was the primary dependent measure. Weight was measured in street clothes, without shoes, on a calibrated digital scale (Tanita), at baseline and at six months. Height was measured using a wall-mounted stadiometer (Seca Corporation, Hanover, MD) at baseline.
Self-monitoring
Self-monitoring log-ins were continuously monitored electronically during treatment, with records to indicate whether a participant logged into the self-monitoring page on any given day. For each day of the six-month program, participants received a dichotomous code for “did not self-monitor=0” or “self-monitored at least one item=1.” Previous research has suggested the level of detail in the self-monitoring journal may not be as crucial as the process of self-monitoring itself (Helsel et al., 2007). Therefore, the presence of any self-monitoring data was coded rather than the content or accuracy of the information that was self-monitored. Weekly self-monitoring “journals” were defined as self-monitoring for the seven days prior to the weekly group chat and a total of 24 weekly “journals” were possible.
Demographic Information
Participants self-reported age, gender, race/ethnicity, marital status and education on questionnaires completed at baseline.
Data Analyses
Descriptive analyses of self-monitoring log-ins were conducted, examining overall log-ins, as well as weekday and weekend (i.e., Saturdays and Sundays) log-ins by demographic factors. A multivariate linear regression model was used to examine independent associations between weekend and weekday log-ins with six-month weight change, controlling for demographic factors. In addition, participants were grouped into four weight loss categories to facilitate evaluation of the self-monitoring behavior at each level of weight loss success at each treatment interval. Categories of weight loss success at 6-months considered were: No Weight Loss (<0% weight loss); Minimal Weight Loss (0–5% weight loss); Moderate Weight Loss (>5% weight loss and <10% weight loss); and High Weight Loss (≥10% weight loss). An analysis of variance was used to compare average log-ins by weight loss category, with Tukey adjustments for multiple comparisons. To further explore how self-monitoring changed over time, log-in behaviors were isolated for Weeks One through Four, Weeks Five through Eight, and Weeks Nine through Twenty-Four and examined individually at each of these treatment intervals. Given recent research (West et al., e-published before publication) demonstrating the emergence of indicators of overall weight loss success early in treatment, there is reason to be particularly interested in early behavioral indicators of success when these factors may be modifiable. Therefore, early in the treatment program, shorter time period of four-weeks each were examined and the remainder of the treatment period (16 weeks) was examined in aggregate. This was done to allow identification of a potential “critical” period for consistent self-monitoring early in treatment and to characterize when this might be. Within treatment interval, the number of consecutive days of self-monitoring (i.e., number of consecutive days with at least one log-in per day) was quantified using a statistical runs perspective. The run length of consecutive days of self-monitoring was calculated. For example, a run of length of one would represent a single day of monitoring followed by a non-monitoring day and a run length of five would represent five consecutive days of monitoring followed by a non-monitoring day. Run lengths of continuous self monitoring were calculated for each participant within each treatment interval. Run lengths could range from one day to six days, with more than 6 days collapsed into the 6 day run length. A repeated-measures ANOVA then examined the number of runs of various lengths for the four weight loss categories within each of the three treatment intervals, with a specific focus upon the statistical interaction of run lengths and weight loss to determine whether the weight loss categories differed in their consistency of self-monitoring during each of the three treatment intervals. For those interactions that were statistically significant, individual paired comparisons of weight loss groups were conducted using Fisher’s Least Significant Difference test. All analyses were conducted using either SAS Version 9.2 (SAS Institute: Cary, NC) or SYSTAT Version 11 (SYSTAT Software, Inc; Richmond, CA).
Results
The 161 participants randomized to the online condition were predominately female (92%), obese (mean BMI=35.6±5.7), middle aged (mean 46.2±9.8 years; range: 22–68 years), employed full time (85%), married (68%), with 31% identifying as African American and 69% identifying as Caucasian. The majority (69%) of the participants were college graduates; of the other participants, 9% graduated from high school, 2% had vocational training beyond high school, and 20% had some college education. Participants achieved a mean weight loss of −5.5±5.6 kg at six months, which represented an average of −5.8±5.4% of their baseline weight. The sample was distributed across the weight loss success groups as follows: 12% No Weight Loss (<0% weight loss); 35% Low Weight Loss (0–5% weight loss); 30% Moderate Weight Loss (>5% weight loss and <10% weight loss); and 23% High Weight Loss (≥10% weight loss).
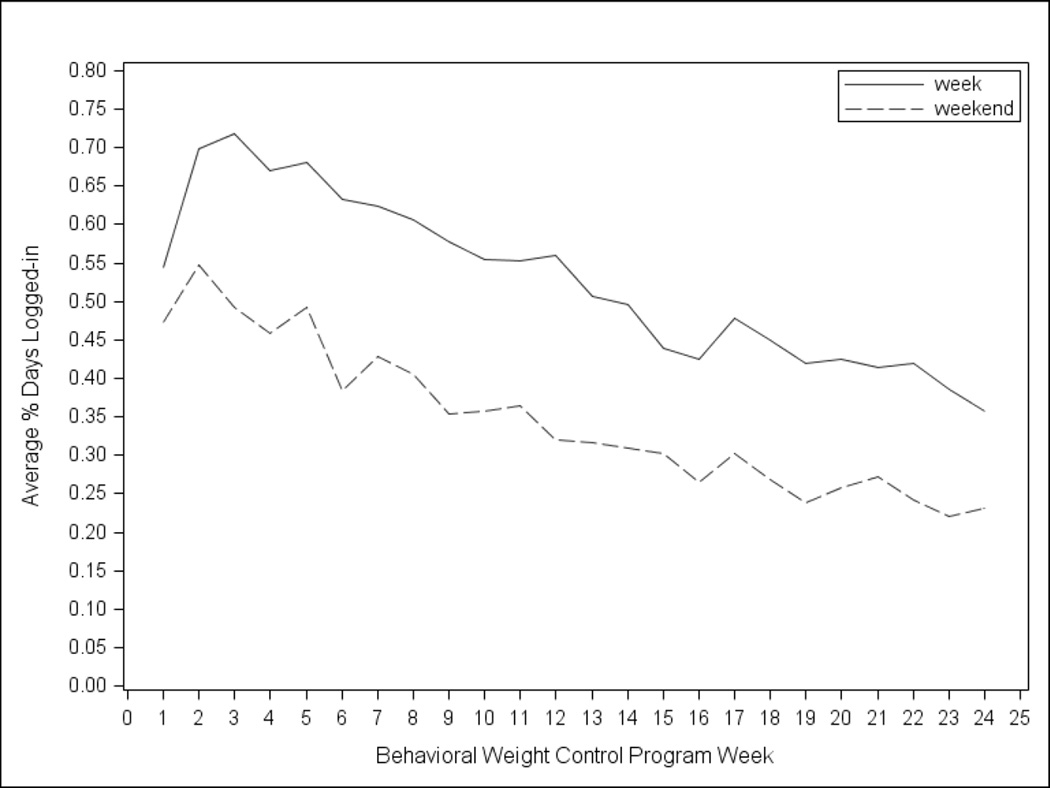
Overall, 91% of participants (n=147) logged in to the self-monitoring page at least once over the 6-month period, and the remaining analyses only include these participants who logged in at least once over the 6-month period. Participants submitted 73% of weekly self-monitoring journals (including at least one entry). Over 6 months, these participants logged in to the self-monitoring page an average of 28% of weekdays and 17% of weekend days. Log-ins peaked early in the program with participants logging in for 3.59 weekdays in the third week of the program and 1.10 days per weekend (Figure 1). The frequency of log-ins then slowly decreased such that by the end of the six-month program, log-ins had decreased to an average of 1.79 days per week and 0.44 days per weekend.
Figure 1.
Mean Percentage of Days that Participants Logged-In Over a 6-Month Behavioral Weight Control Program
Demographic Variables and Self-Monitoring
Female participants were significantly less likely to log-in overall to the self-monitoring tool (β=−0.18; SE=0.09; p<0.05), compared to male participants. Women logged in on 46% of days, while men logged in on 69% of days. With each one year increase in age, self-monitoring log-ins increased by 0.0044 (SE=0.09; p=0.059), indicating a trend of greater self-monitoring among older participants compared to younger participants. When examining who was self-monitoring on weekdays and weekends specifically, female participants were significantly less likely to log-in on weekdays (β=−0.19; SE=0.09; p<0.05) compared to male participants, and there was a trend for fewer log-ins for female participants on weekends (β=−0.16; SE=0.09; p=0.068). Age was associated with being more likely to log-in on weekdays and weekends, such that with each additional year of age, log-in increased by 0.005 (SE=0.002; p=0.056) on weekdays and by 0.004 on weekends (SE=0.002; p=0.088).. Race, education and marital status were not significant predictors of self-monitoring.
Weight Loss and Self-Monitoring (Aim 1)
Overall self-monitoring log-ins were a significant predictor of 6-month weight loss, even after adjustment for demographic factors (β = −0.11, p<0.0001). Both weekday and weekend log-ins were significant and independent predictors of 6-month weight loss, even after the adjustment for demographic factors. Each 10% increase in weekday log-ins was associated with a 1% increase in weight loss (β = −0.1, p<0.0001). With each additional 10% in weekend log-ins, weight loss increased by 0.9% (β = −0.09, p<0.0001). Weekday and weekend log-ins were highly correlated (r=0.83) suggesting that they measure the same thing, therefore were not examined within the same model jointly. Each was independently the most significant variable in their respective models and accounted for the largest proportion of variance (Weekday r-squared = 0.37; weekend r-squared = 0.3). Inclusion of other demographic variables in each model accounted for additional 0.07% of the variance.
The High and Moderate Weight Loss groups logged in on a significantly higher proportion of the possible days overall, on weekdays, and on weekend days, as compared to the No Weight Loss and the Low Weight Loss groups (all ps<0.0001). There were no significant differences in proportion of log-ins overall, on weekdays, or weekend days, between the High and Moderate Weight Loss groups nor between the No Weight Loss and the Low Weight Loss groups (all ps>0.05).
Self-Monitoring Across Treatment Intervals by Weight Loss Groups (Aim 2)
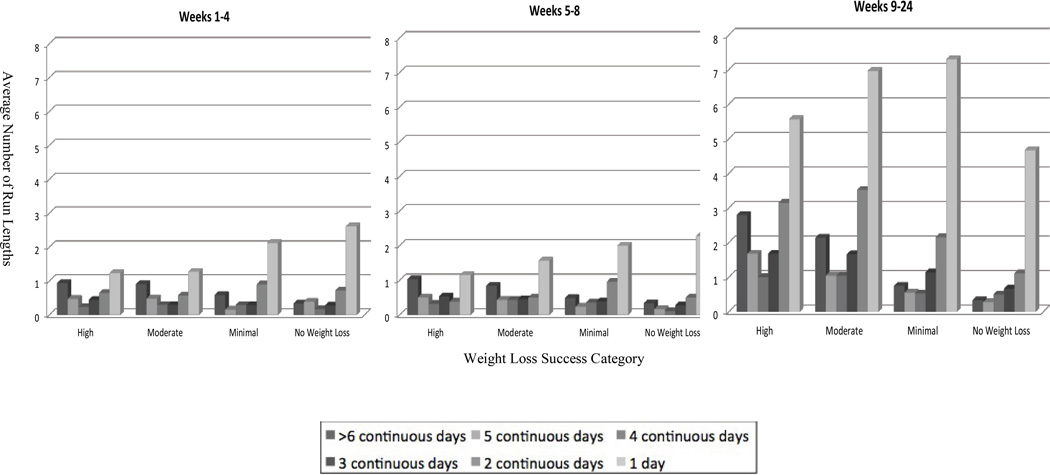
During Weeks One through Four, the number of periods of self-monitoring of six or more days showed a significant difference between the four weight loss groups (p<0.05) (Figure 2). Specifically, both the High and Moderate Weight Loss groups had significantly greater number of runs of six consecutive days or more of self-monitoring as compared to the No Weight Loss and the Low Weight Loss groups (all ps<0.05). There were no significant group differences for periods of self-monitoring of five, four, three, or two days (p>0.05). However, there were significant group differences for one day durations (p<0.01). Both the No Weight Loss and the Low Weight Loss groups had significantly greater runs of one day as compared to the High and Moderate Weight Loss groups (all ps<0.05).
Figure 2.
Average Number of Run Lengths By Weight Loss Success Category and Program Period.
During Weeks Five through Eight, there was not a significant interaction between weight loss category and consistency of self-monitoring (p = 0.15) (Figure 2). Thus, during this treatment interval the weight loss groups did not differ in their self-monitoring pattern.
During Weeks Nine through Twenty-Four, the number of periods of self-monitoring of six or more days once again differed significantly between the four weight loss groups (p<0.01) (Figure 2). Specifically, the LSD comparisons revealed that both the Moderate and High Weight Loss groups had more frequent periods of six or more days compared to those in the No Weight Loss and the Low Weight Loss groups (all ps<0.001). In addition, self-monitoring periods of five days during Weeks Nine through Twenty-Four differed significantly across groups (p<0.01). The LSD paired comparisons indicated that the High Weight Loss group had a greater number of self-monitored periods of five days compared to both the No Weight Loss and the Low Weight loss groups (all ps<0.01). No group differences were observed for self-monitoring of four days duration (p=0.061), although differences were observed for three days (p<0.05). Both the High and Moderate Weight Loss groups had greater number of periods of three day self-monitoring run compared to the No Weight Loss group (all ps<0.05). Group differences for two-day self-monitoring runs during Weeks Nine through Twenty-Four were significant (p<0.01), although self-monitoring runs of one day were not (p=0.23). Both the Moderate and High Weight Loss groups had greater number of self-monitoring periods of two days compared to the No Weight Loss group (all ps<0.05). The Low Weight loss group had fewer self-monitored periods of two days compared to the Moderate Weight Loss group only (p<0.05).
Discussion
This study demonstrated that participants who consistently self-monitor (i.e., periods of self-monitoring greater or equal to six days) early in a behavioral weight control program were significantly more likely to achieve clinically significant weight losses at 6 months (i.e., greater than a five percent weight loss) (Institute of Medicine, 1995). However, it appears that it is crucial to continue self-monitoring throughout a six-month behavioral weight control program, as consistent self-monitoring continued to distinguish those individuals who achieved a clinically significant weight loss from those who did not, in the latter weeks of the program (i.e., Weeks Nine through 24). Thus, consistent with findings from paper and pencil self-monitoring (Boutelle & Kirschenbaum, 1998; Burke et al., 2008; Diabetes Prevention Program Research Group, 2004; Helsel et al., 2007; Streit et al., 1991; West et al., 2007), online self-monitoring overall throughout a program was strongly associated with weight loss outcomes.
In addition to the importance of consistent periods of self-monitoring, we found that monitoring on both weekdays and weekends were independent significant predictors of weight loss success. Thus, it appears that both weekday and weekend self-monitoring are key components for weight loss success, consistent with previous research that found that keeping regular patterns of eating on both weekdays and weekends was crucial for long-term weight control (Wing & Phelan, 2005). However, we found that participants were less likely to self-monitor on weekends, consistent with previous research on paper-and-pencil recording (Clemes et al., 2008). It is possible that weekdays and weekends have unique challenges for self-regulation and there may be unique challenges or a surfeit of barriers for weekend self-monitoring. Weekend self-monitoring may be crucial to provide the ongoing performance feedback and reinforcement of goals that is required to successfully cope with the particular challenges that weekends appear to present to participants (Jula & Seppanen, 1999; O'Dwyer et al., 2005; Racette et al., 2008). Jula and colleagues (Jula & Seppanen, 1999) found individuals consumed significantly more overall calories on weekends compared to weekdays and that 80% of the total increase energy intake over weekday consumption was accounted for by alcohol on Friday, 50% of the increase on Saturday, and 30% of the increase on Sunday. In addition, O’Dwyer and colleagues (O'Dwyer et al., 2005) found that individuals consume a higher percentage of fat on weekends compared to weekdays, and Racette and colleagues (Racette et al., 2008) noted consistent weight gains on weekend days due to higher dietary intake on Saturdays and lower physical activity on Sundays compared to weekdays. Therefore, future programs may wish to explicitly address the need for consistent self-monitoring by articulating clear goals for both weekends and weekdays. An emphasis on the importance of both weekday and weekend self-monitoring, alerting participants that they may need to develop different self-monitoring strategies for weekends than those which work for them on weekdays (time of day, online access venue, etc) and cautioning that particular dietary intake and physical activity challenges may occur uniquely on weekdays and weekends might optimize weight loss success.
Contrary to the notion of a “digital divide,” or disparities in the successful utilization of technology by age, race, or education level, we did not find significantly lower online self-monitoring among older participants, those participants in racial minority groups, and those participants with lower education levels. In fact, consistent with previous research (Mossavar-Rahmani et al., 2004; Sevick et al., 2010), we found trends indicating that older participants may be more likely to self-monitor as compared to younger participants. The findings from the current study showing greater self-monitoring among older participants may help to explain why older participants appear to be particularly successful in lifestyle interventions (Diabetes Prevention Program Research Group, 2006; Lindstrom et al., 2008). In addition, consistent with Sevick and colleagues’ (Sevick et al., 2010) findings regarding self-monitoring on personal digital assistants, we did not find racial or education level differences in frequency of online self-monitoring, indicating that these demographic factors did not preclude effective use of technology.
Consistent with Hollis and colleagues (Hollis et al., 2008), we found gender differences in adherence to self-monitoring such that female participants were significantly less likely to log-in on weekdays compared to male participants and there was a trend for fewer log-ins for female participants on weekends. These findings are also consistent with previous research indicating that men enrolled in a behavioral weight control program tend to lose more weight (Wadden et al., 2009) and are more compliant with treatment recommendations such as achieving activity goals (Diabetes Prevention Program Research Group, 2004; Hollis et al., 2008). It has been assumed that the gender differences in lean body mass may explain why men tend to lose more weight in behavioral weight control programs; based on a growing body of research including the current study, it appears that there may be behavioral reasons as well for greater weight losses among men. However, as our sample was predominately female, these findings should be interpreted with caution, and it will be beneficial for future research to examine gender differences in self-monitoring in studies that include substantial samples of both men and women.
This study has several strengths and limitations. First, while online self-monitoring allowed for micro-analysis of patterns of self-monitoring, we are limited in our generalization of this study’s results to online self-monitoring and cannot assume that the same findings would hold for paper-and-pencil self-monitoring, which is still the most common approach in behavioral weight control programs. However, the consistency of the current study’s findings with findings from studies employing paper-and-pencil self monitoring lend confidence that generalizations may be reasonable. In addition, while we used self-monitoring log-ins as a proxy for the act of self-monitoring, it was not possible for us to track the activities of participants during each log-in. Finally, we did not collect information about whether any of the participants in this study were engaged in shift work or had a nontraditional work week, for whom the standard definition of a weekend day may not be as meaningful.
In sum, a focused analysis on daily patterns of self-monitoring and progression of self-monitoring over the course of treatment may be a fruitful direction of inquiry to inform behavioral weight control treatment development. A stronger emphasis on the unique importance of consistency of self-monitoring for consecutive periods of self-monitoring and monitoring on both weekdays and weekend days may enhance long-term weight loss outcomes. Further, early identification of individuals likely to experience attenuated weight losses based on short self-monitoring bouts may permit prompt intervention to re-engage these individuals before they experience extended lack of success. Increased intensity of intervention to “rescue” individuals who appear to be struggling in a behavioral weight control intervention has shown some promise (Carels et al., 2005; Carels et al., 2007). The current study would suggest that indications of likely success (and also likely failure) emerge as early as one month into a 6-month program. Treatment approaches as currently implemented do not have strong processes to reverse early failure nor do they usually have strong incentives for early success. The data from this study would argue that stronger procedures for identifying and responding to both outcomes might enhance long-term weight loss.
Acknowledgments
This research was supported by the NIH grant DK056746.
Contributor Information
Rebecca A. Krukowski, University of Arkansas for Medical Sciences.
Jean Harvey-Berino, University of Vermont.
Zoran Bursac, University of Arkansas for Medical Sciences.
Taka Ashikaga, University of Vermont.
Delia Smith West, University of Arkansas for Medical Sciences.
References
- Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obesity Research. 1998;6(3):219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- Burke LE, Conroy MB, Sereika SM, Elci OU, Styn MA, Acharya SD, et al. The effect of electronic self-monitoring on weight loss and dietary intake: A randomized behavioral weight loss trial. Obesity. 2011;19(2):338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Sereika SM, Music E, Warziski M, Styn MA, Stone A. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemporary Clinical Trials. 2008;29(2):182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carels RA, Darby L, Cacciapaglia HM, Douglass OM, Harper J, Kaplar ME, et al. Applying a stepped-care approach to the treatment of obesity. Journal of Psychosomatic Research. 2005;59:375–383. doi: 10.1016/j.jpsychores.2005.06.060. [DOI] [PubMed] [Google Scholar]
- Carels RA, Darby L, Cacciapaglia HM, Konrad K, Coit C, Harper J, et al. Using motivational interviewing as a supplement to obesity treatment: A stepped-care approach. Health Psychology. 2007;26(3):369–374. doi: 10.1037/0278-6133.26.3.369. [DOI] [PubMed] [Google Scholar]
- Clemes SA, Hamilton SL, Lindley MR. Four-week pedometer-determined activity patterns in normal-weight, overweight and obese adults. Preventive Medicine. 2008;46(4):325–330. doi: 10.1016/j.ypmed.2007.11.013. [DOI] [PubMed] [Google Scholar]
- Cussler EC, Teixeira PJ, Going SB, Houtkooper LB, Metcalfe LL, Blew RM, et al. Maintenance of weight loss in overweight middle-aged women through the Internet. Obesity. 2008;16(5):1052–1060. doi: 10.1038/oby.2008.19. [DOI] [PubMed] [Google Scholar]
- D'Zurilla TJ, Goldfried MR. Problem solving and behavior modification. Journal of Abnormal Psychology. 1971;78:107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. Achieving weight and activity goals among Diabetes Prevention Program lifestyle participants. Obesity Research. 2004;12:1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. The influence of age on the effects of lifestyle modification and metformin in prevention of diabetes. Journal of Gerontology: Series A, Biological Sciences and Medical Sciences. 2006;61A(10):1075–1075. doi: 10.1093/gerona/61.10.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: a pilot study comparing a structured behavioral intervention to a commercial program. Obesity. 2007;15(1):155–164. doi: 10.1038/oby.2007.520. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Pintauro S, Buzzell P, Gold EC. Effect of internet support on the long-term maintenance of weight loss. Obesity Research. 2004;12:320–329. doi: 10.1038/oby.2004.40. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, West D, Krukowski R, Prewitt E, VanBiervliet A, Ashikaga T, et al. Internet delivered behavioral obesity treatment. Preventive Medicine. 2010;51(2):123–128. doi: 10.1016/j.ypmed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helsel DL, Jakicic JM, Otto AD. Comparison of techniques for self-monitoring eating and exercise behaviors on weight loss in a correspondence-based intervention. Journal of the American Dietetic Association. 2007;107(10):1807–1810. doi: 10.1016/j.jada.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Weight loss during the intensive intervention phase of the Weight-Loss Maintenance trial. American Journal of Preventive Medicine. 2008;35(2):118–126. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Weighing the options. Washington, DC: National Academy Press; 1995. [Google Scholar]
- Jula A, Seppanen R. Influence of days of the week on reported food, macronutrient and alcohol intake among an adult. European Journal of Clinical Nutrition. 1999;53(10):808. doi: 10.1038/sj.ejcn.1600853. [DOI] [PubMed] [Google Scholar]
- Kirschenbaum DS. Self-regulatory failure: a review with clinical implications. Clinical Psychology Review. 1987;7:77–104. [Google Scholar]
- Lindstrom J, Peltonen M, Eriksson JG, Aunola S, Hamalainen H, Ilanne-Parikka P, et al. Determinants for the effectiveness of lifestyle intervention in the Finnish Diabetes Prevention Study. Diabetes Care. 2008;31(5):857–862. doi: 10.2337/dc07-2162. [DOI] [PubMed] [Google Scholar]
- Mossavar-Rahmani Y, Henry H, Rodabough R, Bragg C, Brewer A, Freed T, et al. Additional self-monitoring tools in the dietary modification component of the women's health initiative. Journal of the American Dietetic Association. 2004;104(1):76–85. doi: 10.1016/j.jada.2003.10.017. [DOI] [PubMed] [Google Scholar]
- O'Dwyer NA, McCarthy SN, Burke SJ, Gibney MJ. The temporal pattern of the contribution of fat to energy and of food groups to fat at various eating locations: implications for developing food-based dietary guidelines. Public Health Nutrition. 2005;8(03):249–257. doi: 10.1079/phn2004700. [DOI] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. Journal of Consulting and Clinical Psychology. 2001;69(4):722–726. [PubMed] [Google Scholar]
- Perry CL, Baranowski T, Parcel GS. How individuals, environments and health behavior interact: Social Learning Theory. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 1990. [Google Scholar]
- Racette SB, Weiss EP, Schechtman KB, Steger-May K, Villareal DT, Obert KA, et al. Influence of weekend lifestyle patterns on body weight. Obesity. 2008;16(8):1826–1830. doi: 10.1038/oby.2008.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevick MA, Stone RA, Zickmund S, Wang Y, Korytkowski M, Burke LE. Factors associated with probability of personal digital assistant-based dietary self-monitoring in those with type 2 diabetes. Journal of Behavioral Medicine. 2010;33:315–325. doi: 10.1007/s10865-010-9257-9. [DOI] [PubMed] [Google Scholar]
- Streit KJ, Stevens NH, Stevens VJ, Rossner J. Food records: a predictor and modifier of weight change in a long-term weight loss program. Journal of the American Dietetic Association. 1991;91:213–216. [PubMed] [Google Scholar]
- Tate D, Jackvony E, Wing R. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an internet weight loss program. Archives of Internal Medicine. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- Tate D, Wing R, Winett R. Using Internet technology to deliver a behavioral weight loss program. Journal of the American Medical Association. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Bassett D, Swartz A, Strath S, Parr B, Reis J, et al. A preliminary study of one year of pedometer self-monitoring. Annals of Behavioral Medicine. 2004;28(3):158–162. doi: 10.1207/s15324796abm2803_3. [DOI] [PubMed] [Google Scholar]
- Tuomisto MT, Terho T, Korhonen I, Lappalainen R, Tuomisto T, Laippala P, et al. Diurnal and weekly rhythms of health-related variables in home recordings for two months. Physiology & Behavior. 2006;87(4):650–658. doi: 10.1016/j.physbeh.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. New England Journal of Medicine. 2005;353(20):2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Wadden TA, West DS, Neiberg RH, Wing RR, Ryan DH, Johnson KC, et al. One-year weight losses in the Look AHEAD study: Factors associated with success. Obesity. 2009;17(4):713–722. doi: 10.1038/oby.2008.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West DS, Gore SA, DiLillo V, Greene PG, Bursac Z. Motivational interviewing improves weight loss in women with Type 2 Diabetes. Diabetes Care. 2007;30(5):1081–1087. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]
- West DS, Harvey-Berino J, Krukowski RA, Skelly J. Pretreatment Weight Change is Associated with Obesity Treatment Outcomes. Obesity. doi: 10.1038/oby.2011.22. (e-published ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Phelan S. Long-term weight loss maintenance. American Journal of Clinical Nutrition. 2005;82(1):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]